Abstract
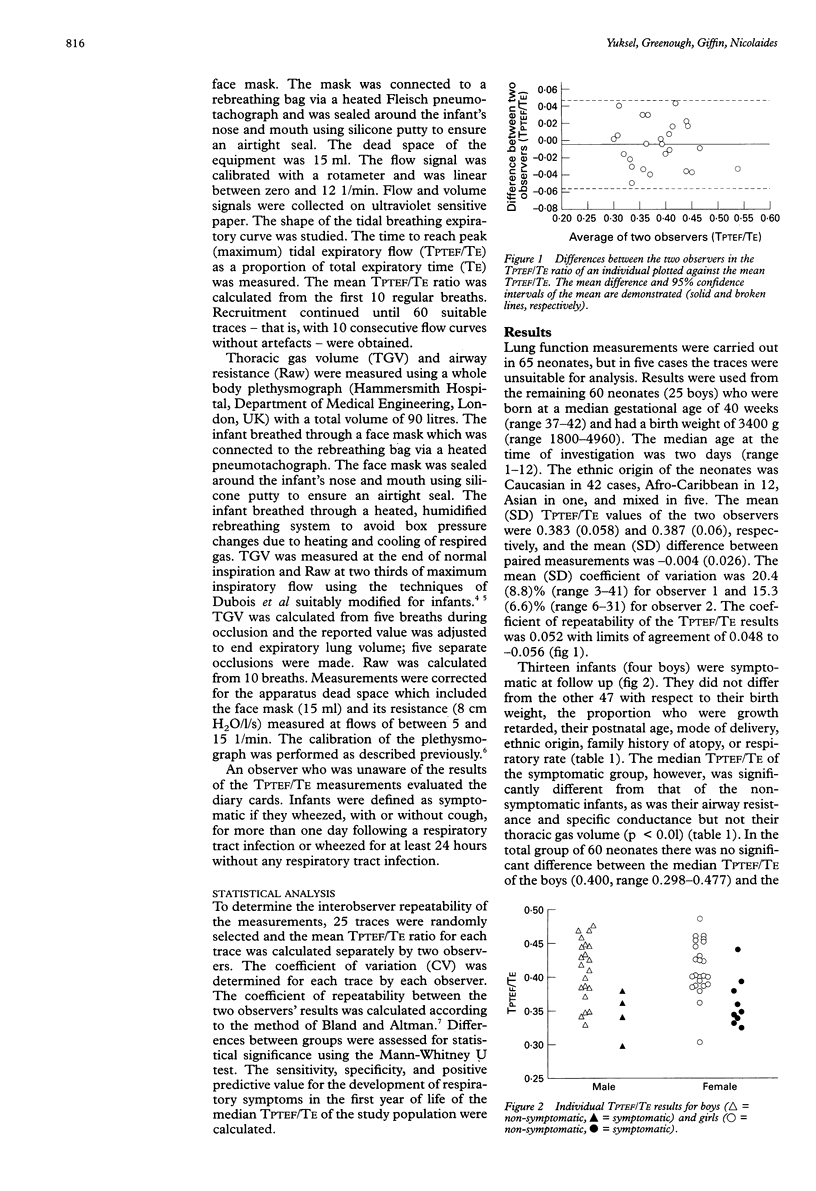
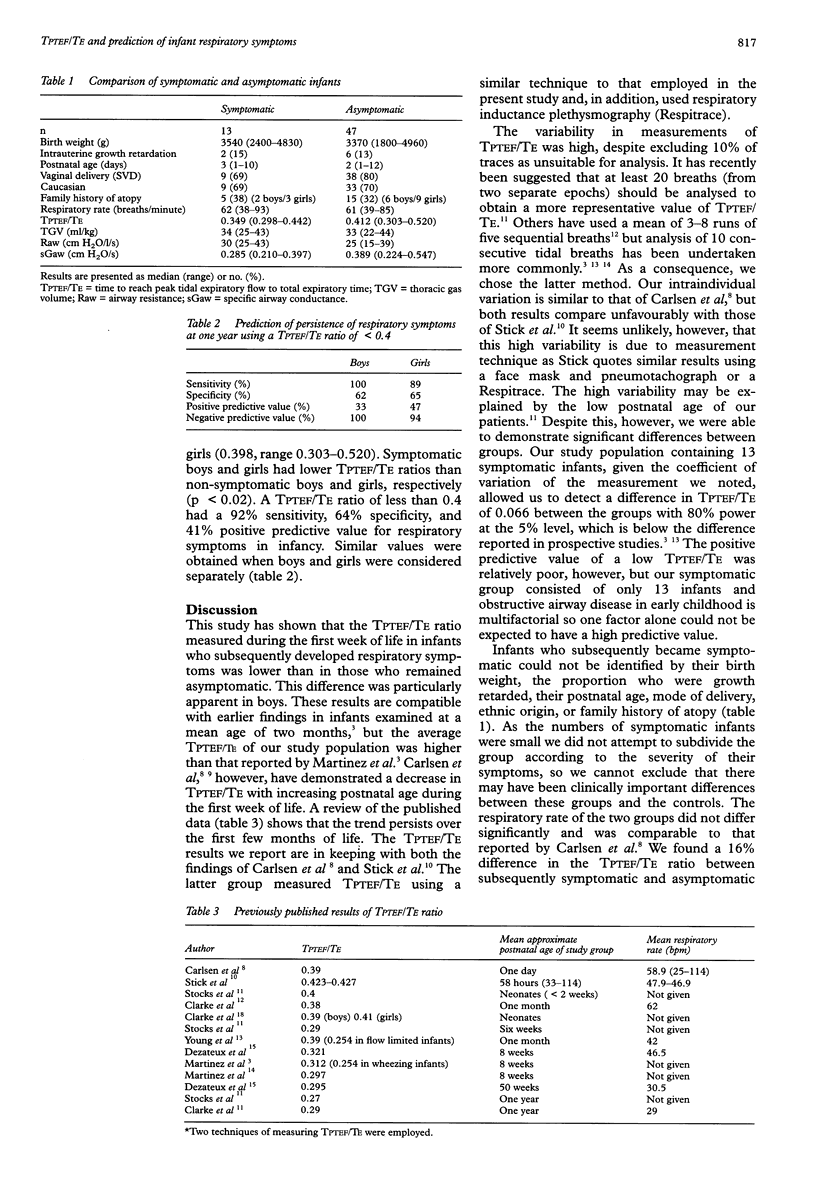
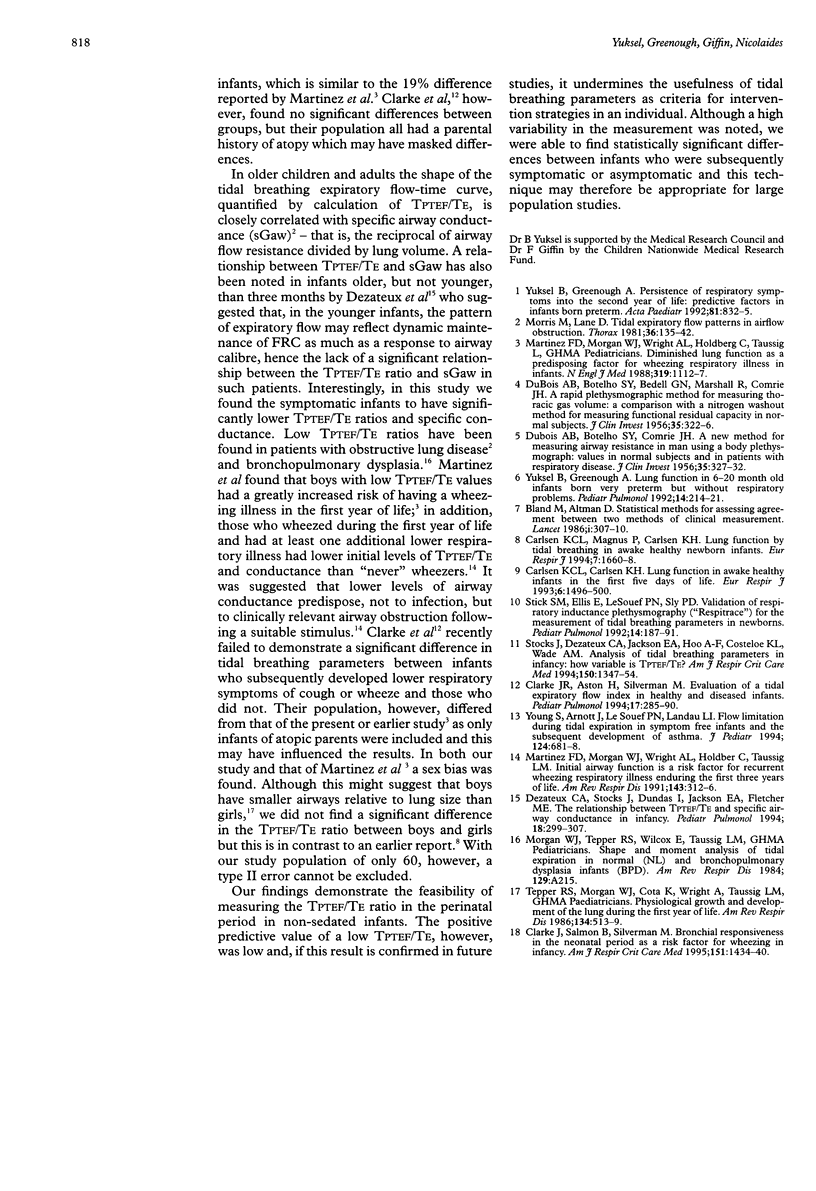
BACKGROUND: Assessment of tidal breathing parameters may be a useful method of predicting respiratory problems in early childhood. Low values of TPTEF/TE (the ratio of the proportion of time to reach peak tidal expiratory flow to total expiratory time) outside the neonatal period have been significantly related to respiratory tract illness with wheezing in boys in the first year of life. METHODS: TPTEF/TE measurements in the perinatal period were evaluated in nonsedated infants and the predictive value of this early measurement for subsequent respiratory morbidity during infancy was assessed. Flow during tidal breathing was measured while the infant slept quietly in a plethysmograph using a Fleisch pneumotachograph inserted into an infant face mask. Recruitment continued until traces from 60 infants with 10 consecutive flow curves without artefacts were obtained. In addition, plethysmographic measurements of airway resistance (Raw) and thoracic gas volume (TGV) were measured and specific conductance (sGaw) calculated. Parents recorded their infant's cough and wheeze during the first 12 months of life. RESULTS: Sixty five measurements were made in 60 infants with a mean age of two days and gestational age of 40 weeks. Two observers separately calculated TPTEF/TE ratios on 25 traces randomly selected from the pool of 60. The mean difference between the two observers was -0.004 (limits of agreement 0.048 to -0.056). Thirteen infants became symptomatic (wheeze, with or without cough); their median TPTEF/TE ratio (0.349) was significantly lower than the rest of the cohort (median 0.412) and they also had significantly higher Raw and lower sGaw. The positive predictive value of a low TPTEF/TE ratio, however, was only 41%. CONCLUSIONS: These results suggest that the use of this test in the prediction of future respiratory disease in an individual is limited.
Full text
PDF
Selected References
These references are in PubMed. This may not be the complete list of references from this article.
