Abstract
AIM: To evaluate whether pyrrolidine dithiocarbamate (PDTC), an enhancer of HO production, attenuates intestinal IR injury.
METHODS: Eighteen male rats were randomly allocated into three groups: (a) sham; (b) IR, consisting of 30 min of intestinal ischemia, followed by 2-h period of reperfusion; and (c) PDTC treatment before IR. Intestinal microvascular perfusion (IMP) was monitored continuously by laser Doppler flowmetry. At the end of the reperfusion, serum samples for lactate dehydrogenase (LDH) levels and biopsies of ileum were obtained. HO activity in the ileum was assessed at the end of the reperfusion period.
RESULTS: At the end of the reperfusion in the IR group, IMP recovered partially to 42.5% of baseline (P<0.05 vs sham), whereas PDTC improved IMP to 67.3% of baseline (P<0.01 vs IR). There was a twofold increase in HO activity in PDTC group (2 062.66±106.11) as compared to IR (842.3±85.12) (P<0.001). LDH was significantly reduced (P<0.001) in PDTC group (585.6±102.4) as compared to IR group (1 973.8±306.5). Histological examination showed that the ileal mucosa was significantly less injured in PDTC group as compared with IR group.
CONCLUSION: Our study demonstrates that PDTC improves the IMP and attenuates IR injury of the intestine possibly via HO production. Additional studies are warranted to evaluate the clinical efficacy of PDTC in the prevention of IR injury of the small intestine.
Keywords: Intestine, Ischemia-reperfusion injury, Heme oxygenase, Pyrrolidine
INTRODUCTION
Intestinal ischemia and subsequent reperfusion (IR) injury is encountered in a variety of clinical conditions, including hypovolemic shock[1], strangulation obstruction[2], cardiovascular surgery[3], abdominal aortic surgery[4], and small bowel transplantation[5]. The attenuation of IR injury is vital for intestinal graft function and survival after small bowel transplantation[6]. IR injury is associated with the breakdown of microvascular perfusion with subsequent impairment of tissue oxygenation[7]. The maintenance of microvascular perfusion is the ultimate determinant of viability of an organ[8]. IR injury of the intestine is a systemic phenomenon resulting in bacterial translocation[9], endotoxemia[10], acute respiratory distress syndrome[11], acute hepatic injury[12], which may eventually lead to multiple organ dysfunction syndrome[13].
Therapeutic strategies aimed at ameliorating IR injury have focused both on preventing the effects of reactive oxygen species and on downregulating the signal transduction cascades related to the expression of pro-inflammatory genes. Pharmacologic preconditioning based on enhancing the production or activity of endogenous protective molecules has also been proposed as an alternative therapeutic intervention. Among such agents, pyrrolidine dithiocarbamate (PDTC) has a variety of biochemical activities, such as redox state alternation, chelation of heavy metals, and enzyme inhibition[14]. PDTC was initially regarded as a potent inhibitor of nuclear factor-kappa B (NF-κB) and used as an antioxidant compound to counteract the toxic effects of free radicals[15]. PDTC is one of the most effective inducers of heme oxygenase-1 (HO-1), which also confers cytoprotection against oxidative stress[16]. HO is the rate-limiting enzyme in the conversion of heme into carbon monoxide (CO), biliverdin (which is rapidly converted to bilirubin) and free iron (Fe2+)[17]. Three isoforms of HO have so far been identified: inducible HO-1; constitutively expressed HO-2; and HO-3 which is related to HO-2, but is less well characterized[17]. The HO system is thought to play a pivotal role in the maintenance of antioxidant and oxidant homeostasis during cellular injury. The HO system exerts four major beneficial effects broadly: (a) antioxidant function; (b) maintenance of the microcirculation; (c) anti-apoptosis; and (d) anti-inflammatory function[17]. The antioxidant function relies on heme degradation, production of bilirubin[18], and the formation of ferritin via Fe2+[19]. The production of CO with its vasodilatory and anti-platelet properties maintains the microcirculation and may be involved in anti-apoptotic and cell arrest mechanisms. The HO system exerts anti-inflammatory effects via the modulation of endothelial adhesion molecules.
