Abstract
AIM: To investigate the efficacy and clinical outcome of patients treated with an over-the-scope-clip (OTSC) system for severe gastrointestinal hemorrhage, perforations and fistulas.
METHODS: From 02-2009 to 10-2012, 84 patients were treated with 101 OTSC clips. 41 patients (48.8%) presented with severe upper-gastrointestinal (GI) bleeding, 3 (3.6%) patients with lower-GI bleeding, 7 patients (8.3%) underwent perforation closure, 18 patients (21.4%) had prevention of secondary perforation, 12 patients (14.3%) had control of secondary bleeding after endoscopic mucosal resection or endoscopic submucosal dissection (ESD) and 3 patients (3.6%) had an intervention on a chronic fistula.
RESULTS: In 78/84 patients (92.8%), primary treatment with the OTSC was technically successful. Clinical primary success was achieved in 75/84 patients (89.28%). The overall mortality in the study patients was 11/84 (13.1%) and was seen in patients with life threatning upper GI hemorrhage. There was no mortality in any other treatment group. In detail OTSC application lead to a clinical success in 35/41 (85.36%) patients with upper GI bleeding and in 3/3 patients with lower GI bleeding. Technical success of perforation closure was 100% while clinical success was seen in 4/7 cases (57.14%) due to attendant circumstances unrelated to the OTSC. Technical and clinic success was achieved in 18/18 (100%) patients for the prevention of bleeding or perforation after endoscopic mucosal resection and ESD and in 3/3 cases of fistula closure. Two application-related complications were seen (2%).
CONCLUSION: This largest single center experience published so far confirms the value of the OTSC for GI emergencies and complications. Further clinical experience will help to identify optimal indications for its targeted and prophylactic use.
Keywords: Over-the-scope-clip, Endoscopic therapy, Gastrointestinal bleeding, Perforation, Fistula
Core tip: In this retrospective study a novel endoscopic over-the-scope-clip (OTSC) was evaluated for the treatment of severe gastrointestinal bleeding, perforation and fistula. 101 OTSCs were applied in 84 patients with a primary clinical success in 75/84 patients for all applications corresponding to 89%. Severe bleeding was successfully treated in 35/41 patients with upper gastrointestinal (GI) bleeding (85.36%) and in all 3 patients with severe lower GI bleeding. Technical success of perforation closure was 100% while clinical success was seen in 4/7 cases (57.14%) due to attendant circumstances unrelated to the OTSC. Technical and clinic success was achieved in 18/18 patients for the prevention of secondary perforation or bleeding after endoscopic mucosal resection and endoscopic submucosal dissection and in 3/3 fistula closures. Two application-related complications were seen. This largest single center experience published so far confirms the high value of the OTSC for the endoscopic treatment of GI emergencies and complications.
INTRODUCTION
The over-the-scope clip (OTSC; OVESCO Endoscopy AG, Tuebingen, Germany) is a new endoscopic device, which recently obtained technical approval not only in Europe but also in the US and other non-European countries. The clip consists of super-elastic Nitinol and has the shape of a bear trap mounted on a transparent plastic housing. Comparable to the application mechanism of current variceal band ligation devices, the clip is applied by turning a wheel that is attached onto the shaft of the endoscope. This applies traction on a thread that releases the clip from the distal cap resulting in approximation of tissue between the grasping teeth of the OTSC. Similar to a surgical anastomotic stapling device, the tissue is kept vital based on a pre-defined distance between the clip teeth promoting sufficient vascular perfusion. Basic experiments were performed in porcine models for natural orifice translumenal endoscopic surgery (NOTES) procedures, endoscopic full-thickness resection and defect closure after targeted perforation, as well as for bleeding in a simulator model[1-6].
The macroclip has been commercialized in Europe since 2008[7-9]. In the United States a 510K application (No. K093908) was obtained in December 2010 for clinical use in endoscopic marking, hemostasis and closure of gastrointestinal perforations (< 20 mm). However, published clinical data are limited thus far. In this current retrospective analysis of 84 patients, we aimed to provide clinical data on using the macroclip for GI emergencies such as severe GI bleeding, perforations and fistulas as well as for the prevention of bleeding and perforation after complex resective procedures. To our knowledge this is the largest single center experience on the OTSC use published so far.
MATERIALS AND METHODS
The OTSC is approved for clinical application for the indications used. Informed consent was obtained before all endoscopic interventions. A retrospective review of all patients who underwent OTSC placement between 02-2009 and 10-2012 at our institution was performed. Key data were collected prospectively and analyzed retrospectively on patient demographics, indications for the procedure, previously attempted therapies, technical and clinical success of the procedure as well as adverse events. Technical success was defined as number/percentage of OTSCs attempted and successfully deployed. Clinical success was defined based on the intended treatment, achieving hemostasis for GI bleeding cases, lack of contrast extravasation on fluoroscopic examination in the cases of perforation/fistula closures.
For applications in the upper gastrointestinal tract routinely a 12/6t OTSC was applied. In the lower GI tract routinely the 14/6t OTSC was used in the rectum and the 12/6t OTSC in the colon proximal to the rectum. All OTSC placements were performed by four advanced endoscopists. As a routine for clip placement, a double-channel gastroscope was used in case of acute bleeding events in the upper GI tract as well as in the colon if the lesion could be reached with the gastroscope (EG530D Fujifilm, Tokyo, Japan, see below). Otherwise, a standard colonoscope (EC590Z M-type; Fujifilm, Tokyo, Japan) was used. All cases were performed under midazolam/propofol sedation.
