Abstract
Workers required to wear respirators must undergo additional respirator fit testing if a significant change in body weight occurs. Approximately 10% of working women of reproductive age will be pregnant and experience a significant change in weight, yet the effect of pregnancy-associated weight gain on respirator fit is unknown. Cephalo-facial anthropometric measurements and quantitative fit testing of N95 filtering facepiece respirators (N95 FFR) of 15 pregnant women and 15 matched, non-pregnant women were undertaken for comparisons between the groups.There were no significant differences between pregnant and non-pregnant women with respect to cephalo-facial anthropometric measurements or N95 FFR quantitative fit tests. Healthy pregnant workers, who adhere to the recommended weight gain limits of pregnancy, are unlikely to experience an increase in cephalo-facial dimensions that would mandate additional N95 FFR fit testing above that which is normally required on an annual basis.
Keywords: pregnancy, N95 filtering facepiece respirators, respirator fit testing, cephalo-facial anthropometrics
INTRODUCTION
Women currently comprise 47% of the U.S. workforce and, of the ~36 million working women aged 15 – 44 years, some 10% will be pregnant.(1,2) Approximately 3.3 million U.S. industrial workers and 4.6 million nursing personnel utilize respiratory protective equipment (RPE), such as filtering facepiece respirators (FFR), in the course of their employment.(3) Thus, it stands to reason that a sizeable number of employed women who wear RPE may be pregnant at any given time. Workers who are employed in occupations that necessitate respirator use, as mandated by the Occupational Safety and Health Administration (OSHA), are required to undergo annual respirator fit testing to ensure that the respirators they are using are sufficiently protective.(4) In addition to routine annual testing, OSHA Respiratory Protection Standard 1910.134 states that “The employer shall conduct an additional fit test whenever the employee reports, or the employer, physician or other licensed healthcare provider, supervisor, or program administrator makes visual observations of, changes in the employee's physical condition that could affect respirator fit. Such conditions include, but are not limited to, facial scarring, dental changes, cosmetic surgery, or an obvious change in body weight (underlining added by study authors for emphasis).(4) A prior survey of men and women RPE users(5) has shown a significant association of increased facial dimensions (i.e., face length and face width) with an increase in the Body Mass Index (BMI), an approximation of body habitus derived from the ratio of body weight in kilograms to height in square meters. Pregnancy is not considered an exclusion to wearing RPE and is not mentioned on the OSHA medical questionnaire(4) used to evaluate workers who will be wearing RPE, irrespective of the fact that significant weight gain occurs during gestation. Institute of Medicine guidelines for pregnancy weight gain by BMI category are outlined in TABLE 1.(6) Thus, it would be of value to determine if physiologic pregnancy-related weight gain is associated with significant changes in facial dimensions that might alter the fit of RPE and thereby necessitate additional respirator fit testing. The current investigation, part of a larger study by the National Institute for Occupational Safety and Health (NIOSH) with some of its data previously reported,(3) examined facial anthropometric measurements of pregnant and non-pregnant women and their fit test results for N95 filtering facepiece respirators (N95 FFR), the most commonly utilized respirator in U.S. industry and healthcare.(3) This data could be of value to various stakeholders such as RPE users, respiratory protection program managers and RPE researchers.
TABLE 1.
Institute of Medicine current guidelines for singleton pregnancy weight gain by BMI category.(6)
| Pre-pregnancy BMI | Total Pregnancy Weight Gain |
|---|---|
| Underweight (<18.5 kg/m2) | 12.7 – 18.1 kg |
| Normal weight (18.5 – 24.9 kg/m2) | 11.3 – 15.4 kg |
| Overweight (25.0 – 29.9 kg/m2) | 6.8 – 11.3 kg |
| Obese (>30 kg/m2) | 5.0 – 9.0 kg |
MATERIALS AND METHODS
Fifteen healthy, non-smoking women in the second to mid-third trimester of pregnancy (i.e., 13 - 35 weeks pregnant) and 15 healthy, non-smoking, non-pregnant women, all of whom were experienced in RPE use, were enrolled in the study. The subjects were selected from a larger pool and, because there was no pre-pregnancy anthropometric data with which to match subjects, the pregnant subjects and non-pregnant subjects were matched by stature (to within 2.54 cm [one inch]) because this parameter has a proportional biological relationship with cephalo-facial anthropometrics.(7,8) The study gestational period (13 – 35 weeks) was selected because it is the time of greatest physiologic weight gain during pregnancy.(6) Demographic mean values with standard deviations (95% confidence intervals) of the subjects are outlined in TABLE 2. For comparison of non-pregnant weights between subjects, the pre-pregnancy weight of the each pregnant subject was calculated by subtracting one-half the recommended weight gain of pregnancy (because the pregnant subjects’ mean gestation period of 21.1 weeks was roughly equivalent to one-half the normal 40 week gestation period of pregnancy) as defined by the pregnancy BMI category of underweight, normal weight, overweight, and obese.(6) This resulted in an estimated mean pre-pregnancy weight of 63.0±13.1 kg (55.8 – 70.3) and an estimated mean pre-pregnancy BMI of 23.0±4.7 kg/m2 (20.4 – 25.7). Subjects underwent a screening physical examination by a licensed physician on the day of testing. The study was approved by the NIOSH Human Subjects Review Board, and all subjects provided oral and written informed consent.