To the best of our knowledge, there are no previous studies exploring the effect of PDTC on IR injury of the intestine. Therefore, we have designed the present study to examine whether PDTC preconditioning induces HO expression in the small intestine and reduces the inflammatory response during reperfusion by focusing on the intestinal microvascular perfusion.
MATERIALS AND METHODS
Animals
Male Sprague-Dawley rats, weighing 250-300 g, were used in this study. Rats were kept in a temperature-controlled environment with 12-h light-dark cycle and allowed tap water and standard rat chow pellets ad libitum. Animal care and experimental protocols were performed in accordance with the UK Government Guidance in the Operation of the Animals (Scientific Procedures) Act 1986.
Surgical procedures
Animals were anaesthetized using isoflurane (Baxter, Norfolk, UK) and allowed to breathe spontaneously via concentric mask connected to an oxygen regulator. The animal’s body temperature was maintained at 36-38 oC using a heating pad (Harvard Apparatus Ltd, Kent, UK) and monitored with a rectal temperature probe. The arterial oxygen saturation (SaO2) and heart rate (HR) were continuously monitored with a pulse oximeter (Ohmeda Biox 3740 pulse oximeter, Ohmeda Louisville Co., USA). The left carotid artery was cannulated with a polyethylene catheter (0.76 mm inner diameter, Portex, Kent, UK) and connected to a pressure transducer for the monitoring of mean arterial blood pressure (MABP). The right jugular vein was cannulated with a smaller polyethylene catheter (0.40 mm inner diameter, Portex, Kent, UK) for the administration of normal saline (1 mL/100 g body weight/h) to compensate for intra-operative fluid evaporation. All animals had an intravenous bolus of heparin (20 U/kg) to prevent potential thrombus formation in the ischemic segment of the intestine due to hemostasis.
Laparotomy was carried out through a midline incision. The superior mesenteric artery (SMA) was identified and dissected out from the mesentery to enable the passage of a 4/0 vicryl (Ethicon, Edinburgh, UK) suture loop. The SMA was occluded according to the method described by Arumugam et al[20]. The free ends of the vicryl suture were then passed through a 5-cm segment of polyethylene tube (1.4 mm inner diameter). The tube was then gently advanced over the suture onto the mesentery and fixed in place with a hemostat. Reperfusion started when the hemostat was released. The animal’s abdomen was covered with a plastic wrap (Saran wrap) to prevent fluid evaporation. At the end of the experiment, the animals were killed by exsanguination.
Experimental design
Rats were randomly allocated to three study groups (n = 6/group). Group 1: sham laparotomy, the SMA was identified and passage of vicryl suture was performed, but without vascular occlusion. Group 2: IR, the SMA was clamped for 30 min, followed by a 2-h period of reperfusion. Group 3: PDTC+IR, the animals received intramuscularly a single dose of 100 mg/kg of PDTC (Sigma Chemical Co., St. Louis, MO, USA) 30 min before IR.
Measurement of intestinal microvascular perfusion
Intestinal microvascular perfusion was measured by a surface laser Doppler flowmeter (LDF, DRT4, Moor Instruments Limited, Axminster, UK) in flux units. The Doppler signal varies linearly with the product of the total number of moving red blood cells in the measured volume of a few cubic millimeter multiplied by the mean velocity of these red blood cells. The numeric product is termed as perfusion units or blood cell flux units. LDF has been validated as a method for measuring gastrointestinal microvascular blood flow in animal models[21] and in clinical studies[22]. The LDF probe was placed on a fixed site on the serosa of the ileum and was held in place by a probe holder. Serosal blood flow has previously been shown to correlate well with mucosal flow[23].