After identifying the lesion, the endoscope was withdrawn and the OTSC mounted on the distal end. The endoscope was re-inserted, and the lesion was centered within the cap of the OTSC followed by suctioning of the tissue into the cap. In the setting of GI perforations and insufficient suction to effectively aspirate tissue into the cap due to air leakage from the perforation site a traditional gasping forceps or the “Twin Grasper” system (OVESCO Corp., Tuebingen, Germany) was used to pull the defect into the cap. In the few fistula cases, we used a combination of suction and grasping the tissue with a standard grasper.
A double-channel endoscope proved especially useful in severe bleeding cases since suction capability was assured via the second channel. A Y-adapter was attached for intermediate forceful flushing through the instrumentation channel leaving the second channel open for suction. When the twin grasper was used it was inserted into the second channel to avoid preemptive firing of the OTSC due to friction between the instrument and the thread.
Follow-up exams were conducted only if considered useful by the endoscopist. Otherwise routine follow-up intervals depending on the individual clinical pathology and procedure were performed.
RESULTS
Descriptive statistics were used for absolute values, percentages, means or medians with ranges and standard deviation wherever appropriate.
From February 2009 until October 2012, 84 patients [median age, 71 years (range, 2-98 years), 34 women, 50 men, ASA 2-4] were treated with 101 OTSC clips (77 12/6t clips and 24 14/6t clips) (Table 1). Overall technical success was achieved in 78/84 (92.8%) patients. In 75/84 patients (89.28%), a primary successful clinical treatment could be achieved (Table 2). The mean number of OTSCs placed on the initial endoscopic exam was 1 (range, 1-3). Only 2/84 patients required a repeat endoscopic intervention with repeat clip placement. Depending on the individual situation, antibiotic prophylaxis was given in 58/84 cases (69%). The results according to the different indications are presented in the following subsections of the paper.
Table 1.
Overview on patient characteristics, indications and overall success rates
| Patients, n | 84 |
| Sex | 50 males |
| 34 females | |
| Age (yr), median | 71 (2-98) |
| Clip type | |
| 12/6T | 77 |
| 14/6T | 24 |
| OTSCs (n total) | 101 |
| Indication for OTSC placement | |
| Upper GI bleeding | 41 |
| Lower GI bleeding | 3 |
| Gastrointestinal perforation | 7 |
| Fistula | 3 |
| Bleeding prevention | 12 |
| Perforation prevention | 18 |
| Technical success | 78/84 (92.85%) |
| Clinical success | 75/84 (89.28%) |
GI: Gastrointestinal; OTSC: Over-the-scope-clip.
Table 2.
Indications and succes of over-the-scope-clip placement
| Indication | n | Technical success | Need for surgery | Death due to relapse | Death due to other cause |
| Perforation closure | |||||
| Incomplete perforation (laceration of mucosa/inner muscle layer) | |||||
| After mechanical stress at the level of the rectosigmoid | 3 | 3 | No | No | No |
| After balloon dilation of pyloric stenosis | 1 | 1 | Yes | No | No |
| Perforation | |||||
| After colonic EMR | 1 | 1 | Yes | No | No |
| Due to colonic methane gas explosion | 1 | 1 | Yes | No | No |
| Intraoperative during cholecystectomy; perforation of a large duodenal diverticulum | 1 | 1 | No | No | No |
| Prevention of secondary perforation after resective techniques | |||||
| EMR | |||||
| Esophageal EMR | 2 | 2 | No | No | No |
| Gastric EMR | 2 | 2 | No | No | No |
| Duodenal EMR | 2 | 2 | No | No | No |
| Cecal EMR | 2 | 2 | No | No | No |
| EMR ascending colon | 1 | 1 | No | No | No |
| Sigmoid EMR | 1 | 1 | No | No | No |
| ESD | |||||
| Esophageal ESD | 3 | 3 | No | No | No |
| Rectal ESD | 5 | 5 | No | No | No |
| Hemostasis severe bleeding | |||||
| Upper GI bleeding | |||||
| Acute ulcer bleeding | |||||
| Forrest Ia | 9 | 4 | 4 | 4 | 1 |
| Forrest Ib | 3 | 3 | No | No | No |
| Forrest IIa | 23 | 23 | No | No | 4 |
| Forrest IIb | 3 | 2 | 1 | 1 | 1 |
| Severe bleeding at GE junction after balloon dilation for achalasia | 1 | 1 | No | No | No |
| Gastric adenocarcinoma | 1 | 1 | 1 | No | No |
| Gastric lymphoma | 1 | 1 | No | No | No |
| Lower GI bleeding | |||||
| Severe bleeding from rectal ulcer | |||||
| Forrest Ia | 2 | 2 | No | No | No |
| Forrest IIb | 1 | 1 | No | No | No |
| Prevention of secondary bleeding after resective techniques | |||||
| EMR | |||||
| Gastric EMR | 1 | 1 | No | No | No |
| Duodenal EMR | 3 | 3 | No | No | No |
| Colorectal EMR | 3 | 3 | No | No | No |
| ESD | |||||
| Esophageal ESD | 1 | 1 | No | No | No |
| Rectal ESD | 4 | 4 | No | No | No |
| Fistula closure | |||||
| After PEG removal | 2 | 2 | No | No | No |
| After dilation of pseudocyst access, false tract | 1 | 1 | No | No | No |
EMR: Endoscopic mucosal resection; ESD: Endoscopic submucosal dissection; GI: Gastrointestinal.
