Abstract
AIM: To evaluate the nature of the “learning curve” for laparoscopy-assisted distal gastrectomy (LADG) with systemic lymphadenectomy for early gastric cancer.
METHODS: The data of 90 consecutive patients with early gastric cancer who underwent LADG with systemic lymphadenectomy between April 2003 and November 2004 were reviewed. The 90 patients were divided into 9 sequential groups of 10 cases in each group and the average operative time of these 9 groups were determined. Other learning indicators, such as transfusion requirements, conversion rates to open surgery, postoperative complication, time to first flatus, and postoperative hospital stay, were evaluated.
RESULTS: After the first 10 LADGs, the operative time reached its first plateau (230-240 min/operation) and then reached a second plateau (<200 min/operation) for the final 30 cases. Although a significant improvement in the operative time was noted after the first 50 cases, there were no significant differences in transfusion requirements, conversion rates to open surgery, postoperative complications, time to first flatus, or postoperative hospital stay between the groups.
CONCLUSION: Based on operative time analysis, this study show that experience of 50 cases of LADG with systemic lymphadenectomy for early gastric cancer is required to achieve optimum proficiency.
Keywords: Laparoscopic gastrectomy, Systemic lymphadenectomy, Learning curve
INTRODUCTION
In Korea, an aggressive surgical approach of gastrectomy with systemic lymphadenectomy has long been the standard treatment, even for superficial cancers, because of the limitations of preoperative assessment for the depth of tumor invasion[1,2] and imaging technique for the detection of regional lymph node metastasis[3-5]. Since its introduction in 1992, laparoscopy-assisted distal gastrectomy (LADG) has become a viable treatment alternative for patients with early gastric cancer[6-8]. Many studies have been conducted on the safety, efficacy, and feasibility of this procedure[9-14]. Surgeons who are seeking to undertake, or who are currently practicing this procedure, should be aware that it is considered as an advanced laparoscopic procedure and it is associated with a significant learning curve. Although many reports have been issued on the learning curves of laparoscopic cholecystectomy[15], laparoscopy-assisted colectomy[16], and laparoscopic urologic procedures[17], no report has been issued on the learning curve of LADG with systemic lymphadenectomy for early gastric cancer.
We hypothesized that the point at which proficiency is reached (as defined as the learning curve plateau) would be associated with improvements in perioperative outcomes, including transfusion requirement, conversion rates to open surgery, postoperative complications, time to first flatus, and postoperative hospital stay. The purpose of this study was to define the nature of the “learning curve” for LADG with systemic lymphadenectomy for early gastric cancer.
MATERIALS AND METHODS
Patients
The Dong-A University Medical Center’s stomach cancer database and the medical records of 90 consecutive patients with early gastric cancer who underwent LADG with systemic lymphadenectomy by a single surgeon (MC Kim) between April 2003 and November 2004 were reviewed. The review board of the Dong-A University Medical Center approved the protocol used for LADG with systemic lymphadenectomy in early gastric cancer patients and written informed consent was obtained from every patient that agreed to LADG with systemic lymphadenectomy.
Patients’ characteristics, pathologic findings, and postoperative outcomes were evaluated. Cases with mucosal lesions suitable for endoscopic mucosal resection (EMR) and with a history of upper abdominal surgery were excluded. The indication for EMR at our hospital is a Tm lesion with a size of <2 cm with no ulcer.
