Abstract
Research involving the lymphatic system has experienced an exponential progression during the past decade largely because of advancement of modern technology and discovery of several lymphatic specific molecules. The eye provides an excellent site for lymphatic studies due to its accessible location and the unique feature of tissue heterogeneity – while some tissues are lymphatic-rich, others are lymphatic-free or -inducible. This review provides an update on our current understanding of ocular lymphatics and possible associated eye diseases.
Keywords: lymphatics, lymphatic pathway, lymphangiogenesis, eye/ocular disease
The lymphatic system was first described in the 17th century (1) at almost the same time as the blood circulation. However, compared to blood vessels which have been studied intensively in the past, lymphatics have suffered centuries of ignorance. Unlike blood vessels, lymphatics are not easily visible. Anatomically, the lymphatic network differs from that of blood circulation in that a) it is a unidirectional channel rather than a circuit; and b) lymphatic capillaries have large interendothelial gaps without tight junctions, pericytes, or a continuous basement membrane. These anatomical features have been used heavily to identify the lymphatics, particularly in earlier studies. The recent discovery of several lymphatic endothelial molecules and the advancement of modern molecular and imaging technology have ignited intensive research with rapid progress in the field (2–7). Among these lymphatic-specific molecules are VEGFR-3 (vascular endothelial growth factor receptor-3), LYVE-1 (lymphatic vessel endothelial hyaluronan receptor-1), podoplanin (a transmembrane glycoprotein), and Prox-1 (a transcription factor) (8–11). The list of lymphatic factors and markers will continue to expand as more investigations are carried out in the field.
In parallel to the blood circulatory system, the lymphatic network penetrates most tissues in the body and plays critical roles in many functions, which include but are not limited to immune responses, cancer metastasis, fat and vitamin absorption, and body fluid regulation. Numerous diseases and conditions are therefore associated with lymphatic dysfunctions, such as inflammatory diseases, transplant rejection, diabetes, autoimmune diseases, AIDS, and lymphedema (2–4,12,13). To date, there is little effective treatment for many of these disorders, and these remain fields with continuing and increasing demand for new therapeutic protocols.
Unlike most tissues in the body which are normally endowed with lymphatic vessels, ocular tissues are by nature heterogeneous: while the conjunctiva is rich in lymphatics, the cornea and the retina are devoid of them. However, lymphangiogenesis is induced in the inflamed cornea. It was also recently reported that a large population of non-endothelial LYVE-1+ cells resides in most ocular tissues (14,15). This tissue heterogeneity is summarized in Table 1.
TABLE 1.
Lymphatic Characteristics of Ocular Tissues
| Category | Tissues |
|---|---|
| Lymphatic-rich | Eyelids, lacrimal glands, conjunctiva, limbus, optic nerve sheath, extraocular muscles, connective tissues of the extraocular muscle cones, choroid (avian eyes) |
| Lymphatic-free | Cornea, lens, iris, ciliary body, retina, choroid, sclera |
| Lymphatic-inducible | Cornea, iris, ciliary body |
| LYVE-1+ cells | Cornea, conjunctiva, limbus, iris, ciliary body, choroid, retina, sclera, extraocular muscles, optic nerve sheath |
Due to its accessible location and the unique feature of tissue heterogeneity, the eye provides an excellent site for lymphatic studies. A broad spectrum of lymphatic disorders has also been identified in the eye, whether they are local forms or ocular manifestations of systemic diseases. While some ocular tissues have been intensively studied and others are yet to be elucidated, this review provides an update on our current understanding of ocular lymphatics and possible associated eye diseases.
TISSUE HETEROGENEITY
Cornea
The cornea is the most well studied and characterized tissue in ocular lymphatic research. As the forefront medium in the passage of light to the retina, it by nature maintains transparency and is devoid of any vasculatures. The presence, longevity, and importance of lymphatic vessels in the cornea under pathological situations were questioned for a long time, but it is now known that: (a) lymphatics are induced in the cornea after inflammatory, infectious, traumatic, chemical or toxic insults (Fig. 1) (14,16–24); (b) corneal lymphatics can be induced independently of blood vessels (23); and (c) the lymphatic pathway is absolutely critical for the induction of corneal transplantation immunity (4,22,25,26).
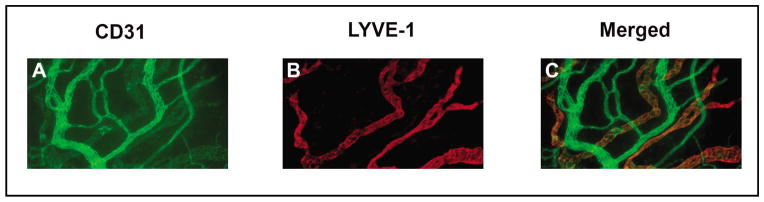
Fig. 1.
Representative micrographs showing newly developed lymphatics (LYVE-1highCD31low) in the inflamed cornea. Red: LYVE-1 (a lymphatic marker); Green: CD-31 (a panendothelial marker); Merged: yellow. Original magnification: X100.
Corneal transplantation is the most common and successful form of solid-tissue transplantation in humans with a two-year survival rate of 90 percent on uninflamed (low-risk) corneas. However, this rate is greatly reduced to less than 50 percent on inflamed and vascularized (high-risk) corneas (4,27–30). Unfortunately, many patients who are blind as a result of corneal diseases fall in this high-rejection category. To date, there is no effective management of this situation. The pharmacotherapy of corneal transplant rejection has changed little over the past decades with corticosteroids of limited efficacy and fraught with side effects such as glaucoma, cataracts, and opportunistic infections.
As demonstrated in Fig. 2, the immune reflex arc in corneal transplantation mainly consists of the following components (i) the afferent pathway of lymphatic vessels through which antigens and antigen presenting cells migrate to the draining lymph nodes, (ii) the lymph nodes where T cell priming occurs, and (iii) the efferent pathway of blood vessels through which the primed T cells are homed to the targeted corneal grafts. Once induced, corneal lymphatics enhance the high-volume delivery of antigens and antigen-presenting cells and accelerate inflammation and transplant rejection (4,29). Interestingly, it has been shown that surgical severing of the lymphatic pathway leads to 100 (low-risk) and 90 (high-risk) percent transplant survival in mice (25,26). However, surgical lymphadenectomy for promoting transplant survival is not practical in humans. It is therefore essential to understand the molecular mechanisms underlying this pathway - a prerequisite to discover new therapeutic targets. It is becoming increasingly evident that a variety of factors are involved in lymphatic processes and their molecular blockade promotes corneal transplant survival (22,24,31–33).
