Abstract
Rationale: Therapeutic alliance is a novel measure of the multifaceted caregiver–clinician relationship and a promising intervention target for improving patient-centered outcomes. However, therapeutic alliance has not been studied in an intensive care unit (ICU) setting.
Objectives: To explore the relationships among caregiver-reported therapeutic alliance and psychological distress as well as patient, caregiver, and ICU clinician factors.
Methods: In this cross-sectional study, we enrolled consecutive patient caregivers of mechanically ventilated patients discharged from all ICUs at Duke University and the Medical University of South Carolina Hospitals between December 2013 and August 2014.
Measurements and Main Results: Caregivers completed an in-person, hospital-based interview that included measures of therapeutic alliance with the ICU physicians (Human Connection Scale) as well as patient centeredness of care; symptoms of depression, anxiety, and post-traumatic stress; decisional conflict; and quality of communication. We performed a multivariate regression to characterize associations between Human Connection Scale scores and key variables. A total of 56 caregivers were included in these exploratory analyses. Patients were largely disabled (47%) and Medicare insured (53%). Caregivers were highly educated and generally had high therapeutic alliance (median, 55; interquartile range, 48–58) with the ICU clinicians. Therapeutic alliance was strongly correlated with patient centeredness (r = 0.78) and poorly correlated with psychological distress (r < 0.2). Stepwise multivariate modeling revealed that higher therapeutic alliance was associated with fewer baseline patient comorbidities as well as caregiver report of greater trust in the ICU team, better quality of communication, and less decisional conflict (all P < 0.012).
Conclusions: Therapeutic alliance encompasses measures of trust, communication, and cooperation, which are intuitive to forming a good working relationship. Therapeutic alliance among ICU caregivers is strongly associated with both modifiable and nonmodifiable factors. Our exploratory study highlights new intervention targets that may inform strategies for improving the quality of the caregiver–clinician interaction.
Keywords: therapeutic alliance, surrogate decision maker, psychological distress, quality of life, critical illness
Understanding patient- and caregiver-reported outcomes is necessary to providing holistic care in all settings, particularly in the stressful intensive care unit (ICU) environment. When patient/caregiver–clinician collaboration is suboptimal in ICUs, negative effects can be seen on decision-making quality in the short term as well as psychological distress in the longer term; moral distress and burnout can occur among clinicians (1–4). Conversely, interventions that focus on enhancing these interactions can alleviate distress, improve communication, and better align values and choice (5–7).
The nature and quality of the patient/caregiver–clinician relationship in the ICU setting has generally been described through measures of communication quality, the extent to which decision making is shared, and the presence of conflict (8–10). However, the strength and quality of the patient/caregiver–clinician relationship—the therapeutic alliance—includes other factors that are measured less frequently but are increasingly perceived as important (11). These elements include the extent to which participants feel trust, experience mutual caring and respect, work well together, believe the clinician understands their concerns about illness, and understand the information provided (12, 13). Recently, Mack and colleagues developed and validated a novel therapeutic alliance scale in the context of a large multicenter cohort of patients with advanced cancer (14). They found that strong therapeutic alliance was associated with better emotional functioning and decreased use of intensive care at the end of life.
Given the sizable number of patients who receive care in ICUs and the recognized need for improving patient-centered outcomes in this setting, we assessed therapeutic alliance between ICU family caregivers and ICU clinicians. In our exploratory study, we conceptualized therapeutic alliance as an important intersection of various patient, caregiver, and clinician factors that might in turn influence caregiver outcomes, including patient-centeredness of care and psychological distress. We also believed it was important to identify potentially modifiable aspects of therapeutic alliance to guide future intervention studies in patient-centered outcomes research in ICU populations.
Methods
Setting and Participants
We enrolled participants between December 2013 and August 2014 from Duke University and the Medical University of South Carolina. We screened adult ICUs (medical, surgical, neurologic) daily at Duke University Medical Center and the Medical University of South Carolina. Informal caregivers were eligible if they were self-described as a primary caregiver aged 18 years or older for a patient who received mechanical ventilation for more than 48 hours in an adult ICU, extubated, and eligible for transfer out of the ICU. Exclusion criteria were involvement in any ICU-based study that included an intervention designed to address psychological distress, planned discharge to hospice, and lack of spoken English fluency. Institutional review board approval was obtained for both sites, and informed consent was obtained for each participant. Participants were compensated $10 for their time.
Survey Procedures and Measures
Caregivers were interviewed once in person by study staff within a day of providing informed consent, generally within 1 day of transfer to the hospital ward. Patient electronic medical charts were abstracted for sociodemographic information and clinical characteristics (diagnosis, number of chronic medical comorbidities [15], illness severity [16], advance directives, code status). Caregivers also provided information on sociodemographics, religion, financial distress, and education. Additional questionnaire items included:
-
•
Therapeutic alliance: We adapted the Human Connection Scale (HCS) to assess the caregiver–ICU clinician (not patient–clinician) relationship, dropping a single item that dealt with cancer (14). The final survey included 15 Likert-scaled items that were scored from 1 (not at all/never) to 4 (a large extent/extremely); ranges included 15 (low therapeutic alliance) to 60 (high therapeutic alliance). Caregivers were instructed to rate their overall general impression of ICU attending physicians if they interacted with more than one.