Gastrointestinal bleeding
Forty-one patients were treated with active or recent massive upper gastrointestinal bleeding (hemoglobin < 7 g/dL at admission or prior to emergency endoscopy; Table 2). Of these 13/41 (31.7%) had failure of a previously attempted hemostasis method (standard through the scope hemoclips or adrenalin injection plus hemoclip) (Figure 1A-D). Technical success in this group was 35/41 (85.36%). A total of 43 clips were applied in this group with only two patients requiring multiple clip application.
Figure 1.
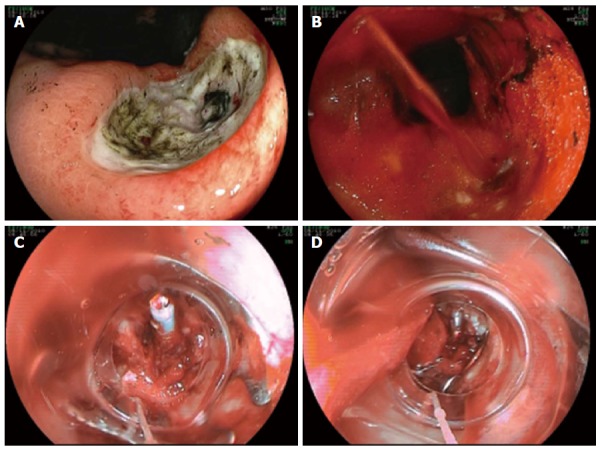
Ulcer (Forrest IIa) at the gastric angulus (A-D). Acute bleeding after attempt of closure of the visible vessel using a standard hemoclip. Successful hemostasis using a 12/6t over-the-scope-clip.
In 38 cases (92.7%), the acute bleeding was related to peptic ulcer disease, in 2 cases (4.9%) due to bleeding of malignant ulcers (one gastric adenocarcinoma, one gastric lymphoma) and in one patient (2.4%) due to deep muscle laceration and serious bleeding at the level of the GE junction after a 30 mm balloon dilatation for achalasia (Table 2). In the peptic ulcer disease group, 13 ulcers were located in the stomach (antrum n = 2, angulus n = 2, corpus n = 9), 8 in the pyloric channel or duodenal bulb and 17 in the 2nd or 3rd duodenum. Of the 41 upper GI bleeding patients, 31/41 (75.60%) were on pre-existing anticoagulation. 9/41 (21.95%) took warfarin, 17/41 (41.46%) aspirin, 4/41 (9.75%) heparin/enoxaparin and 1 (2.4%) was anti-coagulated with a combination of aspirin plus clopidogrel.
In the GI bleeding group, clinical success was achieved in 35/41 patients (85.36%). One patient treated had experienced massive re-bleeding from an ulcer on the posterior wall of the duodenal bulb after a prior attempt of hemostasis using conventional endoscopic hemostasis techniques (injection and hemoclip) and following surgical over-sewing of the gastroduodenal artery. An extensive re-bleeding after surgery was successfully stopped by OTSC application onto the ulcer ground (Figures 2A-D; Video 1). Unfortunately, the patient re-bled a third time already on solid food on post-operative day (POD) 10 after the first OTSC application. Due to a high operative risk based on advanced chronic obstructive pulmonary disease, repeat application of the OTSC again was successfully performed. The patient survived and was discharged on POD 7 after the second OTSC.
Figure 2.
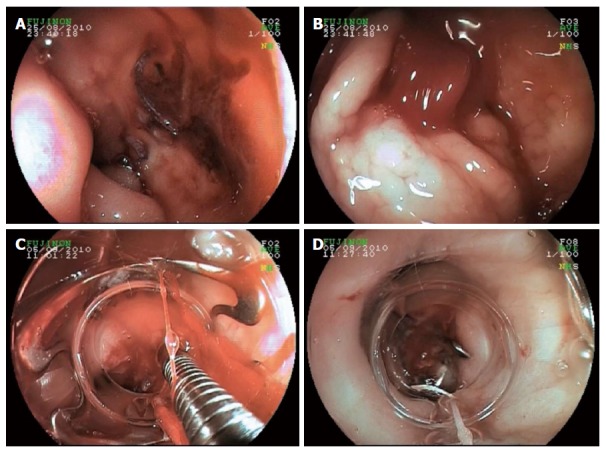
Severe recurrent ulcer bleeding from the gastroduodenal artery at the posterior wall of the duodenal bulb despite primary endoscopic clipping and surgical oversewing (A-D). Visible surgical threads at the ulcer base (A); Intermittent massive re-bleeding at rinsing and suction (B); Successful application of a 12/6t Over-the-Scope-Clip by pulling the ulcer bed into the transparent distal attachment cap (C, D).
Five patients (12.2%) underwent additional surgical treatment due to high-risk bleeding lesions or unsuccessful treatment. Of these patients, four had presented with a Forrest Ia bleeding lesion and one patient with a Forrest IIb lesion (Table 2). In four of five cases, the initial clip placement had been difficult due to a reduced visibility in a Forrest Ia bleeding situation. In one patient with a Forrest IIb lesion, clip placement was unsuccessful (Table 2).
In three patients, the GI bleeding originated from a lower source, at the rectum level (radiation proctitis with repetitively bleeding from a rectal ulcer n = 2, a rectal ulcer of unknown cause n = 1). Technical and clinical success in this group was 3/3 (100%) (Table 2).
Perforation closures
In regards to perforation closure, technical success was 7/7 (100%). A total of 9 OTSC clips were applied. Two patients needed two OTSCs placed side by side due to perforation size (Table 2).
