Abstract
The CKD-associated decline in soluble α-Klotho levels is considered detrimental. Some in vitro and in vivo animal studies have shown that anti-oxidant therapy can upregulate the expression of α-Klotho in the kidney. We examined the effect of anti-oxidant therapy on α-Klotho concentrations in a clinical cohort with mild tot moderate chronic kidney disease (CKD). We performed a post-hoc analysis of a prospective randomized trial involving 62 patients with mild to moderate CKD (the ATIC study), all using an angiotensin-converting enzyme inhibitor (ACEi) or angiotensin receptor blocker (ARB) for 12 months. On top of that, the intervention group received anti-oxidative therapy consisting of the combination of pravastatin (40 mg/d) and vitamin E (α-tocopherol acetate, 300 mg/d) while the placebo was not treated with anti-oxidants. α-Klotho concentrations were measured at baseline and after 12 months of anti-oxidant therapy. Data were analysed using T-tests and Generalized Estimating Equations, adjusting for potential confounders such as vitamin D, parathyroid hormone, fibroblast-growth-factor 23 (FGF23) and eGFR. The cohort existed of 62 patients with an eGFR (MDRD) of 35 ± 14 ml/min/1.72m2, 34 were male and mean age was 53.0 ± 12.5 years old. Anti-oxidative therapy did successfully reduce oxLDL and LDL concentrations (P <0.001). α-Klotho concentrations did not change in patients receiving either anti-oxidative therapy (476.9 ± 124.3 to 492.7 ± 126.3 pg/mL, P = 0.23) nor in those receiving placebo 483.2 ± 142.5 to 489.6 ± 120.3 pg/mL, P = 0.62). Changes in α-Klotho concentrations were not different between both groups (p = 0.62). No evidence was found that anti-oxidative therapy affected α-Klotho concentrations in patients with mild-moderate CKD.
Introduction
Prevention and better treatment of cardiovascular (CV) disease in CKD is one of the main challenges in current nephrology. Despite successful interventions on traditional risk factors such as blood pressure, dyslipidaemia and proteinuria, CV risk in CKD remains excessively high [1]. A rapidly increasing body of evidence supports involvement of the fibroblast growth factor 23 (FGF23)-klotho-vitamin D axis in the pathogenesis of cardiovascular disease in CKD patients [2]. Therapeutic reduction of oxidative stress in patients with CKD, for instance with HMG-CoA reductase inhibitors, could improve CV outcome [3]. However, whether antioxidant therapy induces favorable changes in the FGF23-Klotho-vitamin D axis and thereby improvements in CV outcome is unknown.
The α-Klotho gene was discovered in 1997 as an anti-aging gene [4]. α-Klotho is predominantly produced in the kidneys [5]. α-Klotho expression is downregulated by CKD-associated uremic toxins and oxidative stress and enhanced activity of the renin-angiotensin-aldosterone system (RAAS) [6–8]. A vicious circle could ensue, because vitamin D deficiency increases renin and subsequently angiotensin II, which is known to suppress α-Klotho and leads to subsequent high FGF23 concentrations, which in turn suppress vitamin D activation[9]. Lower α-Klotho concentrations are associated with progressive CKD[10], higher prevalence of cardiovascular disease[11], arterial stiffness [12], vascular calcification[13].
Therefore, increasing α-Klotho could be a legitimate goal in CKD patients. Several recent studies assessed different experimental options to up-regulate endogenous α-Klotho [7,9,14–24] through therapeutic reduction of oxidative stress with the administration of anti-oxidants [9,21,22] and HMG-CoA reductase inhibitors [23,24] However, whether anti-oxidant therapy increases α-Klotho in patients is unknown.
We hypothesized that a 12-month anti-oxidant therapy compared to placebo, induces an increase of α-Klotho. Therefore, in this study we measured α-Klotho before and after treatment with anti-oxidative therapy (vitamin E combined with a statin) or placebo in patients with mild to moderate CKD who participated in the Anti-Oxidant Therapy in Chronic Renal Insufficiency (ATIC) Study.