TABLE 2.
Demographic mean values with standard deviations (95% confidence intervals) of subjects.
| Measured Variable | Pregnant Subjects | Non-pregnant Subjects |
|---|---|---|
| Age | 28.7±2.5 yrs (27.3 – 30.1) | 26.3±4.8 yrs (23.6 – 29.0) |
| Height | 166.1±4.8 cm (163.4 = 168.8) | 166.0±5.3 cm (163.0 – 169.0) |
| Weight | 69.0±11.8 kg (62.5 – 75.5) | 65.8±9.0 kg (60.7 – 70.8) |
| Body Mass Index | 24.6±4.0 kg/m2 (20.1 – 25.9) | 24.2±3.2 kg/m2 (22.4 – 26.0) |
| Gestational Age | 21/1±5.3 wks (18.1 – 24.0) | N/A |
Subjects initially had weight and height measured and BMI calculated, followed by anthropometric measurements of 13 cephalo-facial landmarks typically utilized for respirator fit testing investigations.(9) All cephalo-facial anthropometric measurements were carried out by one trained, experienced anthropometric technician utilizing anthropometric spreading calipers and Martin-type sliding calipers (GPM, Basel, CH) to measure linear distances between facial landmarks, a Burton digital pupilometer (RH Burton Co., Grove City, OH, US) to measure distances between pupils, and a tape measure for circumference measurements. Subjects were then randomized to wearing one of two popular styles of N95 FFR (3M 9210 flat fold model “one size fits most” [3M Company, St. Paul, MN]; Moldex pre-molded, cup-shaped model 2200 medium/large size or model 2201 small size [Moldex, Culver City, CA]). The N95 FFR was first donned as per the manufacturer's instructions and positive and negative user seal checks were performed to assess the seal of the respirator to the face.(4) If any seal check was failed, the subject adjusted the respirator and repeated the seal checks until both user seal checks were passed, following which the N95 FFR was worn for a three minute acclimation period. Subjects then underwent respirator quantitative fit testing with the Portacount Plus® Model 8020 fit tester with N95 Companion (TSI, Shoreview, MN) that measured the particle count inside and outside the N95 FFR while subjects performed a series of seven one-minute exercises while standing (normal breathing, deep breathing, turning the head side to side, moving the head up and down, talking, bending over, normal breathing) and one 15 second exercise (grimace). The particle count of the test laboratory was enhanced with nebulized sodium chloride solution. The ratio of the particle count inside the N95 FFR to the particle count outside the respirator is termed the fit factor. Because fit factors are typically log-normally distributed,(10) they were log-transformed and the geometric mean fit factor (GMFF) was used for statistical analysis. A GMFF of ≥100, indicative of ≤1% entry of particles into the respirator wearer's breathing zone, is considered a minimum passing score on the OSHA fit test.(4) The pass rates for the initial (randomized) N95 FFR models were 59% (13/22) and 50% (11/22) for the pregnant and non-pregnant subjects, respectively. Subjects not passing the initial fit test with the randomized N95 FFR style were subsequently fit tested with the other style and all subjects passed fit testing with one or the other styles of N95 FFRs (3M 9210 [13 pregnant and 7 non-pregnant subjects], Moldex 2200 [3 non-pregnant subjects], Moldex 2201 [2 pregnant and 5 non-pregnant subjects]) as indicated by a GMFF of ≥100.
