Abstract
Objective
Evaluate the effectiveness of an acute period of cognitive and physical rest on concussion.
Participants
50 consecutive patients with diagnosed concussions.
Design
Participants were assessed before (N=25) and after (N=25) a policy change which incorporated cognitive and physical rest. The Rest group patients were withheld from activities, including classes, for the remainder of the injury day and the following day whereas the No-Rest group patients were not provided any post-injury accommodations.
Main Measures
Patients were assessed on a graded symptom checklist, Balance Error Scoring System, Standard Assessment of Concussion, and computerized neuropsychological tests. The number of days until each test achieved baseline values was compared between groups with independent sample t-test.
Results
The No-Rest group achieved asymptomatic status sooner than the Rest group (5.2±2.9 days and 3.9±1.9 days respectively, P=0.047). There were no differences between groups for time to baseline values on the balance error scoring system, standard assessment of concussion, computerized neuropsychological tests, or time to clinical recovery.
Conclusion
A prescribed day of cognitive and physical rest was not effective in reducing post-concussion recovery time. These results agree with a previous study and suggest that light activity post-concussion may not be deleterious to the concussion recovery process.
Keywords: Concussion, Mild Traumatic Brain Injury, Cognitive Rest, Physical Rest, Recovery
INTRODUCTION
The 4th International Consensus Statement on Concussion in Sport (4th CIS) indicates that cognitive and physical rest are the cornerstone of acute concussion treatment.1 While acknowledging the supporting evidence is sparse; the 4th CIS recommends an initial period of rest in the acute symptomatic time (24–48 hours) post–concussion.1,2 This period of rest is suggested to encompass reduced or limited cognitive, physical, and social activities by restricting school attendance, academic work, electronics usage, and exercise including both sports-related activity and physical education classes.1 In addition to the supposition that this may reduce symptoms and hasten recovery time, it is believed to provide an added benefit of reducing the risk for repeat concussion and the rare, but potentially fatal, second impact syndrome.3–6 Overall, it is generally perceived by clinicians that a day or two of rest will, at worst, do little harm and therefore should be included in concussion management guidelines.7 However, rest as a treatment has been shown to be inappropriate, and potentially harmful, for multiple medical conditions and, as a treatment modality, should be subject to the same methodological study as all treatment paradigms.8–11
The principle of evidence based medicine encompasses the integration of clinical expertise, the best available external clinical evidence, and patient perspective to maximize the care of the individual.12 While clinical expertise supports post-concussion rest, the external clinical evidence is limited and largely derived from animal research.13–15 Physiologically, the rationale for rest is likely based on the post-concussion neurometabolic cascade and the resulting energy crisis, an increased demand for glucose in an environment of reduced cerebral blood flow, which occurs in the first hours and days following a concussion.14 Animal studies have postulated that cognitive or physical post-concussion activity redirects the needed glucose and energy supplies away from brain recovery processes which thereby slows the restoration of neural pathways.13 Consequently, these models have suggested that post-concussion exercise may be associated with delayed neurometabolic recovery whereas rest improved recovery.15,16 There are numerous anecdotal reports suggesting that early post-concussive activity is associated with impaired academic performance along with a recurrence or exacerbation of concussion related symptoms.4,17–19 Similarly, periods of post-concussion rest have been reported to reduce symptoms and allow a quicker recovery.4
These anecdotal reports of improved recovery with post-concussion rest are not fully supported by the external clinical evidence.7,20,21 Rather, a trend is appearing whereby too little or too much activity may impair recovery. Majerske, based on retrospective chart review, suggested those individuals who had either the lowest (defined as no school or exercise activity) or highest (full school activity and game participation) level of post-concussion activity were associated with the poorest outcomes based on computerized neuropsychological testing (CNT).20 Conversely, those classified as performing light activity (defined as school activity and light activity at home such as slow jogging or mowing the lawn) had improved recovery on CNT.20 Further, Brown recently reported that individuals with the highest cognitive activity had the slowest symptom based recovery; however, the lowest and moderate activity level individual demonstrated similar recovery curves, albeit statistical results were not reported on these groups.21 Finally, a recommendation for five days of strict rest was not advantageous over two days of rest amongst adolescents presenting to a pediatric emergency department.22 This limited clinical evidence, while largely inconclusive, may suggest too little or too much activity could be detrimental to concussion recovery.
Recently there has been a rise in the number of sports concussion clinics which treat athletes and community members who suffer concussions outside of the more traditional athletic health care system wherein treatment is provided by athletic trainers and team physicians.23 Within this model, Moser identified significant improvements in CNT and symptoms following a prescribed one week of cognitive and physical rest.24 Conversely, in a similar model, a retrospective cohort study failed to identify improved recovery, based on time to symptom resolution, in those individuals provided recommendations of cognitive rest.7 These studies investigated patients with delayed recovery as participants had high initial symptom scores despite the initial evaluation occurring an average of 19 – 36 days post-injury.7,24 This may be indicative of a referral bias, whereby cases perceived as more severe were seen at the clinics, as the 4th CIS suggests 80 – 90% of concussions resolve within 7 – 10 days.1
Cognitive and physical rest is now routinely recommended following a sports-related concussion.1,7 However, there is limited evidence supporting this recommendation and no prospective studies investigate the effectiveness of acute cognitive and physical rest immediately post-concussion as recommended by the 4th CIS. Therefore, the purpose of this study was to evaluate the effectiveness of one day of cognitive and physical rest on traditional concussion recovery metrics amongst a population of college aged student–athletes. We hypothesize that individuals who were recommended rest would have shorter time to recovery.
