Abstract
Objectives
Patulous Eustachian tube (PET) is a challenging clinical problem with limited medical and surgical options. The current study systematically reviews the literature to determine the safety and efficacy of surgical treatments for PET.
Data Sources
Medline, Google Scholar, and Cochrane databases.
Methods
Studies evaluating the surgical management of PET were extracted based on defined inclusion criteria. Data including surgical techniques, outcomes, and complications were extracted and analyzed.
Results
1616 studies were retrieved from the initial search. Fourteen studies comprising a total of 226 patients (253 sides) met inclusion criteria and were evaluated for surgical techniques, patient outcomes and complications. All studies were classified as Level 4 evidence per definition provided by the Oxford Center for Evidence Based Medicine. The most commonly reported techniques were ET plugging (3 studies), PE tube placement (2 studies), and suture ligation (2 studies). Postoperative follow-up ranged from 2 to 60 months (mean, 20.6 months). Outcome measures varied significantly between individual studies, with overall symptom improvement reported at between 22% and 100% (mean 72.4%, 95% CI 62.5% - 81.2%). A low incidence of minor complications was reported in 9 of 14 studies.
Conclusions
Current literature evaluating the surgical management of PET is limited and comprised entirely of Level 4 studies. Comparisons between techniques were not possible due to the small number of studies and variable outcome measures. Future larger studies evaluating defined outcomes and quality of life measures are needed to determine the comparative efficacy of surgical treatments for this challenging condition.
Keywords: Patulous Eustachian tube, Eustachian tube dysfunction, autophony, eustachian, patulous, outcomes, surgery
INTRODUCTION
The Eustachian tube (ET) is an important anatomic structure that contributes to the ventilation and overall health of the middle ear. Obstruction or dysfunction of the ET due to failure of intermittent opening of the tubal orifice can often result in chronic symptoms of pain, aural fullness, and dizziness 1-3. Unfortunately, there is also a subset of patients who experience symptoms secondary to pathologic patency of the ET. Patulous Eustachian tube (PET) was first described by Schwartze in 1864 and can result in a multitude of symptoms including voice autophony, breathing autophony, and aural fullness, among other complaints 4. Possible etiologies of PET include atrophy of the peritubal fat tissue, loss of venous tone of the pterygoid venous plexus, and peritubal musculature dysfunction 5. PET has also been associated with weight loss and pregnancy 2,5,6.
Although PET is a well-recognized pathologic entity, standardized treatment algorithms have yet to be established. Both surgical and non-surgical interventions have been described in the literature, most of which aim to narrow or close the ET pharyngeal orifice. Conservative, non-surgical methods are numerous and have included weight gain, topical estrogen, and insufflation with boric or salicylic acid 2,7. For those who fail conservative approaches, surgical intervention may be indicated. Several different surgical methods have likewise been reported including injection of bulking agents 8,9, fat/cartilage plugging 10,11, ligation of the orifice 12,13, endoluminal cauterization 14, and hamulotomy 15. Despite the multitude of treatment modalities reported in the literature, success rates have generally been variable, and no consensus on management exists. The purpose of this study is to systematically review published surgical approaches for PET and compare the safety and efficacy of individual interventions.
METHODS
Systematic Review
A comprehensive systematic literature review was performed using defined inclusion and exclusion criteria. Literature searches were independently performed for studies published between 1960 and 2014 using the Medline, Google Scholar, and Cochrane databases. Studies not published in the English language, cadaveric studies, and non-human studies were excluded, as were case reports and cases series with fewer than three patients. To be included in the systematic review, studies had to 1) Describe a surgical technique for patulous Eustachian tube, and 2) Present a quantifiable outcome measure. Titles and abstracts of retrieved articles were reviewed independently by the study authors. Any remaining articles received a full-text review by at least two authors, followed by clarification of any discrepancies. Data was subsequently extracted from individual studies and entered into a database for further analysis. Variables analyzed included number of patients, surgical technique, outcome measures and complications.