Heme oxygenase assay
HO activity in ileal microsomal fractions was measured using a spectrophotometric assay of bilirubin production according to the method previously described by Motterlini et al[24]. Briefly, tissue microsomes were added to the following mixture: MgCl2 (2 mmol/L), phosphate-buffered saline (100 mmol/L, pH 7.4; Sigma, UK), rat liver cytosol as a source of biliverdin reductase (3 mg of total protein), hemin (10 µmol/L; Sigma, UK), glucose-6-phosphate (2 mmol/L; Sigma, UK), glucose-6-phosphate dehydrogenase (0.2 U; Sigma, UK) and NADPH (0.8 mmol/L; Sigma, UK). The reaction was conducted in the dark for 30 min at 37 °C and terminated by the addition of chloroform (Sigma, UK). The amount of the extracted bilirubin was calculated by the difference in absorption between 464 and 530 nm and an extinction coefficient of 40 mmol/L/cm was used for bilirubin. The total protein content of the samples was determined using a colorimetric assay according to the manufacturer’s instructions (Bio-Rad, UK), and bovine gamma globulin was used as a standard.
Biochemical assays
Blood samples were taken at the end of the experiments from the carotid artery. The blood samples were centrifuged at 2 000 g for 10 min at room temperature to sediment the erythrocytes. The serum was removed and analyzed on a Hitachi 747 auto-analyzer (Hitachi Ltd, Tokyo, Japan) by using commercially available enzymatic kits (Boehringer Mannheim Ltd, East Sussex, UK) for lactate dehydrogenase (LDH), aspartate aminotransferase (AST) and alanine aminotransferase (ALT).
Histological investigation
At the end of the experiment, tissue samples of ileum were taken, fixed in 10% neutral buffered formalin and embedded in paraffin, and 4-μm-thick sections were cut using a microtome and mounted on slides for hematoxylin and eosin staining. Ileal injury was assessed using a scoring system devised by Chiu et al[25] under light microscopy without the knowledge of study groups.
Data collection and statistical analysis
Data from the pulse oximeter, pressure transducer and LDF were fed into a laptop computer and collected continuously at a sampling rate of 2 Hz. The data were calculated as 1-min averages at baseline and every 30 min till the end of the experiment. All values are expressed as mean±SE. ANOVA and Bonferroni adjustment for multiple comparisons were used unless otherwise stated, where unpaired Student’s t-test was used for statistical analysis between groups. P<0.05 was considered statistically significant.
RESULTS
Systemic hemodynamic parameters
In all the animals in the experimental groups, the HR and the SaO2 did not change significantly throughout the experiment (Table 1). In the sham group, MABP did not change significantly throughout the experiment. However, during ischemia, there was a transient increase in MABP from the baseline values in both IR (11.97±0.53 to 14.50±0.67 KPa, P<0.01) and PDTC groups (11.70±0.67 to 14.23±1.33 KPa, P<0.01). However, the MABP did not change significantly during the reperfusion period between the three groups (Table 1).
Table 1.
Systemic hemodynamic parameters in three experimental groups at baseline, 5 min before, at the end of 30 min ischemia and at 1 and 2 h post-reperfusion
| Hemodynamic | Baseline | End of ischemia | 1 h of reperfusion | 2 h of reperfusion | P values |
| parameters | |||||
| Heart rate (BPM) | |||||
| Sham | 250±5 | 252±3 | 240±8 | 230±10 | >0.05 |
| IR | 251±2 | 252±2 | 220±4 | 227±12 | >0.05 |
| PDTC | 252±3 | 251±3 | 240±10 | 232±7 | >0.05 |
| SaO2 (%) | |||||
| Sham | 98±2 | 95±2 | 94±3 | 95±2 | >0.05 |
| IR | 98±1 | 95±2 | 97±2 | 95±3 | >0.05 |
| PDTC | 98±1 | 96±3 | 93±1 | 96±3 | >0.05 |
| MABP (mmHg) | |||||
| Sham | 83±6 | 76± 5 | 74±6 | 78±8 | >0.05 |
| IR | 90±3 | 108±5b | 81±3 | 72±5 | <0.01 |
| PDTC | 87±5 | 107±5b | 79±4 | 73±6 | <0.01 |
Values are expressed as mean±SE of six animals in each group. SaO2: arterial oxygen saturation; MABP: mean arterial blood pressure.
