Abstract
AIM: To assess the prevalence of nutritional disorders in children with inflammatory bowel disease (IBD) in Saudi Arabia.
METHODS: The data from a national cohort of children newly diagnosed with IBD between 2003 and 2012 were analyzed. The diagnosis of IBD and the differentiation between Crohn’s disease (CD) and ulcerative colitis (UC) were confirmed by gastroenterologists according to the standard criteria. The body mass index (BMI) of each child [weight (kg)/height2 (m)] was calculated at the time of diagnosis. The World Health Organization standards and references were used and the BMI for age > +1 and < -2 standard deviation score were used to define overweight and thinness, respectively. Age stratification analysis was performed to investigate any age-related variation in the prevalence of nutritional status between children < 10 years of age and older.
RESULTS: There were 374 children from 0.33 to 17 years of age, including 119 (32%) children with UC and 255 (68%) with CD. All of the children were Saudi nationals, and 68 (57%) of the UC and 150 (59%) of the CD children were males. A positive history of anorexia at the time of diagnosis was found in 30 (25%) patients with UC and 99 (39%) patients with CD. The prevalence of thinness was 31%, 35% and 24% in children with IBD, CD and UC, respectively, with a significantly higher prevalence of thinness in children with CD than in children with UC (P = 0.037) only in the age group of 10-17 years (P = 0.030). The prevalence of overweight was 16 %, 15% and 20 % in the children with IBD, CD and UC, respectively, indicating a higher prevalence in UC that was statistically significant only in the age group of 10-17 years (P = 0.020).
CONCLUSION: A high proportion of children with IBD presented with overweight instead of the classical underweight. Awareness of this finding is important for patient care.
Keywords: Overweight, Thinness, Ulcerative colitis, Crohn disease, Children, Saudi Arabia
Core tip: This study is the first from a developing country to demonstrate that a high proportion of children with inflammatory bowel disease (IBD) presented with overweight instead of the classical underweight. Age stratification revealed a significant variation between Crohn’s disease and ulcerative colitis in the prevalence of thinness as well as overweight between children < 10 years of age and older children. Physicians caring for children should be aware that children with IBD may present with overweight instead of the classical underweight.
INTRODUCTION
Nutritional impairment in the form of poor weight gain, weight loss and underweight (thinness) is one of the most important features of inflammatory bowel disease (IBD), occurring more commonly in children with Crohn’s disease (CD) than in children with ulcerative colitis (UC)[1,2]. However, recent reports in the Western literature have indicated an increasing proportion of adults and children presenting with overweight and obesity rather than underweight[3].
In developing countries, IBD is a new condition in both adults and children[4-6]. A recent study from Saudi Arabia reported a low incidence compared to the findings in the Western literature, although there was a statistically significant increase in trend over time[7]. It has been suggested that studying the characteristics of this emerging condition in new populations may enhance the understanding of these diseases. The lack of information on the nutritional status of children affected with IBD from developing countries in general and Saudi Arabia in particular prompted this study, with the objective to describe the nutritional status in Saudi children with newly diagnosed IBD.
MATERIALS AND METHODS
The data from a national cohort of children newly diagnosed with IBD between 2003 and 2012 were analyzed. The diagnosis of IBD and the differentiation between CD and UC were confirmed by gastroenterologists according to the revised Porto criteria[8]. The World Health Organization (WHO) standards and reference were used[9,10]. Accordingly, overweight and thinness were defined by body mass index (BMI) for age > +1 and < -2 standard deviation, respectively. Weight and length/height were measured at the time of diagnosis and BMI [weight (kg)/height2 (m)] was calculated for each patient and plotted on the relevant WHO charts. Age stratification analysis was performed to investigate any age-related variation in the prevalence of nutritional status between children < 10 years of age and older, in accordance with Paris classification[11]. χ2 test was used to test the significance of estimates, and P-value of < 0.05 was considered to be statistically significant.
This report constitutes a portion of the national study of the characteristics of IBD in Saudi children. The study was approved by the Institutional Review Board, College of Medicine, King Saud University (No. 10/2647/IRB).