Surgical technique
A periumbilical trocar (10 mm) was inserted using the open surgical method, and four trocars were introduced under laparoscopic guidance. A rigid electrolaparoscope (25°, Panoview plus telescope, Richard Wolf, Germany) was then introduced through the umbilical port. Under pneumoperitoneum of 10-14 mmHg, the greater omentum was divided proximally at about 4 cm from the gastroepiploic arcade towards the lower pole of the spleen, using a new hemostatic device (The LigasureTM Vessel Sealing System, Valleylab, Boulder, CO, USA). The roots of the left gastroepiploic vessels were then exposed using an ultrasonic dissector (AutosonixTM, Tyco/US Surgical Inc., Norwalk, CT, USA) and a hook-type bovie, and divided with double LigasureTM clamps. Their perforating branches were dissected away from the greater curvature using an ultrasonic dissector (AutosonixTM, Tyco/US Surgical Inc., Norwalk, CT, USA), and the right gastroepiploic vein and artery were divided individually at their roots with double clips. The right gastric artery was then exposed and divided at its origin with double clips, thus creating room for the dissection of the suprapyloric lymph nodes (No. 5 lymph nodes). The duodenum was then transected 1 cm distal to the pylorus, using an endoscopic stapling device (Endo cutter 45 staple; Ethicon, OH, USA). After switching to an electrolaparoscope (50°, Panoview plus telescope, Richard Wolf, Germany), no. 8a (the common hepatic artery, anterosuperior group), and no. 9 (the celiac axis) lymph nodes were dissected along each artery, by using ultrasonic dissection and a hook-type bovie. In some cases, no. 11p (the proximal splenic artery), 12a (the hepatic artery), and 14v (the superior mesenteric vein) lymph nodes were dissected. The left gastric vein was then divided, and the root of the left gastric artery was exposed and divided with double clips, allowing dissection of the left gastric artery (No. 7 lymph nodes). The perigastric lymph nodes were dissected along the upper lesser curvature up to the esophagogastric junction. A 5-cm upper transverse skin incision that separated three fingers from the substernal angle, was made from the midline to the right side for the Billroth I reconstruction or to the left side for the Billroth II reconstruction. The distal two-thirds of the stomach were resected using a stapler (Proximate linear cutter 100 mm; Ethicon, OH, USA). Billroth I gastroduodenostomy was performed using a circular stapler (Proximate CDH 25; Ethicon, OH, USA), and Billroth II gastrojejunostomy with side to side jejunojejunostomy using two endoscopic stapling devices (Endo cutter 45 staple; Ethicon, OH, USA) or by hand sewing. Irrigation and observation of the operative field were achieved under pneumoperitoneum after closing the 5-cm minilaparotomy wound. Each trocar wound was closed after a closed suction drain had been placed around the anastomosis.
Perioperative management
All patients were managed routinely using a standardized postoperative protocol as follows: (1) No nasogastric intubation or preoperative mechanical bowel preparation; (2) the use of one closed suction drain; (3) sips of water at 48 h after the operation; (4) clear liquid diet after first flatus; (5) the discharge of the patients after tolerance of a soft diet for 2 d; and (6) no postoperative transfusion unless the hemoglobin level fell to or below 80 g/L and the patient complains of anemic symptoms. All patients received a continuous intravenous infusion of mixed analgesics (butorphanol 20 mg, ketorolac 300 mg, metoclopramide 30 mg, saline 100 mL) at 1 mL/h for 3-4 d after surgery.
Calculation of the learning curve
To define the learning curve, the 90 patients were divided into 9 sequential groups of 10 cases in each group and the average operative time of these 9 groups were determined. Other learning indicators, such as transfusion requirements, conversion rates to open surgery, postoperative complication, time to first flatus, and postoperative hospital stay, were evaluated for statistical significance. Statistical analysis was performed using the unpaired Student’s t-test and the Mann-Whitney U-test for continuous variables, and the χ2 and ANOVA tests for categorical variables. For all the three tests, P<0.05 was considered statistically significant. Data were expressed as mean±SD.
RESULTS
Patients’ characteristics and pathologic findings are summarized in Table 1. The mean patient body mass index was 22.8 kg/m2. Of the 22 patients with a submucosal lesion, two patients had one metastatic lymph node. There were no significant differences in patients’ characteristics, oncological radicality, and pathology between the two groups.
Table 1.