Statistical Analysis
Risk of bias was quantitatively assessed with Begg-Mazumdar and Eggar tests. A random effects (DerSimonium-Laird) model was used and heterogeneity was measured using the I2 statistic. This is a well-characterized measure of study heterogeneity that assesses the percentage of variance in a meta-analysis that may be due to heterogeneity, rather than random chance alone. StatsDirect software, version 2.8.0 was used for all calculations.
RESULTS
Systematic Review
The literature search produced a total of 1616 articles. 1464 studies were excluded based on title and/or abstract review. The majority of excluded studies were review articles, single case reports, or focused only on medical management of PET. Details of the selection process are illustrated in Figure 1. After removing duplicate articles, a total of 48 articles remained for full text review, 34 of which were subsequently excluded primarily due to a lack of defined outcome measures or due to a focus on Eustachian tube dysfunction rather than PET. A total of 14 articles were included in the systematic review, all of which were case series representing level 4 evidence.
Figure 1.
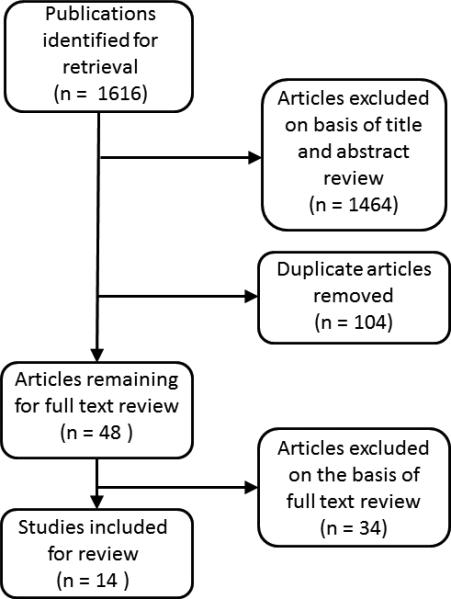
Article selection process for systemic literature search.
Patient Demographics
The 14 retrieved studies included a total of 226 patients and treatment of 253 sides (ears) (Table 1). Mean reported follow-up was 20.6 months. The most commonly reported techniques were ET plugging 7,16,17 (3 studies), PE tube placement 18,19 (2 studies), and suture ligation 12,13 (2 studies). Additional techniques included hydroxyapatite injection 20, implantation of autologous cartilage 3, diathermy 21, gelatin injection 8, cauterization 9, pterygoid hamulotomy 22, and transection/transposition of the tensor veli palatine muscle1,15.
Table 1.
Characteristics and outcomes of included studies.
| Study | Patients (Sides) | Procedure | F/U, months | Outcome measures | % Improved |
|---|---|---|---|---|---|
| Vazeafshar 2014 | 14 (23) | Endoscopic endonasal injection of hydroxyapatite | 17.5 (9-36) | Subjective improvement (complete/significant/unchange d/worse) - autophony, fullness, popping/clicking, pain, vertigo | 59 |
| Rotenberg 2013 | 11 (14) | Endoscopic endonasal multilayer closure (fat plugging, endoluminal cauterization, suture ligation) | 6 | Autophony score, Postoperative audiometry | 86 |
| Ikeda 2011 | 14 (19) | Ventilation tube placement and/or myrigotomy with ET plugging | NS | Improvement in habitual sniffing | 89 |
| Poe 2007 | 11 (14) | Endoscopic transnasal/transoral reconstruction of ET with autologous cartilage or alloderm | 15.8 (3-30) | Subjective improvement in autophony (complete/significant/unchanged/worse) | 93 |
| Takano 2006 | 10 (15) | Endoscopic transnasal/transoral ligation of eustachian tube | 13-27 | Symptom resolution and sonotubometry | 60 |
| Sato 2005 | 35 (42) | Trans-typanic insertion of silicone plug | 38.9 (6-68) | Symptom resolution, sonotubometry and tubotympanoaerodynamography | 71 |
| Dyer 1991 | 4 (4) | Trans-typanic ET occlusion via catheter with ventilation tube | NS | Symptom resolution | 100 |