RESULTS
There were 375 children from 0.33 to 17 years of age, including 119 (31.7%) patients with UC, 255 (68%) patients with CD and one (0.3%) patient with IBD-undetermined. The latter, however, was not included in the analysis. All of the children were Saudi nationals, and 68 (57%) of the UC and 150 (59%) of the CD children were male. A positive history of anorexia at the time of diagnosis was noted in 30 (25%) patients with UC and 99 (39%) patients with CD. A history of weight loss at the time of the diagnosis was positive in 42% of the patients with UC and 78% of the patients with CD. The distribution of nutritional status in the 374 children is shown in Table 1, indicating a prevalence of thinness of 31%, 35%, and 24% in IBD, CD, and UC children, respectively, with a significantly higher prevalence of thinness in CD children than UC children (P = 0.037). In contrast, the prevalence of overweight was 16%, 15% and 20 % in the children with IBD, CD and UC, respectively, with no statistically significant difference between the children with UC and CD (P = 0.219).
Table 1.
Nutritional status distribution n (%)
| WHO definitions | UC = 119 (32) | CD = 255 (68) | IBD = 374 (100) |
| Thinness (< -2 SD) | 28 (24)a | 89 (35)a | 117 (31) |
| Normal | 67 (56) | 129 (50) | 196 (53) |
| Overweight (> +1 SD) | 24 (20)b | 37 (15)b | 61 (16) |
P = 0.037,
P = 0.219. WHO: World Health Organization; UC: Ulcerative colitis; CD: Crohn’s disease; IBD: Inflammatory bowel disease.
The age-specific prevalence of thinness is shown in Table 2, indicating a significantly higher prevalence in CD patients 10-17 years of age (P = 0.030) compared with those < 10 years, whereas no significant age-related difference was noted in the UC or IBD group. The age-specific prevalence of overweight is depicted in Table 3. In UC patients, although not statistically significant, the prevalence of overweight was higher in the 10-17 year age group than in those < 10 years of age (P = 0.064). However, there was a significantly higher prevalence of overweight in the 10- to 17-year-old patients with UC than in those with CD (P = 0.020), whereas no significant age-related difference was noted in patients with CD or IBD. An overview of the age distribution of BMI in children with overweight is presented in Figure 1, indicating no clear pattern of distribution. Finally, there was no significant difference between males and females in the prevalence of overweight or thinness in the patients with UC, CD or IBD (P > 0.05).
Table 2.
Age-specific prevalence of thinness n (%)
| Age (yr) | UC | CD | P value | IBD |
| < 10 | 18/67a (26.9) | 19/55 (34.5) | 0.359 | 37/122b (30.3) |
| 10-17 | 10/52a (19.2) | 70/200 (35) | 0.030 | 80/252b (32) |
| 0.33-17 | 28/119 (24) | 89/255 (35) | 0.037 | 107/374 (31) |
P = 0.450;
P = 0.874. UC: Ulcerative colitis; CD: Crohn’s disease; IBD: Inflammatory bowel disease.
Table 3.
Age-specific prevalence of overweight n (%)
| Age (yr) | UC | CD | P value | IBD |
| < 10 | 9/67a (9) | 9/55b (16) | 0.843 | 18/122c (15) |
| 10-17 | 15/52a (29) | 28/200b (14) | 0.020 | 43/252c (17) |
| 0.33-17 | 24/119 (20) | 37/255 (15) | 0.219 | 61/374 (16) |
P = 0.065;
P = 0.822;
P = 0.676. UC: Ulcerative colitis; CD: Crohn disease; IBD: Inflammatory bowel disease.
Figure 1.
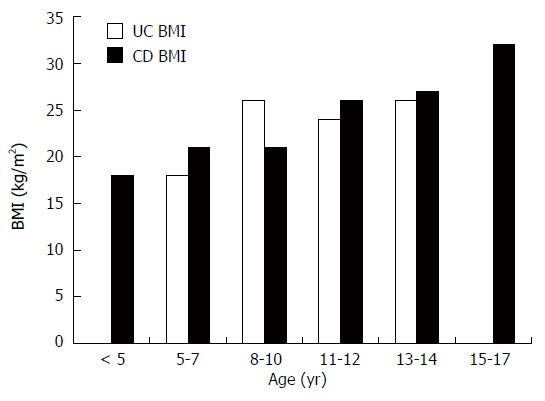
Body mass index distribution of children with overweight by age at diagnosis for ulcerative colitis and crohn disease. UC: Ulcerative colitis; CD: Crohn’s disease; BMI: Body mass index.
DISCUSSION
Nutritional impairment in children with IBD is one of the most important features of these diseases, and the assessment of nutritional status is essential for treating these children. Although the causes of thinness are not completely understood, contributing factors include anorexia, inadequate caloric intake, malabsorption, loss of nutrients, chronic inflammation, and including effect of proinflammatory cytokines[12]. In addition to the well-known weight loss in patients presenting with IBD, overweight and obesity have been recently reported at the time of diagnosis in an increasing number of children[13,14].