Methods and Materials
Study population
For the current analysis we performed a post-hoc analysis on subjects from the prospective randomised ATIC trial of whom blood and urine samples were available (25). Originally in this study 93 subjects with mild-moderate CKD (creatinine clearance of 15–70 mL/min/1.73m2 according to the Cockroft-Gault equation), on background treatment of inhibition of the renin-angiotensin system (RAS) by either angiotensin receptor blockers (ARB) or angiotensin converting enzyme (ACE)-inhibition were randomised to either a anti-oxidant regime comprising of pravastatin (40 mg/d) starting at baseline followed by the addition of vitamin E (α-tocopherol acetate, 300 mg/d) at month 6, or placebo for 12 months. Endpoints of the original study were common carotid intima-media thickness, brachial artery flow-mediated dilatation, albuminuria and renal function (eGFR). Details and results of the study have been published previously [25]. Excluded were subjects with diabetes, active vasculitis, nephrotic syndrome, renal transplantation, a fasting cholesterol level higher than 270 mg/dL (7.00 mmol/L), cholesterol-lowering therapy within 3 months prior to inclusion, or ischemic coronary, cerebrovascular, or peripheral arterial disease. The patients included in the ATIC study already provided informed consent for their samples to be stored and used in the future for research purposes without any further asking.
Data collection
Of the 93 patients from the ATIC study, complete serum samples were available from 62 patients, which formed the base of the current analysis. The following data were recorded: age, gender, body mass index, smoker or non-smoker, renal function as determined by eGFR (MDRD) and serum creatinine (μmol/L). Plasma-oxidized low-density lipoprotein (oxLDL) and malondialdehyde were measured as quantitative indicators of oxidative stress. α-Klotho and vitamin D (25(OH)D) and phosphate concentrations were measured in serum samples and parathyroid hormone (PTH) and c-terminal fibroblast-growth-factor-23 (cFGF23) concentrations in plasma samples, all at baseline and after 12 months of treatment. The α-Klotho immunoassay (IBL international GmbH, Hamburg, Germany) was used to measure α-Klotho [26] with an intra-assay variation of <5% and an inter assay variation < 7.5%; c-terminal FGF23 was measured in EDTA-plasma using ELISA (Immutopics) [27]with an intra-assay variation of <5% and an inter assay variation < 10%. 25(OH)D was measured using the radioimmunoassay (Diasorin) (intra-assay variation of <10% above a concentration of 25 nmol/L and inter assay variation < 11% above a concentration of 25 nmol/L) and PTH using an automated immunoassay (Architect Abbott Diagnostics) (both intra- and inter assay variation <5% above a concentration of 1 pmol/L). Creatinine and phosphate were measured in 24-hour urine samples. All assays were run in the year 2013.
Statistical analysis
Continuous variables are given as mean ± standard deviation for normally distributed data or as median [interquartile range] for skewed data. Categorical variables are given as number of patients and percentages. Normally distributed numerical variables were compared using an unpaired T-test, otherwise Mann-Whitney U test was used; categorical variables were compared by Chi-square test. Changes within the two treatment groups of oxLDL, LDL, MDA, eGFR and cFGF23 were analysed using paired T-test; between group differences were analysed using an unpaired T-test on deltas (Δ). In order to adjust the effects of the two treatment strategies on α-Klotho for confounders, General Estimating Equations, a regression technique suitable for longitudinal data analysis, was used. In the model with α-Klotho as dependent variable and treatment as determinant, vitamin D, parathyroid hormone, cFGF23 and renal function were added as confounders. In addition, to evaluate effect modification of the intervention, the product of time and group (time*group) was added as an independent variable in these analysis. A non-parametric correlation analysis was made between α-Klotho levels and FGF23 using Spearman’s rho. P-values < 0.05 were considered statistically significant. All analyses were performed using IBM SPSS Statistics software version 20. Details of statistical analysis are available in the S1 File.
Results
Characteristics of the study population
Data were analysed from 62 patients, 34 patients in the anti-oxidant intervention group, 28 in placebo group. In our cohort were fewer men than woman but otherwise it is a representative reflection of the original ATIC cohort. The mean age of the participants was 53 years old (range from 20–79 years old) and all patients suffered from chronic kidney disease stage 3–4 (eGFR 15–60 mL/min/1.73 m2)[28]. At baseline, there were no important differences in demographic and clinical parameters between both arms, as shown in Tables 1 and 2. Full data set available in the S2 File.