Placement of the OTSC was clinically successful in 4/7 cases (57.14%) due to causes not related to the OTSC application. In one patient with an extremely rare case of colonic disruption due to a methane gas explosion during electrocautery use, a CT scan performed immediately post procedure revealed free fluid and gas in the abdominal cavity. The patient therefore underwent sigmoid resection and lavage of the peritoneal cavity the same day. The resected surgical specimen showed a successful closure of the two 1.5 cm wall defects. One patient had a perforation after endoscopic mucosal resection (EMR) of a 2 x 2 cm polyp at the hepatic flexure, which was successfully treated with two 14/6t OTSC clips (Figure 3A-I, Video 2). The patient showed clinical signs of perforation with a distended abdomen after placement of the second large OTSC (21 mm outer diameter of the device). However, the perforation site which was suspected at the level of a sigmoid diverticulosis could not be identified endoscopically. Abdominal imaging immediately post procedure revealed free fluid and gas in the abdominal cavity. The patient underwent sigmoid resection with confirmation of a diverticular perforation and had an uneventful course. No defect at the level of the hepatic flexure could be detected intraoperatively. Furthermore, a 2-year old patient was treated with a 12/6t OTSC clip after suspicion of an incomplete perforation due to a balloon dilatation of a pyloric stenosis. Due to unsecure closure at the level of the pylorus surgical removal of the clip and a pyloroplasty were performed.
Figure 3.
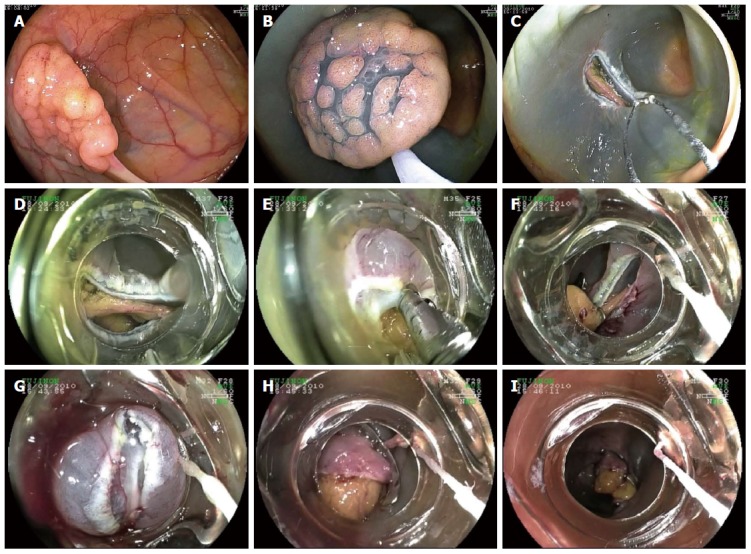
Acute perforation after endoscopic mucosal resection of a 2 cm tubulovillous adenoma at the right colonic flexure (A-I). Successful closure of the large defect using two large 14/6t over-the-scope-clips applied side-to-side.
Three patients were treated after endoscopic laceration of the mucosa ± superficial muscle layer (incomplete perforation with increased secondary perforation risk). One of the three lacerations occurred when passing the endoscope through a narrow descending colon with multiple diverticula. The other two appeared while pushing the endoscope probably too forcefully forward through the lower and mid sigmoid. Technical and clinical success were 100% with a 12/6t OTSC system placed in all three cases. No leakage of contrast medium was detected on fluoroscopic examination directly after the closure. One patient was treated with an OTSC clip after laparoscopic cholecystectomy with iatrogenic injury of a large duodenal diverticulum located close to the cystic stump.
Prevention of secondary perforation or bleeding
Eighteen patients underwent OTSC application to prevent secondary perforation (PSP) after incomplete wall damage during complex widespread endoscopic resection (10 EMR cases and 8 ESD cases; Table 2). Technical and clinical success in this group was 18/18 (100%). A total of 29 clips were applied and 7/18 (38.8%) patients had multiple OTSC applications at the same procedure. No leakage was found radiologically by filling the lumen with water-soluble contrast medium directly thereafter or at a control within 24 h. No secondary perforations occurred.
OTSC clip was applied in 12 cases (14.28%) for prevention of secondary bleeding (PSB) after widespread EMR or ESD with multiple blood vessels ≥ 2 mm at the wound ground (Table 2). Technical success in this group was 12/12 (100%), without any bleeding events after the OTSC treatment. In 10/12 patients (83.3%) primary OTSC application was performed, with successful definitive bleeding prevention in all cases. 2/12 (16.6%) patients were successfully treated by OTSC application after failure of standard hemoclips for secondary bleeding prevention after clip placement on vessels during ESD.
Fistula closure
A persistent entero-cutaneous fistula after percutaneous endoscopic gastrostomy removal was successfully closed in 2 patients by OTSC application. One patient with a false lumen that was created during re-dilatation of a gastrocystic tract for exchange of the two transgastric pancreatic pseudocyst drainages was treated successfully by OTSC application (Table 2). Technical success in this group was 3/3 (100%), with a total of 3 clips used. Clinical success was 100% with no patients needing a secondary intervention.
