Abstract
AIM: To investigate the expression of pathological factors of VEGF-C and its receptor FLT-4 in primary gastric cancer and adjacent normal tissues.
METHODS: The expression of VEGF-C and FLT-4 was studied in 80 primary gastric cancers and adjacent normal tissues from the same patients by semi-quantitative reverse transcriptase-polymerase chain reaction (RT-PCR) and immumohistochemistry.
RESULTS: Both primary gastric cancer and adjacent normal tissue could express VEGF-C and FLT-4, and FLT-4 expression was also detected in endothelial cells of stromal blood vessels and lymphatic vessels. There was a significant difference in expression of VEGF-C between primary tumor and adjacent normal tissue samples (P = 0.01), and a statistical correlation between VEGF-C and FLT-4 expression in tumors (P = 0.00886). With regard to VEGF-C expression, there was a significant difference between moderate-poor differential type and high differential type (P = 0.032), and a significant difference between positive and negative lymph node metastases (P = 0.024). However, there was no significant difference between positive and negative serosal invasions (P = 0.219).
CONCLUSION: VEGF-C and its receptor FLT-4 play a role in the development of gastric cancer, and the tumors with expression of VEGF-C and FLT-4 are more likely to have lymph node metastasis.
INTRODUCTION
Invasion and metastasis are the characteristics of malignant tumor. Epithelial malignancy spreads predominantly through lymphatic system, and its metastastic degree is closely related to patient’s prognosis[1]. However, very little is known about the mechanism of lymphangiogenesis and lymph node metastasis. Recent studies have shown that VEGF-C can bind to specific receptor VEGFR3/FLT-4 that express in lymphatic endothelium, stimulate lymphangiogenesis, and promote lymphatic metastasis[2-4]. We investigated the expression and significance of VEGF-C and its receptor FLT-4 in gastric cancer.
MATERIALS AND METHODS
Materials
Reagents Trizol liquid, AMV reverse transcriptase, Oligd(T)14, RNAsin, dNTP, Taq DNA polymerase were purchased from Shanghai Sangon Biological Engineering Technology and Service Co.Ltd, PCR primers were synthesized by Shanghai Sangon Biological Engineering Technology and Service Co. Ltd. The antibodies of VEGF-C and FLT-4 were purchased from Santa Cruz Company.
Clinical data A total of 80 patients with primary gastric cancer were analyzed, with a mean age of 53.5 years, arranging from 38 to 72 years. Routine pathological diagnosis showed that 59 cases were adenocarcinoma and 21 cases were signet carcinoma. Among them, 54 cases presented lymph node metastasis, and 26 cases had no lymph node metastasis.
Methods
Detection of expression of VEGF-C AND FLT-4 Expression of VEGF-C and FLT-4 was assessed in each gastric cancer sample and its adjacent normal tissues by semi-quantitative RT-PCR.
RNA extraction Total RNA was extracted by Trizol one-step procedure, and suspended in DEPC-treated reverse osmosis-H20, and conserved at -70 °C for reverse transcription. RNA yield and purity were determined by standard UV spectrophotometric assay. The ratio of A260/A280 was 1.80.
First strand cDNA synthesis Five µg of the total RNA was dissolved in 20 µl of mixture containing 2 µl 10 × first-strand buffer, 20 U AMV reverse transcriptase, 2 µl dNTP, 20 U RNAsin, 500 ng Oligd(T)14, and DEPC-treated reverse osmosis-H2O. The reaction conditions were as follows: at 42 °C for 60 min, and at 95 °C for 5 min. The first strand cDNA was stored at -20 °C until use.