-
•
Patient-centeredness: The Patient Perception of Patient-Centeredness (PPPC) questionnaire was adapted for caregiver use and administered to assess satisfaction with elements of patient-centered domains of ICU care (17). Scores on this 12-item Likert-scaled instrument range from 12 (low patient centeredness) to 48 (high patient centeredness).
-
•
Psychological distress: We used the Hospital Anxiety and Depression Scale (HADS; score range, 0–42; higher scores reflect greater distress) and the Post-Traumatic Stress Scale-10 (score range, 0–70; higher scores reflect greater distress) to assess symptoms of anxiety, depression, and post-traumatic stress disorder (18, 19).
-
•
Health literacy: This three-item scale was adapted from Peterson and colleagues (20)
-
•
Social support: This was assessed with FSE310592x2, a single Likert-scaled item (never, rarely, sometimes, usually, always) taken from the Patient Reported Outcomes Measurement Information System (PROMIS), “I have someone to confide in or talk to about myself and my problems.”
-
•
Decisional conflict: The low-literacy four-item version of the Decisional Conflict Scale was administered to assess the degree to which ICU-based decision making around life support was viewed (21).
-
•
Quality of communication: We used the 10-point Likert-scaled summary item from the Quality of Communication scale, “Overall, how would you rate the [ICU] physician’s communication with you?” to assess communication quality; higher scores reflect better perceived communication (22).
-
•
Quality of life: The Euro-QOL’s 100-point visual analog scale was used to assess caregivers’ current perceived quality of life, from 0 (worst quality of life imaginable) to 100 (best imaginable quality of life) (23).
Statistical Analysis
We analyzed the data using STATA software (v13, College Station, TX) for this exploratory study. We generated descriptive statistics including means, medians, and frequencies. We used imputation to address missing questionnaire items (no participant had more than two missing items on any single scale), substituting the missing item with the participant’s mean item score. We used Pearson correlations to characterize associations between the key outcome variables (therapeutic alliance, psychological distress, patient centeredness of care) and other patient-, caregiver-, and clinician-level variables. We performed regression modeling with therapeutic alliance as the primary outcome, including variables demonstrating at least a small to moderate association (r > 0.2). A final model was created using a stepwise method. Cronbach α and item-total correlations were performed on the HCS and the PPPC scales. A P less than 0.05 was considered to be statistically significant.
Results
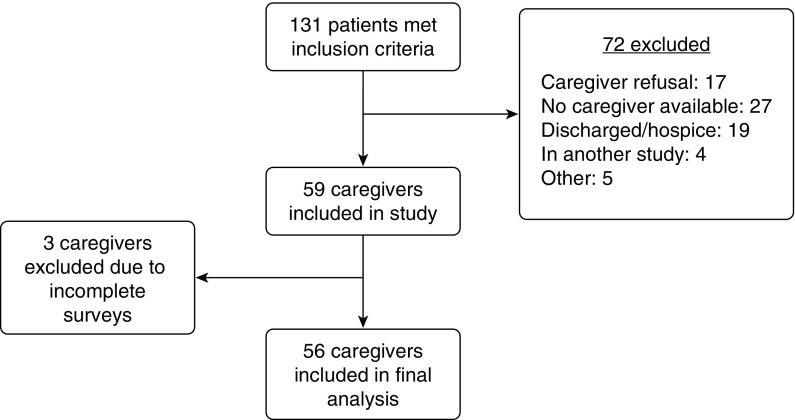
From a total of 131 patients who met inclusion criteria, 72 were excluded, and 59 (45%) patients’ caregivers provided informed consent (Figure 1). A total of 56 caregivers were included in analyses, as three surveys were incomplete. Patients’ ages were diversely distributed (range, 23–79 yr; median, 59 yr), although caregivers were younger (range, 21–73 yr; median, 50 yr). Caregivers described patients predominantly as disabled (47%) or retired (25%); most (53%) were Medicare insured (Table 1). Patients had a median of two chronic comorbid conditions. A total of 18 (31%) caregivers were patients’ spouses; the rest were children (33%), parents (17%), or other family (12%). Caregivers were highly educated (67% with education greater than high school). Patients were largely admitted from the emergency room or as transfers from outside hospitals (Table 2). Most were managed in medical ICUs (83%). The median Acute Physiology and Chronic Health Evaluation (APACHE) II score was 18 (interquartile range [IQR], 12–24).
Figure 1.
Study participant flow.
Table 1.