Table 1. Baseline characteristics of participants.
| Placebo group (n = 28) | Intervention group (n = 34) | |
|---|---|---|
| Age (years) | 51 ± 15 | 54 ± 11 |
| Male, no. (%) | 18 (64.3) | 16 (47.1) |
| BMI (kg/m2) | 25.9 ± 4.0 | 26.5 ± 4.9 |
| Smokers, no. (%) | 12 (52.2) | 11 (47.8) |
| eGFR (ml/min/1.73m2) | 38 (15) | 33 (13) |
| 25(OH)D (nmol/L) | 70.2 ± 31.0 | 66.9 ± 32.5 |
| PTH (pmol/L) (median + IQR) | 8.9 (5.2–13.1) | 8.6 (4.9–13.0) |
Values are expressed as mean ±SD, unless specified otherwise. IQR = interquartile range
Table 2. Time-related results within and between groups.
Values are expressed as mean with 95% confidence interval (95%CI).
| PLACEBO (n = 28) | INTERVENTION (n = 34) | p for between-group difference | |||||
|---|---|---|---|---|---|---|---|
| Baseline | After 12 months of treatment | Baseline | After 12 months of treatment | ||||
| Mean (95%CI) | Mean (95%CI) | p | Mean (95%CI) | Mean (95%CI) | p | ||
| Phosphate (mmol/L) | 1.19 (1.11–1.28) | 1.29 (1.19–1.40) | 0.01 | 1.27 (1.14–1.39) | 1.35 (1.18–1.51) | 0.26 | 0.07 |
| oxLDL (U/L) | 60.2 (53.9–66.5) | 63.4 (56.6–70.1) | 0.03 | 66.8 (62.1–71.4) | 55.1 (62.1–71.4) | <0.001 | <0.001 |
| LDL (mmol/L) | 3.2 (2.9–3.6) | 3.4 (3.0–3.7) | 0.22 | 3.8 (3.5–4.2) | 2.6 (2.3–2.9) | <0.001 | <0.001 |
| MDA (μmol/L) | 7.7 (7.1–8.2) | 8.0 (7.6–8.5) | 0.10 | 7.7 (7.2–8.1) | 7.8 (7.4–8.2) | 0.38 | 0.37 |
| eGFR (mL/min/1.73m2) | 38 (32–43) | 37 (31–43) | 0.30 | 33 (29–38) | 32 (27–37) | 0.10 | 0.60 |
| cFGF23* (RU/mL) | 150.0 (90.8–236.8) | 145.0 (95.0–359.0) | 0.001 | 181.0 (130.0–310.5) | 179.0 (137.8–318.0) | 0.14 | 0.33 |
| α-Klotho (pg/mL) | 483.2 (427.9–538.5) | 489.6 (443.0–536.3) | 0.62 | 476.9 (433.6–520.3) | 492.7 (448.6–536.7) | 0.23 | 0.62 |
| Urinary phosphate (mmol/L) | 12.3 (10.0–14.6) | 12.4 (9.8–15.0) | 0.97 | 11.6 (8.8–14.4) | 9.3 (7.7–11.0) | 0.02 | 0.32 |
* cFGF23 is expressed as median and interquartile range.
Markers of oxidative stress
After 12 months, there was a statistically significant reduction of oxLDL (from 66.8 U/L ± 13.3 to 55.2 U/L ± 12.9, P<0.001) and low-density lipoprotein cholesterol (from 3.8 ± 0.93 mmol/L to 2.6 ± 0.71mmol/L, P<0.001) levels within the intervention group. There was no reduction of plasma malondialdehyde (from 7.7 ± 1.3 μmol/L to 7.8 ± 1.1 μmol/L, P = 0.38) during the study period. Levels of oxLDL, low-density lipoprotein cholesterol and plasma malondialdehyde all increased in the placebo group (from 60.2 U/L ± 15.5 to 63.4 U/L ± 16.7, from 3.2 ± 0.8 mmol/L to 3.4 ± 0.8 mmol/L, and from 7.7 ± 1.3 μmol/L to 8.0 ± 1.2 μmol/L resp.). However, this increase was only significant in the oxLDL levels (see Table 2).