Statistical Analysis
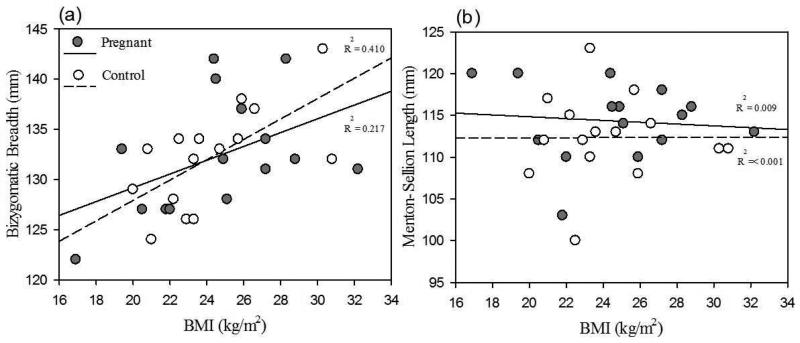
The 13 cephalo-facial anthropometric variables and the N95 FFR fit test results between pregnant and non-pregnant subjects were analyzed by paired t-tests (2-tailed) with associated confidence intervals. A statistical significance was accepted when p<0.05 and all analyses were performed using a statistical software package (SPSS v.18, IBM, Somers, NY). In addition, data sets were plotted comparing pregnant and non-pregnant subjects for face width (Bizygomatic Breadth [FIGURE Ia]) and face length (Menton-Sellion Length [FIGURE Ib]), the two facial anthropometric parameters used to develop the NIOSH bivariate fit test panel for respirator fit testing.(11)
FIGURE I.
Relationship of Bizygomatic Breadth (a) and Menton-Sellion Length (b) to Body Mass Index (BMI) of pregnant and non-pregnant subjects.
RESULTS
There were no significant differences in any demographic variables between pregnant and non-pregnant subjects and there were no significant differences in the GMFFs or cephalo-facial anthropometric measurements between pregnant and non-pregnant subjects (TABLE 3). Of the two variables utilized for the NIOSH bivariate respirator fit test panel,(11) BMI in the current study was more closely correlated with Bizygomatic Breadth than with Menton-Sellion length (FIGURE I). For pregnant subjects, the Pearson correlation coefficients for BMI vs Bizygomatic Breadth and Menton-Sellion length were r=0.466 (p=0.08) and r=0.09 (p=0.73), respectively. For non-pregnant subjects, these respective correlation coefficients were r=0.641 (p=0.01) and r=0.01 (p=0.98), and for pregnant versus non-pregnant subjects were r=0.53 (p=0.01) and r=0.03 (p=0.85).
TABLE 3.
Mean values for facial anthropometric measurements and geometric fit factors of matched pregnant and non-pregnant subjects.
| Anthropometric Variable (mm) | Subjects |
p-value | |
|---|---|---|---|
| Pregnant (n=15) | Non-pregnant (n=15) | ||
| Bigonial Breadth | 101.8±7.0 [97.9–105.6] | 104.1±4.4 [101.6 –106.5] | 0.19 |
| Bizygomatic Breadth | 132.3±5.9 [129.0–135.5] | 132.2±5.0 [129.4 –134.9] | 0.92 |
| Interpupillary Breadth | 61.3±3.0 [59.6–62.9] | 60.4±4.2 [58.0 –62.7] | 0.49 |
| Lip Length | 49.3±3.7 [47.2–51.2] | 47.6±2.6 [46.1 –49.0] | 0.14 |
| Menton-Sellion Length | 114.3±4.6 [111.7–116.8] | 112.3±5.2 [109.4 –115.2] | 0.25 |
| Menton-Subnasale Length | 63.4±4.2 [61.0–65.7] | 62.9±4.4 [60.4 –65.3] | 0.75 |
| Nasal Root Breadth | 17.3±1.5[16.4 –18.1] | 17.4±2.4 [16.0 –18.7] | 0.91 |
| Nose Breadth | 32.2±2.9 [30.5–33.8] | 32.3±4.8 [29.6 –34.9] | 0.96 |
| Nose Protrusion | 21.8±1.7 [20.8–22.7] | 20.5±2.4 [19.2 –21.8] | 0.10 |
| Sellion-Subnasale Length | 51.2±2.5 [49.8–52.5] | 48.7±3.7 [46.6 –50.7] | 0.06 |
| Minimal Frontal Breadth | 109.3±5.5 [106.3–112.3] | 109.0±5.5 [105.9 –112.0] | 0.83 |
| Head Breadth | 147.0±3.3 [145.1–148.8] | 147.7±3.1 [145.9 –149.3] | 0.45 |
| Head Circumference | 559.7±16.2 [550.7–568.7] | 566.9±22.6 [554.4–579.4] | 0.18 |
| Geometric Mean Fit Factor | 152.9±44.6 [128.1–177.5] | 175.5±62.2 [141.0–209.9] | 0.33 |
Values are mean ± SD [95% confidence interval, Lower – Upper bound]
DISCUSSION