Patient and caregiver sociodemographics
| Demographic | Patients (n = 56) | Caregivers (n = 56) |
|---|---|---|
| Age, yr | ||
| ≤45 | 12 (21) | 18 (32) |
| 46–64 | 20 (36) | 28 (50) |
| ≥65 | 24 (43) | 10 (18) |
| Sex | ||
| Female | 21 (39) | 45 (78) |
| Race | ||
| African American | 24 (41) | 24 (41) |
| White | 32 (54) | 32 (54) |
| Residence before admission | ||
| Home | 34 (65) | |
| Inpatient rehabilitation | 1 (3) | |
| Nursing facility | 2 (4) | |
| Long-term acute care | 1 (3) | |
| Other acute care hospital | 14 (27) | |
| Charlson comorbidity score, median (IQR) | 2 (0–3) | |
| Religion | ||
| Catholic | 6 (11) | 5 (9) |
| Protestant | 44 (77) | 43 (75) |
| Other | 6 (12) | 8 (16) |
| Faith and/or spirituality | ||
| Moderately or very important | — | 49 (88) |
| Marital status | ||
| Married | 28 (50) | 42 (75) |
| Divorced | 9 (16) | 4 (7) |
| Single | 19 (34) | 10 (18) |
| Employment | ||
| Full time | 6 (11) | 30 (52) |
| Part time | 2 (4) | 5 (9) |
| Disabled | 27 (47) | 4 (7) |
| Retired | 14 (24) | 12 (21) |
| Unemployed | 2 (4) | 2 (4) |
| Education | ||
| <High school | — | 4 (7) |
| High school graduate | — | 14 (25) |
| Some college | — | 14 (25) |
| College graduate | — | 15 (26) |
| Advanced degree | — | 9 (16) |
| Financial distress | 20 (36) | |
| Caregiver relationship to patient | ||
| Spouse | — | 18 (32) |
| Child | — | 19 (34) |
| Parent | — | 10 (18) |
| Sibling | — | 4 (7) |
| Other family | — | 5 (9) |
| Insurance status | ||
| Medicare | 26 (46) | — |
| Medicaid | 7 (13) | — |
| Commercial | 12 (21) | — |
| None | 11 (20) | — |
| Previous treatment for psychiatric condition | 9 (16) | |
| Current treatment for: | ||
| Depression | — | 4 (7) |
| Anxiety | — | 6 (11) |
| PTSD | — | 0 (0) |
Definition of abbreviations: IQR = interquartile range; PTSD = post-traumatic stress disorder.
Data presented as n (%) unless otherwise noted.
Table 2.
Clinical characteristics of patients and intensive care unit setting
| n (%) or Median (IQR) | |
|---|---|
| Admission source | |
| Emergency room | 17 (32) |
| Hospital ward | 10 (19) |
| Transfer OSH | 22 (42) |
| Postoperative | 2 (4) |
| Other | 1 (2) |
| ICU type | |
| Medical | 43 (83) |
| Surgical | 9 (17) |
| APACHE II score | 18 (12–24) |
| Discharge disposition | |
| Home | 40 (70) |
| Nursing home | 11 (20) |
| Long-term acute care | 1 (2) |
| Hospice | 1 (2) |
| Dead | 4 (6) |
Definition of abbreviations: APACHE = Acute Physiology and Chronic Health Evaluation; ICU = intensive care unit; IQR = interquartile range; OSH = outside hospital.
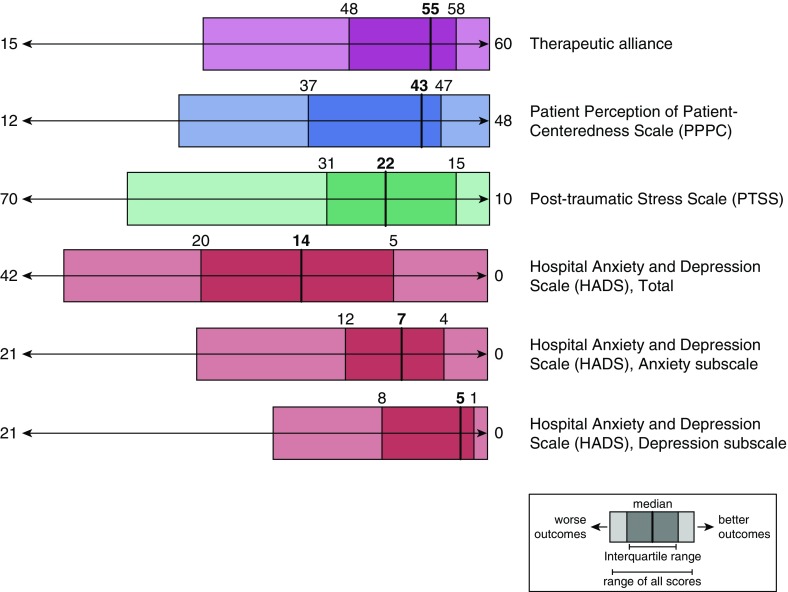
The main study outcomes are shown in Figure 2. Therapeutic alliance scores were relatively high (median, 55; IQR, 48–58), and seven (13%) had maximum scores of 60. Similarly, median patient-centeredness scores were 43 (IQR, 37–47) and near the upper range of the scale; 13 (23%) caregivers’ scores reported the maximum of 48. Respondents’ psychological distress was moderate, as reflected by their median PTSS scores (22; IQR, 15–31), HADS total scores (14; IQR, 5–20), HADS anxiety scores (7; IQR, 4–12), and HADS depression scores (5; IQR, 1–8). Interestingly, no factors related to either the clinician–caregiver interaction or the patient’s clinical status correlated with post-traumatic stress or anxiety and depression.