| Chen 1990 | 46 (60) | Ventilation tube placement | NS | Symptom resolution | 53 |
| Robinson 1999 | 8 (9) | ET diathermy | 15.9 (3-36) | Symptom resolution | 22 |
| O'Connor 1981 | 7 (9) | ET cauterization with silver nitrate | NS | Symptom resolution | 78 |
| Bluestone 1981 | 4 (4) | Trans-typanic ET occlusion via catheter with ventilation tube | Up to 36 months | Symptom resolution | 100 |
| Virtanen 1982 | 13 (16) | Pterygoid hamulotomy with transposition or transection of tensor veli palatini tendon | 24 | Symptom resolution and sonotubometry | 69 |
| Ogawa 1976 | 16 (22) | Transnasal infusion of gelatin sponge into ET | NS | Symptom resolution | 73 |
| Stroud 1974 | 3 (3) | Transpalatal transposition of tensor veli palatini | NS | Symptom resolution | 100 |
Patient Outcomes
A wide variety of outcome measurements were used in the 14 included studies. The most commonly used method for measuring efficacy was subjective improvement or resolution of patient symptoms. A minority of studies used a defined scoring system to assess individual patient symptoms (autophony, aural fullness, etc.) 3,20. Objective measurements including sonotubometry, audiometry, and tubotympanoaerodynamography were used in four studies12,13,15,16. Rotenberg et al. performed audiograms and tympanograms 6 months after surgery and noted no impact on hearing for any study subjects 12. Virtanen et al. reported normalization of sonotubometric recordings in 9 of 16 ears following pterygoid hamulotomy with or without surgery of the tensor veli palatini muscle, consistent with patient-reported symptomatic improvement of 69% 15. The remaining two studies showed improvement in sonotubometry in a majority of patients 13,16.
Overall symptom improvement ranged between 22% and 100% (mean 72.4%, 95% CI 62.5% - 81.2%) as shown in Figure 2. No significant bias was detected using the Begg-Mazumdar (p = 0.66) and Eggar (p = 0.56) tests. The bias assessment of individual studies is presented in Figure 3. Moderate heterogeneity was identified with an I2 (inconsistency) of 62.1% (95% CI 20.7% – 77.4%), suggesting that at least some of the variance in outcomes between studies may be due to study heterogeneity. Four studies reported symptomatic improvement in 100% of study participants, however, each of these studies included 4 or fewer patients. Three studies reported symptomatic improvement in greater than 80% of study patients. These studies used variable approaches including myringotomy/tympanostomy tube placement with or without ET plugging 18, fat plugging/suture ligation 12, and reconstruction of the ET orifice with autologous cartilage 3. Surgical approaches with the lowest reported efficacy included ET diathermy (22%) 21 and ventilation tube placement (53%) 19. Comparison between techniques was difficult due to lack of a defined assessment criteria or scoring system in most studies.
Figure 2.
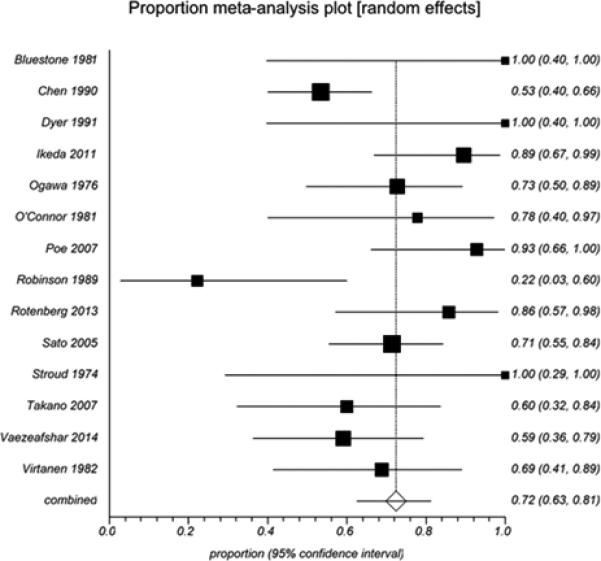
Forest plot for the success rate (% of patients with improvement in symptoms) of PET surgery.
Figure 3.