Given the increasing prevalence of obesity (defined as weight ≥20% of ideal weight(12)) in the U.S. populace, concerns have been voiced over the impact of obesity-related increases in facial dimensions upon the fit of respirators.(5) This is logical, given that an increase in buccal region (cheek) dimensions frequently occurs in concert with significant excess weight gain(13,14) due to concurrent expansion of facial adipocytes (fat cells). Face width and length are the major determinants of a person's position in a specific cell of the NIOSH respirator fit test panel. These measurements aid in estimating the size of a respirator that will best fit that individual and have been shown to be increased in obesity.(5) Under the influence of the gestational hormone progesterone, body fat begins to accumulate in femoral and abdominal regions(15) during the first two trimesters of pregnancy. This fat is mobilized during the third trimester for energy needs and upcoming lactation requirements, such that pregnancy is the only normal physiological process for an adult that increases body weight by ≥20%.(16) Although significant increases in body weight are the norm during pregnancy, this should not be attributed solely to fat deposition and thereby imply a possible increase in facial dimensions. Prior studies have shown only modest increases in pregnancy-associated body fat of pre-gestational, normal weight women (i.e., 2% at 7 weeks of gestation,(17) 3.8 kg at 14 weeks gestation,(18) 4.9 kg at 36 weeks of gestation(19)). The majority of physiologic pregnancy weight gain is attributable to the combined weights of the fetus, placenta, amniotic fluid, increased maternal blood and plasma volume, enlarged uterus, and increased breast mass,(15) none of which is likely to be associated with increased facial adipocyte size.
Our data indicate that pregnant women with a mean pre-pregnancy normal BMI, and non-pregnant women matched by stature and of similar mean age, weight and BMI, were not significantly different with respect to cephalo-facial anthropometric measurements and quantitative respirator fit test results (TABLE 3). The mean difference between the estimated pre-pregnancy weight and the actual pregnancy weight of study subjects was only 6.0 kg and within the guidelines for recommended weight gain during pregnancy.(6) This makes it unlikely to have had a significant impact on facial features. The impact on facial dimensions of excess weight gain versus the normal physiologic weight gain of pregnancy can be appreciated by comparing the pregnant and non-pregnant subjects’ mean Bizygomatic Breadth (132.3 mm and 132.2 mm, respectively; p=0.92) and Menton-Sellion Length (114.3 mm and 112.3 mm, respectively; p=0.25) with women subjects in the NPPTL/NIOSH respirator fit panel survey of 3,997 persons (Bizygomatic Breadth 135.1 mm, Menton-Sellion Length 113.4 mm), the majority (71.9%) of whom were overweight or obese.(9) It is plausible that an increase in facial width (i.e., Bizygomatic Breadth) is a more sensitive indicator of an increase in facial size related to weight gain than facial length (i.e., Menton-Sellion Length), but this supposition would require additional study to fully verify (FIGURE I). A previous anthropometric study of RPE users(5) also found that increased BMI significantly affected Bizygomatic Breadth more than Menton-Sellion Length.