Renal function and cFGF23
After 12 months, the mean eGFR had decreased from 33 ± 13 mL/min/1.73m2 to 32 ± 14 mL/min/1.73m2 in the intervention group (P = 0.10) and decreased from 38 ± 15 mL/min/1.73m2 to 37 ± 16 mL/min/1.73m2 in the placebo group (P = 0.30) (P = 0.60 for between-group difference).
The median of cFGF23 changed from 181.0 RU/mL (IQR: 130.0–310.5) to 179.0 RU/mL (137.8–318.0) in the intervention group (P = 0.14). In the placebo group the median of cFGF23 changed from 150.0 (90.8–236.8) RU/mL to 145.0 (IQR: 95.0–359.0) RU/mL (P = 0.001) (P for between-group difference = 0.33).
Effect of anti-oxidative therapy on circulating Klotho concentrations
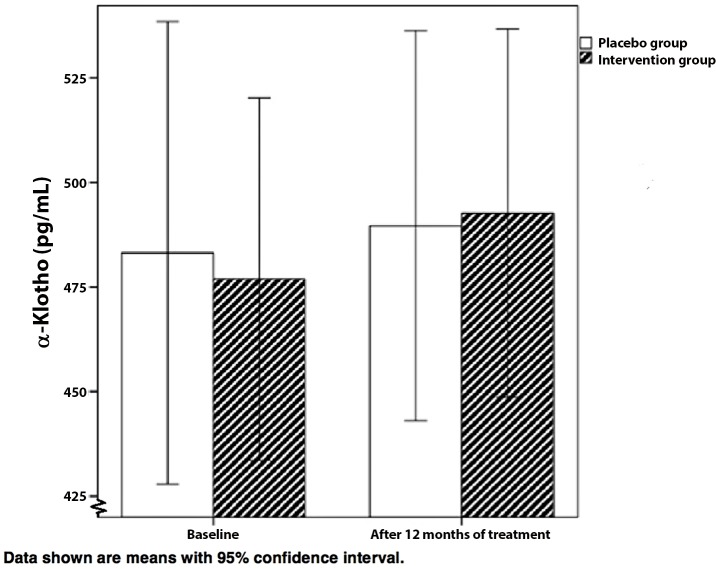
α-Klotho concentrations at baseline increased from mean 476.9 ± 124.3 pg/mL to mean 492.7 ± 126.3 pg/mL for the intervention group (P = 0.23). In the placebo group α-Klotho concentrations increased from mean 483.2 ± 142.5 pg/mL to mean 489.6 ± 120.3 pg/mL (P = 0.62). The interaction term showed that α-Klotho levels did not significantly change over time in the intervention group compared to the placebo group (P = 0.62, Fig 1, and model 2, Table 3). Adjusting for the potential confounders eGFR, cFGF23, PTH and 25 hydroxyvitamin D3 did not influence results between the groups (p = 0.89, model 3 in Table 3).
Fig 1. The effect of anti-oxidative therapy on α-Klotho concentrations.
Data shown are means with 95% confidence interval.
Table 3. The effect of anti-oxidant treatment on α-Klotho in a multivariable GEE analysis.
| Intervention versus placebo (change in pg/ml α-Klotho) | β (95% CI) |
|---|---|
| Crude | -1.6 (-62.5–59.3) |
| Model 11 | 8.4 (-53.8–70.6) |
| Model 22 | 3.6 (-62.8–70.0) |
| Model 33 | 8.9 (-71.5–89.4) |
1 Model 1: Adjusted for time course, MDRD
2 Model 2: Adjusted for variables from Model 1, plus an interaction term between group and time
3 Model 3: Adjusted for all variables from Model 2 plus 25OH-vitamin D, cFGF23, PTH, phosphate, calcium
We found no correlation between α-Klotho concentrations and cFGF23 levels (Spearman correlation coefficient = -0.045, p = 0.73).
Discussion
This study demonstrates that there is no effect of the combined treatment with pravastatin and vitamin E as anti-oxidative therapy on α-Klotho concentrations in patients with mild-moderate CKD, despite that efficacy of anti-oxidative therapy to reduce oxidative stress was demonstrated by a decline of oxLDL concentrations.