Figure 2.
Study outcomes. Scores for each questionnaire are displayed as indicated in the figure legend above, with extremes displayed as more negative (i.e., more distress) to the left and more positive (i.e., less distress) to the right. Medians are represented by the dark vertical lines and corresponding numerical values in bold above the lines. Interquartile ranges are represented by darker color shades, with numerical values of their boundaries shown above. Lighter shaded sections represent the entire range of all participant responses. The scale of each questionnaire's values has been adjusted to fit a 100-point standard distance.
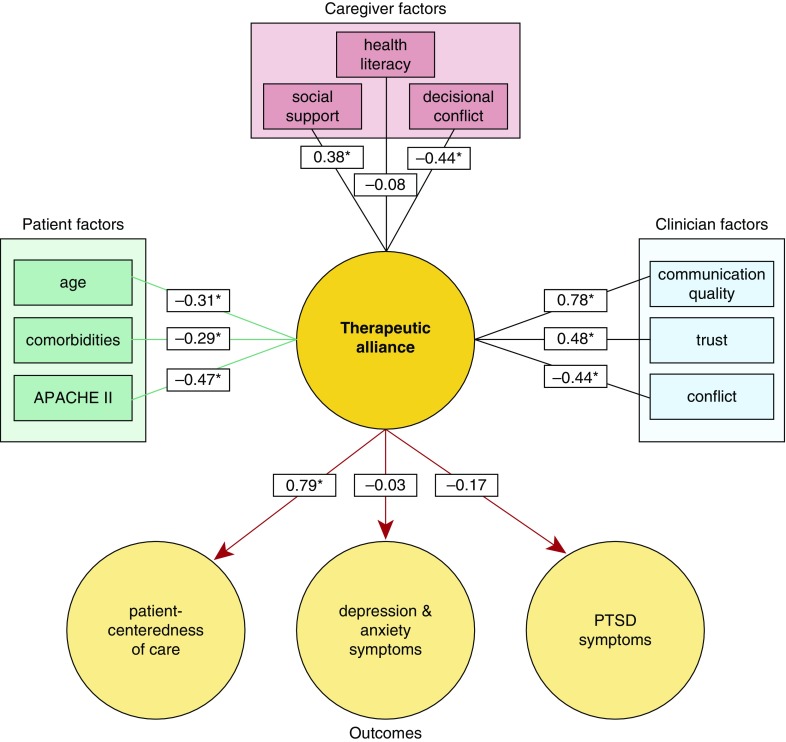
We evaluated the association between therapeutic alliance and patient-centered care, post-traumatic stress, and anxiety and depression within the context of patient, caregiver, and clinician characteristics in our conceptual model using Pearson correlations (Figure 3). Although therapeutic alliance was strongly correlated with patient centeredness (r = 0.79, P < 0.05), it was poorly associated with psychological distress and quality of life (all P > 0.05), as shown in our conceptual model (see Table E1 in the online supplement). The caregiver factor most strongly associated with better therapeutic alliance was with perceived social support (r = 0.38); lower scores were associated with higher levels of decisional conflict (r = −0.44). Caregiving burden, quality of life, faith, caregiver age, and health literacy were not associated with therapeutic alliance (all r < 0.1). Advanced patient age, greater numbers of comorbid conditions, and higher APACHE II score on ICU Day 1 were associated with lower reported therapeutic alliance (Table 3). Descriptors of the caregiver–clinician interaction positively correlated with therapeutic alliance were perception that ICU treatments reflected patient wishes, trust in the ICU team, and quality of communication (all P < 0.05); conflict with the ICU team was associated with lower alliance. Multiple regression modeling demonstrated that higher therapeutic alliance was associated with fewer baseline comorbidities, higher trust in ICU physicians, better quality of communication, and less decisional conflict (all P < 0.02) (Table 3).
Figure 3.
Therapeutic alliance and its relationship to key stakeholder characteristics and outcomes in our conceptual model. Correlations are shown between key variables in the figure. Asterisks represent correlations with P < 0.05. APACHE = Acute Physiology and Chronic Health Evaluation; PTSD = post-traumatic stress disorder.
Table 3.