METHODS
Participants
The participants for this study were drawn from a prospective study on concussion management and this study was based on a policy change to incorporate cognitive and physical rest into the recovery protocol. Specifically, the Sports Medicine staff (team physicians and athletic trainers) revised the concussion management protocol in July 2012, independent of this research study, such that all student-athletes with diagnosed concussions thereafter were withheld from all activities for the remainder of that day and were provided for one additional day of cognitive and physical rest. The first cohort was a 25 participant “No-Rest” group that suffered concussions over the two academic years prior to July 2012 and were not prescribed rest. This group consisted of all eligible participants who met the inclusion and exclusion criteria prior to July 2012. The second cohort was a 25 participant “Rest” group who were prescribed cognitive and physical rest. This group consisted of the first 25 concussions after the protocol change that met the inclusion and exclusion criteria. This approach did not allow for matching; however, the two groups were relatively homogeneous. (Table 1)
Table 1. Participant Demographics.
The individuals participated in football (N=24), soccer (N=10), cheerleading (N=9), basketball (N=4), swimming (N=1), tennis (N=1), baseball (N=1).
| Gender | Age (years) | Height (m) | Weight (kg) | Previous Concussions | LOC | PTA | |
|---|---|---|---|---|---|---|---|
| Rest | 18M/7F | 19.8 ± 1.2 | 1.73 ± 0.08 | 80.9 ± 20.1 | 0.6 ± 0.7 | 12.0% | 28.0% |
| No Rest | 13M/12F | 19.4 ± 1.3 | 1.75 ± 0.13 | 82.2 ± 25.0 | 0.8 ± 0.9 | 12.0% | 44.0% |
There were no significant differences (P>0.05) between groups for demographic characteristics, injury history, or acute injury presentation.
The inclusion criteria for participation were patients suffering a typically recovering (resolution within a month of injury) concussion, had complete baseline data available, and had completed the institution specific return to participation protocol. Participants were excluded from the study if they suffered a substantial comorbidity (e.g., suspected cervical injury), suffered another injury prior to full return to participation, or had incomplete baseline data. Four potential participants did not meet inclusion/exclusion criteria (one suspected cervical spine injury, three without complete baseline data) and were thus not included in the 50 participants. The concussions were initially identified by a certified athletic trainer and then confirmed independently through clinical examination by a licensed physician using standard diagnostic criteria consistent with the 4th CIS.1 All participants provided written and oral informed consent as approved by the institutional review board.
Instruments
The concussion clinical assessment battery herein included 1) a graded symptom checklist (GSC), 2) the Immediate Post-Concussion Assessment and Cognitive Testing (ImPACT) computerized neuropsychological test (CNT), 3) the Balance Error Scoring System (BESS), and 4) Standard Assessment of Concussion (SAC) tests. This clinical assessment battery has been thoroughly described in the literature.1,25–27 Briefly, the BESS is the most commonly utilized and recommended balance test which consists of 3 stances (double, single, and tandem) on 2 surfaces (firm and foam).1,28 The BESS is scored by summing the number of errors committed per stance, with a maximum of 10 errors per stance and therefore 60 total errors, with a lower score representing better balance.29,30 The SAC is a brief mental screening with four sections (orientation, immediate recall, concentration, and delayed recall) designed to identify impairments in cognitive processing following a concussion.31 The SAC is scored out of a possible 30 points with a higher score representing better cognitive performance.31 The GSC required participants to self-report the presence and severity of 22 common concussion symptoms on a 0 – 6 scale (0: symptom not present, 6: most severe) with a potential range of 0 – 132.32 Finally, ImPACT is a widely utilized CNT consisting of 6 test modules which renders 4 composite scores and has acceptable reliability, validity, sensitivity, and specificity.28,33
Procedures
In the summer of 2012, the sports medicine staff, the athletic trainers and team physicians, revised the concussion management policies to incorporate cognitive and physical rest consistent with the recommendations of the 3rd CIS.34 Specifically, beginning July 1, 2012, all student-athletes with diagnosed concussions were withheld from all activities for the remainder of that day and were provided for one additional day of cognitive and physical rest. On this defined “rest” day, the student-athlete was instructed to not attend any classes, team meetings or study hall, as well as not perform academic work (e.g., homework, studying for exams, writing papers), refrain from excessive television, computer or other electronics usage, and to limit text messaging. Similarly, to encourage physical rest, injured student-athletes were withheld from all athletic activities (e.g., team or individual practice, strength and conditioning sessions, treatment for other injuries), personal exercise (e.g., campus recreation facilities), and instructed to rest in a quiet environment throughout the day with the exception of reporting to the athletic training room for their concussion follow-up assessment. Specifically, the student-athlete was provided medical documentation for the class absence from the Student Disabilities Services office and coaches were instructed the individuals were not to partake in team activities of any kind that day. All members of the Rest group completed this protocol and every participant in this group only was directly asked, by both their treating athletic trainer and a member of the research team separately, about their compliance with the rest instructions. Patient self-report of activity level was documented by both the treating clinician and a member of the research team. The No-Rest group suffered their sports-related concussion prior to July 1, 2012, were not provided any cognitive rest-related accommodations following the concussion and were not excused from attending classes/team meeting the following day and were also not excused from any homework assignments, tests, or projects. The research team was not able to confirm class attendance; however, the intercollegiate athletics programs closely monitors classroom attendance and absence is strongly discouraged. The No-Rest group was withheld from participation in intercollegiate athletics and workouts while symptomatic; however, no additional restrictions were placed on their activities of daily living outside of intercollegiate athletics.