PCR amplification The primers of VEGF-C, FLT-4 and β-actin were synthesized according to the primer design principles, all primers span an intron to control against amplification of genomic DNA sequences. Four µl first strand cDNA was amplified in 20 µl volume. The primers of VEGF-C yielded 206 bp product as follows: 5’-end primer: 5’-AAGGAGGCTGGCAACATAAC-3’, 3’-end primer: 5’-CCACATCTGTAGACGGACAC-3’. Following an initial denaturation at 94 °C for 5 min, the samples were amplified by 30 cycles of denaturation at 94 °C for 30 s, annealing at 58 °C for 30 s, extension at 72 °C for 30 s, and ended by extension at 72 °C for 10 min. The primers of FLT-4 yielded a 298 bp product as follows: 5’-end primer: 5’-AGCCATTCATCAACAAGCCT-3’, 3’-end primer: 5’-GGCAACAGCTGGATGTCATA-3’. Following an initial denaturation at 94 °C for 5 min, the samples were amplified by 28 cycles of denaturation at 94 °C for 30 s, annealing at 58 °C for 1 min, extension at 72 °C for 1 min, and ended by extension at 72 °C for 10 min. The primers of β-actin, which was amplified with VEGF-C and FLT-4 as an internal control, yielded a 644 bp product as follows: 5’-end primer: 5’-ACGTTATGGATGATGATATCGC-3’, 3’-end primer: 5’-CTTAATGTCACGCACGATTTCC-3’. The PCR products were separated on 1.7% agarose gel, stained with ethidium bromide, and analyzed with Quantity one 4.1.0 software. The ratios of VEGF-C/β-actin, and FLT-4/β-actin were used to semiquantify the levels of VEGF-C and FLT-4.
Immunohistochemistry Immunohistochemical studies of VEGF-C and FLT-4 expression in gastric cancer and adjacent normal tissues were performed by the avidin-biotin-peroxidase technique, as previously described[5].
Statistical analysis Statistical analyses were made with SPSS software, version 10.0.
RESULTS
Results of RT-PCR
Eighty primary gastric cancers and adjacent normal tissues from the same patients were examined for the expression of VEGF-C and FLT-4 by RT-PCR. In 80 cases of primary tumors, VEGF-C and FLT-4 were expressed in 58 (72.5%) and 51 (63.75%) cases, respectively. However, in 80 adjacent normal samples, VEGF-C and FLT-4 were expressed in 13 (16.25%) and 16 (20%), respectively. The expression of VEGF-C and FLT-4 in primary gastric cancer was significantly different from that in adjacent normal tissues (P = 0.01 and P = 0.038 respectively, Figure 1, Table 1).
Figure 1.
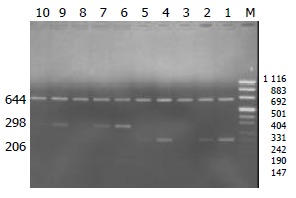
Semi-quantitative RT-PCR amplified products of VEGF-C and FLT-4 in primary gastric cancer and adjacent nor-mal tissues. Lane-M: puc mix marker 8 (1116, 883, 692, 501, 404, 331, 242, 190, 147, 110, 67, 34, 26, 19) bp, 644 bp: internal standards, 298 bp: FLT-4 expression, 206 bp: VEGF-C expression, Lane 1: Control of VEGF-C positive expression in placenta, Lane 6: Control of FLT-4 positive expression in placenta, Lanes 2, 4: VEGF-C expression in primary gastric cancer, Lanes 3, 5: VEGF-C expression in adjacent normal tissues, Lanes 7, 9: FLT-4 expression in primary gastric cancer, Lanes 8, 10: FLT-4 expression in adjacent normal tissues.
Table 1.
Expression of VEGF-C and FLT-4 in primary gastric cancers and adjacent normal tissues detected by semi-quanti-tative RT-PCR (mean ± SD)
| Cases | VEGF-C | FLT-4 | |
| Primary gastric cancers | 80 | 0.555 ± 0.399a | 0.335 ± 0.261b |
| Adjacent normal tissues | 80 | 0.146 ± 0.311c | 0.153 ± 0.275d |
P = 0.01 vs groupc,
P = 0.038 vs groupd.