This lack of significant difference in facial anthropometrics of the current study's pregnant and non-pregnant subjects, coupled with the lack of significant fat deposition of women with normal physiological weight gain during pregnancy,(17-19) infers that the normal physiological weight gain of pregnancy should not generally result in significant deposition of facial fat and resultant increase in facial dimensions. This further suggests that any concerns regarding the need for additional fit testing, related to the physiologic weight gain of women in the second and third trimesters of pregnancy who adhere to the recommended weight gain of pregnancy,(6) may be unfounded. This has additional ramifications, above and beyond time and costs associated with fit testing, given that some concern has been raised over the issue of the impact on pregnant women of elevated levels of carbon dioxide in the hoods utilized for respirator qualitative fit testing.(20) It may be that significant increases in Bizygomatic Breadth measurements of pregnant and non-pregnant women who wear RPE could be a useful marker for the consideration of additional fit testing, but this hypothesis would require a study with large numbers of appropriate subjects. Women who exceed the recommended weight gain of pregnancy and those who suffer from pregnancy-associated disorders that result in facial edema (e.g., pre-eclampsia), may experience increases in facial dimensions that could impact respirator fit. Additionally, some women in the 8th and 9th months of pregnancy develop non-pitting edema of the face that is related to increased vascularization and permeability of skin capillaries and salt and water retention. This facial edema may be associated with the recumbent posture of sleep as it is most apparent in the morning and decreases during the day (note, dependent edema is physiologic in pregnancy, but facial edema may be a sign of renal or cardiac disease(21,22)). The non-recumbent nature of most work involving RPE would diminish such recumbent-related facial edema and likely minimize any impact on fit factors, though this hypothesis would require validation. The data from the current study are of additional significance due to the apparently limited information available regarding facial anthropometrics associated with pregnancy. Despite an extensive literature search utilizing multiple search engines, the authors were able to identify only one study reporting such data. Slade(23) reported a significantly greater mean facial width for pregnant women at four months of gestation compared with similarly aged, non-pregnant controls (124.8 mm±7.2, 109.0 mm±1.45, respectively). However, the sample sizes of the pregnant subjects and controls were different (40 vs 20) and the (unadjusted) weights of the pregnant subjects and the controls were very similar (59.8 kg vs 60.25 kg, respectively) suggesting possible differences in stature that might be reflective of differences in facial features. Further, no information was provided on the health status of the pregnant subjects that would have elucidated if any subjects had pregnancy-related disorders that might result in changes in facial dimensions (e.g., pre-eclampsia). Notably, the facial widths (Bizygomatic Breadth) of the pregnant subjects and controls were considerably less than those of the current study (TABLE 3), no doubt reflecting the increase in body dimensions of the general populace over the past 35+ years since the study(23) was published.
Limitations of the current study include the relatively small size of the investigated groups (n=15 each), but is tempered by the fact that all subjects were experienced with RPE, and that recruitment and testing of pregnant women entails more complex issues than with non-pregnant women given the (appropriate) concerns for simultaneous maternal and fetal well-being. Also, we did not have pre-pregnancy anthropometric measurements and fit testing results that would have had the pregnant subjects serve as their own controls, so that we had to rely on a non-pregnant control group. However, pregnant and non-pregnant subjects in the current study were well matched for stature, an anthropometric parameter that is related to cephalo-facial measurements(7,8) and had similar mean age, body weight and BMI. Ideally, a larger study should be carried out that includes anthropometric measurements and respirator fit tests in the pre-pregnancy period and in the latter stages of pregnancy of normal weight and obese women, given that it has been shown in a recent study that 73% of pregnant women exceeded the Institute of Medicine-recommended weight gain of approximately 11 – 16 kg (25 -35 lbs) for women of pre-pregnancy normal BMI.(24) Facial anthropometric measurements are subject to issues of repeatability and reproducibility, with accuracy typically 1-3 mm(25) and acceptability generally considered to be up to 1.5 mm.(26) In order to fully demonstrate a significant difference in measured parameters that are subject to significant variability, a significantly larger sample size would be needed. Of further note in the current study, one of the FFRs was a “one size fits most” and the other respirator was offered in either a small size or a medium/large size. Respirators that are sized small typically fit a very small proportion of the population (narrow faces and chins) whereas the medium/large size will fit a much larger array of facial features. The small sized respirators may be so tailored to a narrow range of facial features that their ability to accommodate changes due to pregnancy would be different than with a medium/large respirator, which is already more forgiving of different facial dimensions. The issue of lack of accommodation of small facial features with a single-size design N95 FFR was highlighted in California during the recent pandemic influenza and would need to be addressed in future studies.(27)
CONCLUSIONS
Pregnant women with pre-gestational period normal BMI and adherence to recommended pregnancy weight gain guidelines,(6) who wear N95 FFRs in the work environment, may not need to undergo additional respirator fit testing during pregnancy over concerns about potential pregnancy-related physiologic weight gain. Pregnancy-associated physiologic weight gain alone should not alter the ability of a healthy pregnant woman to pass a respirator fit test with the same N95 FFR used in the immediate pre-pregnant state. Given the potentially large numbers of pregnant women who wear RPE in the occupational setting and for other reasons (e.g., during respiratory infectious disease outbreaks such as pandemic influenza, for airborne particle protection during activities such as woodworking, as protection from environmental allergens, etc.), this is an important issue. A larger study involving facial anthropometric measurements and respirator fit testing in the pre-pregnancy state and during the last two trimesters of pregnancy, that includes both overweight and normal weight pregnant women, is well warranted and needed to validate the findings of the current study.