Both groups completed a standard post-concussion return to participation protocol which closely mirrored the recommendations of the 3rd CIS.34 Specifically, the participants were withheld from all team related physical activity (e.g., practice, games, workouts) until they self-reported being asymptomatic and achieved baseline values on the clinical battery (SAC, BESS, and CNT). The No-Rest group was allowed to attend and observe practices and/or games, attend team meetings, and were not excused from classes/homework/exams during this symptomatic time period. The Rest group was withheld from these activities for the remainder of the day they suffered the concussion as well as the subsequent day. Once the individual achieved baseline values on the clinical battery and self-reported asymptomatic, both groups began an identical 7 day progressive return protocol consistent with the 3rd and 4th CIS recommendations.1,34 At the completion of the protocol, pending physician evaluation, they received clearance for full unrestricted sports participation on day 7. Both groups completed the identical recovery protocol once baseline scores were achieved.
The clinical testing battery commenced on the day following the concussion and consisted of the complete testing battery – the GSC, BESS, SAC, and CNT. All testing procedures were consistent with contemporary clinical assessment techniques.1,28 All participants completed the GSC in an interview format with a certified athletic trainer who recorded the number and intensity of the symptoms. The SAC and BESS were performed in a quiet area with limited distractions and assessed by a certified athletic trainer in an environment similar to the baseline testing procedures. The CNT was performed independently in a private office without any other individuals present which differed from the group testing which occurred at baseline. Thereafter, participants completed the GSC daily until they were self-reported asymptomatic. Once asymptomatic, the BESS and SAC were readministered daily until the individual achieved their baseline values. The CNT was also readministered every 2 – 3 days after asymptomatic until the individual’s four composite scores no longer exceeded the reliable change index on a valid test.
Data and Statistical Analysis
There were five primary dependent variables in the study, 1) the number of days till the participant was symptom free; the number of days till baseline values were met or exceeded on the 2) CNT, 3) BESS, and 4) SAC; and 5) time till clinical recovery. The four assessment values were operationally defined as the day the individual, when compared to baseline, committed equal or fewer errors on BESS, an equal or higher score on SAC, had all 4 CNT composite scores not exceeding the reliable change index on a valid test, and self-reported asymptomatic. The time to clinical recovery was defined as the number of days until all tests were baseline and the participant would begin the progressive exercise program for the purpose of return to participation. Multiple participants “passed” components of the clinical battery on day 1 post-injury (e.g., SAC score was equal to or higher than baseline) despite self-reporting concussion symptoms and were classified as recovered on day 1 for the specific test (SAC: 40%, BESS: 36%, CNT: 10%). Further, multiple individuals endorsed symptoms during baseline preseason testing; however, the concussion management protocol required the individual to be asymptomatic (a GSC total score of “0”) without the use of medications in order to be classified as asymptomatic. The number of days until recovery on each of the five dependent variables was compared between groups (Rest vs No Rest) with independent sample t-tests. However, as Clinical Recovery is not independent of the other four dependent variables, a Bonferroni correction was applied to set the alpha level at 0.25 for this specific dependent variable. As a secondary analysis, the 4 composite scores of CNT were compared with a 2 (group) × 2 (test session) repeated measures ANOVA.
RESULTS
There were no differences between groups for demographic characteristics, concussion history, initial concussion presentation, or baseline scores on the clinical assessment battery. (Tables 1 and 2, Figures 1 and 2) There were also no significant differences in initial severity of the concussion as indicated by the change in BESS (P=0.842), SAC (P=0.808), or GSC (P=0.517). (Figures 1 and 2)
Table 2.
ImPACT Composite Scores at Baseline and Day 1 Post-Injury.
| CNT Baseline Values | ||||
|---|---|---|---|---|
| Verbal Memory | Visual Memory | Processing Speed | Reaction Time | |
| Rest Group | 87.4 ± 8.2 | 71.4 ± 11.6 | 39.6 ± 5.3 | 0.58 ± 0.06 |
| No–Rest Group | 85.8 ± 8.5 | 76.9 ± 9.4 | 40.9 ± 5.9 | 0.56 ± 0.07 |
| CNT Post – Injury Values | ||||
| Verbal Memory | Visual Memory | Processing Speed | Reaction Time | |
| Rest Group | 84.1 ± 9.9 | 73.5 ± 13.2 | 37.2 ± 6.8 | 0.63 ± 0.07† |
| No–Rest Group | 78.1 ± 13.4† | 64.4 ± 14.6*† | 36.3 ± 7.9† | 0.67 ± 0.17† |
There were no significant differences between groups at baseline.
The No-Rest group was had a significantly lower Visual Memory composite score (P=0.026) at Day 1 Post–Injury.
There was a significant difference within group between Baseline and Day 1 Post – Injury.
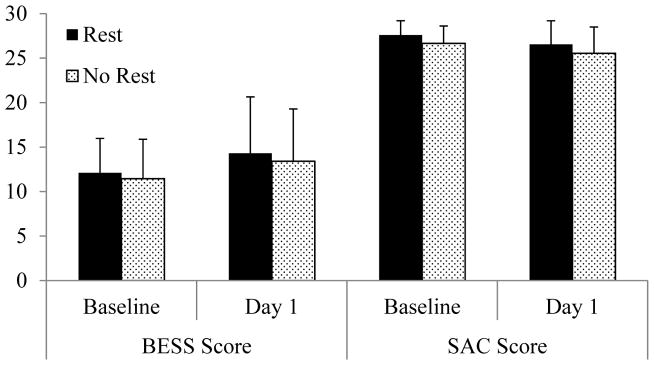
Figure 1. SAC and BESS Scores at Baseline and Day 1 Post–Injury.