Meanwhile, in 58 cases of gastric cancer with VEGF-C positive expression, FLT-4 was coexpressed in 42 cases (82.35%), but 22 cases of gastric cancer with VEGF-C negative expression showed FLT-4 expression in 9 cases (40.91%). The VEGF-C expression in primary tumors was significantly correlated with FLT-4 (P = 0.00886).
Result of immunohistochemistry
Human placenta served as a positive control. Positive expression of VEGF-C and FLT-4 showed brown staining in the cytoplasm of tumor or normal cells, more than 500 cells were calculated in different microscopic fields of slides, and percentage of positive cells was evaluated. Staining intensities were scored according to the following scale: -, no cells stained; +, less than 25% of cells stained; ++, 26% to 50% of cells stained; +++, 51% to 75% of cells stained; ++++, more than 75% of cells stained.
Immunohistochemical staining revealed that VEGF-C was expressed in 55 of 80 primary tumors (68.75%) and 11 of 80 adjacent normal tissues (13.75%), FLT-4 was expressed in 49 of 80 primary tumors (61.25%) and 14 of 80 adjacent normal tissues (17.5%), FLT-4 also expressed in endothelium of small blood and lymphatic vessels. There was a significant difference in the expression of VEGF-C and FLT-4 between gastric cancer and adjacent normal tissues (Table 2, Figure 2).
Table 2.
Expression of VEGF-C and FLT-4 in primary gastric cancers and adjacent normal tissues detected by immumohis-tochemistry
| Positive expression | Primary gastric | Adjacent normal | ||
|
cancer (cases) |
tissue (cases) |
|||
| VEGF-C | FLT-4 | VEGF-C | FLT-4 | |
| + | 3 | 2 | 2 | 3 |
| ++ | 7 | 8 | 4 | 5 |
| +++ | 20 | 18 | 3 | 3 |
| ++++ | 25 | 21 | 2 | 3 |
Figure 2.
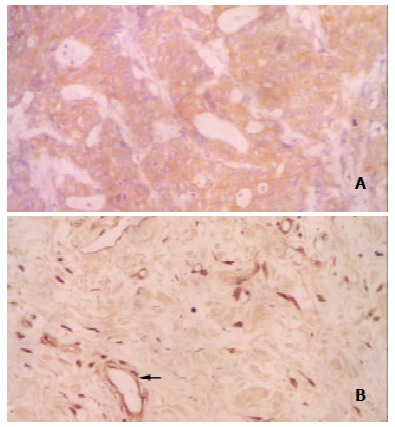
Expression of VEGF-C and FLT-4 in gastric cancer. A: VEGF-C positive expression in gastric cancer, × 400. B: FLT-4 positive expression in gastric cancer, × 200. (←endothelial cells of vessels).
Pathologic factors affecting expression of VEGF-C
Several pathological factors, including histological type, lymph node metastasis, serosal invasion, were investigated to predict the expression of VEGF-C in gastric cancer. The results showed that there was a significant difference in expression of VEGF-C between moderately-poorly differentiated type and highly differentiated type (P = 0.032), and a significant difference between positive lymph node metastasis and negative lymph node metastasis (P = 0.024). However, there was no significant difference between positive and negative serosal invasions (P = 0.219, Table 3).
Table 3.