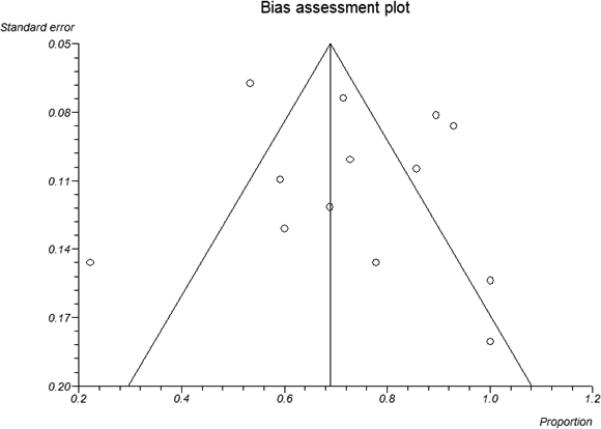
Funnel plot of study proportions for detection of publication bias.
Complications
Few complications were reported in the 14 included studies (Table 2). The most commonly reported complication was middle ear effusion, with additional complications and patient complaints including otorrhea, foreign body sensation, pain, epistaxis, and tinnitus. Few studies reported objective measures for middle ear or audiologic function following PET surgery. For most surgical approaches, the frequency of revision procedures was less than 20%. No major complications were reported.
Table 2.
Complications of PET surgery.
| Study | Patients (sides) | Procedure | Complications | Additional Procedures |
|---|---|---|---|---|
| Vazeafshar 2014 | 14 (23) | Hydroxyapatite injection | No reported complications | Repeat injection in 2 patients (4 sides) |
| Rotenberg 2013 | 11 (14) | Fat plugging, suture ligation | Epistaxis (1 patient); Need for PE tube removal (3 patients), ME effusion (1 patient) | Revision surgery in 2 ears |
| Ikeda 2011 | 14 (19) | Ventilation tube placement ± ET plugging | ME effusion (1 patient) | Plug insertion required in 2 of 8 patients initially treated with PE tube alone, ME effusion (1 patient) |
| Poe 2007 | 11 (14) | ET reconstruction with autologous cartilage | ME effusion (1 patient) | Hydroxyapatite injection in 1 patient 10 months after initial procedure |
| Takano 2006 | 10 (15) | ET ligation | ME effusion (1 patient), Persistent odynophagia (1 patient) | Revision surgery in 3 patients (3 ears) |
| Sato 2005 | 35 (42) | Insertion of silicone plug | Foreign body sensation (majority of patients) | Plug upsizing required in 11 ears; Unable to place plug due to narrow ET orifice in 2 ears |
| Dyer 1991 | 4 (4) | ET plugging with catheter | No reported complications | None reported |
| Chen 1990 | 46 (60) | Ventilation tube placement | Persistent otorrhea (2 patients); TM perforation (2 patients) | Repeated myringotomy (2-5) required in 10 ears |
| Robinson 1999 | 8 (9) | ET diathermy | ME effusion (2 patients) | None reported |
| O'Connor 1981 | 7 (9) | ET cauterization | Low incidence of ME effusion | Revision surgery in 2 patients |
| Bluestone 1981 | 4 (4) | ET plugging with catheter | No reported complications | None reported |
| Virtanen 1982 | 13 (16) | Pterygoid hamulotomy/ten sor veli palatini transposition | No reported complications | None reported |
| Ogawa 1976 | 16 (22) | Gelatin injection | Tinnitus (2 ears) | Repeated injection in 4 patients (6 ears) |
| Stroud 1974 | 3 (3) | Transposition of tensor veli palatini | No reported complications | None reported |
ME, middle ear; TM, tympanic membrane; PE, pressure equalization
DISCUSSION
Patulous Eustachian tube is a fairly rare but often frustrating clinical entity for both patient and practitioner. Medical management is sufficient in some cases but often produces limited or temporary improvement in many patients, necessitating the need for surgical intervention. Based on our systematic literature review, most surgical techniques appear to be moderately effective at addressing PE symptoms and improving patient quality of life. However, despite clinically significant improvement, many patients remain at least partially symptomatic, and overall, surgical interventions for PET appear to fall short of expected outcomes.