For the BESS, there were no differences between Rest and No-Rest groups at Baseline (12.1 ± 3.9 errors and 11.5 ± 4.4 errors respectively, P=0.578), on Day 1 (14.3 ± 6.3 errors and 13.4 ± 5.9 errors respectively, P=0.608), or the change from Baseline to Day 1 (2.2 ± 5.8 errors and 2.0 ± 5.6 errors respectively, P=0.883). For the SAC, there were no differences between Rest and No-Rest groups at Baseline (27.6 ± 1.6 errors and 26.7 ± 1.9 errors respectively, P=0.073), on Day 1 (26.6 ± 2.6 errors and 25.5 ± 3.0 errors respectively, P=0.209), or the change from Baseline to Day 1 (1.0 ± 2.8 errors and 1.1 ± 3.1 errors respectively, P=0.920).
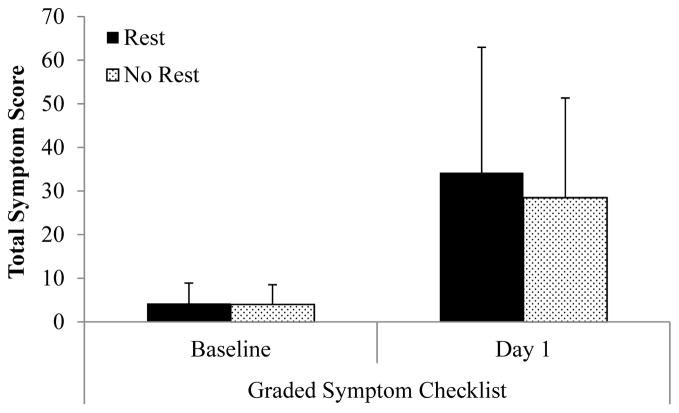
Figure 2. Graded Symptom Checklist Scores at Baseline and Day 1 Post–Injury.
There were no differences between Rest and No-Rest groups at Baseline (4.2 ± 4.7 and 4.0 ± 4.5 respectively, P=0.854), at Day 1 (34.2 ± 28.7 and 28.5 ± 22.9 respectively, P=0.437), and for change between Baseline and Day 1 (30.0 ± 27.8 and 25.2 ± 23.7 respectively, P=0.517). There was a significant increase within groups for both Rest (P<0.001) and No-Rest (P<0.001) between Baseline and Day 1.
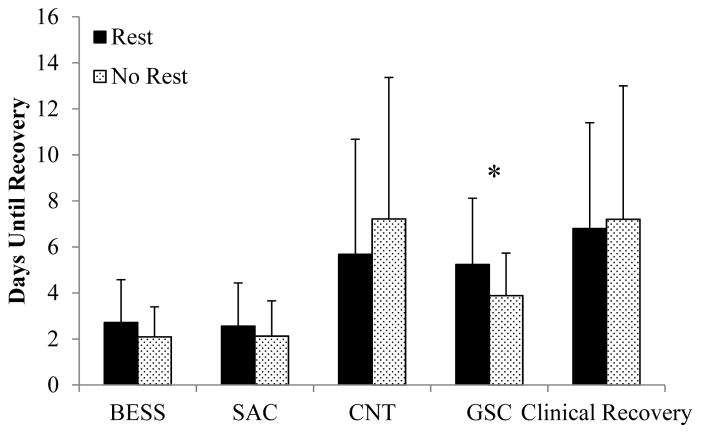
The Rest group was symptomatic significantly longer than the No-Rest group (5.2 ± 2.9 days and 3.9 ± 1.9 days respectively, t=2.035, P=0.047). There was no difference between Rest and No-Rest group for time to baseline for the BESS (2.7 ± 1.9 days and 2.1 ± 1.3 days respectively, P=0.183), SAC (2.6 ± 1.9 days and 2.1 ± 1.5 days respectively, P=0.368), CNT (5.7 ± 5.0 days and 7.1 ± 6.3 days respectively, P=0.395) or the time to clinical recovery (6.8 ± 4.6 days and 7.2 ± 5.8 days respectively, P=0.809). (Figure 3) The No-Rest group had significantly lower Visual Memory Composite score compared to the Rest group on Day 1 post-injury. Acutely post-injury, the No-Rest group had significant reductions in all 4 composite scores compared to their baseline performance whereas the Rest group only demonstrated significant reductions in Reaction Time composite score. (Table 2)
Figure 3. Days to baseline values for each clinical measure between the Rest and No-Rest groups.
*There was a significant difference between groups for time to self-report symptom free status (Rest: 5.2 ± 2.9 days and No-Rest: 3.9 ± 1.9 days, t=2.035, P=0.047). (BESS: Balance Error Scoring System; SAC: Standard Assessment of Concussion; CNT: Computerized Neuropsychological Testing; GSC: Graded Symptom Checklist; Clinical Recovery: Number of Days until Baseline on All Tests).
DISCUSSION
The recommendation for cognitive and physical rest is now standard in most concussion position and consensus statements.1,27,35,36 The limited previous studies addressing the value of rest had used either retrospective design or assessed atypical patient groups and identified inconsistent results. Therefore, we evaluated 50 consecutive concussion participants before and after a policy change to incorporate an acute period of cognitive and physical rest. The main finding of this study was the No-Rest group was asymptomatic significantly earlier (1.3 days) than the Rest group and there were no differences between groups in recovery time for BESS, SAC, CNT, and clinical recovery. The average Rest group participant in this study received approximately 40 hours of cognitive and physical rest assuming a rest period from a 4 pm concussion till academic class beginning at 8am after the rest day (e.g., from ~4 pm Wednesday till 8 am Friday morning). Within the context of this design and specific to college student-athletes, these results suggest that a day of cognitive and physical rest during the acute post-concussion period was not effective at improving concussion recovery in this sample of 50 participants.