Acknowledgements
the authors wish to thank Michael Bergman, MS and Drs. Ziqing Zhuang and Ronald Shaffer of NPPTL/NIOSH, and David Caretti of the U.S. Army's Edgewood Chemical and Biological Center for their manuscript reviews and helpful suggestions.
Footnotes
Disclaimer: The findings and conclusions in this report are those of the authors and do not necessarily represent the views of the National Institute for Occupational Safety and Health. Mention of product names does not imply endorsement.
REFERENCES
- 1.U.S. Bureau of Labor Statistics [May 5, 2014];Women in the labor force: a databook. 2013 Available at at http://www.bls.gov/cps/wlf-databook-2012.pdf.
- 2.National Center for Health Statistics, U.S. Department of Health and Human Services Estimated pregnancy rates by outcome for the United States, 1990-2004. National Vital Statistics Reports. 2008;56(15):1–28. [PubMed] [Google Scholar]
- 3.Roberge RJ, Kim J-H, Powell JB. N95 mask use during pregnancy. Am. J. Inf. Control. doi: 10.1016/j.ajic.2014.06.025. in press. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Occupational Safety and Health Administration (OSHA) [May 5, 2014];Occupational Safety and Health Standards, Respiratory Protection Standard 1910.134. 1998 Available at http://www.osha.gov/pls/oshaweb/owadisp.show_document?p_id=12716&p_table=standards.
- 5.Roberge RJ, Zhuang Z, Stein LM. Association of body mass index with facial dimensions for defining respirator fit test panels. J. Int. Soc. Resp. Protect. 2006;23(1,2):44–52. [Google Scholar]
- 6.Institute of Medicine and National Research Council . In: Weight gain during pregnancy: reexamining the guidelines. Rasmussen KM, Yaktine AL, editors. The National Academies Press; Washington, DC: 2009. pp. 263–265. [PubMed] [Google Scholar]
- 7.Krishan K. Estimation of stature from cephalo-facial anthropometry in north Indian population. Forensic. Sci. Intern. 2008;181:52e1–52e6. doi: 10.1016/j.forsciint.2008.08.001. [DOI] [PubMed] [Google Scholar]
- 8.Ewunonu EO, Anibeze CIP. Estimation of stature from cephalic parameters in south-eastern Nigerian population. J. Scientific & Innovative Research. 2013;2(2):425–432. [Google Scholar]
- 9.Zhuang Z, Bradtmiller B. Head-and-face anthropometric survey of U.S. respirator users. J. Occup. Environ. Hyg. 2005;2(11):567–576. doi: 10.1080/15459620500324727. [DOI] [PubMed] [Google Scholar]
- 10.Hauge J, Roe M, Brosseau LM, Colton C. Real-time fit of a respirator during simulated health care tasks. J. Occup. Environ. Hyg. 2012;9(10):563–571. doi: 10.1080/15459624.2012.711699. [DOI] [PubMed] [Google Scholar]
- 11.Zhuang Z, Landsittel D, Benson S, Roberge R, Shaffer R. Facial anthropometric differences among gender, ethnicity, and age groups. Ann. Occup. Hyg. 2010;54(4):391–402. doi: 10.1093/annhyg/meq007. [DOI] [PubMed] [Google Scholar]
- 12.American Heart Association [May 5, 2014];Obesity Information. 2014 Available at http://www.heart.org/HEARTORG/GettingHealthy/WeightManagement/Obesity/Obesity-Information_UCM_307908_Article.jsp.