Surgical intervention for PET appears to be generally safe with few unique risks isolated to the individual interventions performed. The two most frequent complications appear to be middle ear effusions necessitating the need for pressure equilibrium tubes post-operatively and the need for revision surgery. Since the primary objective of surgical intervention is to narrow the pathologically patent pharyngeal orifice of the ET, these findings would seem to suggest that there may be a narrow margin between symptom relief and pathologic occlusion of the ET. It is unclear whether these complications were the result of the particular surgical methods used or due to clinical judgment made intra-operatively. There does not appear to be a significant difference in the development of middle ear sequelae between techniques, as approaches including ventilation tube placement, ET reconstruction, and suture ligation all resulted in similar rates of this particular complication. Fortunately, this and other complications reported in most studies appear amenable to relatively simple corrective interventions. Ultimately, additional studies will be required to compare different interventions, and to analyze the relationship between number of procedures performed by individual surgeons and patient outcomes.
Although most studies in this review included small patient populations, the cumulative data appears to give merit to surgical intervention as a successful means for treating recalcitrant PET. A particular limitation in this review is the lack of validated metrics and diagnostic criteria in most studies. The ability to assess outcomes and make comparisons between surgical approaches would certainly be improved through use of a widely accepted metric for quantifying symptom relief. Some studies utilized a numeric scoring system developed by Poe that uses a 1-5 scoring system to assess post-operative outcomes 3. Scores in this system signify a number of outcomes that range from complete relief to worsening, and allows for stratification based on individual symptoms. The need for a validated assessment tool is amplified by recent studies that have reported rates of patient satisfaction that lag significantly behind reported symptom improvement 12,20. Additionally, these findings demonstrate the importance of thorough pre-operative education and counseling to better prepare patients for the goals of surgery and to set realistic expectations.
The current study represents the first comprehensive and comparative review of surgical techniques for the management of PET. A variety of surgical approaches were identified through our systematic literature search. Overall rates of improvement varied between 13% and 100%, with a mean reported success rate of 72.4%. Unfortunately, there have yet to be any studies that compare individual surgical approaches and no single technique has been found to be superior in either surgical outcomes or safety. We were unable to make statistically rigorous comparisons between techniques in this review, as the individual study populations were small and included variable outcome measures. In the absence of additional data, surgeons should continue to offer interventions based on experience, personal skillset, and patient wishes.
CONCLUSIONS
Patulous Eustachian tube is a well-defined entity that is difficult to treat both medically and surgically. A wide range of surgical techniques have been described in the literature, however, studies analyzing the safety and efficacy of these techniques is limited and mostly comprised of level IV studies. In general, surgical intervention appears to be a safe treatment modality with moderate successful treatment outcomes. Future, large patient studies are needed to more accurately define surgical outcomes and identify superior surgical methods.
Footnotes
Presented at the 117th Annual Meeting of the Triological Society at COSM; May 15-16, 2014
Financial disclosures: No relevant disclosures
Conflicts of interest: None
REFERENCES