Characteristics and pathologic results of patients
| Total | 1–50 cases | 51–90 cases | P | |
| Total number of patients | 90 | 50 | 40 | |
| Age (yr, mean±SD) | 55.7±12.0 | 56.3±11.3 | 54.9±12.9 | 0.6907 |
| Sex ratio (male:female) | 50:40 | 26:24 | 24:16 | 0.5854 |
| Body mass index (kg/m2, mean±SD) | 22.8±2.7 | 23.1±2.5 | 22.5±2.9 | 0.1700 |
| Comorbidity (%) | 29 (32.2) | 13 (26.0) | 16 (40.0) | 0.2359 |
| Method of reconstruction | 0.5343 | |||
| B–I | 67 | 39 | 28 | |
| B–II | 23 | 11 | 12 | |
| T stage | 0.1758 | |||
| Tis | 2 | 1 | 1 | |
| Tm | 66 | 33 | 33 | |
| Tsm | 22 | 16 | 6 | |
| N stage | 0.8439 | |||
| N0 | 87 | 49 | 38 | |
| N1 | 3 | 1 | 2 | |
| Extent of lymphadenectomy | 0.4709 | |||
| D1+α | 11 | 8 | 3 | |
| D1+β | 68 | 36 | 32 | |
| D2 | 11 | 6 | 5 | |
| Retrieved LN number (mean±SD) | 27.0±9.7 | 25.4±10.0 | 28.9±8.9 | 0.1330 |
| Resection margin (cm, mean±SD) | ||||
| Proximal | 4.2±2.6 | 3.8±2.4 | 4.7±2.7 | 0.1472 |
| Distal | 5.1±3.1 | 5.0±3.1 | 5.3±3.0 | 0.5752 |
LN, lymph node; D1+α: D1+no. 7 LN; D1+β: D1+no. 7, 8a, 9 LN; D2: D1+β+no. 11p, 12a, 14v LN.
Mean operative time was 227.2 min (Table 2). Open conversion was required intraoperatively in two cases due to excessive intra-abdominal fat (n = 1) or intra-abdominal adhesion (n = 1). The body mass index of the patient with excessive intra-abdominal fat was 29.3 kg/m2. Fifteen complications occurred in 13 patients. These complications included wound complications, intra-abdominal bleeding, anastomotic bleeding, dumping syndrome, subcutaneous emphysema, intra-abdominal abscess, and anastomotic stricture. All these complications were treated by conservative management without reoperation. No deaths occurred in this series.
Table 2.
Overall postoperative outcomes
| Total | 1–50 cases | 51–90 cases | P | |
| Operative time (min, mean±SD) | 227.2±48.0 | 251.3±47.3 | 227.2±48.0 | <0.0001 |
| No. of transfused patients (%) | 5 (5.6) | 3 (6.0) | 2 (5.0) | 0.837 |
| Time to first flatus (d, mean±SD) | 3.1±0.8 | 3.1±0.9 | 3.1±0.6 | 0.805 |
| Postoperative hospital stay (d, mean±SD) | 7.5±1.2 | 7.6±1.4 | 7.4±1.0 | 0.610 |
| Postoperative complication (%) | 13 (14.4) | 6 (12.0) | 7 (17.5) | 0.663 |
Defining the learning curve
Figure 1 shows two plateaus in operative time vs cumulative case number plot for LADG with systemic lymphadenectomy. After the first 10 LADGs, the operative time reached its first plateau (230-240 min/operation) and then reached a second plateau (<200 min/operation) for the final 30 cases, which was between 30 and 40 min/operation faster than that for the first 10-50 cases. We considered that learning was complete at the second plateau, and not at the first. When we compared the postoperative outcomes of the first 50 cases with the last 40 cases, no significant difference was observed despite the fact that mean operative time had been obviously reduced for the last 40 cases (Table 3).
Figure 1.
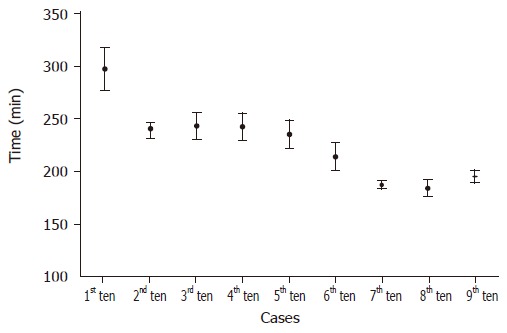
LADG with systemic lymphadenectomy (operative time vs number of cases experienced).