Mortality
Overall, a total of 11 patients (11/84, 13.09%) died in the study group with all of the patients being in the gastrointestinal bleeding group. The mortality rate due to bleeding and hemorrhagic shock in the Forrest Ia group was the highest with 4/41 (9.75%). One patient died despite endoscopic and subsequent surgical intervention due to hemorrhagic shock. In an 87-year patient and a 92-year old patient, surgery was refused by the surgeons and relatives, respectively. Both patients died due to re-bleeding from penetrating ulcers. Seven patients died from causes not related to re-bleeding: two due to respiratory insufficiency and multi-organ failure, three due to acute heart failure (two following a non-ST segment myocardial infarction and one a cardio-renal syndrome), one due to methicillin-resistant staphylococcus aureus sepsis and one patient due to cerebral bleeding.
Complications
As mentioned above one patient with successful primary OTSC closure of a large colonic perforation following EMR resection of a polyp at the hepatic flexure, a secondary perforation was detected in the relatively narrow sigmoid colon with multiple diverticula. It is presumed that the secondary perforation occurred when advancing the endoscope with the second of the two macroclips with 21 mm outer diameter. The patient underwent uneventful surgical resection of the sigmoid colon. During the surgery the perforation at the level of the right colonic flexure was inspected and noted to be successfully closed with two 14/6t OTSC clips and was preserved. The postoperative course of the patient was uneventful.
We observed one case of capture of a conventional grasper forceps within the teeth of the OTSC following its release. The clip had been placed in an attempt of perforation prevention, and was being placed in the distal esophagus because of suspected inner muscle layer resection following cap-EMR. The handle of the grasper was cut and the endoscope was removed. An attempt of focal APC coagulation was applied to try to open the OTSC but failed. Neither was successful the capture of the two horns on one side of the OTSC in a mechanical lithotripsy basket and metal spiral. A final attempt by removing the clip gently mechanically and being ready to close a perforation with another OTSC was finally successful. The tip of the endoscope had been prepared with a hard distal attachment cap as used for cap EMR (14.8 mm outer diameter, MAJ-291, Olympus Optical, Tokyo, Japan). The further course after clip removal was uneventful and a second OTSC not needed.
DISCUSSION
Gastrointestinal bleeding and perforations require immediate and careful endoscopic intervention to prevent hemodynamic compromise from exsanguination or complications from extra-luminal fluid accumulation with sepsis from inadequate perforation closure. Traditionally, GI bleeding has been managed endoscopically with electrocautery, epinephrine injection or hemoclip application. Often, multiple hemoclips may be necessary. Perforations in the upper and lower GI-tract have been generally managed by surgeons but appear to be amenable to endoscopic closure thus avoiding surgery in patients that often have significant comorbidities. The over-the-scope-clip has become an important tool in the armamentarium of the interventional endoscopist though introduced in the market only recently. However, experience from large patient series is still limited and most of the published literature is experimental or reports small case series[10-12]. Controlled porcine studies have shown successful defect closure in various NOTES procedures as well as in artificial duodenal and colonic perforations[2,5,13,14]. Initial clinical data on the successful treatment of eleven patients with severe gastric and colonic bleeding and perforations of the GI tract using the OTSC were reported by Kirschniak et al[7] in 2007. He recently reported the largest monocentric retrospective series on 50 patients treated for bleeding, perforations and fistulas using the OTSC[12]. Haito-Chavez et al[15] confirmed the data in a first North Italian series. To date, the largest published experience is an international, multicenter study on the use of the OTSC for GI fistulae, perforations and leaks in 188 patients.
In this large retrospective single center series, we were able to confirm observations from Repici et al[10] and from Manta et al[16] that the OTSC facilitates the treatment of life-threatening bleeding not amenable to standard hemostatic procedures and devices. Given that severe upper gastrointestinal bleeding is one of the most challenging emergencies in gastroenterology. The mortality rate still ranges between 3.5% and 14%[17-19]. Having effective tools to manage difficult bleeding cases is imperative and may change outcomes especially for high-risk patients. The data reported in our case series on patients presenting with severe non-variceal gastrointestinal bleeding (Forrest Ia, Ib, IIa and IIb; hemoglobin < 7g/dL) are encouraging. Nevertheless, the OTSC application system may have its limitations in emergency bleeding situations. After identifying the bleeding source, the scope has to be removed in order to mount the device on the endoscope, comparable to a variceal band ligator. However, mounting the system on the endoscope is fast and easy and the skills are acquired after a short learning period[20].
In 2006, Schurr et al[1,21] published data about the closure of iatrogenic colon perforations with the OTSC in an experimental survival animal study in pigs. The authors concluded that the OTSC system is a simple and secure closure method for iatrogenic colon perforations, and may be considered as an alternative to surgical repair. Weiland et al[22] evaluated success rates of the OTSC in closure of iatrogenic gastrointestinal perforations and anastomotic leaks in a systematic literature review in 2013. In their analysis a total of 17 clinical case series and 22 preclinical research articles were evaluated. They found a high mean rate of 80%-100% on procedural success and durable closure in 57%-100%. Our clinical data confirm these results for perforation closure. One limitation, however, was that our overall case number of perforations was small. A reproducible closure of transmural GI defects appears to be possible with the OTSC in an experimental setting[23]. However, Matthes et al[20] showed in their porcine model that only tissue defects from 5 to 20 mm in the stomach and 10 to 25 mm in the colon could be closed reliably using one OTSC. For larger defects 2 clips were recommended.