Fig. 2.
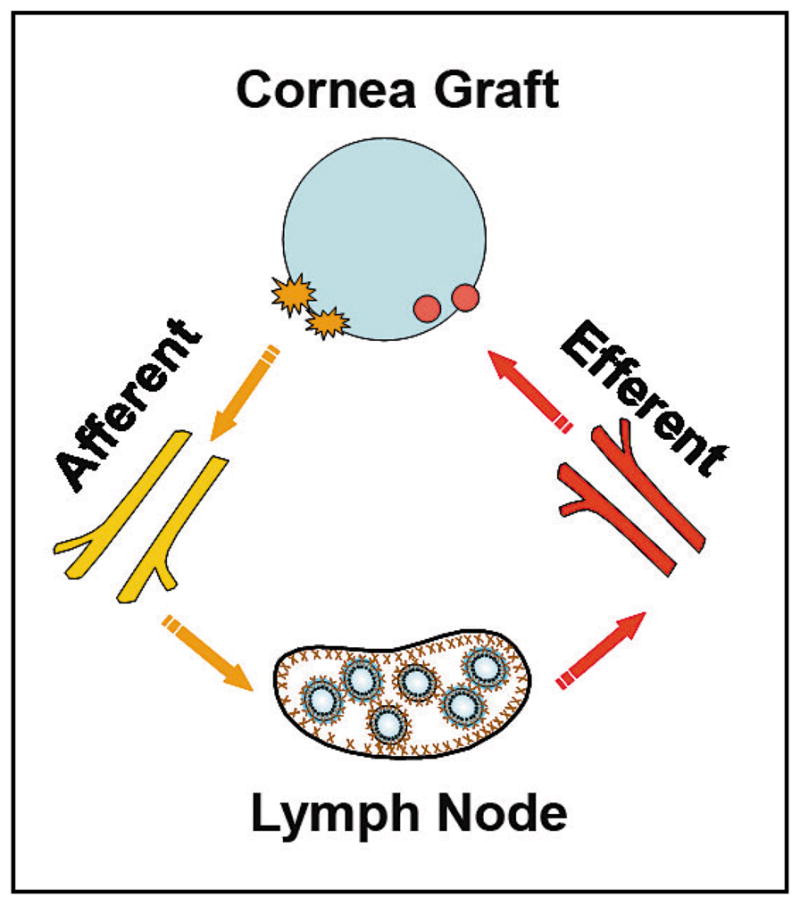
Importance of lymphatic and blood vessels as entry and exit processes of the immune reflex arc involved in corneal transplant rejection. Yellow: lymphatics of the afferent pathway facilitating antigen-presenting cell trafficking; Red: blood vessels of the efferent pathway facilitating T cell infiltration to the graft.
From a broader perspective point of view, the cornea provides an ideal tissue for lymphatic studies due to its accessible location, transparent nature, and lymphatic-free and -inducible characteristics. A variety of corneal models have been designed for lymphatic research including models of chemical burns, suture placement, micropocket implantation, and transplantation. It is anticipated that results from corneal studies will also shed light on our understanding of other lymphatic related diseases. The fruitfulness of using the cornea for lymphatic studies can also be predicted from the fact that during the past decades, more than one third of our basic knowledge on blood vessels is derived from studies with the cornea (personal communication, Judah Folkman).
Conjunctiva
In contrast to the cornea, normal conjunctiva is endowed with both blood and lymphatic vessels (14,34–39) which support the essential metabolic functions of the tissue as well as provision of cellular immune effectors to the anterior compartment of the eye. Little is known about the mechanisms by which the clear vascular distinction between the two neighboring tissues is achieved and what resources are utilized to transform the cornea into a lymphatic-rich tissue when the system is challenged under patho-inflammatory conditions. Two recent studies demonstrated that normal conjunctiva is endowed with a large population of bone marrow-derived LYVE-1+ cells of macrophage lineage (Fig. 3) (14,15). Although there has been no clear evidence, it is plausible to hypothesize that these cells might contribute to corneal lymphangiogenesis during inflammation. The close link between these two systems was also indicated by a recent study demonstrating that the conjunctival lymphatics dilated during corneal inflammation after mustard gas insult (40).
Fig. 3.
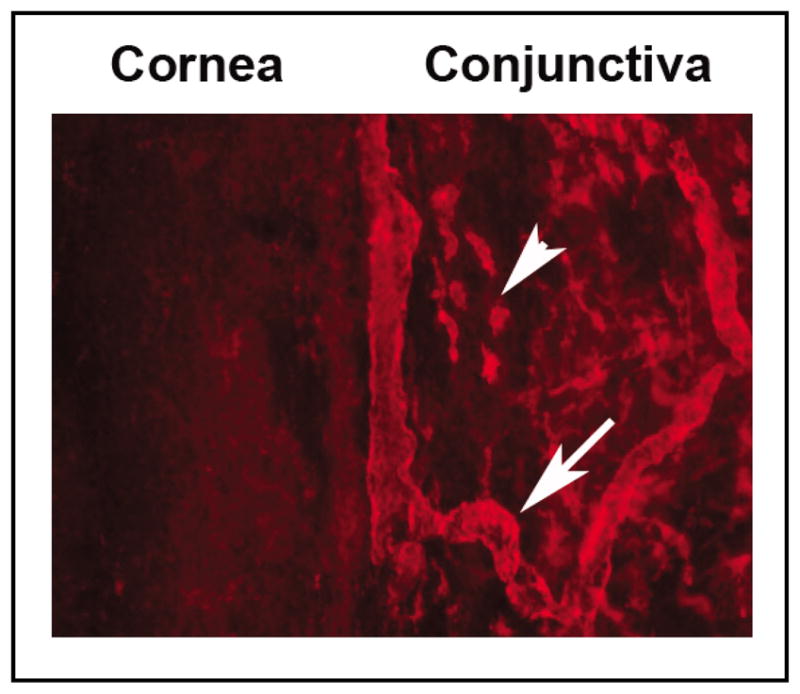
Representative micrographs demonstrating the lymphatic-rich (arrow) conjunctiva and the lymphatic-free cornea. A number of LYVE-1+ cells (arrowhead) also exist in the limbus and conjunctiva. Original magnification: X100.