The prescribed rest period is endorsed by expert opinion and supported by anecdotal evidence suggesting that post-concussion cognitive and physical rest is associated with reduced time to recovery.1,4 In patients with atypical prolonged recovery, cognitive and physical rest appeared to have some effectiveness in reducing post-concussion symptoms and improving CNT performance.7,24 However, Majerske suggested that light activity, as opposed to either absolute rest or full activity, was associated with improved recovery in high school athletes.20 Further, Brown reported those with the highest levels of cognitive activity experienced delayed recovery, but complete rest and low activity recovered similarly.21 Prolonging rest, up to five days, may also not be effective at improving recovery rates in the pediatric population.22 Herein, we investigated typical concussions, individuals who recovered within a month,26,37 and found a shorter time to asymptomatic status in the No-Rest group and no differences between groups in recovery times across the objective clinical assessment battery. Taken together, these results could suggest that light activity may not be detrimental in the acute recovery process and that acute cognitive and physical rest may not be associated with shortened recovery.
This finding runs contrary to our hypothesis, expert opinion, and anecdotal evidence which all suggested that an acute period of rest would be beneficial in the recovery process. One possible explanation is the prescribed rest, which included removal from academic and team functions, may increase depression risk and decreased physical capacity as the patient is removed from their regular activities of daily living.49 Indeed, just three days of bed rest reduces exercise performance and neurohormonal response to exercise with reductions greatest in those with the highest fitness levels.10 Further, fatigue and somatic depressive symptoms emerge within 7 days of exercise cessation.11 While it’s unlikely a single day of rest would result in clinically diagnosed depression, concussions do result in increased mood disorder and anxiety which could be exacerbated by removal from the patient’s normal activities.38,39 Thomas suggested that “situational depression”, the emotional distress associated with school and activity restriction, was a contributing factor to the lack of improvement from five days of strict rest.22 This could be particularly pertinent to concussion management as concussions have often been referred to as an “invisible injury” and athletes have reported being questioned about the legitimacy of their injury.40,41 Symptoms are state dependent and can be influenced by extensive psychosocial, personal, and emotional characteristics.42 It is important to note that symptoms typically resolve slower post-concussion than clinical balance and cognitive assessments.25,26 Thus, removing the individual from their normal environment and activities of daily living could exacerbate or prolong concusion symptoms.
A gold-standard for identification of concussion recovery remains elusive, but clinically it is commonly defined as achieving or exceeding baseline values on balance, cognitive, and CNT as well as self-reporting asymptomatic.1,27 The resolution of concussion symptoms is a core component of appropriate concussion management and, along with a clinical examination, is the indicator most relied upon in clinical settings to determine a student-athlete’s recovery.1,7,28,37 Surprisingly, the No-Rest group in this study self-reported being asymptomatic an average of 1.3 days earlier than the Rest group. While it is beyond the scope of this study to identify all potential influences of symptom reporting, it is important to note that several common confounders were unlikely to have influenced these results. Specifically, females tend to report a greater number, severity, and duration of concussion symptoms;43 however, the No-Rest group (N=12) had more female participants than the Rest group (N=7). Further, premorbid health status has been associated with time to symptom resolution.44 There were no differences between groups for GSC at baseline (P=0.854), initial post-injury (P=0.437), or change from baseline to post-injury (P=0.457). (Figure 2) It is important to note there is no “gold-standard” symptom checklist in the literature and this study was delimited to the 22-item GSC endorsed by the 3rd CIS in the SCAT–2 assessment tool.34
In an effort to improve concussion management beyond patient self-report of symptoms; objective balance, cognitive, and CNT assessments have been developed.31,33 Following a concussion, BESS and SAC typically resolve within several days of injury and both groups herein averaged 2 – 3 days for recovery on these tests.25,26 The participants were assessed on both tests on the day following injury and the average BESS score increased, worsened, by 2.1 errors and the average SAC score decreased 1.1 points and these changes were not different between groups. The impairments noted are consistent with several large studies for changes on the day following a concussion.25,26,37 Similarly, individuals typically achieve baseline values on CNT within a week and the participants herein generally recovered within these timeframes.33 The No-Rest group appeared to present worse on CNT testing on Day 1 with all four composite scores being significantly worse than baseline whereas the Rest group only had a significant impairment in the Reaction Time Composite. Further, the No–Rest group had a significantly worse score on the Visual Memory Composite than the Rest group. (Table 2) This generally worse initial presentation for the No-Rest group can potentially explain their non-significant 1.4 day delay in achieving baseline values compared to the Rest group. It is important to the note that only the number of days until all four composite scores achieved baseline values was utilized to define recovery as clinically this would be the time point when the individual was progressed in the concussion management plan. These findings suggest that an acute period of rest did not improve recovery time on objective clinical concussion assessments.
Concussions are inherently unique to the individual and the recovery process may vary accordingly.36 However, by several metrics (e.g., poorer initial performance on CNT, higher rate of PTA), the No-Rest group appeared to have a poorer initial presentation suggesting this may not be associated with recovery time. McCrea recently reported the presence of loss of consciousness (LOC), post-traumatic amnesia (PTA), and increased initial symptoms are associated with prolonged recovery.37 However, the No-Rest group herein had a higher rate of PTA (44% to 28%) and there were no differences between groups for LOC rate and initial symptom severity. Thus, for rest recommendations related to typical recovering concussions, the initial presentation of the injury does not appear to influence recovery time.