P<0.01 vs baseline.
Intestinal microvascular perfusion
IMP did not alter significantly during the course of the experiment in the sham group. There were significant differences between IR and PDTC groups in IMP at 30 min of reperfusion (46.7±2.8% in IR vs 67.3±6.2% in PDTC, P<0.01). The increase in IMP persisted till the end of the 2-h reperfusion period (42.5±2.8% in IR vs 69.1±4.5% in PDTC, P<0.01) (Figure 1).
Figure 1.
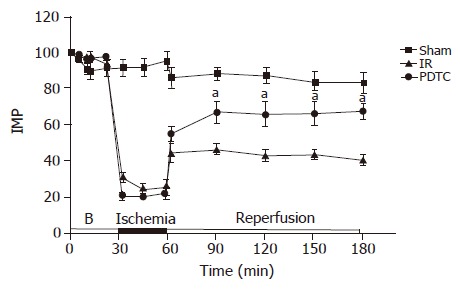
Intestinal microvascular perfusion in (% of baseline) during 30 min of ischemia and 2 h of reperfusion measured by L-DF. Values are expressed as mean±SE of six animals in each group (aP<0.05 vs IR). B: Baseline.
HO activity assay
The mean HO activity in the sham group was 409.66±62.95 pmol bilirubin/(mg protein·h). PDTC led to a twofold increase in HO activity (2 085.83±158.65) as compared to IR (768.66±103.82) (P<0.001, Figure 2).
Figure 2.
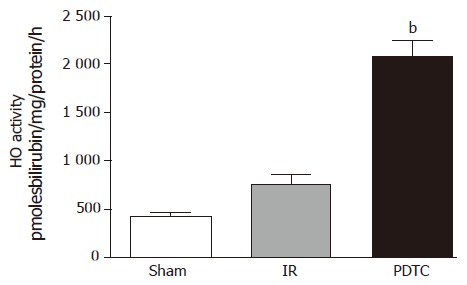
Ileal HO activity in all three experimental groups at the end of 2 h of reperfusion (bP<0.01 vs IR).
Biochemical analysis
LDH was significantly reduced in PDTC group (576.3±98.7) as compared to IR group (1 866.0±267.5) (P<0.001, Figure 3). The LDH value in sham group at the end of the reperfusion was 335.23±77.7. Significant changes were not detected in serum indicators of liver function (AST and ALT) in any of the groups (data not shown).
Figure 3.
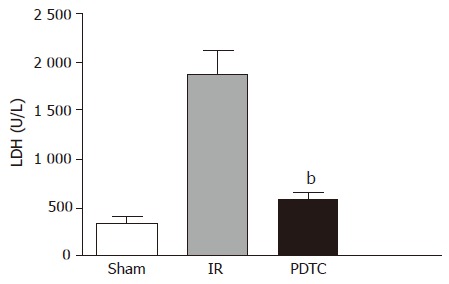
Serum LDH levels (U/L) at the end of 2 h reperfusion period. Values are expressed as mean±SE of six animals in each group. In PDTC group, LDH was significantly lower compared to the IR group (bP<0.001 vs IR).
Histological analysis
IR resulted in an increase in the histological score from a mean of 1.0±0.2 in sham-operated animals to 3±0.2. PDTC treatment improved the histological score significantly to 1.5±0.5 (P<0.01, Figures 4 and 5).
Figure 4.
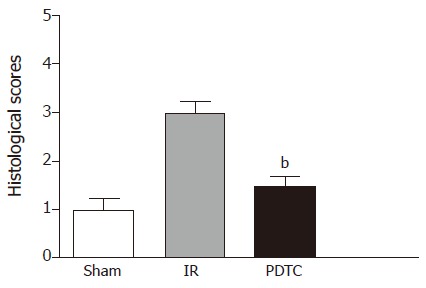
Comparison of histological scores of ileal mucosa between three experimental groups (bP<0.01 vs IR).
Figure 5.