Correlation between pathological factors and VEGF-C expression in 80 primary gastric cancers
| Pathological factors | No. of cases | VEGF-C mRNA | P |
| (mean ± SD) | |||
| Histological type | |||
| Moderately-Poorly | 51 | 0.485 ± 0.345 | P = 0.032 |
| differential | |||
| Highly differential | 29 | 0.200 ± 0.290 | |
| Lymph node metastasis | |||
| Positive | 54 | 0.579 ± 0.290 | P = 0.024 |
| Negative | 26 | 0.282 ± 0.314 | |
| Serosal invasion | |||
| Positive | 59 | 0.567 ± 0.268 | P = 0.219 |
| Negative | 21 | 0.390 ± 0.330 |
DISCUSSION
In the 1970’s, Folkman first found that tumor growth and metastasis were dependent on intratumoral angiogenesis. Since then, a large number of studies have emphasized the angiogenesis of tumors, but the roles of lymphatic vessels in tumor growth and metastasis were neglected. However, it is well known that lymphatic metastasis is mainly responsible for the spread of epithelial malignant tumors, and its metastasis degree is closely related to the prognosis of patients. Consisting of simple endothelium, without tight junction, and incomplete, even defect of basic membrane, accordingly, the permeability of small lymphatic vessels is larger than that of small blood vessels, and it is beneficial to tumor metastasis. However, up to now, it is still controversial about intratumoral lymphangiogenesis, mechanism of lymphangiogenesis and relationship between lymphangiogenesis and tumor metastasis.
VEGF-C family is a group of highly conservative secreted glycoproteins, which regulate vasculogenesis, lymphangiogenesis, and vascular permeability, and have been implicated in many physiological and pathological processes[6-8]. VEGF-C is a member of the VEGF family, its encoding gene is located in 4q34, VEGF-C has 7 extrons and shares 30% autologousity with VEGF. The studies showed that VEGF-C expressed in normal placenta, ovary, small intestine, skeleton muscle, spleen, colon, etc.[9-12].
VEGFR-3/FLT-4, which belongs to the platelet-derived growth factor for receptor subfamily of receptor tyrosine kinase, was extensively expressed in embryonic tissues[13-16]. In adult however, VEGFR-3/FLT-4 was mainly expressed in lymphatic endothelia, so it was regarded as a special marker of lymphatic endothelia. The density and distribution of lymphatic vessels could be detected by VEGFR-3/FLT-4 antibody[17-21].
Recent studies showed that, the binding of VEGF-C to its special receptor FLT-4, could induce tyrosine phosphorylation of receptors, activate MAPK via intracellular kinase reaction, and finally promote proliferation of lymphatic endothelia, and lymphangiogenesis[22-25].
Karpanen’s results showed that VEGF-C could promote growth of tumor cells, which was correlated with the growth of lymphatic vessels around tumors and the intralymphatic spread of cancer[26]. Several clinical studies have proved that overexpression of VEGF-C in solide tumors, such as squamous cell carcinomas of head and neck, thyroid carcinoma, prostate cancer, gastric cancer, colorectal carcinoma, breast cancer, esophageal squamous carcinoma, cervical cancer, lung cancer, was relevant to lymphatic spread[27-31].
Akagi[32] examined the relationship between expression of VEGF-C in 99 primary tumors and 18 metastatic lymph nodes from colorectal cancer and clinicopathological features by semi-quantitative reverse transcriptase-polymerase chain reaction (RT-PCR) and immumohistochemistry. The results showed that the expression of VEGF-C was correlated with lymphatic involvement, lymph node metastasis, and depth of invasion. To study the correlation between lymphogenous metastasis in early gastric carcinoma (EGC) and the expression of VEGF-C, Kabashima[33] selected 35 cases of lymph node metastasis-positive [n(+)] EGC and 70 cases of lymph node metastasis-negative [n(-)] EGC. Clinicopathologically, there were significant differences in median size, lymphatic invasion, and venous invasion between the two groups, the incidence of positive-expression of VEGF-C in n(+) EGC was significantly higher than that in n(-) EGC. In breast cancer, the expression of VEGF-C was correlated with lymphatic vessel invasion, the 5-year disease free survival rate of the VEGF-C positive group was significantly poorer than that of the VEGF-C negative group[34]. The expression of VEGF-C in breast cancer cells could increase intratumoral lymphangiogenesis, resulting in significantly enhanced metastasis to regional lymph nodes and lungs, and the degree of tumor lymphangiogenesis was highly correlated with the extent of lymph node and lung metastases[35].