- 13.Reither EN, Hause RM, Swallen KC. Looks that kill: predicting adult health and mortality from adolescent facial characteristics in yearbook photographs. Center for Demography and Ecology, University of Wisconsin-Madison; [May 8, 2014]. Wording Paper No. 2006-11. Available at http://www.ssc.wisc.edu/wlsresearch/publications/files/_private/Reither-Hauser-Swallen_Looks.That.Kill_CDE_2006-11.pdf. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Levine JA, Ray A, Jensen MD., MD Relation between chubby cheeks and visceral fat. (Correspondence) New Engl. J. Med. 1998;339(26):1946–1947. doi: 10.1056/NEJM199812243392619. [DOI] [PubMed] [Google Scholar]
- 15.Gunderson EP. Childbearing and obesity in women: weight before, during, and after pregnancy. Obstet. Gynecol. Clin. North Am. 2009;36(2):317–332. doi: 10.1016/j.ogc.2009.04.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Gunderson EP, Abrams B. Epidemiology of gestational weight gain and body weight changes after pregnancy. Epidem. Rev. 2000;22(2):261–274. doi: 10.1093/oxfordjournals.epirev.a018038. [DOI] [PubMed] [Google Scholar]
- 17.Clapp JF, III, Seaward BL, Sleamaker RH, Hiser J. Maternal physiologic adaptations to early human pregnancy. Am. J. Obstet. Gynecol. 1988;159(6):1456–1460. doi: 10.1016/0002-9378(88)90574-1. [DOI] [PubMed] [Google Scholar]
- 18.Lederman SA, Paxton A, B Heymsfield S, Wang J, Thornton J J, Pierson RN., Jr Body fat and water changes during pregnancy in women with different body weight and weight gain. Obstet. Gynecol. 1997;90(4 pt 1):483–488. doi: 10.1016/s0029-7844(97)00355-4. [DOI] [PubMed] [Google Scholar]
- 19.Soltani H, Fraser RB RB. A longitudinal study of maternal anthropometric changes in normal weight, overweight and obese women during pregnancy and postpartum. Br. J. Nutrition. 2000;84(1):95–101. doi: 10.1017/s0007114500001276. [DOI] [PubMed] [Google Scholar]
- 20.Laferty EA, McKay RT RT. Physiological effects and measurement of carbon dioxide and oxygen levels during qualitative respirator fit testing. J. Chem. Health Safety. 2006;13(5):22–28. [Google Scholar]
- 21.Henry F, Quatresooz P, Valverde-Lopez JC, Pierard GE. Blood vessel changes during pregnancy. Am. J. Clin. Dermatol. 2006;7(1):65–69. doi: 10.2165/00128071-200607010-00006. [DOI] [PubMed] [Google Scholar]
- 22.Kumari R, Jaisankar TJ, Thappa DM. A clinical study of skin changes in pregnancy. Indian J. Dermatol. Venereol. Leprol. 2007;73(2):141–145. doi: 10.4103/0378-6323.31910. [DOI] [PubMed] [Google Scholar]
- 23.Slade PD. Awareness of body dimensions during pregnancy: an analogue study. Psychol. Med. 1977;7(2):245–252. doi: 10.1017/s0033291700029329. [DOI] [PubMed] [Google Scholar]
- 24.Johnson J, Clifton RG RG, Roberts JM, et al. Pregnancy outcomes with weight gain above or below the 2009 Institute of Medicine guidelines. Obst. Gynecol. 2013;121(5):969–975. doi: 10.1097/AOG.0b013e31828aea03. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Institute of Medicine . Assessment of the NIOSH head-and-face anthropometric survey of U.S. respirator users. The National Academies Press; Washington, D.C.: 2007. p. p37. [Google Scholar]
- 26.Deli R, Galantucci LM, Laino R, et al. Three dimensional methodology for photogrammetric acquisition of the soft tissues of the face: A new clinical-instrumental protocol. Prog. Orthodon. 2013;14.32 doi: 10.1186/2196-1042-14-32. doi.10.1186/2196-1042-14-32. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Berry Ann R, NIOSH investigation of 3M model 8000 filtering facepiece respirators as requested by the California Occupational Safety and Health Administration, Division of Occupational Safety and Health . Health Hazard Evaluation Report HEYA 2010-0044-3109 California Occupational Safety and Health Administration. Division of Occupational Safety and Health; Oakland, CA: May, 2010. [April 22, 2015]. Available at http://www.cdc.gov/niosh/hhe/reports/pdfs/2010-0044-3109.pdf. [Google Scholar]