Therapeutic alliance and its relationship to key patient, caregiver, and clinician factors: exploratory regression modeling results
| Therapeutic Alliance, Unadjusted, Mean (SD)* | P Value | Regression Model β (95% CI)† | P Value | |
|---|---|---|---|---|
| Patient age, yr | 0.046 | — | — | |
| <55 | 55 (7) | |||
| ≥55 | 51 (7) | |||
| Patient Charlson Comorbidity Index score | 0.009 | 4.74 (2.29–7.18) | <0.001 | |
| <2 Comorbidities | 55 (6) | |||
| ≥2 Comorbidities | 49 (7) | |||
| Patient APACHE II score | 0.033 | — | — | |
| <20 | 54 (6) | |||
| ≥20 | 50 (9) | |||
| Caregiver social support | 0.001 | — | — | |
| High | 55 (6) | |||
| Low | 48 (8) | |||
| Caregiver report that treatment reflected patient wishes | 0.004 | — | — | |
| Yes | 55 (5) | |||
| No or unsure | 50 (8) | |||
| Caregiver trust in ICU team | <0.001 | 4.43 (1.70–7.18) | 0.002 | |
| High | 56 (4) | |||
| Low | 47 (8) | |||
| Caregiver report of conflict with ICU team | 0.045 | — | — | |
| Low or none | 55 (6) | |||
| Moderate or high | 51 (8) | |||
| Caregiver report of quality of communication | <0.001 | 5.97 (2.76–9.2) | <0.001 | |
| High | 55 (5) | |||
| Low | 44 (7) | |||
| Caregiver report of decisional conflict | 0.001 | 4.21 (0.95–7.47) | 0.012 | |
| Low | 54 (6) | |||
| High | 46 (8) |
Definition of abbreviations: APACHE = Acute Physiology and Chronic Health Evaluation; CI = confidence interval; HADS = Hospital Anxiety and Depression Scale; HCS = Human Connection Scale; ICU = intensive care unit; PTSS = post-traumatic stress scale.
Relationship between HCS score and variable; P value from paired t tests. Variables not included in modeling because HCS–variable r < 0.2: caregiver age, faith, health literacy, active coping use, caregiver burden, caregiver quality of life, HADS anxiety score, HADS depression score, HADS total score, and PTSS score.
Relationship between HCS score and key variables using stepwise regression model adjusted for variables shown; constant = 44.05 (40.73–47.37), P < 0.001.
Item-total correlations for therapeutic alliance scores were strongest for items addressing how much caregivers liked and respected their physician, how thorough they believed the physician was, how much they trusted the physician, how open-minded the physician was, and how much the physician appeared to care (all r > 0.7 and all P < 0.05; Table E2). Of note, patient-centeredness item-total correlations were highest for the extent to which the team explained things, satisfaction with ICU discussions, the extent to which the team explained options for life support, and the amount of encouragement physicians gave caregivers in choosing their patient care role (all r > 0.6 and all P < 0.05; Table E3).
Discussion
Patient-centered care is a fundamental element of high-quality health care delivery (24). Patient-centered care is complex, in that it should reflect patient preferences, needs, and values, and thus varies between patients confronted with identical clinical scenarios. In recognizing that patients exist in the context of their personal and social circumstances, the concept of patient-centered care has evolved to include the family (25). Regulatory commissions have provided road maps for hospitals and providers to better meet the holistic needs of patients and families (26). The concept of family-centered care is particularly relevant in ICU patient populations, as very often family members must act as patient surrogates. In this exploratory study, we describe for the first time how therapeutic alliance—a multidimensional measure of the quality of the family–clinician relationship—is strongly associated with families’ perceptions of patient-centered care.
Therapeutic alliance is a relatively new concept that integrates patient, caregiver, and clinician factors into a measurable construct (11). The conceptual support for such a measure is linked to a variety of observations, including the positive effects of the patient–clinician relationship on decision-making quality, health outcomes, as well as on treatment response (27–32). Therefore, a number of factors relevant to these relationships are aggregated in a single measure—which has not previously been studied in an ICU population. The strength of this therapeutic alliance—the human connection comprising support, caring, respect, trust, understanding, attention, and empathy—encompasses more than just the commonly studied, yet important, areas of communication quality, shared decision making, and conflict (8–10, 33, 34). Although therapeutic alliance has been studied in an outpatient setting (14, 17), our ICU-based results highlight a novel exploration of this promising construct.
Potentially modifiable factors associated with therapeutic alliance include perceived social support and intuitive supportive elements of the clinician–caregiver interaction, such as communication quality, trust, and respect. However, we also found other uncommonly considered qualities of care, such as clinician thoroughness, offering of hope, showing concern, and being open-minded, were strongly associated with greater therapeutic alliance. This highlights novel focal points that are valued by caregivers and are potential areas of future interventions to enhance patient centeredness of care. Furthermore, therapeutic alliance may be a promising holistic measure of the quality and patient centeredness of care (35).
Nonmodifiable factors associated with therapeutic alliance include patient factors such as illness severity, patient age, and the number of comorbidities. It is possible that caregivers of more severely ill patients might not bond as well with the ICU clinician due to greater stress, more intense life support decision-making needs, an inherent difference in the content of their interaction with the ICU clinician, or because longer stays reflect greater exposure to multiple clinicians and worse continuity. Clinicians caring for older and more seriously ill patients may withdraw to an extent because of low perceived utility of care. Advanced patient age has been reported by Mack and colleagues as well to be associated with lower therapeutic alliance (14). These findings suggest that age-based palliative care triggers may have some merit, as there appears to be a potentially unmet need among the elderly that extends beyond just the higher risk of mortality (36). Although these patient factors cannot be changed, it is possible that different communication strategies could improve therapeutic alliance among such patients’ family members. Interestingly, therapeutic alliance was not associated with caregiver traits such as age, faith, and health literacy. This may suggest that therapeutic alliance measures the actual quality of the clinical interaction rather than caregiver traits that are difficult to change.