Previously published data on the OTSC have shown that indications for the use of the OTSC are not limited to iatrogenic GI perforations and bleedings. Also fistulas and secondary leaks could be successfully closed using the OTSC system if an effective external drainage is guaranteed[24-28]. Baron et al[29] recently published their experience in a retrospective US multicenter study on OTSC placement. 31 of 45 patients included had anastomotic leaks or fistulae. Of these, clinical success with permanent closure was achieved in 20/31 cases (65%). Haito-Chavez et al[15] showed a similar long-term success in 60.2% of patients with a median follow-up of 146 d. Further clinical trials are needed to clarify optimal indications and limitations of the system.
There are no evidence-based recommendations concerning re-nutrition after successful application of conventional clips or OTSCs, e.g., after severe GI bleeding. We experienced a case of heavy re-bleeding 10 d after successful hemostasis with severe bleeding from the gastroduodenal artery. The patient had eaten solid food at that time including meat. Until further clinical experience is gained, we empirically recommend for our patients with heavy bleeding and OTSC application a liquid diet on the first 3 post-interventional days and a soft diet for at least 14 d after the intervention to reduce the risk of a premature OTSC loss.
Prospective randomized trials of emergency situations are difficult to conduct and therefore data is limited. Our experience indicates that the OTSC may represent a helpful tool for the prevention of secondary necrosis and perforation after widespread endoscopic resections. However, results of prospective trials are currently lacking.
A very rare complication using the OTSC system may be the capture of a grasping instrument within the teeth of the clip as happened in one case in our series. This potentially severe complication can effectively be avoided by sufficient retraction of the instrument into the distal cap before releasing the clip as recommended by the company. Even if in most cases the OTSC is simply applied by suction this should not be forgot, especially in emergency situations. Misplacement of the clip can potentially necessitate clip removal. Until now, only few cases of OTSC removal have been published so far. Fähndrich et al[30] were the first to demonstrate successful opening of the clip in three patients using a Nd:YAG-Laser. One limitation of the Nd:YAG laser aside potential tissue damage in case of misapplication is its lack of availability in every endoscopy unit. Neumann et al[31] showed in an “ex vivo” porcine model a guidewire removal technique in 8 of 15 cases with a low removal success rate of 53.3%. On the one side a removal of the OTSC seems feasible with these different techniques, on the other hand they all have limitations and in our opinion there is a need of a secure and easy removal system. Schmidt et al[32] reported on a prototype of a “Clip Cutter” device (DC ClipCutter, Ovesco Endoscopy). Similar to spark gap formation in a car engine by electrical discharge the clip is opened by holding it between a fork-like device. Until now, there is a lack of data concerning what happens with the OTSC and the application site over time. The OTSC itself is composed from nitinol and suited as permanent implant. While some OTSC seems to fall off spontaneously others seem to be overgrown by hyperplastic tissue. Systematic studies in different anatomical locations are needed in order to give recommendations for a systematic secondary control or removal.
In conclusion, our study confirms the usefulness of the OTSC for the treatment of severe gastrointestinal bleeding, fistula closure and the non-surgical management of perforations. Further studies for its systematic use in high-risk bleeding patients or as a prophylactic measure to avoid secondary perforation or bleeding in multimorbid patients are eagerly awaited.
COMMENTS
Background
The over-the-scope clip (OTSC) is a new endoscopic device, which recently obtained technical approval not only in Europe but also in the US and other non-European countries. The OTSC has become an important tool in the armamentarium of the interventional endoscopist though introduced in the market only recently. However, experience from large patient series is still limited and most of the published literature is experimental or reports small case series.
Innovations and breakthroughs
In this current retrospective analysis of 84 patients, the authors aimed to provide clinical data on using the macroclip for gastrointestinal (GI) emergencies such as severe GI bleeding, perforations and fistulas as well as for the prevention of bleeding and perforation after complex resective procedures. To the best of current knowledge, this is the largest single center experience on the OTSC use published so far.
Applications
This largest single center experience published so far confirms the high value of the OTSC for the endoscopic treatment of GI emergencies and complications.
Peer-review
Good series of OTSC usage in a wide range of clinical indications. The endoscopic pictures are useful but will benefit from labelling of the pictures to identify, parts of the photo that may not be so clear to general readers not familiar with the OTSC system.
Footnotes
Supported by The “Endo-Verein Erlangen”, a registered non-profit training organization, Baiersdorf, Germany.
Institutional review board statement: The study was reviewed and approved by the Institutional Review Board and the Ethics Committee of St. Bernward Academic Teaching Hospital Hildesheim, Germany.
Informed consent statement: All involved persons, subjects or legally authorized representative gave their informed consent (written or verbal) prior to study enrollment and treatment. Identity of all subjects including all details were anonymized.
Conflict-of-interest statement: All authors declare that there is no conflict of interest with the paper presented.
Data sharing statement: Informed consent for data sharing was not obtained but the presented data are anonymized and the risk of identification is low. No additional data are available. Questions regarding the technical appendix, statistical code and data set are available from the corresponding author at juehochber@mac.com.