Uveal Tract
Consisting of three major structures, the iris, ciliary body, and choroid, the uveal tract is normally devoid of any lymphatics in vertebrates. However, lymphatics are present in avian choroid, and they drain into the venous system (41–43). Additionally, lymphatic dilation is also found in avian models of myopia (44,45).
Distinctive from the alymphatic cornea, which is also devoid of blood vessels, the uveal tract is rich in blood supply. It also contains numerous LYVE-1+ cells (15,46), among which a unique population also co-express Sca-1 in the iris root, indicating that they are lymphatic progenitor cells (15). It is speculated that these cells might supply uveal lymphangiogenesis under pathological situations. Allied to this are two recent studies illustrating that lymphangiogenesis was induced in the iris after lens prickling (47) and in the ciliary body in melanomas with extraocular extension (48). However, the sources of the cells contributing to the active lymphangiogenesis were never elucidated, and clear evidence linking the progenitor cells in the iris root to the newly formed lymphatics is still missing.
Retina
Similar to the uveal tract, the normal retina is rich in blood vessels but absent of lymphatics. Though it was reported previously that cervical lymphostasis resulted in lymphostatic retinopathy (49), there has been no definite demonstration of inducible lymphangiogenesis in this tissue. It was also recently found that the retina is normally endowed with a number of LYVE-1+ cells (15), of which the functional roles are yet to be determined. It will be interesting to investigate whether the retina maintains alymphatic status under all circumstances. If this turns out to be true, this tissue will provide a superb site to explore potentially powerful mechanisms of lymphatic inhibition.
Others
The long held notion that lymphatics are present in ocular tissues of the eyelids, lacrimal glands, optic nerve sheath, and extraocular muscles was also confirmed by modern technology (15,35,37,38,50–54). Not surprisingly, LYVE-1+ cells also populate these sites (15). However, whether these cells function to contribute to active lymphangio-genesis is still a mystery.
LYMPHATIC ASSOCIATED EYE DISORDERS
Vision is the most vulnerable of our five senses. A wide array of ocular disorders have been identified to be associated with lymphatic dysfunction. Among them are inflammatory diseases (4,16–21,24,55,56), tumor and cancer metastasis (48,57–67), transplant rejection (22,25,26,31,32,68), venous lymphatic malformations (69–73), surgical complications (74–76), and ocular manifestations of numerous systemic diseases (77–95). These clinical phenotypes and their lymphatic abnormalities are summarized in Table 2. Several examples of ocular abnormalities in hereditary lymphedema syndromes are also illustrated in Fig. 4 (87).
TABLE 2.
Clinical Phenotypes and Associated Lymphatic Findings
| Clinical Presentation* | Lymphatic Abnormalities |
|---|---|
| Cancer and tumor metastasis | Lymphatic invasion |
| Conjunctival myxoma | Lymphatic dilation |
| Conjunctival Lymphangiectasia | Lymphatic dilation |
| Chemosis | Lymphatic defects or blockade |
| Mustard gas keratitis | Conjunctival lymphatic dilation |
| Corneal inflammation | Lymphangiogenesis |
| Transplant rejection | Lymphatic drainage |
| Orbital cellulitis | Impaired lymphatic drainage |
| Pilomatricoma | Lymphatic dilation |
| Chalazion | Flattened lymphatics |
| Dermatochalasis | Lymphatic dilation |
| Blepharochalasis | Lymphatic proliferation and dilation |
| Avian myopia | Lymphatic distension |
| Harlequin and Horner syndromes | Lymphatic surgery complication |
| Hyperthyroidism/Myxedema | Lymphatic dilation |
| Lymphatic filariasis | Lymphatic dissemination |
| Toxoplasmosis | Lymphatic dissemination |
| Tuberculosis | Lymphatic dissemination |
| Trichinosis | Lymphatic dissemination |
| Conjunctival kaposi’s sarcoma | Lymphovascular neoplasm |
| Meige syndrome/Conjunctival edema | Lymphatic structural defects |
| Milroy’s disease/Eyelid and conjunctival edema | Lymphedema |
| Lymphedema-ptosis syndrome | Lymphedema |
| Lymphedema-distichiasis syndrome | Lymphatic hyperplasia |
| Lymphedema-hypoparathyroidism syndrome | Lymphedema |
| Mucke syndrome/Conjunctival edema | Lymphedema |
| Chorioretinal dysplasia-lymphedema syndrome | Lymphedema |
| Melkersson-Rosenthal syndrome/Eyelid edema | Lymphatic dilatation |
| Lymphedematous rosacea/Eyelid edema | Impaired lymphatic drainage |
| Turner’s syndrome/Conjunctival chemosis | Lymphangiectasis |
| Noonan syndrome/Ptosis and hypertelorism | Intestinal lymphangiectasia |
| Persistent müllerian derivatives | Intestinal lymphangiectasia |
| Behcet’s disease | Intestinal lymphangiectasia |
| Venous-lymphatic malformations/Lymphangiomas | Lymphatic malformation |
Local forms or systemic diseases with ocular manifestations.
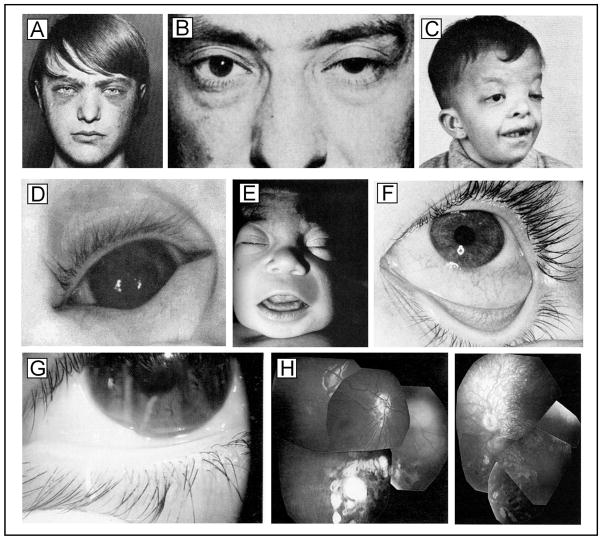
Fig. 4.