Our data contradict experimental in vitro and in vivo animal studies that showed decreased Klotho expression in the kidney following oxidative stress. Subsequent administration of a free radical scavenger prevented this Klotho downregulation by oxidative stress [7,9,21,22,29–31]. The lack of an increase in α-Klotho concentrations under clinical anti-oxidative therapy in our study could have several explanations. First of all, we measured circulating α-Klotho concentrations; most of the previous in vitro and in vivo animal studies measured renal membrane bound Klotho. Second, we do not know if the anti-oxidative therapy patients received in this study was of sufficient potency to induce an upregulation of α-Klotho. Although the decline in oxLDL was statistically significant, we cannot exclude that more pronounced attenuation of oxidative stress would have resulted in higher concentrations of α-Klotho. However, Tamura et al. treated hypercholesterolemic patients during 8 weeks with a lower dose pravastatin than in our study (10 mg/day vs 40 mg/day) and they showed a significant reduction in plasma malondialdehyde with 14±13% [32]. Administration of rosuvastatin 20mg/day reduced both oxLDL and malondialdehyde levels in patients with atherosclerotic cerebrovascular disease [33]. Supplementation of vitamin E also has shown to decrease oxidative stress in an earlier study in patients with end-stage kidney disease [34]. We were not informed about therapy compliance of the patients in the ATIC study. However, given the response in both LDL cholesterol and oxLDL this is an unlikely explanation for the lack of effects on α-Klotho.
Even more, the patients in this study all used an ACEi or ARB from at least 2 weeks before baseline. Karalliedde et al. showed that treatment with valsartan, an ARB, is associated with an increase in sKlotho levels in patients with type 2 diabetes, systolic hypertension and albuminuria [35]. It is therefore conceivable that an previous increment of α-Klotho concentrations induced by inhibitors of the RAS prevented a subsequent further rise by our anti-oxidant strategy. The patients in our study had indeed higher baseline concentrations of α-Klotho when compared to the α-Klotho concentrations in patients with CKD stage 3 and 4 mentioned in the study of Kim et al. (10)
No data on α-tocopherol concentrations are available for our study, therefore we cannot exclude that α-tocopherol concentrations were sufficient at baseline, limiting an effect of anti-oxidative therapy on α-Klotho concentrations.
There are some limitations to this study that need to be acknowledged. The sample size of 62 patients is relatively small, leaving the possibility of a type II error. This also limited the ability to correct for confounding. However, a statistically significant difference in oxidative stress, as measured by oxLDL, was found between the two treatment arms, implicating that a difference in α-Klotho would had been detected in case oxidative stress had been an important factor. We cannot rule out however that the magnitude of reduction in oxidative stress was insufficient to influence α-Klotho concentrations. In the original ATIC study however, the multistep intervention was sufficient to modulate common carotid intima media thickness, albuminuria and brachial artery flow-mediated dilation. In addition to the potential of a type II error, small sample size in general limits the external validity of our findings. Another potential weakness, as mentioned, is that all patients were using either ARB or ACE-inhibitors, which may have induced an unnoticed, increase in α-Klotho, and precluded a further increment.
Finally, the IBL-assay used to measure α-Klotho concentrations has also some shortcomings. It is uncertain if and which forms of α-Klotho are detected and a cross reactivity with other solutes cannot be excluded [26,36].
The strengths of this study are the prospectively collected data with a randomised design, and the attained contrast between treatment groups in terms of biochemical indices of oxidative stress.
In conclusion, this study could not confirm our hypothesis that anti-oxidative therapy with pravastatin and vitamin E increases α-Klotho concentrations in patients with mild-moderate CKD on background therapy with ACE-inhibitors. Further research on this topic is warranted.
Supporting Information
(SAV)
(SAV)
Acknowledgments
This work is supported by a consortium grant from the Dutch Kidney Foundation (NIGRAM Consortium, Grant No. CP10.11).
The NIGRAM consortium consists of the following principal investigators:
R. Bindels1, J.G. Hoenderop1, M.H. de Borst2, J.L. Hillebrands2, G.J. Navis2, P.M. ter Wee3 and M.G. Vervloet3#
1Department of Physiology, Radboud university medical center Nijmegen, The Netherlands.