- Bland J. M., Altman D. G. Statistical methods for assessing agreement between two methods of clinical measurement. Lancet. 1986 Feb 8;1(8476):307–310. [PubMed] [Google Scholar]
- Clarke J. R., Aston H., Silverman M. Evaluation of a tidal expiratory flow index in healthy and diseased infants. Pediatr Pulmonol. 1994 May;17(5):285–290. doi: 10.1002/ppul.1950170504. [DOI] [PubMed] [Google Scholar]
- Clarke J. R., Salmon B., Silverman M. Bronchial responsiveness in the neonatal period as a risk factor for wheezing in infancy. Am J Respir Crit Care Med. 1995 May;151(5):1434–1440. doi: 10.1164/ajrccm.151.5.7735597. [DOI] [PubMed] [Google Scholar]
- DUBOIS A. B., BOTELHO S. Y., BEDELL G. N., MARSHALL R., COMROE J. H., Jr A rapid plethysmographic method for measuring thoracic gas volume: a comparison with a nitrogen washout method for measuring functional residual capacity in normal subjects. J Clin Invest. 1956 Mar;35(3):322–326. doi: 10.1172/JCI103281. [DOI] [PMC free article] [PubMed] [Google Scholar]
- DUBOIS A. B., BOTELHO S. Y., COMROE J. H., Jr A new method for measuring airway resistance in man using a body plethysmograph: values in normal subjects and in patients with respiratory disease. J Clin Invest. 1956 Mar;35(3):327–335. doi: 10.1172/JCI103282. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dezateux C. A., Stocks J., Dundas I., Jackson E. A., Fletcher M. E. The relationship between tPTEF:tE and specific airway conductance in infancy. Pediatr Pulmonol. 1994 Nov;18(5):299–307. doi: 10.1002/ppul.1950180507. [DOI] [PubMed] [Google Scholar]
- Lødrup Carlsen K. C., Magnus P., Carlsen K. H. Lung function by tidal breathing in awake healthy newborn infants. Eur Respir J. 1994 Sep;7(9):1660–1668. doi: 10.1183/09031936.94.07091660. [DOI] [PubMed] [Google Scholar]
- Lødrup-Carlsen K. C., Carlsen K. H. Lung function in awake healthy infants: the first five days of life. Eur Respir J. 1993 Nov;6(10):1496–1500. [PubMed] [Google Scholar]
- Martinez F. D., Morgan W. J., Wright A. L., Holberg C. J., Taussig L. M. Diminished lung function as a predisposing factor for wheezing respiratory illness in infants. N Engl J Med. 1988 Oct 27;319(17):1112–1117. doi: 10.1056/NEJM198810273191702. [DOI] [PubMed] [Google Scholar]
- Martinez F. D., Morgan W. J., Wright A. L., Holberg C., Taussig L. M. Initial airway function is a risk factor for recurrent wheezing respiratory illnesses during the first three years of life. Group Health Medical Associates. Am Rev Respir Dis. 1991 Feb;143(2):312–316. doi: 10.1164/ajrccm/143.2.312. [DOI] [PubMed] [Google Scholar]
- Morris M. J., Lane D. J. Tidal expiratory flow patterns in airflow obstruction. Thorax. 1981 Feb;36(2):135–142. doi: 10.1136/thx.36.2.135. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Stick S. M., Ellis E., LeSouëf P. N., Sly P. D. Validation of respiratory inductance plethysmography ("Respitrace") for the measurement of tidal breathing parameters in newborns. Pediatr Pulmonol. 1992 Nov;14(3):187–191. doi: 10.1002/ppul.1950140308. [DOI] [PubMed] [Google Scholar]
- Stocks J., Dezateux C. A., Jackson E. A., Hoo A. F., Costeloe K. L., Wade A. M. Analysis of tidal breathing parameters in infancy: how variable is TPTEF:TE? Am J Respir Crit Care Med. 1994 Nov;150(5 Pt 1):1347–1354. doi: 10.1164/ajrccm.150.5.7952563. [DOI] [PubMed] [Google Scholar]
- Tepper R. S., Morgan W. J., Cota K., Wright A., Taussig L. M. Physiologic growth and development of the lung during the first year of life. Am Rev Respir Dis. 1986 Sep;134(3):513–519. doi: 10.1164/arrd.1986.134.3.513. [DOI] [PubMed] [Google Scholar]
- Young S., Arnott J., Le Souef P. N., Landau L. I. Flow limitation during tidal expiration in symptom-free infants and the subsequent development of asthma. J Pediatr. 1994 May;124(5 Pt 1):681–688. doi: 10.1016/s0022-3476(05)81355-1. [DOI] [PubMed] [Google Scholar]
- Yuksel B., Greenough A. Lung function in 6-20 month old infants born very preterm but without respiratory troubles. Pediatr Pulmonol. 1992 Dec;14(4):214–221. doi: 10.1002/ppul.1950140404. [DOI] [PubMed] [Google Scholar]
- Yuksel B., Greenough A. Persistence of respiratory symptoms into the second year of life: predictive factors in infants born preterm. Acta Paediatr. 1992 Oct;81(10):832–835. doi: 10.1111/j.1651-2227.1992.tb12113.x. [DOI] [PubMed] [Google Scholar]