Ocular abnormalities in hereditary lymphedema syndromes. A. Ptosis, conjunctival edema, and medial eyebrow flare in Lymphedema-hypoparathyroidism syndrome. B. Unilateral ptosis in Lymphedema-ptosis syndrome. C. Ptosis and hypertelorism in Noonan syndrome with intestinal lymphangiectasia. D. Ectropion uveae and E. Bilateral subepicanthal folds with facial edema in Persistent mullerian derivatives with intestinal lymphangiectasia. F. Conjunctival edema and chemosis in Mucke syndrome. G. Distichiasis and chemosis in Lymphedema-distichiasis syndrome. H. Punched-out lesions in the retina of siblings with Chorioretinal dysplasia-lymphedema syndrome. Composite reproduced with permission from Northup et. al., Lymphology (87) with original permissions and citations.
Not included in Table 2 are several other phenotypes for which the lymphatic association is neither conclusive nor fully understood. For example, we recently discovered a distinctive LYVE-1+ cellular network in the hyaloid vascular system (HVS), a transient structure nourishing the embryonic lens and the primary vitreous of developing eyes (96). It is known that failure of HVS regression leads to several serious blinding ocular pathologies such as persistent hyperplastic tunica vasculosa lentis (PHTVL), persistent hyperplastic primary vitreous (PHPV), and persistent prepupillary membrane (PPM) (97). Glaucoma represents another example of ambiguity: while one study failed to detect the similarity between lymphatics and aqueous drainage channels (98), another concluded that the inner wall of the Schlemm’s canal shared endothelial characteristics of initial lymphatics (99). Allied to this latter study were results from several earlier studies demonstrating that (i) months after trabeculectomy, lymphatic vessels were identified in the newly formed transscleral channel (100); and (ii) the lymphatic drainage partnered with the veins to enable aqueous humour outflow after filtering operations (101,102). In the case of sympathetic ophthalmia, there has been no clear-cut evidence on its lymphatic association. However, it was indicated that the exposure of ocular antigens to subconjunctival lymphatics might play an important role in its pathogenesis (103,104).
CONCLUSIONS
Great progress has been achieved in ocular lymphatic research during the past few years. However, our knowledge differs greatly among ocular tissues and is still rather limited in many areas. With improvements in technology, increased knowledge, and joint efforts from diverse disciplines, we expect to witness many exciting discoveries in the near future.
Given its unique feature of tissue heterogeneity and the vast arrays of study models that can be derived from it, the eye will continue to serve as an excellent site for lymphatic research. It is anticipated that beyond its contributions to ocular diseases, research on the eye, a window to the body, will additionally shed light for the discovery of new therapeutic protocols for other lymphatic related diseases.
Acknowledgments
This work is supported in part by research grants from National Institutes of Health and the University of California at Berkeley. The author thanks Peter Mallen for graphical assistance.
References
- 1.Aselli G. De lactibus sive lacteis venis. Milan. Mediolani: 1627. [Google Scholar]
- 2.Alitalo K, Tammela T, Petrova TV. Lymphangiogenesis in development and human disease. Nature. 2005;438:946–953. doi: 10.1038/nature04480. [DOI] [PubMed] [Google Scholar]
- 3.Brown P. Lymphatic system: unlocking the drains. Nature. 2005;436:456–458. doi: 10.1038/436456a. [DOI] [PubMed] [Google Scholar]
- 4.Cursiefen C, Chen L, Dana MR, et al. Corneal lymphangiogenesis: Evidence, mechanisms, and implications for corneal transplant immunology. Cornea. 2003;22:273–281. doi: 10.1097/00003226-200304000-00021. [DOI] [PubMed] [Google Scholar]
- 5.Folkman J, Kaipainen A. Genes tell lymphatics to sprout or not. Nat Immunol. 2004;5:11–12. doi: 10.1038/ni0104-11. [DOI] [PubMed] [Google Scholar]
- 6.Jackson DG. The lymphatics revisited: New perspectives from the hyaluronan receptor LYVE-1. Trends Cardiovasc Med. 2003;13:1–7. doi: 10.1016/s1050-1738(02)00189-5. [DOI] [PubMed] [Google Scholar]
- 7.Oliver G, Detmar M. The rediscovery of the lymphatic system: Old and new insights into the development and biological function of the lymphatic vasculature. Genes Dev. 2002;16:773–783. doi: 10.1101/gad.975002. [DOI] [PubMed] [Google Scholar]
- 8.Kaipainen A, Korhonen J, Mustonen T, et al. Expression of the fms-like tyrosine kinase 4 gene becomes restricted to lymphatic endothelium during development. Proc Natl Acad Sci USA. 1995;92:3566–3570. doi: 10.1073/pnas.92.8.3566. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Banerji S, Ni J, Wang SX, et al. LYVE-1, a new homologue of the CD44 glycoprotein, is a lymph-specific receptor for hyaluronan. J Cell Biol. 1999;144:789–801. doi: 10.1083/jcb.144.4.789. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Breiteneder-Geleff S, Soleiman A, Horvat R. Podoplanin—a specific marker for lymphatic endothelium expressed in angiosarcoma. Verh Dtsch Ges Pathol. 1999;83:270–275. [PubMed] [Google Scholar]