The Human Connection Scale (HCS) measuring therapeutic alliance and the PPPC have properties worth scrutinizing. First, they were highly correlated (r = 0.79), and as shown in the online supplement, a number of items address similar factors. However, the two scales frame their respective approaches differently. The PPPC focuses more on whether certain clinician actions were done, whereas the HCS focuses predominantly on a family member’s perceptions about the quality of these actions. The HCS seemed to reflect quality of communication more strongly than the PPPC, which was more strongly associated with the amount of decisional conflict the respondent had. Second, neither metric was strongly associated with acute psychological distress. It is possible that the low to moderate level of psychological distress in our population as well as our relatively small sample were related to this finding. Third, like other instruments used to characterize elements of the clinician–patient/family interaction (22), both questionnaires had high median scores that suggest a concerning “ceiling effect” should they be used as primary outcomes in a clinical trial. Also, our results are similar to those of Mack and colleagues’ exploration of therapeutic alliance among patients (mean score = 53) (14). Still, given our small sample and lack of longitudinal administration, judgments about the HCS’s psychometric performance are premature. Finally, it is worth pointing out that some HCS items are similar in wording to items we used to assess trust and communication. However, HCS items that were most strongly associated with total HCS scores included those characterizing dimensions broader than these concepts, including clinician thoroughness, respect, open mindedness, and care shown for patients.
This study has limitations. It was conducted in two academic medical centers in the southeastern United States. Therefore, our results could be different in nonacademic centers, other parts of the country, or with less-educated caregivers. We also sampled caregivers of patients who survived mechanical ventilation and agreed to discuss their experience with our team. As such, our findings cannot inform a better understanding of therapeutic alliance and end-of-life care and may not capture the full range of caregiver beliefs. Our sample size did not permit exploration of how different caregiver, patient, and clinician outcomes impacted therapeutic alliance when considered together in a sophisticated model. Also, we adapted the HCS from its original setting (oncology clinics) and target (patients rating a single physician) to the multiprovider ICU setting and informal caregivers. Although caregivers reported no difficulties understanding the adapted HCS or our instructions to think of their general experience with the main ICU physician, variation in interpretation could be significant. Last, because we used a cross-sectional design, we are not able to describe the responsiveness of the HCS to change or its minimal clinically important difference in score. Further study should focus on better understanding the psychometric properties of the HCS as well as perceived therapeutic alliance among a more diverse population and in the context of how ICU staffing, nursing, and communication models affect it.
In conclusion, therapeutic alliance is a patient/caregiver-centered metric that provides a novel insight into the degree to which supportive relationships are formed in an ICU between people who are initially strangers. Better understanding the bond between the clinician and caregiver provides new targets for interventions to improve the quality of ICU care.
Footnotes
Supported by National Institutes of Health grant R01 HL109823 (C.E.C.).
Previously presented at the 2015 American Thoracic Society International Conference, Denver, Colorado.
Author Contributions: Study design and concept: N.G.H. and C.E.C.; statistical analysis: C.E.C. and N.G.H.; writing and review: N.G.H., C.E.C., D.W.F., and N.N.; supervising data collection: N.G.H., N.N., D.W.F., and C.E.C.; acquisition of funding: C.E.C.; final approval: N.G.H., N.N., D.W.F., and C.E.C.; accountable for all work: N.G.H. and C.E.C.
This article has an online supplement, which is accessible from this issue’s table of contents at www.atsjournals.org
Author disclosures are available with the text of this article at www.atsjournals.org.