Most of the studies demonstrated that VEGF-C was mainly produced by cancer cells, and VEGFR-3/FLT-4 by endothelial cells of the stromal lymphatic vessels, the incidence of VEGF-C was closely correlated with VEGFR-3/FLT-4 expression in the primary tumors. VEGF-C produced by cancer cells might induce the expression of VEGFR-3/FLT-4 on lymphatic endothelial cells, consequently, the activation of VEGF-C/FLT-4 paracrine loop induced the lymphangiogenesis[36].
However, the study by Gumingham[37] obtained opposite results, in which a significant correlation was found between expression of VEGF-C and VEGFR-3/FLT-4 in breast cancer, but no significant difference in VEGF-C expression between normal and neoplastic breast tissues and no association between VEGF-C and either lymph node status or number of involved nodes, patient age, tumor size, estrogen receptor status, or tumor grade were found.
We studied the correlation between VEGF-C and VEGFR-3/FLT-4 expression in 80 primary gastric cancers and adjacent normal tissues by semi-quantitative reverse transcriptase-polymerase chain reaction (RT-PCR) and immumohistochemistry. The results showed that there was a significant difference in VEGF-C expression between primary tumor and adjacent normal tissue samples, and a significant correlation between expression of VEGF-C and VEGFR-3/FLT-4 in tumor tissues. The present study also clearly demonstrated that expression of VEGF-C and VEGFR-3/FLT-4 was closely related to the histological type of tumors and lymph node metastasis. Expressions of VEGF-C and VEGFR-3/FLT-4 were detected both in primary gastric cancer and in adjacent normal tissues. However, the former was significantly higher than the latter. Meanwhile, VEGFR-3/FLT-4 expression was detected in endothelial cells of stromal blood vessels and lymphatic vessels.
Tumor cell metastasis to regional lymph nodes is an early event in tumor spread, and this index is frequently used to predict disease prognosis[38]. VEGF-C is the first growth factor related to lymphangiogenesis, and the study of lymphangiogenesis of tumors is only at its beginning. Its mechanisms and mediators await further studies.
Footnotes
Edited by Ma JY and Wang XL
References
- 1.Gershenwald JE, Fidler IJ. Cancer. Targeting lymphatic metastasis. Science. 2002;296:1811–1812. doi: 10.1126/science.10731318. [DOI] [PubMed] [Google Scholar]
- 2.Karkkainen MJ, Petrova TV. Vascular endothelial growth factor receptors in the regulation of angiogenesis and lymphangiogenesis. Oncogene. 2000;19:5598–5605. doi: 10.1038/sj.onc.1203855. [DOI] [PubMed] [Google Scholar]
- 3.Parr C, Jiang WG. Quantitative analysis of lymphangiogenic markers in human colorectal cancer. Int J Oncol. 2003;23:533–539. doi: 10.3892/ijo.23.2.533. [DOI] [PubMed] [Google Scholar]
- 4.Arinaga M, Noguchi T, Takeno S, Chujo M, Miura T, Uchida Y. Clinical significance of vascular endothelial growth factor C and vascular endothelial growth factor receptor 3 in patients with nonsmall cell lung carcinoma. Cancer. 2003;97:457–464. doi: 10.1002/cncr.11073. [DOI] [PubMed] [Google Scholar]
- 5.Kishimoto K, Sasaki A, Yoshihama Y, Mese H, Tsukamoto G, Matsumura T. Expression of vascular endothelial growth factor-C predicts regional lymph node metastasis in early oral squamous cell carcinoma. Oral Oncol. 2003;39:391–396. doi: 10.1016/s1368-8375(02)00143-4. [DOI] [PubMed] [Google Scholar]