- 11.Wigle JT, Oliver G. Prox1 function is required for the development of the murine lymphatic system. Cell. 1999;98:769–778. doi: 10.1016/s0092-8674(00)81511-1. [DOI] [PubMed] [Google Scholar]
- 12.Witte MH, Bernas MJ, Martin CP. Lymphangiogenesis and lymphangiodysplasia: From molecular to clinical lymphology. Microsc Res Tech. 2001;55:122–145. doi: 10.1002/jemt.1163. [DOI] [PubMed] [Google Scholar]
- 13.Rockson SG. Diagnosis and management of lymphatic vascular disease. J Am Coll Cardiol. 2008;52:799–806. doi: 10.1016/j.jacc.2008.06.005. [DOI] [PubMed] [Google Scholar]
- 14.Chen L, Cursiefen C, Barabino S. Novel expression and characterization of lymphatic vessel endothelial hyaluronate receptor 1 (LYVE-1) by conjunctival cells. Invest Ophthalmol Vis Sci. 2005;46:4536–4540. doi: 10.1167/iovs.05-0975. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Xu H, Chen M, Reid DM. LYVE-1-positive macrophages are present in normal murine eyes. Invest Ophthalmol Vis Sci. 2007;48:2162–2171. doi: 10.1167/iovs.06-0783. [DOI] [PubMed] [Google Scholar]
- 16.Collin HB. Endothelial cell lined lymphatics in the vascularized rabbit cornea. Invest Ophthalmol. 1966;5:337–354. [PubMed] [Google Scholar]
- 17.Collin HB. Ultrastructure of lymphatic vessels in the vascularized rabbit cornea. Exp Eye Res. 1970;10:207–213. doi: 10.1016/s0014-4835(70)80029-x. [DOI] [PubMed] [Google Scholar]
- 18.Collin HB. A quantitative electron microscopic study of growing corneal lymphatic vessels. Exp Eye Res. 1974;18:171–180. doi: 10.1016/0014-4835(74)90104-3. [DOI] [PubMed] [Google Scholar]
- 19.Iwamoto T, Smelser GK. Electron microscope studies on the mast cells and blood and lymphatic capillaries of the human corneal limbus. Invest Ophthalmol. 1965;4:815–834. [PubMed] [Google Scholar]
- 20.Junghans BM, Collin HB. Limbal lymphangiogenesis after corneal injury: An autoradiographic study. Curr Eye Res. 1989;8:91–100. doi: 10.3109/02713688909013898. [DOI] [PubMed] [Google Scholar]
- 21.Szalay J, Pappas GD. Fine structure of rat corneal vessels in advanced stages of wound healing. I. Permeability to intravenously injected thorium dioxide. Microvasc Res. 1970;2:319–329. doi: 10.1016/0026-2862(70)90022-1. [DOI] [PubMed] [Google Scholar]
- 22.Chen L, Hamrah P, Cursiefen C. Vascular endothelial growth factor receptor-3 mediates induction of corneal alloimmunity. Nat Med. 2004;10:813–815. doi: 10.1038/nm1078. [DOI] [PubMed] [Google Scholar]
- 23.Chang LK, Garcia-Cardena G, Farnebo F. Dose-dependent response of FGF-2 for lymphangiogenesis. Proc Natl Acad Sci USA. 2004;101:11658–11663. doi: 10.1073/pnas.0404272101. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Cursiefen C, Chen L, Borges LP. VEGF-A stimulates lymphangiogenesis and hemangiogenesis in inflammatory neovascularization via macrophage recruitment. J Clin Invest. 2004;113:1040–1050. doi: 10.1172/JCI20465. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Yamagami S, Dana MR. The critical role of lymph nodes in corneal alloimmunization and graft rejection. Invest Ophthalmol Vis Sci. 2001;42:1293–1298. [PubMed] [Google Scholar]
- 26.Yamagami S, Dana MR, Tsuru T. Draining lymph nodes play an essential role in alloimmunity generated in response to high-risk corneal transplantation. Cornea. 2002;21:405–409. doi: 10.1097/00003226-200205000-00014. [DOI] [PubMed] [Google Scholar]
- 27.The collaborative Transplantation Studies Research Group. The Collaborative Corneal Transplantation Studies (CCTS) Effectiveness of histocompatibility matching in high-risk corneal transplantation. Arch Ophthalmol. 1992;110:1392–1403. [PubMed] [Google Scholar]
- 28.Maguire MG, Stark WJ, Gottsch JD. Risk factors for corneal graft failure and rejection in the collaborative corneal transplantation studies. Collaborative Corneal Transplantation Studies Research Group. Ophthalmology. 1994;101:1536–1547. doi: 10.1016/s0161-6420(94)31138-9. [DOI] [PubMed] [Google Scholar]
- 29.Chong EM, Dana MR. Graft failure IV. Immunologic mechanisms of corneal transplant rejection. Int Ophthalmol. 2008;28:209–222. doi: 10.1007/s10792-007-9099-9. [DOI] [PubMed] [Google Scholar]
- 30.Streilein JW, Yamada J, Dana MR. Anterior chamber-associated immune deviation, ocular immune privilege, and orthotopic corneal allografts. Transplant Proc. 1999;31:1472–1475. doi: 10.1016/s0041-1345(99)00010-x. [DOI] [PubMed] [Google Scholar]
- 31.Hos D, Bock F, Dietrich T. Inflammatory corneal (lymph)angiogenesis is blocked by VEGFR-tyrosine kinase inhibitor ZK 261991, resulting in improved graft survival after corneal transplantation. Invest Ophthalmol Vis Sci. 2008;49:1836–1842. doi: 10.1167/iovs.07-1314. [DOI] [PubMed] [Google Scholar]
- 32.Cursiefen C, Cao J, Chen L. Inhibition of hemangiogenesis and lymphangiogenesis after normal-risk corneal transplantation by neutralizing VEGF promotes graft survival. Invest Ophthalmol Vis Sci. 2004;45:2666–2673. doi: 10.1167/iovs.03-1380. [DOI] [PubMed] [Google Scholar]