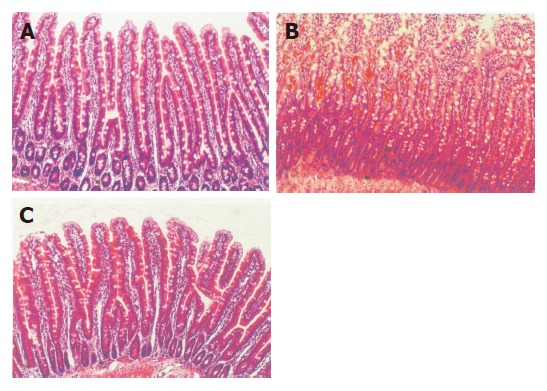
Representative photomicrographs of histological sections of ileum (a) in sham operated animals, (b) subjected to 30-min period of ischemia and 2-h period of reperfusion (IR) and (c) subjected to PDTC+IR (H&E, original magnification ×100).
DISCUSSION
The present study clearly showed that PDTC improved the small bowel microvascular perfusion and increased HO activity, while ameliorating IR injury. Serum LDH levels, which is used as a marker for intestinal injury[6], reflected intestinal damage in IR group, whereas PDTC decreased these levels. IR injury resulted in villous and crypt damage, which attributed to hemorrhage and necrosis, whereas PDTC ameliorated this effect. These results suggest that PDTC protects small bowel from IR injury possibly via HO production.
The model of 30-min period of SMA occlusion with 2-h reperfusion was reliable with no procedure-related mortality, suggesting that 30 min of intestinal ischemia is non-lethal but induces substantial intestinal injury. A considerable number of experimental studies have indicated that IR injury of the intestine occurs in a biphasic manner characterized by different time frames and mechanisms: (a) an early phase that immediately follows the ischemia and lasts for 2-3 h; and (b) a late phase which begins 12-24 h from the ischemia and lasts for about 3-4 d[13]. Hence, a period of 2 h of reperfusion following ischemia was chosen to assess the changes in the early phase of reperfusion injury. One of the effective approaches for attenuating IR injury is to induce endogenous antioxidant genes, such as HO-1.
PDTC has been shown to be a potent inducer of HO-1 in many experimental models[16,14]. Whereas increasing evidences suggest that HO-1 induction may mediate cellular protection against oxidant injury in both in vitro and in vivo models, the role of HO in the intestinal microcirculation is poorly understood. In this study, the effects of PDTC on IR-induced intestinal microcirculatory changes were studied by continuously measuring intestinal blood flow with LDF, which has been used extensively in both animals and human beings[22]. It is non-invasive, safe, and easy to use[23]. This technique allows repeated measurements of blood flow without access to venous or arterial blood. In our study, the comparison of IMP between the groups at different time points showed that PDTC increased the IMP in the initial 30 min of reperfusion, suggesting that the mechanism of pharmacologic preconditioning by PDTC modulating flow in the microcirculation is an immediate phenomenon. Therefore, the effect of PDTC is likely to involve modulation of immediate microcirculatory events at the level of capillaries and postcapillary venules, because these are the primary sites of microcirculatory failure induced by IR injury.
The results of the present study clearly demonstrated that PDTC induced maintenance of adequate microvascular perfusion in vivo, and indicated that this protective effect might be mediated through the action of HO, which catalyzes the conversion of heme to CO, biliverdin and free iron. CO and its action on capillary pericytes may play a major role in this protection. It is well known that capillaries are associated abluminally with pericytes which protrude primary cytoplasmic processes running along the axes of the capillaries[26]. From these primary processes, lateral processes arise, which completely encircle the capillaries and form tight connections to the endothelial cells[26]. These pericytes contain muscle cytoskeletal proteins, in particular alpha-smooth muscle actin, which regulate microvascular blood flow[27]. In the liver, Ito cells, which are the sinusoids-associated pericytes, are primarily responsible for CO-mediated regulation in sinusoidal blood flow[28]. In addition, there is an increasing evidence that CO inhibits the aggregation of platelets[29], which could result in highly improved microvascular perfusion because of unhindered flow. Hence, tissue viability increases because of improved nutritional supply and better elimination of toxic residues of oxidative stress. Recently, Nakao et al[30] demonstrated that inhalation of CO ameliorates IR injury in a model of bowel transplantation.