Open-Access: This article is an open-access article which was selected by an in-house editor and fully peer-reviewed by external reviewers. It is distributed in accordance with the Creative Commons Attribution Non Commercial (CC BY-NC 4.0) license, which permits others to distribute, remix, adapt, build upon this work non-commercially, and license their derivative works on different terms, provided the original work is properly cited and the use is non-commercial. See: http://creativecommons.org/licenses/by-nc/4.0/
Peer-review started: May 7, 2015
First decision: June 23, 2015
Article in press: December 1, 2015
P- Reviewer: Ooi LLPJ S- Editor: Yu J L- Editor: A E- Editor: Zhang DN
References
- 1.Schurr MO, Hartmann C, Ho CN, Fleisch C, Kirschniak A. An over-the-scope clip (OTSC) system for closure of iatrogenic colon perforations: results of an experimental survival study in pigs. Endoscopy. 2008;40:584–588. doi: 10.1055/s-2008-1077354. [DOI] [PubMed] [Google Scholar]
- 2.von Renteln D, Schmidt A, Vassiliou MC, Gieselmann M, Caca K. Natural orifice transluminal endoscopic surgery gastrotomy closure with an over-the-endoscope clip: a randomized, controlled porcine study (with videos) Gastrointest Endosc. 2009;70:732–739. doi: 10.1016/j.gie.2009.03.010. [DOI] [PubMed] [Google Scholar]
- 3.von Renteln D, Schmidt A, Vassiliou MC, Rudolph HU, Caca K. Endoscopic full-thickness resection and defect closure in the colon. Gastrointest Endosc. 2010;71:1267–1273. doi: 10.1016/j.gie.2009.12.056. [DOI] [PubMed] [Google Scholar]
- 4.Voermans RP, van Berge Henegouwen MI, Bemelman WA, Fockens P. Hybrid NOTES transgastric cholecystectomy with reliable gastric closure: an animal survival study. Surg Endosc. 2011;25:728–736. doi: 10.1007/s00464-010-1242-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Arezzo A, Kratt T, Schurr MO, Morino M. Laparoscopic-assisted transgastric cholecystectomy and secure endoscopic closure of the transgastric defect in a survival porcine model. Endoscopy. 2009;41:767–772. doi: 10.1055/s-0029-1215025. [DOI] [PubMed] [Google Scholar]
- 6.Naegel A, Bolz J, Zopf Y, Matthes K, Mueller B, Kraus F, Neurath MF, Maiss J. Hemodynamic efficacy of the over-the-scope clip in an established porcine cadaveric model for spurting bleeding. Gastrointest Endosc. 2012;75:152–159. doi: 10.1016/j.gie.2011.08.009. [DOI] [PubMed] [Google Scholar]
- 7.Kirschniak A, Kratt T, Stüker D, Braun A, Schurr MO, Königsrainer A. A new endoscopic over-the-scope clip system for treatment of lesions and bleeding in the GI tract: first clinical experiences. Gastrointest Endosc. 2007;66:162–167. doi: 10.1016/j.gie.2007.01.034. [DOI] [PubMed] [Google Scholar]
- 8.Seebach L, Bauerfeind P, Gubler C. “Sparing the surgeon”: clinical experience with over-the-scope clips for gastrointestinal perforation. Endoscopy. 2010;42:1108–1111. doi: 10.1055/s-0030-1255924. [DOI] [PubMed] [Google Scholar]
- 9.Parodi A, Repici A, Pedroni A, Blanchi S, Conio M. Endoscopic management of GI perforations with a new over-the-scope clip device (with videos) Gastrointest Endosc. 2010;72:881–886. doi: 10.1016/j.gie.2010.04.006. [DOI] [PubMed] [Google Scholar]
- 10.Repici A, Arezzo A, De Caro G, Morino M, Pagano N, Rando G, Romeo F, Del Conte G, Danese S, Malesci A. Clinical experience with a new endoscopic over-the-scope clip system for use in the GI tract. Dig Liver Dis. 2009;41:406–410. doi: 10.1016/j.dld.2008.09.002. [DOI] [PubMed] [Google Scholar]
- 11.Albert JG, Friedrich-Rust M, Woeste G, Strey C, Bechstein WO, Zeuzem S, Sarrazin C. Benefit of a clipping device in use in intestinal bleeding and intestinal leakage. Gastrointest Endosc. 2011;74:389–397. doi: 10.1016/j.gie.2011.03.1128. [DOI] [PubMed] [Google Scholar]
- 12.Kirschniak A, Subotova N, Zieker D, Königsrainer A, Kratt T. The Over-The-Scope Clip (OTSC) for the treatment of gastrointestinal bleeding, perforations, and fistulas. Surg Endosc. 2011;25:2901–2905. doi: 10.1007/s00464-011-1640-2. [DOI] [PubMed] [Google Scholar]
- 13.Voermans RP, van Berge Henegouwen MI, Bemelman WA, Fockens P. Novel over-the-scope-clip system for gastrotomy closure in natural orifice transluminal endoscopic surgery (NOTES): an ex vivo comparison study. Endoscopy. 2009;41:1052–1055. doi: 10.1055/s-0029-1215231. [DOI] [PubMed] [Google Scholar]
- 14.Kratt T, Küper M, Traub F, Ho CN, Schurr MO, Königsrainer A, Granderath FA, Kirschniak A. Feasibility study for secure closure of natural orifice transluminal endoscopic surgery gastrotomies by using over-the-scope clips. Gastrointest Endosc. 2008;68:993–996. doi: 10.1016/j.gie.2008.06.057. [DOI] [PubMed] [Google Scholar]