2Department of Internal Medicine, Division of Nephrology, University Medical Center Groningen, Groningen, The Netherlands
3Department of Nephrology, VU University Medical Center, Amsterdam, The Netherlands.
# Lead author of the NIGRAM consortium (m.vervloet@vumc.nl)
Data Availability
All relevant data are within the paper and its Supporting Information files. The patients included in the ATIC study already provided informed consent for their samples to be stored and used in the future for research purposes without any further asking.
Funding Statement
The NIGRAM consortium is fully supported by the Dutch Kidney Foundation (CP10.11).
References
- 1.Foley RN, Parfrey PS, Sarnak MJ. Epidemiology of cardiovascular disease in chronic renal disease. Journal of the American Society of Nephrology: JASN. 1998;9(12 Suppl):S16–23. [PubMed] [Google Scholar]
- 2.Olauson H, Vervloet MG, Cozzolino M, Massy ZA, Urena Torres P, Larsson TE. New insights into the FGF23-Klotho axis. Seminars in nephrology. 2014;34(6):586–97. 10.1016/j.semnephrol.2014.09.005 [DOI] [PubMed] [Google Scholar]
- 3.Baigent C, Landray MJ, Reith C, Emberson J, Wheeler DC, Tomson C, et al. The effects of lowering LDL cholesterol with simvastatin plus ezetimibe in patients with chronic kidney disease (Study of Heart and Renal Protection): a randomised placebo-controlled trial. Lancet. 2011;377(9784):2181–92. 10.1016/S0140-6736(11)60739-3 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Kuro-o M, Matsumura Y, Aizawa H, Kawaguchi H, Suga T, Utsugi T, et al. Mutation of the mouse klotho gene leads to a syndrome resembling ageing. Nature. 1997;390(6655):45–51. [DOI] [PubMed] [Google Scholar]
- 5.Hu MC, Shi M, Zhang J, Pastor J, Nakatani T, Lanske B, et al. Klotho: a novel phosphaturic substance acting as an autocrine enzyme in the renal proximal tubule. FASEB journal: official publication of the Federation of American Societies for Experimental Biology. 2010;24(9):3438–50. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Kuro-o M. Klotho as a regulator of oxidative stress and senescence. Biological chemistry. 2008;389(3):233–41. 10.1515/BC.2008.028 [DOI] [PubMed] [Google Scholar]
- 7.Mitani H, Ishizaka N, Aizawa T, Ohno M, Usui S, Suzuki T, et al. In vivo klotho gene transfer ameliorates angiotensin II-induced renal damage. Hypertension. 2002;39(4):838–43. [DOI] [PubMed] [Google Scholar]
- 8.Sun CY, Chang SC, Wu MS. Suppression of Klotho expression by protein-bound uremic toxins is associated with increased DNA methyltransferase expression and DNA hypermethylation. Kidney international. 2012;81(7):640–50. 10.1038/ki.2011.445 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Yoon HE, Ghee JY, Piao S, Song JH, Han DH, Kim S, et al. Angiotensin II blockade upregulates the expression of Klotho, the anti-ageing gene, in an experimental model of chronic cyclosporine nephropathy. Nephrology, dialysis, transplantation: official publication of the European Dialysis and Transplant Association—European Renal Association. 2011;26(3):800–13. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Kim HR, Nam BY, Kim DW, Kang MW, Han JH, Lee MJ, et al. Circulating alpha-klotho levels in CKD and relationship to progression. American journal of kidney diseases: the official journal of the National Kidney Foundation. 2013;61(6):899–909. [DOI] [PubMed] [Google Scholar]