The data reported in this study are derived from a multicenter national sample of Saudi children with an estimate of 80% coverage and are therefore representative of the Saudi population of children ranging in age from 0.33 to 17 years with a confirmed diagnosis of IBD. In this analysis, we used BMI to define overweight and thinness in accordance with current recommendations[15,16]. In this report, assessment at diagnosis excluded any effect of therapy, allowing for a more accurate definition of the impact of IBD on nutritional status. The WHO definitions and references were used because of unavailability of local data on z scores at the time of this analysis, and the intention was to facilitate comparison with studies in other populations.
In this study, the 78% prevalence of weight loss in patients with CD and 42% in patients with UC at the time of diagnosis are within the range (40% to 90% in CD patients and 20%-55% in UC patients) reported in the Western literature[17], indicating a more important impact of CD than UC on nutritional status. Additionally, the 35% prevalence of thinness in patients with CD is comparable with the 32% in a report from France[18]. The high prevalence of thinness of 31 %, 35% and 24 % in patients with IBD, CD and UC contrasts with the lower prevalence rates reported from the United States[3]. However, the significantly more common prevalence of thinness in patients with CD than in patients with UC is similar to the reports in the literature likely reflecting the effects of more extensive disease in the patients with CD than in the patients with UC[3]. The discrepancy between the high prevalence of history of weight loss and thinness indicates that a significant proportion of patients lost weight from higher SD scores but still above the -2 SD score and is therefore not included in the prevalence of thinness as defined by the level of BMI < -2 SD.
Overweight and obesity in IBD have been increasingly reported in children and adults at the time of diagnosis of IBD. Studies from the United States reported a prevalence of overweight in 23.6%, 20% and 31% in children with IBD, CD, and UC, respectively[3,19], which is similar to the increased rate of overweight in the general pediatric population in the United States[20,21]. This report from Saudi Arabia revealed a prevalence of BMI > +1 SD of 16%, 15% and 20% in children with IBD, CD and UC, respectively, an unexpected finding in a developing country in general but an expected finding in developing countries such as Saudi Arabia, considered to be “in transition”, where the improved economic status led to a change toward more sedentary activity and a Western dietary lifestyle. This high rate of overweight in IBD and particularly UC children is consistent with the estimated prevalence of overweight (21%) in the general pediatric population of the Saudi Arabia[22]. We are unaware of reports on the prevalence of overweight in IBD children from other developing countries for comparison.
The age-specific analysis of nutritional status in this report revealed that the significantly higher prevalence of thinness in children with CD (P = 0.037) occurred only in the 10- to 17-year age group (P = 0.030), not in those < 10 years of age (P = 0.359), suggesting more severe and widespread CD in older children coupled with poor diet. Similarly, the age-specific prevalence of overweight in IBD in this study revealed a significantly higher prevalence in children with UC than in children with CD ranging in age between 10 and 17 years, not in children < 10 years of age. Although the explanation for this finding is not clear, we speculate that different dietary lifestyle of older children with easier access to high fat containing food might be a contributing factor. These age-related findings, not reported in the literature, indicated the importance of age stratification in the description of nutritional status and added to the particularities of IBD in children < 10 years old, as described in the Paris classification.
In conclusion, in this study from a developing country, the finding of a high prevalence of thinness is expected and was similar to findings in the Western literature. However, the high prevalence of overweight, especially in older children with UC, was an unexpected presenting feature of IBD in a developing country but consistent with the findings in the Western literature. Accordingly, physicians caring for children should be aware that overweight, rather than thinness, is not an uncommon nutritional presentation of IBD. Prospective studies are warranted to define the impact of overweight and obesity on the natural history and management of IBD in children.
COMMENTS
Background
Nutritional impairment in the form of poor weight gain, weight loss and underweight (thinness) is one of the most important features of inflammatory bowel disease (IBD), occurring more commonly in children with Crohn’s disease (CD) than ulcerative colitis (UC). However most of the data are from Western populations. Because of the increasing reports of IBD from developing countries, data on nutritional status are needed.
Research frontiers
Nutrition and growth assessment of children with IBD is important in patient care. The pattern and prevalence of nutritional impairment in children from developing countries are not known. This study reports on the increasingly high prevalence of overweight rather than the classical underweight to increase the awareness of this clinical nutritional presentation of IBD.