Table 3.
Comparison of postoperative outcomes (first 50 patients vs last 40 patients)
| Operative time (min) | Open conversion | Transfusion requirement | Time to first flatus (d) | Hospital stay (d) | Complication (patients) | |
| First 50 patients | 251.3±47.3 | 1 | 3 | 3.1±0.9 | 7.6±1.4 | 7 |
| Last 40 patients | 197.0±27.7 | 1 | 2 | 3.1±0.6 | 7.4±1.0 | 6 |
P<0.0001
DISCUSSION
The proportion of cancers invading the mucosa or submucosa represents about a half of surgical gastric cancer cases in Korea. Recently, many gastric surgeons have expressed a high level of interest in laparoscopic surgery for early gastric cancer, because laparoscopic surgery has been proven to have substantial advantages over conventional open surgery[14,18-20]. However, LADG with systemic lymphadenectomy is considered technically more complicated than other laparoscopic procedures (e.g., cholecystectomy, Nissen fundoplication, colon resection, or splenectomy) because many great vessels must be identified and extensive lymph node dissection is necessary for radical gastrectomy.
The definition of the completion of learning is clearly arbitrary. To determine that learning has occurred, some have used the minimization of operative complications or the reaching of a steady mean operative time as measures. According to the learning curves of other laparoscopic procedures, surgeons who have performed more than 20 laparoscopic cholecystectomies[15] or 8 laparoscopic urologic procedures[17] have lower complication rates. As for colorectal surgery, approximately 11-15 completed laparoscopic colectomies were found to be needed to comfortably learn this procedure[21]. We hypothesized that the point at which learning has been achieved (as defined by the operative time plateau) would be associated with an improved postoperative outcome. However, though a significant improvement in operative time was noted after the first 50 cases, this did not correspond with a significant reduction in other postoperative outcomes, including transfusion requirements, conversion rates to open surgery, postoperative complications, time to first flatus, or postoperative hospital stay. This finding may be attributed to, firstly, regardless of operative time, transfusion requirement or conversion to open surgery which was rare, and postoperative complications occurred evenly in each of the nine groups. Second, time to first flatus was not proportioned to operative time. The mean time to first flatus in the present study was 3.1 d, although flatus has been reported to return at a mean 2.5 d after laparoscopic gastrectomy and 3.5 d after conventional open gastrectomy[22,23]. However, the previous result of 2.6 d may have been caused by less extensive lymphadenectomy (D1+α).
Although Kitano et al.[11] reported that the mean operative time of 116 cases for LADG with D1+α lymphadenectomy (perigastric and no. 7 lymph nodes dissection) was 234 min, Noshiro et al.[13] found a mean operative time for 79 cases of LADG with D1+β lymphadenectomy of over 300 min. In another study of 43 LADGs was performed for 2 years, the mean operative time was 225 min despite LADG with D1+β lymphadenectomy[24]. We performed 90 LADGs with D1+β lymphadenectomy for 20 mo, and mean operative time of the present study was 227.2 min. We believe that the operative time required for LADG in gastric cancer is related to the extent of the lymphadenectomy, constant LADG practice, the experience of open radical gastrectomy, information and familiarity with the laparoscopic system and instruments, and the skill of the operative team.
In conclusion, based on operative time analysis, our study shows that experience of 50 cases of LADG with systemic lymphadenectomy for early gastric cancer is required to achieve optimum proficiency.