The participants in the Rest group were instructed to reduce cognitive and physical activity for the remainder of the injury day as well as the following day, an average of approximately 40 hours from the time of their concussion. The participant’s athletic trainer and/or member of the research team specifically queried the participants’ compliance daily; however, the research team had no additional method available to confirm compliance and accuracy of participant reporting. Patient self-report, however limited, has been the predominate method for tracking cognitive and physical activity post-concussion, typically by reporting activity over a week or longer window.7,20–22,24 Ideally accelerometers, pedometers, or activity tracking devices could be utilized to quantify physical activity and this could be incorporated into future studies. Further, the No-Rest group’s activity was not monitored by the research team; however, it is unlikely these participants would have skipped classes or team activities as this was strongly disincentivized by coaches and athletic administrators. The Rest group deviated from the concept of total rest by reporting to the athletic training room for a medical evaluation which included the concussion clinical assessment battery on the designated rest day. However, this is likely consistent with standard concussion management protocols, but must be considered when extrapolating the results of this study. Further, the exact time of each concussion was not recorded and thus the 40 hours of rest is an approximation based on chart review of the injury and the normal team practice or game times. The focus herein is on the additional day of rest as both groups would have been recommended to rest the remainder of the injury day. All participants herein were medically managed by the same sports medicine staff following the same protocols and assessment batteries; however, there were multiple individual certified athletic trainers involved in the care of the student-athletes which may also limit the extrapolation of the results. Finally, the no-rest group was delimited to concussions which occurred between August 2010 and July 2012 as CNT was not initiated by the host institution until the Fall 2010 seasons; however, three potential participants suffered concussions within this time frame but were excluded for not having CNT baseline data.
The main finding of this study was the lack of a reduced time to recovery amongst college–aged student–athletes who were provided an acute cognitive and physical rest period following a sports-related concussion. The most common predictors of delayed recovery; including being female, poorer initial presentation, higher baseline symptoms, and poorer CNT test performance, were either statistically worse in the No-Rest group or were not different between groups. This suggests that a single day of prescribed cognitive and physical rest in the acute post-concussion period was not effective at reducing recovery time. However, it is not known if the duration of post-concussion rest, approximately 40 hours, was insufficient to provide the theoretical benefits believed to be associated with post-concussion rest. Participants in this study were within the 24 – 48 hours of rest recommended by the 3rd CIS; however, future studies should investigate a longer rest period, incorporating light exercise earlier in recovery, and tracking cognitive and physical activity throughout the recovery process.1 Further, although symptom resolution was quicker in the No-Rest group, it is important to note that symptoms are a purely subjective report and it is suspected that patients may deny the presence of symptoms in an effort to hasten return to participation.45,46 Finally, this study adds to the growing body of literature which suggests that an acute period cognitive and physical rest may not be an effective at reducing post-concussion recovery time.
Footnotes
Conflict of Interest: There are no conflicts of interest for any of the authors associated with this manuscript.
Funding Disclosure: This project was funded by the National Institute of Health/Neurological Disorders and Stroke (1R15NS070744). The funding agency had no role in the development of the manuscript or the decision to submit to the Journal of Head Trauma Rehabilitation.
References
- 1.McCrory P, Meeuwisse WH, Aubry M, et al. Consensus statement on concussion in sport: the 4th international conference on concussion in sport, zurich, November 2012. J Athl Train. 2013;48(4):554–575. doi: 10.4085/1062-6050-48.4.05. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Schneider KJ, Iverson GL, Emery CA, McCrory P, Herring SA, Meeuwisse WH. The effects of rest and treatment following sport-related concussion: a systematic review of the literature. Br J Sports Med. 2013;47(5):304–307. doi: 10.1136/bjsports-2013-092190. [DOI] [PubMed] [Google Scholar]
- 3.Cantu RC. Second-impact syndrome. Clin Sports Med. 1998;17(1):37–44. doi: 10.1016/s0278-5919(05)70059-4. [DOI] [PubMed] [Google Scholar]
- 4.Logan K. Cognitive Rest Means I Can’t Do What?! Athletic Training and Sports Health Care. 2009;1(6):251–252. [Google Scholar]