Innovations and breakthroughs
This is the first report on the prevalence of nutritional presentation of IBD in children in developing countries. The high prevalence of overweight in IBD is rarely reported worldwide. In addition, the finding of significant variation between CD and UC in prevalence of thinness as well as overweight between children < 10 years of age and older children indicates the importance of age stratification.
Applications
The most important application is to make the physicians caring for children that a high proportion may present with overweight and not underweight.
Peer-review
The authors report on the pattern and prevalence of nutritional impairment in children with inflammatory bowel disease at the time of diagnosis and before any treatment, reflecting the impact of inflammation on nutritional status. The identification of increasing prevalence of overweight is important for patient care. Further studies from developing countries are needed to confirm these finding and to study nutritional issues in more details.
Footnotes
Supported by The Deanship of Scientific Research at King Saud University through Research Group, No. RG-1436-007.
Institutional review board statement: This report constitutes a portion of the national study of the characteristics of IBD in Saudi children, approved by the Institutional Review Board, College of Medicine, King Saud University (No. 10/2647/IRB).
Conflict-of-interest statement: The authors declare no conflicts of interest.
Data sharing statement: No additional data are available.
Open-Access: This article is an open-access article which was selected by an in-house editor and fully peer-reviewed by external reviewers. It is distributed in accordance with the Creative Commons Attribution Non Commercial (CC BY-NC 4.0) license, which permits others to distribute, remix, adapt, build upon this work non-commercially, and license their derivative works on different terms, provided the original work is properly cited and the use is non-commercial. See: http://creativecommons.org/licenses/by-nc/4.0/
Peer-review started: June 27, 2015
First decision: August 26, 2015
Article in press: November 13, 2015
P- Reviewer: Mendall MA S- Editor: Gong ZM L- Editor: A E- Editor: Zhang DN
References
- 1.Thangarajah D, Hyde MJ, Konteti VK, Santhakumaran S, Frost G, Fell JM. Systematic review: Body composition in children with inflammatory bowel disease. Aliment Pharmacol Ther. 2015;42:142–157. doi: 10.1111/apt.13218. [DOI] [PubMed] [Google Scholar]
- 2.Hill RJ. Update on nutritional status, body composition and growth in paediatric inflammatory bowel disease. World J Gastroenterol. 2014;20:3191–3197. doi: 10.3748/wjg.v20.i12.3191. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Kugathasan S, Nebel J, Skelton JA, Markowitz J, Keljo D, Rosh J, LeLeiko N, Mack D, Griffiths A, Bousvaros A, et al. Body mass index in children with newly diagnosed inflammatory bowel disease: observations from two multicenter North American inception cohorts. J Pediatr. 2007;151:523–527. doi: 10.1016/j.jpeds.2007.04.004. [DOI] [PubMed] [Google Scholar]
- 4.Al-Qabandi WA, Buhamrah EK, Hamadi KA, Al-Osaimi SA, Al-Ruwayeh AA, Madda J. Inflammatory bowel disease in children, an evolving problem in Kuwait. Saudi J Gastroenterol. 2011;17:323–327. doi: 10.4103/1319-3767.84487. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Ahmaida A, Al-Shaikhi S. Childhood Inflammatory Bowel Disease in Libya: Epidemiological and Clinical features. Libyan J Med. 2009;4:70–74. doi: 10.4176/081210. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Wang XQ, Zhang Y, Xu CD, Jiang LR, Huang Y, Du HM, Wang XJ. Inflammatory bowel disease in Chinese children: a multicenter analysis over a decade from Shanghai. Inflamm Bowel Dis. 2013;19:423–428. doi: 10.1097/MIB.0b013e318286f9f2. [DOI] [PubMed] [Google Scholar]