- 6.Pepper MS. Lymphangiogenesis and tumor metastasis: myth or reality. Clin Cancer Res. 2001;7:462–468. [PubMed] [Google Scholar]
- 7.Cao Y, Linden P, Farnebo J, Cao R, Eriksson A, Kumar V, Qi JH, Claesson-Welsh L, Alitalo K. Vascular endothelial growth factor C induces angiogenesis in vivo. Proc Natl Acad Sci USA. 1998;95:14389–14394. doi: 10.1073/pnas.95.24.14389. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Enholm B, Paavonen K, Ristimäki A, Kumar V, Gunji Y, Klefstrom J, Kivinen L, Laiho M, Olofsson B, Joukov V, et al. Comparison of VEGF, VEGF-B, VEGF-C and Ang-1 mRNA regulation by serum, growth factors, oncoproteins and hypoxia. Oncogene. 1997;14:2475–2483. doi: 10.1038/sj.onc.1201090. [DOI] [PubMed] [Google Scholar]
- 9.Lee J, Gray A, Yuan J, Luoh SM, Avraham H, Wood WI. Vascular endothelial growth factor-related protein: a ligand and specific activator of the tyrosine kinase receptor Flt4. Proc Natl Acad Sci USA. 1996;93:1988–1992. doi: 10.1073/pnas.93.5.1988. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Laitinen M, Ristimäki A, Honkasalo M, Narko K, Paavonen K, Ritvos O. Differential hormonal regulation of vascular endothelial growth factors VEGF, VEGF-B, and VEGF-C messenger ribonucleic acid levels in cultured human granulosa-luteal cells. Endocrinology. 1997;138:4748–4756. doi: 10.1210/endo.138.11.5500. [DOI] [PubMed] [Google Scholar]
- 11.Ohta Y, Shridhar V, Bright RK, Kalemkerian GP, Du W, Carbone M, Watanabe Y, Pass HI. VEGF and VEGF type C play an important role in angiogenesis and lymphangiogenesis in human malignant mesothelioma tumours. Br J Cancer. 1999;81:54–61. doi: 10.1038/sj.bjc.6690650. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Boardman KC, Swartz MA. Interstitial flow as a guide for lymphangiogenesis. Circ Res. 2003;92:801–808. doi: 10.1161/01.RES.0000065621.69843.49. [DOI] [PubMed] [Google Scholar]
- 13.Pajusola K, Aprelikova O, Korhonen J, Kaipainen A, Pertovaara L, Alitalo R, Alitalo K. FLT4 receptor tyrosine kinase contains seven immunoglobulin-like loops and is expressed in multiple human tissues and cell lines. Cancer Res. 1992;52:5738–5743. [PubMed] [Google Scholar]
- 14.Lymboussaki A, Partanen TA, Olofsson B, Thomas-Crusells J, Fletcher CD, de Waal RM, Kaipainen A, Alitalo K. Expression of the vascular endothelial growth factor C receptor VEGFR-3 in lymphatic endothelium of the skin and in vascular tumors. Am J Pathol. 1998;153:395–403. doi: 10.1016/S0002-9440(10)65583-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Salven P, Mustjoki S, Alitalo R, Alitalo K, Rafii S. VEGFR-3 and CD133 identify a population of CD34+ lymphatic/vascular endothelial precursor cells. Blood. 2003;101:168–172. doi: 10.1182/blood-2002-03-0755. [DOI] [PubMed] [Google Scholar]
- 16.Hamrah P, Chen L, Zhang Q, Dana MR. Novel expression of vascular endothelial growth factor receptor (VEGFR)-3 and VEGF-C on corneal dendritic cells. Am J Pathol. 2003;163:57–68. doi: 10.1016/S0002-9440(10)63630-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Clarijs R, Schalkwijk L, Hofmann UB, Ruiter DJ, de Waal RM. Induction of vascular endothelial growth factor receptor-3 expression on tumor microvasculature as a new progression marker in human cutaneous melanoma. Cancer Res. 2002;62:7059–7065. [PubMed] [Google Scholar]