- 1.Stroud MH, Spector GJ, Maisel RH. Patulous eustachian tube syndrome. Preliminary report of the use of the tensor veli palatini transposition procedure. Arch Otolaryngol. 1974;99:419–421. doi: 10.1001/archotol.1974.00780030433006. [DOI] [PubMed] [Google Scholar]
- 2.Pulec JL, Simonton KM. Abnormal Patency of the Eustachian Tube: Report on 41 Cases. The Laryngoscope. 1964;74:267–271. doi: 10.1002/lary.5540740211. [DOI] [PubMed] [Google Scholar]
- 3.Poe DS. Diagnosis and management of the patulous eustachian tube. Otology & neurotology : official publication of the American Otological Society, American Neurotology Society [and] European Academy of Otology and Neurotology. 2007;28:668–677. doi: 10.1097/mao.0b013e31804d4998. [DOI] [PubMed] [Google Scholar]
- 4.Schwartze H. Respiratorische Behebung des Trommelfelles. Arch Ohrenheilkd. 1864 [Google Scholar]
- 5.Aedo C MD, Der C. Trompa patulosa. Rev Otorrinolaringol Cir Cabeza Cuello. 2009;69:61–70. [Google Scholar]
- 6.Suehs O. The abnormally open eustachian tube. The Laryngoscope. 1960;70:1418–1426. [Google Scholar]
- 7.Dyer RK, Jr., McElveen JT., Jr. The patulous eustachian tube: management options. Otolaryngology--head and neck surgery. 1991;105:832–835. doi: 10.1177/019459989110500610. [DOI] [PubMed] [Google Scholar]
- 8.Ogawa S, Satoh I, Tanaka H. Patulous Eustachian tube. A new treatment with infusion of absorbable gelatin sponge solution. Arch Otolaryngol. 1976;102:276–280. doi: 10.1001/archotol.1976.00780100062006. [DOI] [PubMed] [Google Scholar]
- 9.O'Connor AF, Shea JJ. Autophony and the patulous eustachian tube. The Laryngoscope. 1981;91:1427–1435. doi: 10.1288/00005537-198109000-00003. [DOI] [PubMed] [Google Scholar]
- 10.Doherty JK, Slattery WH., 3rd Autologous fat grafting for the refractory patulous eustachian tube. Otolaryngology--head and neck surgery. 2003;128:88–91. doi: 10.1067/mhn.2003.34. [DOI] [PubMed] [Google Scholar]
- 11.Kong SK, Lee IW, Goh EK, Park SH. Autologous cartilage injection for the patulous eustachian tube. American journal of otolaryngology. 2011;32:346–348. doi: 10.1016/j.amjoto.2010.03.008. [DOI] [PubMed] [Google Scholar]
- 12.Rotenberg BW, Busato GM, Agrawal SK. Endoscopic ligation of the patulous eustachian tube as treatment for autophony. The Laryngoscope. 2013;123:239–243. doi: 10.1002/lary.23635. [DOI] [PubMed] [Google Scholar]
- 13.Takano A, Takahashi H, Hatachi K. Ligation of eustachian tube for intractable patulous eustachian tube: a preliminary report. Eur Arch Otorhinolaryngol. 2007;264:353–357. doi: 10.1007/s00405-006-0185-9. [DOI] [PubMed] [Google Scholar]
- 14.Halstead TH. Pathology and surgery of the eustachian tube. Arch Otolaryngol Head Neck Surg. 1926;4:189–195. [Google Scholar]
- 15.Virtanen H, Palva T. Surgical treatment of patulous eustachian tube. Arch Otolaryngol. 1982;108:735–739. doi: 10.1001/archotol.1982.00790590057016. [DOI] [PubMed] [Google Scholar]
- 16.Sato T, Kawase T, Yano H, Suetake M, Kobayashi T. Trans-tympanic silicone plug insertion for chronic patulous Eustachian tube. Acta oto-laryngologica. 2005;125:1158–1163. doi: 10.1080/00016480510038167. [DOI] [PubMed] [Google Scholar]
- 17.Bluestone CD, Cantekin EI. Management of the patulous Eustachian tube. The Laryngoscope. 1981;91:149–152. doi: 10.1288/00005537-198101000-00023. [DOI] [PubMed] [Google Scholar]
- 18.Ikeda R, Oshima T, Oshima H. Management of patulous eustachian tube with habitual sniffing. Otology & neurotology. 2011;32:790–793. doi: 10.1097/MAO.0b013e3182184e23. [DOI] [PubMed] [Google Scholar]
- 19.Chen DA, Luxford WM. Myringotomy and tube for relief of patulous eustachian tube symptoms. The American journal of otology. 1990;11:272–273. [PubMed] [Google Scholar]
- 20.Vaezeafshar R, Turner JH, Li G, Hwang PH. Endoscopic hydroxyapatite augmentation for patulous Eustachian tube. The Laryngoscope. 2014;124:62–66. doi: 10.1002/lary.24250. [DOI] [PubMed] [Google Scholar]
- 21.Robinson PJ, Hazell JW. Patulous eustachian tube syndrome: the relationship with sensorineural hearing loss. Treatment by eustachian tube diathermy. The Journal of laryngology and otology. 1989;103:739–742. doi: 10.1017/s0022215100109946. [DOI] [PubMed] [Google Scholar]