- 5.Guskiewicz KM, McCrea M, Marshall SW, et al. Cumulative effects associated with recurrent concussion in collegiate football players: the NCAA Concussion Study. JAMA. 2003;290(19):2549–2555. doi: 10.1001/jama.290.19.2549. [DOI] [PubMed] [Google Scholar]
- 6.McCrea M, Guskiewicz K, Randolph C, et al. Effects of a Symptom-Free Waiting Period on Clinical Outcome and Risk of Reinjury After Sport-Related Concussion. Neurosurgery. 2009;65(5):876–882. doi: 10.1227/01.NEU.0000350155.89800.00. [DOI] [PubMed] [Google Scholar]
- 7.Gibson S, Nigrovic LE, O’Brien M, Meehan WP., 3rd The effect of recommending cognitive rest on recovery from sport-related concussion. Brain Inj. 2013;27(7–8):839–842. doi: 10.3109/02699052.2013.775494. [DOI] [PubMed] [Google Scholar]
- 8.Silverberg ND, Iverson GL. Is rest after concussion “the best medicine?”: recommendations for activity resumption following concussion in athletes, civilians, and military service members. J Head Trauma Rehabil. 2013;28(4):250–259. doi: 10.1097/HTR.0b013e31825ad658. [DOI] [PubMed] [Google Scholar]
- 9.Allen C, Glasziou P, Del Mar C. Bed rest: a potentially harmful treatment needing more careful evaluation. Lancet. 1999;354(9186):1229–1233. doi: 10.1016/s0140-6736(98)10063-6. [DOI] [PubMed] [Google Scholar]
- 10.Smorawinski J, Nazar K, Kaciuba-Uscilko H, et al. Effects of 3-day bed rest on physiological responses to graded exercise in athletes and sedentary men. J Appl Physiol. 2001;91(1):249–257. doi: 10.1152/jappl.2001.91.1.249. [DOI] [PubMed] [Google Scholar]
- 11.Berlin AA, Kop WJ, Deuster PA. Depressive mood symptoms and fatigue after exercise withdrawal: The potential role of decreased fitness. Psychosom Med. 2006;68(2):224–230. doi: 10.1097/01.psy.0000204628.73273.23. [DOI] [PubMed] [Google Scholar]
- 12.Sackett DL, Rosenberg WMC, Gray JAM, Haynes RB, Richardson WS. Evidence based medicine: What it is and what it isn’t - It’s about integrating individual clinical expertise and the best external evidence. Br Med J. 1996;312(7023):71–72. doi: 10.1136/bmj.312.7023.71. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Crane AT, Fink KD, Smith JS. The effects of acute voluntary wheel running on recovery of function following medial frontal cortical contusions in rats. Restor Neurol Neurosci. 2012;30(4):325–333. doi: 10.3233/RNN-2012-120232. [DOI] [PubMed] [Google Scholar]
- 14.Giza CC, Hovda DA. The neurometabolic cascade of concussion. J Athl Train. 2001;36(3):228–235. [PMC free article] [PubMed] [Google Scholar]
- 15.Griesbach GS, Hovda DA, Molteni R, Wu A, Gomez-Pinilla F. Voluntary exercise following traumatic brain injury: brain-derived neurotrophic factor upregulation and recovery of function. Neurosci. 2004;125(1):129–139. doi: 10.1016/j.neuroscience.2004.01.030. [DOI] [PubMed] [Google Scholar]
- 16.Ouyang L, Xiao Y, Yue C, et al. Quiet rest ameliorates biochemical metabolism in the brain in a simple concussion rabbit model Evaluation of hydrogen proton magnetic resonance spectroscopy. Neural Regen Res. 2011;6(33):2617–2621. [Google Scholar]
- 17.Grady MF, Master CL, Gioia GA. Concussion Pathophysiology: Rationale for Physical and Cognitive Rest. Pediatr Annu. 2012;41(9):377–382. doi: 10.3928/00904481-20120827-12. [DOI] [PubMed] [Google Scholar]
- 18.Gioia GA, Vaughan C, Reesman J. Characterizing Post-Concussion Exertional Effects n the Child and Adolescent. J Int Neuropsychol Soc. 2010;16(S1):178. [Google Scholar]
- 19.Solomon GS. A comment on “exertion” after sports-related concussion. J Neuropsychiatry Clin Neurosci. 2007;19(2):195–196. doi: 10.1176/jnp.2007.19.2.195. [DOI] [PubMed] [Google Scholar]
- 20.Majerske CW, Mihalik JP, Ren D, et al. Concussion in sports: Postconcussive activity levels, symptoms, and neurocognitive performance. J Athl Train. 2008;43(3):265–274. doi: 10.4085/1062-6050-43.3.265. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Brown NJ, Mannix RC, O’Brien MJ, Gostine D, Collins MW, Meehan WP., 3rd Effect of cognitive activity level on duration of post-concussion symptoms. Pediatrics. 2014;133(2):e299–304. doi: 10.1542/peds.2013-2125. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Thomas DG, Apps JN, Hoffmann RG, McCrea M, Hammeke T. Benefits of Strict Rest After Acute Concussion: A Randomized Controlled Trial. Pediatrics. 2015;5:2014–0966. doi: 10.1542/peds.2014-0966. [DOI] [PubMed] [Google Scholar]
- 23.Reynolds E, Collins MW, Mucha A, Troutman-Ensecki C. Establishing a clinical service for the management of sports-related concussions. Neurosurgery. 2014;75(4):S71–81. doi: 10.1227/NEU.0000000000000471. [DOI] [PubMed] [Google Scholar]
- 24.Moser RS, Glatts C, Schatz P. Efficacy of Immediate and Delayed Cognitive and Physical Rest for Treatment of Sports-Related Concussion. J Pediatrics. 2012;161(5):922–926. doi: 10.1016/j.jpeds.2012.04.012. [DOI] [PubMed] [Google Scholar]
- 25.McCrea M, Barr WB, Guskiewicz K, et al. Standard regression-based methods for measuring recovery after sport-related concussion. J Int Neuropsychol Soc. 2005;11(1):58–69. doi: 10.1017/S1355617705050083. [DOI] [PubMed] [Google Scholar]