- 18.Jussila L, Valtola R, Partanen TA, Salven P, Heikkilä P, Matikainen MT, Renkonen R, Kaipainen A, Detmar M, Tschachler E, et al. Lymphatic endothelium and Kaposi's sarcoma spindle cells detected by antibodies against the vascular endothelial growth factor receptor-3. Cancer Res. 1998;58:1599–1604. [PubMed] [Google Scholar]
- 19.Valtola R, Salven P, Heikkilä P, Taipale J, Joensuu H, Rehn M, Pihlajaniemi T, Weich H, deWaal R, Alitalo K. VEGFR-3 and its ligand VEGF-C are associated with angiogenesis in breast cancer. Am J Pathol. 1999;154:1381–1390. doi: 10.1016/S0002-9440(10)65392-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Kaipainen A, Korhonen J, Mustonen T, van Hinsbergh VW, Fang GH, Dumont D, Breitman M, Alitalo K. Expression of the fms-like tyrosine kinase 4 gene becomes restricted to lymphatic endothelium during development. Proc Natl Acad Sci USA. 1995;92:3566–3570. doi: 10.1073/pnas.92.8.3566. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Lymboussaki A, Olofsson B, Eriksson U, Alitalo K. Vascular endothelial growth factor (VEGF) and VEGF-C show overlapping binding sites in embryonic endothelia and distinct sites in differentiated adult endothelia. Circ Res. 1999;85:992–999. doi: 10.1161/01.res.85.11.992. [DOI] [PubMed] [Google Scholar]
- 22.Kawakami M, Furuhata T, Kimura Y, Yamaguchi K, Hata F, Sasaki K, Hirata K. Quantification of vascular endothelial growth factor-C and its receptor-3 messenger RNA with real-time quantitative polymerase chain reaction as a predictor of lymph node metastasis in human colorectal cancer. Surgery. 2003;133:300–308. doi: 10.1067/msy.2003.45. [DOI] [PubMed] [Google Scholar]
- 23.Kubo H, Cao R, Brakenhielm E, Mäkinen T, Cao Y, Alitalo K. Blockade of vascular endothelial growth factor receptor-3 signaling inhibits fibroblast growth factor-2-induced lymphangiogenesis in mouse cornea. Proc Natl Acad Sci USA. 2002;99:8868–8873. doi: 10.1073/pnas.062040199. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Dias S, Choy M, Alitalo K, Rafii S. Vascular endothelial growth factor (VEGF)-C signaling through FLT-4 (VEGFR-3) mediates leukemic cell proliferation, survival, and resistance to chemotherapy. Blood. 2002;99:2179–2184. doi: 10.1182/blood.v99.6.2179. [DOI] [PubMed] [Google Scholar]
- 25.Karkkainen MJ, Saaristo A, Jussila L, Karila KA, Lawrence EC, Pajusola K, Bueler H, Eichmann A, Kauppinen R, Kettunen MI, et al. A model for gene therapy of human hereditary lymphedema. Proc Natl Acad Sci USA. 2001;98:12677–12682. doi: 10.1073/pnas.221449198. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Karpanen T, Egeblad M, Karkkainen MJ, Kubo H, Ylä-Herttuala S, Jäättelä M, Alitalo K. Vascular endothelial growth factor C promotes tumor lymphangiogenesis and intralymphatic tumor growth. Cancer Res. 2001;61:1786–1790. [PubMed] [Google Scholar]
- 27.Neuchrist C, Erovic BM, Handisurya A, Fischer MB, Steiner GE, Hollemann D, Gedlicka C, Saaristo A, Burian M. Vascular endothelial growth factor C and vascular endothelial growth factor receptor 3 expression in squamous cell carcinomas of the head and neck. Head Neck. 2003;25:464–474. doi: 10.1002/hed.10235. [DOI] [PubMed] [Google Scholar]