- 11.Semba RD, Cappola AR, Sun K, Bandinelli S, Dalal M, Crasto C, et al. Plasma klotho and cardiovascular disease in adults. Journal of the American Geriatrics Society. 2011;59(9):1596–601. 10.1111/j.1532-5415.2011.03558.x [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Kitagawa M, Sugiyama H, Morinaga H, Inoue T, Takiue K, Ogawa A, et al. A decreased level of serum soluble Klotho is an independent biomarker associated with arterial stiffness in patients with chronic kidney disease. PloS one. 2013;8(2):e56695 10.1371/journal.pone.0056695 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Hu MC, Shi M, Zhang J, Quinones H, Griffith C, Kuro-o M, et al. Klotho deficiency causes vascular calcification in chronic kidney disease. Journal of the American Society of Nephrology: JASN. 2011;22(1):124–36. 10.1681/ASN.2009121311 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Tsujikawa H, Kurotaki Y, Fujimori T, Fukuda K, Nabeshima Y. Klotho, a gene related to a syndrome resembling human premature aging, functions in a negative regulatory circuit of vitamin D endocrine system. Molecular endocrinology (Baltimore, Md). 2003;17(12):2393–403. [DOI] [PubMed] [Google Scholar]
- 15.Forster RE, Jurutka PW, Hsieh JC, Haussler CA, Lowmiller CL, Kaneko I, et al. Vitamin D receptor controls expression of the anti-aging klotho gene in mouse and human renal cells. Biochemical and biophysical research communications. 2011;414(3):557–62. 10.1016/j.bbrc.2011.09.117 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Haussler MR, Haussler CA, Whitfield GK, Hsieh JC, Thompson PD, Barthel TK, et al. The nuclear vitamin D receptor controls the expression of genes encoding factors which feed the "Fountain of Youth" to mediate healthful aging. The Journal of steroid biochemistry and molecular biology. 2010;121(1–2):88–97. 10.1016/j.jsbmb.2010.03.019 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Zhang H, Li Y, Fan Y, Wu J, Zhao B, Guan Y, et al. Klotho is a target gene of PPAR-gamma. Kidney international. 2008;74(6):732–9. 10.1038/ki.2008.244 [DOI] [PubMed] [Google Scholar]
- 18.Zhang R, Zheng F. PPAR-gamma and aging: one link through klotho? Kidney international. 2008;74(6):702–4. 10.1038/ki.2008.382 [DOI] [PubMed] [Google Scholar]
- 19.Yamagishi T, Saito Y, Nakamura T, Takeda S, Kanai H, Sumino H, et al. Troglitazone improves endothelial function and augments renal klotho mRNA expression in Otsuka Long-Evans Tokushima Fatty (OLETF) rats with multiple atherogenic risk factors. Hypertension research: official journal of the Japanese Society of Hypertension. 2001;24(6):705–9. [DOI] [PubMed] [Google Scholar]
- 20.Yang HC, Deleuze S, Zuo Y, Potthoff SA, Ma LJ, Fogo AB. The PPARgamma agonist pioglitazone ameliorates aging-related progressive renal injury. Journal of the American Society of Nephrology: JASN. 2009;20(11):2380–8. 10.1681/ASN.2008111138 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Saito K, Ishizaka N, Mitani H, Ohno M, Nagai R. Iron chelation and a free radical scavenger suppress angiotensin II-induced downregulation of klotho, an anti-aging gene, in rat. FEBS letters. 2003;551(1–3):58–62. [DOI] [PubMed] [Google Scholar]
- 22.Mitobe M, Yoshida T, Sugiura H, Shirota S, Tsuchiya K, Nihei H. Oxidative stress decreases klotho expression in a mouse kidney cell line. Nephron Experimental nephrology. 2005;101(2):e67–74. [DOI] [PubMed] [Google Scholar]
- 23.Kuwahara N, Sasaki S, Kobara M, Nakata T, Tatsumi T, Irie H, et al. HMG-CoA reductase inhibition improves anti-aging klotho protein expression and arteriosclerosis in rats with chronic inhibition of nitric oxide synthesis. International journal of cardiology. 2008;123(2):84–90. [DOI] [PubMed] [Google Scholar]
- 24.Narumiya H, Sasaki S, Kuwahara N, Irie H, Kusaba T, Kameyama H, et al. HMG-CoA reductase inhibitors up-regulate anti-aging klotho mRNA via RhoA inactivation in IMCD3 cells. Cardiovascular research. 2004;64(2):331–6. [DOI] [PubMed] [Google Scholar]