Footnotes
Science Editor Wang XL and Guo SY Language Editor Elsevier HK
References
- 1.Polkowski M, Palucki J, Wronska E, Szawlowski A, Nasierowska-Guttmejer A, Butruk E. Endosonography versus helical computed tomography for locoregional staging of gastric cancer. Endoscopy. 2004;36:617–623. doi: 10.1055/s-2004-814522. [DOI] [PubMed] [Google Scholar]
- 2.Ishigami S, Yoshinaka H, Sakamoto F, Natsugoe S, Tokuda K, Nakajo A, Matsumoto M, Okumura H, Hokita S, Aikou T. Preoperative assessment of the depth of early gastric cancer invasion by transabdominal ultrasound sonography (TUS): a comparison with endoscopic ultrasound sonography (EUS) Hepatogastroenterology. 2004;51:1202–1205. [PubMed] [Google Scholar]
- 3.Kim MC, Kim HH, Jung GJ, Lee JH, Choi SR, Kang DY, Roh MS, Jeong JS. Lymphatic mapping and sentinel node biopsy using 99mTc tin colloid in gastric cancer. Ann Surg. 2004;239:383–387. doi: 10.1097/01.sla.0000114227.70480.14. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Hayes N, Karat D, Scott DJ, Raimes SA, Griffin SM. Radical lymphadenectomy in the management of early gastric cancer. Br J Surg. 1996;83:1421–1423. doi: 10.1002/bjs.1800831032. [DOI] [PubMed] [Google Scholar]
- 5.Maruyama K, Sasako M, Kinoshita T, Sano T, Katai H. Can sentinel node biopsy indicate rational extent of lymphadenectomy in gastric cancer surgery? Fundamental and new information on lymph-node dissection. Langenbecks Arch Surg. 1999;384:149–157. doi: 10.1007/s004230050185. [DOI] [PubMed] [Google Scholar]
- 6.Huscher CG, Mingoli A, Sgarzini G, Sansonetti A, Di Paola M, Recher A, Ponzano C. Laparoscopic versus open subtotal gastrectomy for distal gastric cancer: five-year results of a randomized prospective trial. Ann Surg. 2005;241:232–237. doi: 10.1097/01.sla.0000151892.35922.f2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Adrales GL, Gandsas A, Mastrangelo MJ, Schwartz R. An introduction to laparoscopic gastric resection. Curr Surg. 2003;60:385–389. doi: 10.1016/S0149-7944(03)00088-6. [DOI] [PubMed] [Google Scholar]
- 8.Kitano S, Shiraishi N. Current status of laparoscopic gastrectomy for cancer in Japan. Surg Endosc. 2004;18:182–185. doi: 10.1007/s00464-003-8820-7. [DOI] [PubMed] [Google Scholar]
- 9.Huscher CG, Mingoli A, Sgarzini G, Sansonetti A, Lirici MM, Napolitano C, Piro F. Videolaparoscopic total and subtotal gastrectomy with extended lymph node dissection for gastric cancer. Am J Surg. 2004;188:728–735. doi: 10.1016/j.amjsurg.2004.08.040. [DOI] [PubMed] [Google Scholar]
- 10.Shimizu S, Noshiro H, Nagai E, Uchiyama A, Tanaka M. Laparoscopic gastric surgery in a Japanese institution: analysis of the initial 100 procedures. J Am Coll Surg. 2003;197:372–378. doi: 10.1016/S1072-7515(03)00419-8. [DOI] [PubMed] [Google Scholar]
- 11.Kitano S, Shiraishi N, Kakisako K, Yasuda K, Inomata M, Adachi Y. Laparoscopy-assisted Billroth-I gastrectomy (LADG) for cancer: our 10 years' experience. Surg Laparosc Endosc Percutan Tech. 2002;12:204–207. doi: 10.1097/00129689-200206000-00021. [DOI] [PubMed] [Google Scholar]
- 12.Uyama I, Sugioka A, Fujita J, Komori Y, Matsui H, Soga R, Wakayama A, Okamoto K, Ohyama A, Hasumi A. Completely laparoscopic extraperigastric lymph node dissection for gastric malignancies located in the middle or lower third of the stomach. Gastric Cancer. 1999;2:186–190. doi: 10.1007/s101200050044. [DOI] [PubMed] [Google Scholar]