- 15.Haito-Chavez Y, Law JK, Kratt T, Arezzo A, Verra M, Morino M, Sharaiha RZ, Poley JW, Kahaleh M, Thompson CC, et al. International multicenter experience with an over-the-scope clipping device for endoscopic management of GI defects (with video) Gastrointest Endosc. 2014;80:610–622. doi: 10.1016/j.gie.2014.03.049. [DOI] [PubMed] [Google Scholar]
- 16.Manta R, Galloro G, Mangiavillano B, Conigliaro R, Pasquale L, Arezzo A, Masci E, Bassotti G, Frazzoni M. Over-the-scope clip (OTSC) represents an effective endoscopic treatment for acute GI bleeding after failure of conventional techniques. Surg Endosc. 2013;27:3162–3164. doi: 10.1007/s00464-013-2871-1. [DOI] [PubMed] [Google Scholar]
- 17.Cooper GS, Chak A, Harper DL, Pine M, Rosenthal GE. Care of patients with upper gastrointestinal hemorrhage in academic medical centers: a community-based comparison. Gastroenterology. 1996;111:385–390. doi: 10.1053/gast.1996.v111.pm8690203. [DOI] [PubMed] [Google Scholar]
- 18.Rockall TA, Logan RF, Devlin HB, Northfield TC. Risk assessment after acute upper gastrointestinal haemorrhage. Gut. 1996;38:316–321. doi: 10.1136/gut.38.3.316. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Rollhauser C, Fleischer DE. Nonvariceal upper gastrointestinal bleeding. Endoscopy. 2002;34:111–118. doi: 10.1055/s-2002-19853. [DOI] [PubMed] [Google Scholar]
- 20.Matthes K, Cohen J, Kochman ML, Cerulli MA, Vora KC, Hochberger J. Efficacy and costs of a one-day hands-on EASIE endoscopy simulator train-the-trainer workshop. Gastrointest Endosc. 2005;62:921–927. doi: 10.1016/j.gie.2005.09.018. [DOI] [PubMed] [Google Scholar]
- 21.Schurr MO, Hartmann C, Kirschniak A, Ho CN, Fleisch C, Buess G. [Experimental study on a new method for colonoscopic closure of large-bowel perforations with the OTSC clip] Biomed Tech (Berl) 2008;53:45–51. doi: 10.1515/bmt.2008.011. [DOI] [PubMed] [Google Scholar]
- 22.Weiland T, Fehlker M, Gottwald T, Schurr MO. Performance of the OTSC System in the endoscopic closure of iatrogenic gastrointestinal perforations: a systematic review. Surg Endosc. 2013;27:2258–2274. doi: 10.1007/s00464-012-2754-x. [DOI] [PubMed] [Google Scholar]
- 23.Matthes K, Jung Y, Kato M, Gromski MA, Chuttani R. Efficacy of full-thickness GI perforation closure with a novel over-the-scope clip application device: an animal study. Gastrointest Endosc. 2011;74:1369–1375. doi: 10.1016/j.gie.2011.07.057. [DOI] [PubMed] [Google Scholar]
- 24.Pohl J, Borgulya M, Lorenz D, Ell C. Endoscopic closure of postoperative esophageal leaks with a novel over-the-scope clip system. Endoscopy. 2010;42:757–759. doi: 10.1055/s-0030-1255634. [DOI] [PubMed] [Google Scholar]
- 25.Conio M, Blanchi S, Repici A, Bastardini R, Marinari GM. Use of an over-the-scope clip for endoscopic sealing of a gastric fistula after sleeve gastrectomy. Endoscopy. 2010;42 Suppl 2:E71–E72. doi: 10.1055/s-0029-1215199. [DOI] [PubMed] [Google Scholar]
- 26.Mangiavillano B, Pisani A, Viaggi P, Arena M, Opocher E, Mangano M, Santoro T, Masci E. Endoscopic sealing of a rectovesical fistula with a combination of an over the scope clip and cyano-acrylate injection. J Gastrointest Oncol. 2010;1:122–124. doi: 10.3978/j.issn.2078-6891.2010.020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Sandmann M, Heike M, Faehndrich M. Application of the OTSC system for the closure of fistulas, anastomosal leakages and perforations within the gastrointestinal tract. Z Gastroenterol. 2011;49:981–985. doi: 10.1055/s-0029-1245972. [DOI] [PubMed] [Google Scholar]
- 28.Arezzo A, Verra M, Reddavid R, Cravero F, Bonino MA, Morino M. Efficacy of the over-the-scope clip (OTSC) for treatment of colorectal postsurgical leaks and fistulas. Surg Endosc. 2012;26:3330–3333. doi: 10.1007/s00464-012-2340-2. [DOI] [PubMed] [Google Scholar]
- 29.Baron TH, Song LM, Ross A, Tokar JL, Irani S, Kozarek RA. Use of an over-the-scope clipping device: multicenter retrospective results of the first U.S. experience (with videos) Gastrointest Endosc. 2012;76:202–208. doi: 10.1016/j.gie.2012.03.250. [DOI] [PubMed] [Google Scholar]
- 30.Fähndrich M, Sandmann M, Heike M. Removal of over the scope clips (OTSC) with an Nd: YAG Laser. Z Gastroenterol. 2011;49:579–583. doi: 10.1055/s-0029-1245871. [DOI] [PubMed] [Google Scholar]
- 31.Neumann H, Diebel H, Mönkemüller K, Nägel A, Wildner D, Vieth M, Siebler J, Neurath MF. Description of a new, endoscopic technique to remove the over-the-scope-clip in an ex vivo porcine model (with video) Gastrointest Endosc. 2012;76:1009–1013. doi: 10.1016/j.gie.2012.07.036. [DOI] [PubMed] [Google Scholar]
- 32.Schmidt A, Riecken B, Damm M, Cahyadi O, Bauder M, Caca K. Endoscopic removal of over-the-scope clips using a novel cutting device: a retrospective case series. Endoscopy. 2014;46:762–766. doi: 10.1055/s-0034-1365493. [DOI] [PubMed] [Google Scholar]