- 25.Nanayakkara PW, van Guldener C, ter Wee PM, Scheffer PG, van Ittersum FJ, Twisk JW, et al. Effect of a treatment strategy consisting of pravastatin, vitamin E, and homocysteine lowering on carotid intima-media thickness, endothelial function, and renal function in patients with mild to moderate chronic kidney disease: results from the Anti-Oxidant Therapy in Chronic Renal Insufficiency (ATIC) Study. Archives of internal medicine. 2007;167(12):1262–70. [DOI] [PubMed] [Google Scholar]
- 26.Heijboer AC, Blankenstein MA, Hoenderop J, de Borst MH, Vervloet MG. Laboratory aspects of circulating alpha-Klotho. Nephrology, dialysis, transplantation: official publication of the European Dialysis and Transplant Association—European Renal Association. 2013;28(9):2283–7. [DOI] [PubMed] [Google Scholar]
- 27.Heijboer AC, Levitus M, Vervloet MG, Lips P, ter Wee PM, Dijstelbloem HM, et al. Determination of fibroblast growth factor 23. Annals of clinical biochemistry. 2009;46(Pt 4):338–40. 10.1258/acb.2009.009066 [DOI] [PubMed] [Google Scholar]
- 28.Kidney Disease: Improving Global Outcomes (KDIGO) CKD Work Group. KDIGO 2012 clinical practice guideline for the evaluation and management of chronic kidney disease. Kidney Int Suppl. 2013;3:1–150. [Google Scholar]
- 29.Aizawa H, Saito Y, Nakamura T, Inoue M, Imanari T, Ohyama Y, et al. Downregulation of the Klotho gene in the kidney under sustained circulatory stress in rats. Biochemical and biophysical research communications. 1998;249(3):865–71. [DOI] [PubMed] [Google Scholar]
- 30.Nagai T, Yamada K, Kim HC, Kim YS, Noda Y, Imura A, et al. Cognition impairment in the genetic model of aging klotho gene mutant mice: a role of oxidative stress. FASEB journal: official publication of the Federation of American Societies for Experimental Biology. 2003;17(1):50–2. [DOI] [PubMed] [Google Scholar]
- 31.Yoon HE, Lim SW, Piao SG, Song JH, Kim J, Yang CW. Statin Upregulates the Expression of Klotho, an Anti-Aging Gene, in Experimental Cyclosporine Nephropathy. Nephron Experimental nephrology. 2012;120(4):e123–e33. 10.1159/000342117 [DOI] [PubMed] [Google Scholar]
- 32.Tamura A, Watanabe T, Nasu M. Effects of atorvastatin and pravastatin on malondialdehyde-modified LDL in hypercholesterolemic patients. Circulation journal: official journal of the Japanese Circulation Society. 2003;67(10):816–20. [DOI] [PubMed] [Google Scholar]
- 33.Moon GJ, Kim SJ, Cho YH, Ryoo S, Bang OY. Antioxidant effects of statins in patients with atherosclerotic cerebrovascular disease. Journal of clinical neurology (Seoul, Korea). 2014;10(2):140–7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Giray B, Kan E, Bali M, Hincal F, Basaran N. The effect of vitamin E supplementation on antioxidant enzyme activities and lipid peroxidation levels in hemodialysis patients. Clinica chimica acta; international journal of clinical chemistry. 2003;338(1–2):91–8. [DOI] [PubMed] [Google Scholar]
- 35.Karalliedde J, Maltese G, Hill B, Viberti G, Gnudi L. Effect of renin-angiotensin system blockade on soluble Klotho in patients with type 2 diabetes, systolic hypertension, and albuminuria. Clinical journal of the American Society of Nephrology: CJASN. 2013;8(11):1899–905. 10.2215/CJN.02700313 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Pedersen L, Pedersen SM, Brasen CL, Rasmussen LM. Soluble serum Klotho levels in healthy subjects. Comparison of two different immunoassays. Clinical biochemistry. 2013;46(12):1079–83. 10.1016/j.clinbiochem.2013.05.046 [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
(SAV)
(SAV)
Data Availability Statement
All relevant data are within the paper and its Supporting Information files. The patients included in the ATIC study already provided informed consent for their samples to be stored and used in the future for research purposes without any further asking.