- 13.Noshiro H, Shimizu S, Nagai E, Ohuchida K, Tanaka M. Laparoscopy-assisted distal gastrectomy for early gastric cancer: is it beneficial for patients of heavier weight? Ann Surg. 2003;238:680–685. doi: 10.1097/01.sla.0000094302.51616.2a. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Adachi Y, Suematsu T, Shiraishi N, Katsuta T, Morimoto A, Kitano S, Akazawa K. Quality of life after laparoscopy-assisted Billroth I gastrectomy. Ann Surg. 1999;229:49–54. doi: 10.1097/00000658-199901000-00006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Moore MJ, Bennett CL. The learning curve for laparoscopic cholecystectomy. The Southern Surgeons Club. Am J Surg. 1995;170:55–59. doi: 10.1016/s0002-9610(99)80252-9. [DOI] [PubMed] [Google Scholar]
- 16.Bennett CL, Stryker SJ, Ferreira MR, Adams J, Beart RW. The learning curve for laparoscopic colorectal surgery. Preliminary results from a prospective analysis of 1194 laparoscopic-assisted colectomies. Arch Surg. 1997;132:41–44; discussion 45. doi: 10.1001/archsurg.1997.01430250043009. [DOI] [PubMed] [Google Scholar]
- 17.See WA, Cooper CS, Fisher RJ. Predictors of laparoscopic complications after formal training in laparoscopic surgery. JAMA. 1993;270:2689–2692. [PubMed] [Google Scholar]
- 18.Kitano S, Shiraishi N, Fujii K, Yasuda K, Inomata M, Adachi Y. A randomized controlled trial comparing open vs laparoscopy-assisted distal gastrectomy for the treatment of early gastric cancer: an interim report. Surgery. 2002;131:S306–S311. doi: 10.1067/msy.2002.120115. [DOI] [PubMed] [Google Scholar]
- 19.Adachi Y, Shiraishi N, Shiromizu A, Bandoh T, Aramaki M, Kitano S. Laparoscopy-assisted Billroth I gastrectomy compared with conventional open gastrectomy. Arch Surg. 2000;135:806–810. doi: 10.1001/archsurg.135.7.806. [DOI] [PubMed] [Google Scholar]
- 20.Weber KJ, Reyes CD, Gagner M, Divino CM. Comparison of laparoscopic and open gastrectomy for malignant disease. Surg Endosc. 2003;17:968–971. doi: 10.1007/s00464-002-8738-5. [DOI] [PubMed] [Google Scholar]
- 21.Simons AJ, Anthone GJ, Ortega AE, Franklin M, Fleshman J, Geis WP, Beart RW. Laparoscopic-assisted colectomy learning curve. Dis Colon Rectum. 1995;38:600–603. doi: 10.1007/BF02054118. [DOI] [PubMed] [Google Scholar]
- 22.Kim MC, Park SY, Jung GJ, Kim HH, Noh SH. The usefulness of intraoperative needle decompression of the colon during radical gastrectomy--a prospective and randomized trial. Hepatogastroenterology. 2004;51:97–99. [PubMed] [Google Scholar]
- 23.Mochiki E, Nakabayashi T, Kamimura H, Haga N, Asao T, Kuwano H. Gastrointestinal recovery and outcome after laparoscopy-assisted versus conventional open distal gastrectomy for early gastric cancer. World J Surg. 2002;26:1145–1149. doi: 10.1007/s00268-002-6286-8. [DOI] [PubMed] [Google Scholar]
- 24.Fujiwara M, Kodera Y, Kasai Y, Kanyama Y, Hibi K, Ito K, Akiyama S, Nakao A. Laparoscopy-assisted distal gastrectomy with systemic lymph node dissection for early gastric carcinoma: a review of 43 cases. J Am Coll Surg. 2003;196:75–81 DOI : 10.1016/S1072-7515(02)01539-9. doi: 10.1016/s1072-7515(02)01539-9. [DOI] [PubMed] [Google Scholar]