- 33.Chen L, Huq S, Gardner H. Very late antigen 1 blockade markedly promotes survival of corneal allografts. Arch Ophthalmol. 2007;125:783–788. doi: 10.1001/archopht.125.6.783. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Freeman LE, Troutt HF. Lymph drainage of the conjunctiva: topographic anatomic study in calves. Am J Vet Res. 1985;46:1967–1970. [PubMed] [Google Scholar]
- 35.Dickinson AJ, Gausas RE. Orbital lymphatics: Do they exist? Eye. 2006;20:1145–1148. doi: 10.1038/sj.eye.6702378. [DOI] [PubMed] [Google Scholar]
- 36.Gusev AM. the Lymphatic Vessels of the Human Conjunctiva. Arkh Anat Gistol Embriol. 1963;45:81–87. [PubMed] [Google Scholar]
- 37.Sherman DD, Gonnering RS, Wallow IH. Identification of orbital lymphatics: enzyme histochemical light microscopic and electron microscopic studies. Ophthal Plast Reconstr Surg. 1993;9:153–169. [PubMed] [Google Scholar]
- 38.Gausas RE, Gonnering RS, Lemke BN. Identification of human orbital lymphatics. Ophthal Plast Reconstr Surg. 1999;15:252–259. doi: 10.1097/00002341-199907000-00006. [DOI] [PubMed] [Google Scholar]
- 39.Weingeist TA. Fine structure and function of ocular tissues. The conjunctiva. Int Ophthalmol Clin. 1973;13:85–91. [PubMed] [Google Scholar]
- 40.Javadi MA, Yazdani S, Sajjadi H. Chronic and delayed-onset mustard gas keratitis: Report of 48 patients and review of literature. Ophthalmology. 2005;112:617–625. doi: 10.1016/j.ophtha.2004.09.027. [DOI] [PubMed] [Google Scholar]
- 41.De Stefano ME, Mugnaini E. Fine structure of the choroidal coat of the avian eye. Lymphatic vessels. Invest Ophthalmol Vis Sci. 1997;38:1241–1260. [PubMed] [Google Scholar]
- 42.De Stefano ME, Mugnaini E. Fine structure of the choroidal coat of the avian eye. Vascularization, supporting tissue and innervation. Anat Embryol (Berl) 1997;195:393–418. doi: 10.1007/s004290050060. [DOI] [PubMed] [Google Scholar]
- 43.Junghans BM, Crewther SG, Crewther DP. Lymphatic sinusoids exist in chick but not in rabbit choroid. Aust NZ J Ophthalmol. 1997;25(Suppl 1):S103–105. doi: 10.1111/j.1442-9071.1997.tb01772.x. [DOI] [PubMed] [Google Scholar]
- 44.Liang H, Crewther SG, Crewther DP. Structural and elemental evidence for edema in the retina, retinal pigment epithelium, and choroid during recovery from experimentally induced myopia. Invest Ophthalmol Vis Sci. 2004;45:2463–2474. doi: 10.1167/iovs.03-1009. [DOI] [PubMed] [Google Scholar]
- 45.Junghans BM, Crewther SG, Liang H. A role for choroidal lymphatics during recovery from form deprivation myopia? Optom Vis Sci. 1999;76:796–803. doi: 10.1097/00006324-199911000-00028. [DOI] [PubMed] [Google Scholar]
- 46.Schroedl F, Brehmer A, Neuhuber WL. The normal human choroid is endowed with a significant number of lymphatic vessel endothelial hyaluronate receptor 1 (LYVE-1)-positive macrophages. Invest Ophthalmol Vis Sci. 2008;49:5222–5229. doi: 10.1167/iovs.08-1721. [DOI] [PubMed] [Google Scholar]
- 47.Kanao T, Miyachi Y. Lymphangiogenesis promotes lens destruction and subsequent lens regeneration in the newt eyeball, and both processes can be accelerated by transplantation of dendritic cells. Dev Biol. 2006;290:118–124. doi: 10.1016/j.ydbio.2005.11.017. [DOI] [PubMed] [Google Scholar]
- 48.Heindl LM, Hofmann TN, Knorr HL. Intraocular Lymphangiogenesis in Malignant Melanomas of the Ciliary Body with Extraocular Extension. Invest Ophthalmol Vis Sci. 2009 doi: 10.1167/iovs.08-2935. [DOI] [PubMed] [Google Scholar]
- 49.Foldi M. Insufficiency of the cervical lymph vessel system; lymphostatic encephalopathy and retinopathy following cervical block dissection. Laryngol Rhinol Otol (Stuttg) 1988;67:435–437. [PubMed] [Google Scholar]
- 50.Cook BE, Jr, Lucarelli MJ, Lemke BN. Eyelid lymphatics I: Histochemical comparisons between the monkey and human. Ophthal Plast Reconstr Surg. 2002;18:18–23. doi: 10.1097/00002341-200201000-00004. [DOI] [PubMed] [Google Scholar]
- 51.Cook BE, Jr, Lucarelli MJ, Lemke BN. Eyelid lymphatics II: A search for drainage patterns in the monkey and correlations with human lymphatics. Ophthal Plast Reconstr Surg. 2002;18:99–106. doi: 10.1097/00002341-200203000-00003. [DOI] [PubMed] [Google Scholar]
- 52.McGetrick JJ, Wilson DG, Dortzbach RK. A search for lymphatic drainage of the monkey orbit. Arch Ophthalmol. 1989;107:255–260. doi: 10.1001/archopht.1989.01070010261033. [DOI] [PubMed] [Google Scholar]
- 53.Killer HE, Laeng HR, Groscurth P. Lymphatic capillaries in the meninges of the human optic nerve. J Neuroophthalmol. 1999;19:222–228. [PubMed] [Google Scholar]
- 54.Gausas RE. Advances in applied anatomy of the eyelid and orbit. Curr Opin Ophthalmol. 2004;15:422–425. doi: 10.1097/01.icu.0000139303.24272.8d. [DOI] [PubMed] [Google Scholar]
- 55.Collin HB. Ocular lymphatics. Arch Am Acad Optom. 1966;43:96–106. doi: 10.1097/00006324-196602000-00004. [DOI] [PubMed] [Google Scholar]
- 56.Gruntzig J, Schicha H, Huth F. Eye and lymph drainage. Z Lymphol. 1979;3:35–45. [PubMed] [Google Scholar]