Biliverdin is subjected to further degradation to bilirubin by the cytosolic enzyme biliverdin reductase[31]. It acts as an antioxidant and is capable of scavenging oxygen free radicals that are thought to be primarily responsible for the tissue injury[18]. Iron, the last product of heme breakdown, acts as an oxidant like other transition metals and catalyzes the formation of reactive hydroxyl radicals (OH) by the Haber-Weiss reaction. Typically, the OH· causes biological damage by stimulating the free chain reaction known as lipid peroxidation, in which OH· attacks the fatty acid side chains of the membrane phospholipids and causes organelle and cell disruption[32]. Therefore, it seems to be of paramount importance to eliminate free iron from the tissue in order to maintain the cellular integrity after the stress event. To enable this process, an additional expression of ferritin, the iron-binding protein, is induced simultaneously by HO[33].
In summary, this study has demonstrated that intestinal IR injury induces rapid microcirculatory breakdown with tissue damage. Administration of PDTC maintains the intestinal microvascular blood flow and markedly attenuates the IR injury. PDTC may be of particular value in preventing IR injury to the small intestine and might help to improve the results of small bowel transplantation. Intestinal IR injury is also an obligatory component of numerous surgical procedures. The results of the present study may, therefore, prove beneficial in many areas of clinical research. Further studies are clearly warranted to evaluate the clinical efficacy of PDTC in the prevention of IR injury of the small intestine.
Footnotes
Science Editor Kumar M and Guo SY Language Editor Elsevier HK
References
- 1.Kong SE, Blennerhassett LR, Heel KA, McCauley RD, Hall JC. Ischaemia-reperfusion injury to the intestine. Aust N Z J Surg. 1998;68:554–561. doi: 10.1111/j.1445-2197.1998.tb02099.x. [DOI] [PubMed] [Google Scholar]
- 2.Akcakaya A, Alimoglu O, Sahin M, Abbasoglu SD. Ischemia-reperfusion injury following superior mesenteric artery occlusion and strangulation obstruction. J Surg Res. 2002;108:39–43. doi: 10.1006/jsre.2002.6528. [DOI] [PubMed] [Google Scholar]
- 3.Ghosh S, Roberts N, Firmin RK, Jameson J, Spyt TJ. Risk factors for intestinal ischaemia in cardiac surgical patients. Eur J Cardiothorac Surg. 2002;21:411–416. doi: 10.1016/s1010-7940(02)00015-5. [DOI] [PubMed] [Google Scholar]
- 4.Reber PU, Peter M, Patel AG, Stauffer E, Printzen G, Mettler D, Hakki H, Kniemeyer HW. Ischaemia/reperfusion contributes to colonic injury following experimental aortic surgery. Eur J Vasc Endovasc Surg. 2001;21:35–39. doi: 10.1053/ejvs.2000.1264. [DOI] [PubMed] [Google Scholar]
- 5.Kimizuka K, Nakao A, Nalesnik MA, Demetris AJ, Uchiyama T, Ruppert K, Fink MP, Stolz DB, Murase N. Exogenous IL-6 inhibits acute inflammatory responses and prevents ischemia/reperfusion injury after intestinal transplantation. Am J Transplant. 2004;4:482–494. doi: 10.1111/j.1600-6143.2004.00368.x. [DOI] [PubMed] [Google Scholar]