References
- 1.You JJ, Dodek P, Lamontagne F, Downar J, Sinuff T, Jiang X, Day AG, Heyland DK ACCEPT Study Team and the Canadian Researchers at the End of Life Network (CARENET) What really matters in end-of-life discussions? Perspectives of patients in hospital with serious illness and their families. CMAJ. 2014;186:E679–E687. doi: 10.1503/cmaj.140673. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Piers RD, Azoulay E, Ricou B, Dekeyser Ganz F, Decruyenaere J, Max A, Michalsen A, Maia PA, Owczuk R, Rubulotta F, et al. APPROPRICUS Study Group of the Ethics Section of the ESICM. Perceptions of appropriateness of care among European and Israeli intensive care unit nurses and physicians. JAMA. 2011;306:2694–2703. doi: 10.1001/jama.2011.1888. [DOI] [PubMed] [Google Scholar]
- 3.Pochard F, Azoulay E, Chevret S, Lemaire F, Hubert P, Canoui P, Grassin M, Zittoun R, le Gall JR, Dhainaut JF, et al. French FAMIREA Group. Symptoms of anxiety and depression in family members of intensive care unit patients: ethical hypothesis regarding decision-making capacity. Crit Care Med. 2001;29:1893–1897. doi: 10.1097/00003246-200110000-00007. [DOI] [PubMed] [Google Scholar]
- 4.Kentish-Barnes N, Chaize M, Seegers V, Legriel S, Cariou A, Jaber S, Lefrant JY, Floccard B, Renault A, Vinatier I, et al. Complicated grief after death of a relative in the intensive care unit. Eur Respir J. 2015;45:1341–1352. doi: 10.1183/09031936.00160014. [DOI] [PubMed] [Google Scholar]
- 5.Lautrette A, Darmon M, Megarbane B, Joly LM, Chevret S, Adrie C, Barnoud D, Bleichner G, Bruel C, Choukroun G, et al. A communication strategy and brochure for relatives of patients dying in the ICU. N Engl J Med. 2007;356:469–478. doi: 10.1056/NEJMoa063446. [DOI] [PubMed] [Google Scholar]
- 6.Cox CE, Lewis CL, Hanson LC, Hough CL, Kahn JM, White DB, Song MK, Tulsky JA, Carson SS. Development and pilot testing of a decision aid for surrogates of patients with prolonged mechanical ventilation. Crit Care Med. 2012;40:2327–2334. doi: 10.1097/CCM.0b013e3182536a63. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Aslakson R, Cheng J, Vollenweider D, Galusca D, Smith TJ, Pronovost PJ. Evidence-based palliative care in the intensive care unit: a systematic review of interventions. J Palliat Med. 2014;17:219–235. doi: 10.1089/jpm.2013.0409. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Cox CE, Martinu T, Sathy SJ, Clay AS, Chia J, Gray AL, Olsen MK, Govert JA, Carson SS, Tulsky JA. Expectations and outcomes of prolonged mechanical ventilation. Crit Care Med. 2009;37:2888–2894, quiz 2904. doi: 10.1097/CCM.0b013e3181ab86ed. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.White DB, Braddock CH, III, Bereknyei S, Curtis JR. Toward shared decision making at the end of life in intensive care units: opportunities for improvement. Arch Intern Med. 2007;167:461–467. doi: 10.1001/archinte.167.5.461. [DOI] [PubMed] [Google Scholar]
- 10.Curtis JR, Engelberg RA, Wenrich MD, Nielsen EL, Shannon SE, Treece PD, Tonelli MR, Patrick DL, Robins LS, McGrath BB, et al. Studying communication about end-of-life care during the ICU family conference: development of a framework. J Crit Care. 2002;17:147–160. doi: 10.1053/jcrc.2002.35929. [DOI] [PubMed] [Google Scholar]
- 11.Mead N, Bower P. Patient-centredness: a conceptual framework and review of the empirical literature. Soc Sci Med. 2000;51:1087–1110. doi: 10.1016/s0277-9536(00)00098-8. [DOI] [PubMed] [Google Scholar]
- 12.Teno JM, Clarridge BR, Casey V, Welch LC, Wetle T, Shield R, Mor V. Family perspectives on end-of-life care at the last place of care. JAMA. 2004;291:88–93. doi: 10.1001/jama.291.1.88. [DOI] [PubMed] [Google Scholar]
- 13.Curtis JR, Wenrich MD, Carline JD, Shannon SE, Ambrozy DM, Ramsey PG. Understanding physicians’ skills at providing end-of-life care perspectives of patients, families, and health care workers. J Gen Intern Med. 2001;16:41–49. doi: 10.1111/j.1525-1497.2001.00333.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Mack JW, Block SD, Nilsson M, Wright A, Trice E, Friedlander R, Paulk E, Prigerson HG. Measuring therapeutic alliance between oncologists and patients with advanced cancer: the Human Connection Scale. Cancer. 2009;115:3302–3311. doi: 10.1002/cncr.24360. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Charlson ME, Pompei P, Ales KL, MacKenzie CR. A new method of classifying prognostic comorbidity in longitudinal studies: development and validation. J Chronic Dis. 1987;40:373–383. doi: 10.1016/0021-9681(87)90171-8. [DOI] [PubMed] [Google Scholar]
- 16.Knaus WA, Draper EA, Wagner DP, Zimmerman JE. APACHE II: a severity of disease classification system. Crit Care Med. 1985;13:818–829. [PubMed] [Google Scholar]
- 17.Stewart M, Brown JB, Donner A, McWhinney IR, Oates J, Weston WW, Jordan J. The impact of patient-centered care on outcomes. J Fam Pract. 2000;49:796–804. [PubMed] [Google Scholar]