- 57.Grossniklaus HE. Tumor vascularity and hematogenous metastasis in experimental murine intraocular melanoma. Trans Am Ophthalmol Soc. 1998;96:721–752. [PMC free article] [PubMed] [Google Scholar]
- 58.Thosani MK, Schneck G, Jones EC. Periocular squamous cell carcinoma. Dermatol Surg. 2008;34:585–599. doi: 10.1111/j.1524-4725.2007.34115.x. [DOI] [PubMed] [Google Scholar]
- 59.Harris MS, Harris GJ, Simons KB. Massive extraocular extension and parotid lymph node metastasis of uveal melanoma. Ophthal Plast Reconstr Surg. 2007;23:430–432. doi: 10.1097/IOP.0b013e31814fb450. [DOI] [PubMed] [Google Scholar]
- 60.Ardjomand N, Komericki P, Langmann G. Lymph node metastases arising from uveal melanoma. Wien Klin Wochenschr. 2005;117:433–435. doi: 10.1007/s00508-005-0329-8. [DOI] [PubMed] [Google Scholar]
- 61.De Stefani A, Lerda W, Usai A. Squamous cell carcinoma of the lacrimal drainage system: Case report and literature review. Tumori. 1998;84:506–510. doi: 10.1177/030089169808400414. [DOI] [PubMed] [Google Scholar]
- 62.Soysal HG, Markoc F. Invasive squamous cell carcinoma of the eyelids and periorbital region. Br J Ophthalmol. 2007;91:325–329. doi: 10.1136/bjo.2006.102673. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63.Kivela T, Tarkkanen A. The Merkel cell and associated neoplasms in the eyelids and periocular region. Surv Ophthalmol. 1990;35:171–187. doi: 10.1016/0039-6257(90)90087-c. [DOI] [PubMed] [Google Scholar]
- 64.Reifler DM, Hornblass A. Squamous cell carcinoma of the eyelid. Surv Ophthalmol. 1986;30:349–365. doi: 10.1016/0039-6257(86)90089-5. [DOI] [PubMed] [Google Scholar]
- 65.Johnson TE, Tabbara KF, Weatherhead RG. Secondary squamous cell carcinoma of the orbit. Arch Ophthalmol. 1997;115:75–78. doi: 10.1001/archopht.1997.01100150077013. [DOI] [PubMed] [Google Scholar]
- 66.Esmaeli B. Sentinel node biopsy as a tool for accurate staging of eyelid and conjunctival malignancies. Curr Opin Ophthalmol. 2002;13:317–323. doi: 10.1097/00055735-200210000-00005. [DOI] [PubMed] [Google Scholar]
- 67.Ho VH, Ross MI, Prieto VG. Sentinel lymph node biopsy for sebaceous cell carcinoma and melanoma of the ocular adnexa. Arch Otolaryngol Head Neck Surg. 2007;133:820–826. doi: 10.1001/archotol.133.8.820. [DOI] [PubMed] [Google Scholar]
- 68.Bachmann BO, Bock F, Wiegand SJ. Promotion of graft survival by vascular endothelial growth factor a neutralization after high-risk corneal transplantation. Arch Ophthalmol. 2008;126:71–77. doi: 10.1001/archopht.126.1.71. [DOI] [PubMed] [Google Scholar]
- 69.Kafil-Hussain N, Khooshabeh R, Graham C. Superficial adnexal lymphangioma. Orbit. 2005;24:141–143. doi: 10.1080/01676830590926549. [DOI] [PubMed] [Google Scholar]
- 70.Smoker WR, Gentry LR, Yee NK. Vascular lesions of the orbit: more than meets the eye. Radiographics. 2008;28:185–204. doi: 10.1148/rg.281075040. quiz 325. [DOI] [PubMed] [Google Scholar]
- 71.Harris GJ, Sakol PJ, Bonavolonta G. An analysis of thirty cases of orbital lymphangioma. Pathophysiologic considerations and management recommendations. Ophthalmology. 1990;97:1583–1592. doi: 10.1016/s0161-6420(90)32370-9. [DOI] [PubMed] [Google Scholar]
- 72.Selva D, Strianese D, Bonavolonta G. Orbital venous-lymphatic malformations (lymphangiomas) mimicking cavernous hemangiomas. Am J Ophthalmol. 2001;131:364–370. doi: 10.1016/s0002-9394(00)00826-6. [DOI] [PubMed] [Google Scholar]
- 73.Katz SE, Rootman J, Vangveeravong S. Combined venous lymphatic malformations of the orbit (so-called lymphangiomas). Association with noncontiguous intracranial vascular anomalies. Ophthalmology. 1998;105:176–184. doi: 10.1016/s0161-6420(98)92058-9. [DOI] [PubMed] [Google Scholar]
- 74.Levine MR, Davies R, Ross J. Chemosis following blepharoplasty: An unusual complication. Ophthalmic Surg. 1994;25:593–596. [PubMed] [Google Scholar]
- 75.Darvall JN, Morsi AW, Penington A. Coexisting harlequin and Horner syndromes after paediatric neck dissection: A case report and a review of the literature. J Plast Reconstr Aesthet Surg. 2008;61:1382–1384. doi: 10.1016/j.bjps.2007.04.008. [DOI] [PubMed] [Google Scholar]
- 76.Gugutschkova P, Angelov B. Lymphatic congestion of the conjunctiva after pre-auricular lymph node excision. Klin Monatsbl Augenheilkd. 1995;207:54–55. doi: 10.1055/s-2008-1035351. [DOI] [PubMed] [Google Scholar]
- 77.Rubegni P, Fimiani M, Tosi GM. Conjunctival edema and alopecia of the external third of the eyebrows in a patient with Meige syndrome. Graefes Arch Clin Exp Ophthalmol. 2000;238:98–100. doi: 10.1007/s004170050017. [DOI] [PubMed] [Google Scholar]
- 78.Hierholzer K, Finke R. Myxedema. Kidney Int Suppl. 1997;59:S82–89. [PubMed] [Google Scholar]
- 79.Bernardini FP, Kersten RC, Khouri LM. Chronic eyelid lymphedema and acne rosacea. Report of two cases. Ophthalmology. 2000;107:2220–2223. doi: 10.1016/s0161-6420(00)00429-2. [DOI] [PubMed] [Google Scholar]
- 80.Morales-Burgos A, Alvarez Del Manzano G, Sanchez JL. Persistent eyelid swelling in a patient with rosacea. PR Health Sci J. 2009;28:80–82. [PubMed] [Google Scholar]
- 81.Lai TF, Leibovitch I, James C. Rosacea lymphoedema of the eyelid. Acta Ophthalmol Scand. 2004;82:765–767. doi: 10.1111/j.1600-0420.2004.00335.x. [DOI] [PubMed] [Google Scholar]