- 7.El Mouzan MI, Saadah O, Al-Saleem K, Al Edreesi M, Hasosah M, Alanazi A, Al Mofarreh M, Asery A, Al Qourain A, Nouli K, et al. Incidence of pediatric inflammatory bowel disease in Saudi Arabia: a multicenter national study. Inflamm Bowel Dis. 2014;20:1085–1090. doi: 10.1097/MIB.0000000000000048. [DOI] [PubMed] [Google Scholar]
- 8.Levine A, Koletzko S, Turner D, Escher JC, Cucchiara S, de Ridder L, Kolho KL, Veres G, Russell RK, Paerregaard A, et al. ESPGHAN revised porto criteria for the diagnosis of inflammatory bowel disease in children and adolescents. J Pediatr Gastroenterol Nutr. 2014;58:795–806. doi: 10.1097/MPG.0000000000000239. [DOI] [PubMed] [Google Scholar]
- 9.The WHO Child Growth Standard: Methods and Development. Geneva, Switzerland: Department of Nutrition for Health and Development, WHO; 2006. [Google Scholar]
- 10.de Onis M, Onyango AW, Borghi E, Siyam A, Nishida C, Siekmann J. Development of a WHO growth reference for school-aged children and adolescents. Bull World Health Organ. 2007;85:660–667. doi: 10.2471/BLT.07.043497. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Levine A, Griffiths A, Markowitz J, Wilson DC, Turner D, Russell RK, Fell J, Ruemmele FM, Walters T, Sherlock M, et al. Pediatric modification of the Montreal classification for inflammatory bowel disease: the Paris classification. Inflamm Bowel Dis. 2011;17:1314–1321. doi: 10.1002/ibd.21493. [DOI] [PubMed] [Google Scholar]
- 12.Hartman C, Eliakim R, Shamir R. Nutritional status and nutritional therapy in inflammatory bowel diseases. World J Gastroenterol. 2009;15:2570–2578. doi: 10.3748/wjg.15.2570. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Wiskin AE, Wootton SA, Hunt TM, Cornelius VR, Afzal NA, Jackson AA, Beattie RM. Body composition in childhood inflammatory bowel disease. Clin Nutr. 2011;30:112–115. doi: 10.1016/j.clnu.2010.07.014. [DOI] [PubMed] [Google Scholar]
- 14.Long MD, Crandall WV, Leibowitz IH, Duffy L, del Rosario F, Kim SC, Integlia MJ, Berman J, Grunow J, Colletti RB, et al. Prevalence and epidemiology of overweight and obesity in children with inflammatory bowel disease. Inflamm Bowel Dis. 2011;17:2162–2168. doi: 10.1002/ibd.21585. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Cole TJ, Bellizzi MC, Flegal KM, Dietz WH. Establishing a standard definition for child overweight and obesity worldwide: international survey. BMJ. 2000;320:1240–1243. doi: 10.1136/bmj.320.7244.1240. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Cole TJ. A chart to link child centiles of body mass index, weight and height. Eur J Clin Nutr. 2002;56:1194–1199. doi: 10.1038/sj.ejcn.1601473. [DOI] [PubMed] [Google Scholar]
- 17.Mamula P, Markowitz JE, Baldassano RN. Inflammatory bowel disease in early childhood and adolescence: special considerations. Gastroenterol Clin North Am. 2003;32:967–95, viii. doi: 10.1016/s0889-8553(03)00046-3. [DOI] [PubMed] [Google Scholar]
- 18.Vasseur F, Gower-Rousseau C, Vernier-Massouille G, Dupas JL, Merle V, Merlin B, Lerebours E, Savoye G, Salomez JL, Cortot A, et al. Nutritional status and growth in pediatric Crohn’s disease: a population-based study. Am J Gastroenterol. 2010;105:1893–1900. doi: 10.1038/ajg.2010.20. [DOI] [PubMed] [Google Scholar]
- 19.Blain A, Cattan S, Beaugerie L, Carbonnel F, Gendre JP, Cosnes J. Crohn’s disease clinical course and severity in obese patients. Clin Nutr. 2002;21:51–57. doi: 10.1054/clnu.2001.0503. [DOI] [PubMed] [Google Scholar]
- 20.Ogden CL, Carroll MD, Curtin LR, McDowell MA, Tabak CJ, Flegal KM. Prevalence of overweight and obesity in the United States, 1999-2004. JAMA. 2006;295:1549–1555. doi: 10.1001/jama.295.13.1549. [DOI] [PubMed] [Google Scholar]
- 21.Ogden CL, Carroll MD, Curtin LR, Lamb MM, Flegal KM. Prevalence of high body mass index in US children and adolescents, 2007-2008. JAMA. 2010;303:242–249. doi: 10.1001/jama.2009.2012. [DOI] [PubMed] [Google Scholar]
- 22.El Mouzan MI, Foster PJ, Al Herbish AS, Al Salloum AA, Al Omer AA, Qurachi MM, Kecojevic T. Prevalence of overweight and obesity in Saudi children and adolescents. Ann Saudi Med. 2010;30:203–208. doi: 10.4103/0256-4947.62833. [DOI] [PMC free article] [PubMed] [Google Scholar]