- 6.Sola A, De Oca J, González R, Prats N, Roselló-Catafau J, Gelpí E, Jaurrieta E, Hotter G. Protective effect of ischemic preconditioning on cold preservation and reperfusion injury associated with rat intestinal transplantation. Ann Surg. 2001;234:98–106. doi: 10.1097/00000658-200107000-00015. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Turnage RH, Kadesky KM, Bartula L, Guice KS, Oldham KT, Myers SI. Splanchnic PGI2 release and "no reflow" following intestinal reperfusion. J Surg Res. 1995;58:558–564. doi: 10.1006/jsre.1995.1088. [DOI] [PubMed] [Google Scholar]
- 8.Kaminski PM, Proctor KG. Attenuation of no-reflow phenomenon, neutrophil activation, and reperfusion injury in intestinal microcirculation by topical adenosine. Circ Res. 1989;65:426–435. doi: 10.1161/01.res.65.2.426. [DOI] [PubMed] [Google Scholar]
- 9.Fujino Y, Suzuki Y, Kakinoki K, Tanioka Y, Ku Y, Kuroda Y. Protection against experimental small intestinal ischaemia-reperfusion injury with oxygenated perfluorochemical. Br J Surg. 2003;90:1015–1020. doi: 10.1002/bjs.4138. [DOI] [PubMed] [Google Scholar]
- 10.Deitch EA. The role of intestinal barrier failure and bacterial translocation in the development of systemic infection and multiple organ failure. Arch Surg. 1990;125:403–404. doi: 10.1001/archsurg.1990.01410150125024. [DOI] [PubMed] [Google Scholar]
- 11.Turnage RH, Guice KS, Oldham KT. Pulmonary microvascular injury following intestinal reperfusion. New Horiz. 1994;2:463–475. [PubMed] [Google Scholar]
- 12.Turnage RH, Kadesky KM, Myers SI, Guice KS, Oldham KT. Hepatic hypoperfusion after intestinal reperfusion. Surgery. 1996;119:151–160. doi: 10.1016/s0039-6060(96)80163-2. [DOI] [PubMed] [Google Scholar]
- 13.Mallick IH, Yang W, Winslet MC, Seifalian AM. Ischemia-reperfusion injury of the intestine and protective strategies against injury. Dig Dis Sci. 2004;49:1359–1377. doi: 10.1023/b:ddas.0000042232.98927.91. [DOI] [PubMed] [Google Scholar]
- 14.Tsuchihashi S, Tamaki T, Tanaka M, Kawamura A, Kaizu T, Ikeda A, Kakita A. Pyrrolidine dithiocarbamate provides protection against hypothermic preservation and transplantation injury in the rat liver: the role of heme oxygenase-1. Surgery. 2003;133:556–567. doi: 10.1067/msy.2003.124. [DOI] [PubMed] [Google Scholar]
- 15.Liu SF, Ye X, Malik AB. Inhibition of NF-kappaB activation by pyrrolidine dithiocarbamate prevents In vivo expression of proinflammatory genes. Circulation. 1999;100:1330–1337. doi: 10.1161/01.cir.100.12.1330. [DOI] [PubMed] [Google Scholar]
- 16.Hartsfield CL, Alam J, Choi AM. Transcriptional regulation of the heme oxygenase 1 gene by pyrrolidine dithiocarbamate. FASEB J. 1998;12:1675–1682. doi: 10.1096/fasebj.12.15.1675. [DOI] [PubMed] [Google Scholar]
- 17.Katori M, Anselmo DM, Busuttil RW, Kupiec-Weglinski JW. A novel strategy against ischemia and reperfusion injury: cytoprotection with heme oxygenase system. Transpl Immunol. 2002;9:227–233. doi: 10.1016/s0966-3274(02)00043-6. [DOI] [PubMed] [Google Scholar]
- 18.Stocker R, Yamamoto Y, McDonagh AF, Glazer AN, Ames BN. Bilirubin is an antioxidant of possible physiological importance. Science. 1987;235:1043–1046. doi: 10.1126/science.3029864. [DOI] [PubMed] [Google Scholar]
- 19.Balla G, Jacob HS, Balla J, Rosenberg M, Nath K, Apple F, Eaton JW, Vercellotti GM. Ferritin: a cytoprotective antioxidant strategem of endothelium. J Biol Chem. 1992;267:18148–18153. [PubMed] [Google Scholar]