- 18.Eid J, Thayer JF, Johnsen BH. Measuring post-traumatic stress: a psychometric evaluation of symptom--and coping questionnaires based on a Norwegian sample. Scand J Psychol. 1999;40:101–108. doi: 10.1111/1467-9450.00105. [DOI] [PubMed] [Google Scholar]
- 19.Zigmond AS, Snaith RP. The hospital anxiety and depression scale. Acta Psychiatr Scand. 1983;67:361–370. doi: 10.1111/j.1600-0447.1983.tb09716.x. [DOI] [PubMed] [Google Scholar]
- 20.Peterson PN, Shetterly SM, Clarke CL, Bekelman DB, Chan PS, Allen LA, Matlock DD, Magid DJ, Masoudi FA. Health literacy and outcomes among patients with heart failure. JAMA. 2011;305:1695–1701. doi: 10.1001/jama.2011.512. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Légaré F, Kearing S, Clay K, Gagnon S, D’Amours D, Rousseau M, O’Connor A. Are you SURE?: assessing patient decisional conflict with a 4-item screening test. Can Fam Physician. 2010;56:e308–e314. [PMC free article] [PubMed] [Google Scholar]
- 22.Engelberg R, Downey L, Curtis JR. Psychometric characteristics of a quality of communication questionnaire assessing communication about end-of-life care. J Palliat Med. 2006;9:1086–1098. doi: 10.1089/jpm.2006.9.1086. [DOI] [PubMed] [Google Scholar]
- 23.EuroQol Group. EuroQol--a new facility for the measurement of health-related quality of life. Health Policy. 1990;16:199–208. doi: 10.1016/0168-8510(90)90421-9. [DOI] [PubMed] [Google Scholar]
- 24.Institute of Medicine Committee on Quality of Health Care in America. Washington, D.C.: National Academy Press; 2001. Crossing the quality chasm: a new health system for the 21st century. [Google Scholar]
- 25.Davidson JE, Powers K, Hedayat KM, Tieszen M, Kon AA, Shepard E, Spuhler V, Todres ID, Levy M, Barr J, et al. American College of Critical Care Medicine Task Force 2004-2005, Society of Critical Care Medicine. Clinical practice guidelines for support of the family in the patient-centered intensive care unit: American College of Critical Care Medicine Task Force 2004-2005. Crit Care Med. 2007;35:605–622. doi: 10.1097/01.CCM.0000254067.14607.EB. [DOI] [PubMed] [Google Scholar]
- 26.The Joint Commission. Advancing effective communication, cultural competence, and patient-family-centered care: a roadmap for hospitals. 2010 [accessed 2015 Jun 16]. Available from: http://www.jointcommission.org/Advancing_Effective_Communication/
- 27.Chiarchiaro J, Buddadhumaruk P, Arnold RM, White DB. Quality of communication in the ICU and surrogate’s understanding of prognosis. Crit Care Med. 2015;43:542–548. doi: 10.1097/CCM.0000000000000719. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Stapleton RD, Engelberg RA, Wenrich MD, Goss CH, Curtis JR. Clinician statements and family satisfaction with family conferences in the intensive care unit. Crit Care Med. 2006;34:1679–1685. doi: 10.1097/01.CCM.0000218409.58256.AA. [DOI] [PubMed] [Google Scholar]
- 29.Anderson WG, Cimino JW, Ernecoff NC, Ungar A, Shotsberger KJ, Pollice LA, Buddadhumaruk P, Carson SS, Curtis JR, Hough CL, et al. A multicenter study of key stakeholders’ perspectives on communicating with surrogates about prognosis in intensive care units. Ann Am Thorac Soc. 2015;12:142–152. doi: 10.1513/AnnalsATS.201407-325OC. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Summers RF, Barber JP. Therapeutic alliance as a measurable psychotherapy skill. Acad Psychiatry. 2003;27:160–165. doi: 10.1176/appi.ap.27.3.160. [DOI] [PubMed] [Google Scholar]
- 31.Kaplan SH, Greenfield S, Ware JE., Jr Assessing the effects of physician-patient interactions on the outcomes of chronic disease. Med Care. 1989;27:S110–S127. doi: 10.1097/00005650-198903001-00010. [DOI] [PubMed] [Google Scholar]
- 32.Joyce AS, Ogrodniczuk JS, Piper WE, McCallum M. The alliance as mediator of expectancy effects in short-term individual therapy. J Consult Clin Psychol. 2003;71:672–679. doi: 10.1037/0022-006x.71.4.672. [DOI] [PubMed] [Google Scholar]
- 33.Tulsky JA. Beyond advance directives: importance of communication skills at the end of life. JAMA. 2005;294:359–365. doi: 10.1001/jama.294.3.359. [DOI] [PubMed] [Google Scholar]
- 34.Curtis JR, Back AL, Ford DW, Downey L, Shannon SE, Doorenbos AZ, Kross EK, Reinke LF, Feemster LC, Edlund B, et al. Effect of communication skills training for residents and nurse practitioners on quality of communication with patients with serious illness: a randomized trial. JAMA. 2013;310:2271–2281. doi: 10.1001/jama.2013.282081. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Curtis JR. Communicating about end-of-life care with patients and families in the intensive care unit. Crit Care Clin. 2004;20:363–380, viii. doi: 10.1016/j.ccc.2004.03.001. [DOI] [PubMed] [Google Scholar]
- 36.Aslakson RA, Curtis JR, Nelson JE. The changing role of palliative care in the ICU. Crit Care Med. 2014;42:2418–2428. doi: 10.1097/CCM.0000000000000573. [DOI] [PMC free article] [PubMed] [Google Scholar]