- 82.Akarsu C, Atasoy P, Erdogan S. Bilateral upper eyelid edema in Melkersson-Rosenthal syndrome. Ophthal Plast Reconstr Surg. 2005;21:243–245. doi: 10.1097/01.iop.0000159177.56965.a6. [DOI] [PubMed] [Google Scholar]
- 83.Higuchi T, Satoh T, Yokozeki H. Palpebral edema as a cutaneous manifestation of hyperthyroidism. J Am Acad Dermatol. 2003;48:617–619. doi: 10.1067/mjd.2003.36. [DOI] [PubMed] [Google Scholar]
- 84.Tsuchiya M, Hibi T, Mizuno Y. Comparative, immunological studies on lymphangiectasia of the small intestine revealed in protein losing gastroenteropathy and Behcet’s disease. Gastroenterol Jpn. 1976;11:88–99. doi: 10.1007/BF02776704. [DOI] [PubMed] [Google Scholar]
- 85.Macher AM, Palestine A, Masur H. Multicentric Kaposi’s sarcoma of the conjunctiva in a male homosexual with the acquired immunodeficiency syndrome. Ophthalmology. 1983;90:879–884. doi: 10.1016/s0161-6420(83)80011-6. [DOI] [PubMed] [Google Scholar]
- 86.Ramasubramanian A, Shields CL, Palamar M. Conjunctival edema and distichiasis in association with congenital lymphedema of the lower legs. Ophthal Plast Reconstr Surg. 2009;25:148–150. doi: 10.1097/IOP.0b013e31819a44a1. [DOI] [PubMed] [Google Scholar]
- 87.Northup KA, Witte MH, Witte CL. Syndromic classification of hereditary lymphedema. Lymphology. 2003;36:162–189. [PubMed] [Google Scholar]
- 88.Dahlberg PJ, Borer WZ, Newcomer KL. Autosomal or X-linked recessive syndrome of congenital lymphedema, hypoparathyroidism, nephropathy, prolapsing mitral valve, and brachytelephalangy. Am J Med Genet. 1983;16:99–104. doi: 10.1002/ajmg.1320160115. [DOI] [PubMed] [Google Scholar]
- 89.Vallet HL, Holtzapple PG, Eberlein WR. Noonan syndrome with intestinal lymphangiectasis. A metabolic and anatomic study. J Pediatr. 1972;80:269–274. doi: 10.1016/s0022-3476(72)80589-4. [DOI] [PubMed] [Google Scholar]
- 90.Bellini C, Bonioli E, Josso N. Persistence of Mullerian derivatives and intestinal lymphangiectasis in two newborn brothers: confirmation of the Urioste syndrome. Am J Med Genet. 2001;104:69–74. doi: 10.1002/ajmg.1599. [DOI] [PubMed] [Google Scholar]
- 91.Urioste M, Rodriguez JI, Barcia JM. Persistence of mullerian derivatives, lymphangiectasis, hepatic failure, postaxial polydactyly, renal and craniofacial anomalies. Am J Med Genet. 1993;47:494–503. doi: 10.1002/ajmg.1320470413. [DOI] [PubMed] [Google Scholar]
- 92.Mucke J, Hoepffner W, Scheerschmidt G. Early onset lymphoedema, recessive form—a new form of genetic lymphoedema syndrome. Eur J Pediatr. 1986;145:195–198. doi: 10.1007/BF00446064. [DOI] [PubMed] [Google Scholar]
- 93.Kolin T, Johns KJ, Wadlington WB. Hereditary lymphedema and distichiasis. Arch Ophthalmol. 1991;109:980–981. doi: 10.1001/archopht.1991.01080070092042. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 94.Casteels I, Devriendt K, Van Cleynenbreugel H. Autosomal dominant microcephaly—lymphoedema-chorioretinal dysplasia syndrome. Br J Ophthalmol. 2001;85:499–500. doi: 10.1136/bjo.85.4.496d. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 95.Bloom D. Hereditary lymphedema (Nonne-Milroy-Meige). Report of a family with hereditary lymphedema associated with ptosis of the eyelids in several generations. New York J Med. 1941;41:856–863. [Google Scholar]
- 96.Saint-Geniez M, D’Amore PA. Development and pathology of the hyaloid, choroidal and retinal vasculature. Int J Dev Biol. 2004;48:1045–1058. doi: 10.1387/ijdb.041895ms. [DOI] [PubMed] [Google Scholar]
- 97.Ito M, Yoshioka M. Regression of the hyaloid vessels and pupillary membrane of the mouse. Anat Embryol (Berl) 1999;200:403–411. doi: 10.1007/s004290050289. [DOI] [PubMed] [Google Scholar]
- 98.Krohn J, Rodahl E. Expression of 5′-nucleotidase and alkaline phosphatase in human aqueous drainage channels. Acta Ophthalmol Scand. 2002;80:642–651. doi: 10.1034/j.1600-0420.2002.800616.x. [DOI] [PubMed] [Google Scholar]
- 99.Ramos RF, Hoying JB, Witte MH. Schlemm’s canal endothelia, lymphatic, or blood vasculature? J Glaucoma. 2007;16:391–405. doi: 10.1097/IJG.0b013e3180654ac6. [DOI] [PubMed] [Google Scholar]
- 100.van der Zypen E, Fankhauser F, Kwasniewska S. The mechanism of aqueous outflow following trabeculectomy. A light and electron microscopic study. Int Ophthalmol. 1989;13:219–228. doi: 10.1007/BF02028215. [DOI] [PubMed] [Google Scholar]
- 101.Benedikt O. The mode of action of trabeculectomy (author’s transl) Klin Monatsbl Augenheilkd. 1975;167:679–685. [PubMed] [Google Scholar]
- 102.Benedikt O. The effect of filtering operations (author’s transl) Klin Monatsbl Augenheilkd. 1977;170:10–19. [PubMed] [Google Scholar]
- 103.Albert DM, Frederick A, Jakobiec MD. Principles and Practice of Ophthalmology. W.B. Saunders Company; New York: 2007. [Google Scholar]
- 104.Rao NA, Robin J, Hartmann D, et al. The role of the penetrating wound in the development of sympathetic ophthalmia experimental observations. Arch Ophthalmol. 1983;101:102–104. doi: 10.1001/archopht.1983.01040010104019. [DOI] [PubMed] [Google Scholar]