- 28.Ishikawa M, Kitayama J, Kazama S, Nagawa H. Expression of vascular endothelial growth factor C and D (VEGF-C and -D) is an important risk factor for lymphatic metastasis in undifferentiated early gastric carcinoma. Jpn J Clin Oncol. 2003;33:21–27. doi: 10.1093/jjco/hyg008. [DOI] [PubMed] [Google Scholar]
- 29.Tsurusaki T, Kanda S, Sakai H, Kanetake H, Saito Y, Alitalo K, Koji T. Vascular endothelial growth factor-C expression in human prostatic carcinoma and its relationship to lymph node metastasis. Br J Cancer. 1999;80:309–313. doi: 10.1038/sj.bjc.6690356. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Kitadai Y, Amioka T, Haruma K, Tanaka S, Yoshihara M, Sumii K, Matsutani N, Yasui W, Chayama K. Clinicopathological significance of vascular endothelial growth factor (VEGF)-C in human esophageal squamous cell carcinomas. Int J Cancer. 2001;93:662–666. doi: 10.1002/ijc.1379. [DOI] [PubMed] [Google Scholar]
- 31.Hashimoto I, Kodama J, Seki N, Hongo A, Yoshinouchi M, Okuda H, Kudo T. Vascular endothelial growth factor-C expression and its relationship to pelvic lymph node status in invasive cervical cancer. Br J Cancer. 2001;85:93–97. doi: 10.1054/bjoc.2001.1846. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Akagi K, Ikeda Y, Miyazaki M, Abe T, Kinoshita J, Maehara Y, Sugimachi K. Vascular endothelial growth factor-C (VEGF-C) expression in human colorectal cancer tissues. Br J Cancer. 2000;83:887–891. doi: 10.1054/bjoc.2000.1396. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Kabashima A, Maehara Y, Kakeji Y, Sugimachi K. Overexpression of vascular endothelial growth factor C is related to lymphogenous metastasis in early gastric carcinoma. Oncology. 2001;60:146–150. doi: 10.1159/000055312. [DOI] [PubMed] [Google Scholar]
- 34.Kinoshita J, Kitamura K, Kabashima A, Saeki H, Tanaka S, Sugimachi K. Clinical significance of vascular endothelial growth factor-C (VEGF-C) in breast cancer. Breast Cancer Res Treat. 2001;66:159–164. doi: 10.1023/a:1010692132669. [DOI] [PubMed] [Google Scholar]
- 35.Skobe M, Hawighorst T, Jackson DG, Prevo R, Janes L, Velasco P, Riccardi L, Alitalo K, Claffey K, Detmar M. Induction of tumor lymphangiogenesis by VEGF-C promotes breast cancer metastasis. Nat Med. 2001;7:192–198. doi: 10.1038/84643. [DOI] [PubMed] [Google Scholar]
- 36.Yonemura Y, Fushida S, Bando E, Kinoshita K, Miwa K, Endo Y, Sugiyama K, Partanen T, Yamamoto H, Sasaki T. Lymphangiogenesis and the vascular endothelial growth factor receptor (VEGFR)-3 in gastric cancer. Eur J Cancer. 2001;37:918–923. doi: 10.1016/s0959-8049(01)00015-6. [DOI] [PubMed] [Google Scholar]
- 37.Gunningham SP, Currie MJ, Han C, Robinson BA, Scott PA, Harris AL, Fox SB. The short form of the alternatively spliced flt-4 but not its ligand vascular endothelial growth factor C is related to lymph node metastasis in human breast cancers. Clin Cancer Res. 2000;6:4278–4286. [PubMed] [Google Scholar]
- 38.Yin T, Ji XL, Shen MS. Relationship between lymph node sinuses with blood and lymphatic metastasis of gastric cancer. World J Gastroenterol. 2003;9:40–43. doi: 10.3748/wjg.v9.i1.40. [DOI] [PMC free article] [PubMed] [Google Scholar]