- 26.McCrea M, Guskiewicz KM, Marshall SW, et al. Acute effects and recovery time following concussion in collegiate football players: the NCAA Concussion Study. JAMA. 2003;290(19):2556–2563. doi: 10.1001/jama.290.19.2556. [DOI] [PubMed] [Google Scholar]
- 27.Broglio SP, Cantu RC, Gioia GA, et al. National Athletic Trainers’ Association position statement: management of sport concussion. J Athl Train. 2014;49(2):245–265. doi: 10.4085/1062-6050-49.1.07. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Kelly KC, Jordan EM, Burdette GT, Buckley TA. NCAA Division I Athletic Trainers Concussion Management Practice Patterns. J Athl Train. 2014;49(5):665–673. doi: 10.4085/1062-6050-49.3.25. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Burk JM, Munkasy BA, Joyner AB, Buckley TA. Balance error scoring system performance changes after a competitive athletic season. Clin J Sport Med. 2013;23(4):312–317. doi: 10.1097/JSM.0b013e318285633f. [DOI] [PubMed] [Google Scholar]
- 30.Rahn C, Munkasy BA, Barry Joyner A, Buckley TA. Sideline Performance of the Balance Error Scoring System during a Live Sporting Event. Clin J Sport Med. 2014 Aug 5; doi: 10.1097/JSM.0000000000000141. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.McCrea M, Kelly JP, Randolph C, et al. Standardized assessment of concussion (SAC): On-site mental status evaluation of the athlete. J Head Trauma Rehabil. 1998;13(2):27–35. doi: 10.1097/00001199-199804000-00005. [DOI] [PubMed] [Google Scholar]
- 32.Collins MW, Iverson GL, Lovell MR, McKeag DB, Norwig J, Maroon J. On-field predictors of neuropsychological and symptom deficit following sports-related concussion. Clin J Sport Med. 2003;13(4):222–229. doi: 10.1097/00042752-200307000-00005. [DOI] [PubMed] [Google Scholar]
- 33.Echemendia RJ, Iverson GL, McCrea M, et al. Advances in neuropsychological assessment of sport-related concussion. Br J Sports Med. 2013;47(5):294–298. doi: 10.1136/bjsports-2013-092186. [DOI] [PubMed] [Google Scholar]
- 34.McCrory P, Meeuwisse W, Johnston K, et al. Consensus statement on concussion in sport: the 3rd International Conference on Concussion in Sport held in Zurich, November 2008. J Athl Train. 2009;44(4):434–448. doi: 10.4085/1062-6050-44.4.434. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Harmon KG, Drezner JA, Gammons M, et al. American Medical Society for Sports Medicine position statement: concussion in sport. Br J Sports Med. 2013;47(1):15–26. doi: 10.1136/bjsports-2012-091941. [DOI] [PubMed] [Google Scholar]
- 36.Herring SA, Cantu RC, Guskiewicz KM, et al. Concussion (mild traumatic brain injury) and the team physician: a consensus statement--2011 update. Med Sci Sports Exerc. 2011;43(12):2412–2422. doi: 10.1249/MSS.0b013e3182342e64. [DOI] [PubMed] [Google Scholar]
- 37.McCrea M, Guskiewicz K, Randolph C, et al. Incidence, Clinical Course, and Predictors of Prolonged Recovery Time Following Sport-Related Concussion in High School and College Athletes. J Int Neuropsychol Soc. 2013;19(1):22–33. doi: 10.1017/S1355617712000872. [DOI] [PubMed] [Google Scholar]
- 38.Hutchison M, Mainwaring LM, Comper P, Richards DW, Bisschop SM. Differential Emotional Responses of Varsity Athletes to Concussion and Musculoskeletal Injuries. Clin J Sport Med. 2009;19(1):13–19. doi: 10.1097/JSM.0b013e318190ba06. [DOI] [PubMed] [Google Scholar]
- 39.Wood RL, McCabe M, Dawkins J. The role of anxiety sensitivity in symptom perception after minor head injury: An exploratory study. Brain Inj. 2011;25(13–14):1296–1299. doi: 10.3109/02699052.2011.624569. [DOI] [PubMed] [Google Scholar]
- 40.Echlin PS. Concussion education, identification, and treatment within a prospective study of physician-observed junior ice hockey concussions: social context of this scientific intervention. Neurosurg Focus Nov. 2010;29(5):E7. doi: 10.3171/2010.10.FOCUS10222. [DOI] [PubMed] [Google Scholar]
- 41.Moreau MS, Langdon J, Buckley TA. The Lived Experience of an In-Season Concussion Amongst NCAA Division I Student-Athletes. Int J Exerc Sci. 2014;7(1):62–74. [Google Scholar]
- 42.Alla S, Sullivan SJ, McCrory P. Defining asymptomatic status following sports concussion: fact or fallacy? Br J Sports Med. 2012;46(8):562–569. doi: 10.1136/bjsm.2010.081299. [DOI] [PubMed] [Google Scholar]
- 43.Covassin T, Elbin RJ. The Female Athlete: The Role of Gender in the Assessment and Management of Sport-Related Concussion. Clin Sports Med. 2011;30(1):125–131. doi: 10.1016/j.csm.2010.08.001. [DOI] [PubMed] [Google Scholar]
- 44.McLean SA, Kirsch NL, Tan-Schriner CU, et al. Health status, not head injury, predicts concussion symptoms after minor injury. Am J Emerg Med. 2009;27(2):182–190. doi: 10.1016/j.ajem.2008.01.054. [DOI] [PubMed] [Google Scholar]
- 45.McCrea M, Hammeke T, Olsen G, Leo P, Guskiewicz K. Unreported concussion in high school football players: implications for prevention. Clin J Sport Med. 2004;14(1):13–17. doi: 10.1097/00042752-200401000-00003. [DOI] [PubMed] [Google Scholar]
- 46.Register-Mihalik JK, Linnan LA, Marshall SW, McLeod TCV, Mueller FO, Guskiewicz KM. Using theory to understand high school aged athletes’ intentions to report sport-related concussion: Implications for concussion education initiatives. Brain Inj. 2013;27(7–8):878–886. doi: 10.3109/02699052.2013.775508. [DOI] [PubMed] [Google Scholar]