- 20.Arumugam TV, Shiels IA, Woodruff TM, Reid RC, Fairlie DP, Taylor SM. Protective effect of a new C5a receptor antagonist against ischemia-reperfusion injury in the rat small intestine. J Surg Res. 2002;103:260–267. doi: 10.1006/jsre.2002.6369. [DOI] [PubMed] [Google Scholar]
- 21.Shepherd AP, Riedel GL. Continuous measurement of intestinal mucosal blood flow by laser-Doppler velocimetry. Am J Physiol. 1982;242:G668–G672. doi: 10.1152/ajpgi.1982.242.6.G668. [DOI] [PubMed] [Google Scholar]
- 22.Thollander M, Hellström PM, Gazelius B. Semi-invasive laser-Doppler flowmetry technique. New application for recordings of hemodynamics in combination with manometry of human small intestine. Int J Microcirc Clin Exp. 1997;17:15–21. [PubMed] [Google Scholar]
- 23.Corbett EJ, Barry BN, Pollard SG, Lodge JP, Bellamy MC. Laser Doppler flowmetry is useful in the clinical management of small bowel transplantation. The Liver Transplant Group. Gut. 2000;47:580–583. doi: 10.1136/gut.47.4.580. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Motterlini R, Foresti R, Intaglietta M, Winslow RM. NO-mediated activation of heme oxygenase: endogenous cytoprotection against oxidative stress to endothelium. Am J Physiol. 1996;270:H107–H114. doi: 10.1152/ajpheart.1996.270.1.H107. [DOI] [PubMed] [Google Scholar]
- 25.Chiu CJ, McArdle AH, Brown R, Scott HJ, Gurd FN. Intestinal mucosal lesion in low-flow states. I. A morphological, hemodynamic, and metabolic reappraisal. Arch Surg. 1970;101:478–483. doi: 10.1001/archsurg.1970.01340280030009. [DOI] [PubMed] [Google Scholar]
- 26.Hirschi KK, D'Amore PA. Pericytes in the microvasculature. Cardiovasc Res. 1996;32:687–698. [PubMed] [Google Scholar]
- 27.Skalli O, Pelte MF, Peclet MC, Gabbiani G, Gugliotta P, Bussolati G, Ravazzola M, Orci L. Alpha-smooth muscle actin, a differentiation marker of smooth muscle cells, is present in microfilamentous bundles of pericytes. J Histochem Cytochem. 1989;37:315–321. doi: 10.1177/37.3.2918221. [DOI] [PubMed] [Google Scholar]
- 28.Suematsu M, Wakabayashi Y, Ishimura Y. Gaseous monoxides: a new class of microvascular regulator in the liver. Cardiovasc Res. 1996;32:679–686. [PubMed] [Google Scholar]
- 29.Brüne B, Ullrich V. Inhibition of platelet aggregation by carbon monoxide is mediated by activation of guanylate cyclase. Mol Pharmacol. 1987;32:497–504. [PubMed] [Google Scholar]
- 30.Nakao A, Kimizuka K, Stolz DB, Neto JS, Kaizu T, Choi AM, Uchiyama T, Zuckerbraun BS, Nalesnik MA, Otterbein LE, et al. Carbon monoxide inhalation protects rat intestinal grafts from ischemia/reperfusion injury. Am J Pathol. 2003;163:1587–1598. doi: 10.1016/S0002-9440(10)63515-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Maines MD. Heme oxygenase: function, multiplicity, regulatory mechanisms, and clinical applications. FASEB J. 1988;2:2557–2568. [PubMed] [Google Scholar]
- 32.Halliwell B. Antioxidant defence mechanisms: from the beginning to the end (of the beginning) Free Radic Res. 1999;31:261–272. doi: 10.1080/10715769900300841. [DOI] [PubMed] [Google Scholar]
- 33.Bauer M, Bauer I. Heme oxygenase-1: redox regulation and role in the hepatic response to oxidative stress. Antioxid Redox Signal. 2002;4:749–758. doi: 10.1089/152308602760598891. [DOI] [PubMed] [Google Scholar]


