Abstract
Objective
To document the demographic and clinical profile of persons who sustained spinal cord injury (SCI) as a result of accidental falls and to determine the usual circumstances surrounding the fall-induced SCI.
Design
Cohort study.
Setting
21 SCI Model Systems centers throughout the United States.
Participants
6,408 individuals with traumatic SCI between 2005 and 2014 were recruited from the National SCI Database. 1,877 (29%) of them were injuries caused by falls.
Interventions
Not applicable.
Outcomes Measures
External causes of injury documented by the International Classification of Diseases, 10th revision, Clinical Modification (ICD-10-CM).
Results
Falls on the same level from slipping, tripping, and stumbling were the most common cause of fall-induced SCI (20%), followed by falls from building (16%), stairs and steps (16%), and ladder (9%). People who were 61 years of age and older had the highest frequency of falls on the same level, while those aged 16–45 years had a higher percentage of falls from buildings, usually work-related. The mechanisms of falls also varied by sex and race. Associated injury and vertebral injury occurred frequently among falls from buildings and ladders. High falls were more likely to be work-related and result in thoracic and complete injury, while low falls were more commonly associated with cervical and motor functionally incomplete injury.
Conclusion
The study findings of different mechanisms of falls by age, sex, race and medical consequences provide an insight for future interventions aimed at high risk persons, activities, and environmental factors for preventing or reducing fall-induced SCI.
Keywords: Accidental falls, Epidemiology, Primary prevention, Spinal cord injuries
Introduction
Spinal cord injury (SCI) as a result of falls has consistently increased over the last 4 decades in the United States. Data from the National Spinal Cord Injury Database (NSCID) show that the percentage of SCI cases caused by falls has increased from 17% in the 1970s to 31% during 2010–2013.1 Fall-induced SCI is particularly common among the elderly, about 75% of SCI cases occurring among persons 76 years of age and older are due to falls.2 Older patients with SCI usually experience a longer hospital stay, increased cost of care, and higher risk of life threatening complications than their younger peers.3–6
Several studies conducted in the United States have reported the environmental events and circumstances surrounding SCI that results from falls. Unfortunately, each was limited by small case series (22 to 273 participants) and out-of-date information (data collection before 2006).7–9 Current knowledge regarding external causes and prevention of fall-induced SCI mainly relies on international reports and data from the general population, particularly the geriatric population.
The global maps for SCI project, launched by the International Spinal Cord Society, provides a structure for an on-going data repository to inform stakeholders of the development and coordination of prevention strategies.10 According to its recent report, falls from low heights or level ground are common in developed countries and are typically associated with tetraplegic injury among the elderly, while falls from greater heights are usually work-related, resulting in paraplegic injury, are predominantly among younger individuals in developing countries. Falls from unprotected rooftops and terraces, falls out of trees while cutting leaves to feed livestock, and falls while carrying a heavy load on one's head are also common regional features in developing countries.11 The World Health Organization's (WHO's) International Perspectives on SCI report recognizes 4 patterns of falls as resulting in SCI: (1) falls on the same level, (2) falls from heights of less than one meter, (3) falls from heights of one meter or more, and (4) being struck by a falling object.12 Effective and ineffective fall interventions are also summarized for each pattern of falls.
To address the needs for current statistics on fall-induced SCI in the United States, the present study analyzed data from the NSCID to: (1) document the demographic and injury profile of persons who sustained an SCI as a result of falls, as compared with SCI cases of non-fall etiologies; (2) determine the usual circumstances surrounding SCI that occurred as a result of accidental falls; and (3) examine whether mechanisms of falls differ by demographic and medical characteristics. We anticipate that descriptive statistics generated from this study will help develop appropriate programs aimed at high risk persons, activities, and environmental factors for preventing or reducing fall-induced SCI in the United States.
Methods
Data source
The NSCID contains information on persons with traumatic SCI who received initial hospital care from one of the 28 SCI Model Systems Centers since 1973. Data collection occurs during initial hospitalization and also currently at post-injury years 1, 5, 10 and every 5 years thereafter, including demographics, medical characteristics, physical functioning, and psychosocial outcomes. Details about the NSCID have been described elsewhere.13 Institutional Review Board approval was obtained at the National SCI Statistical Center as well as locally at each participating SCI Model Systems center before data collection.
Study participants
There were 6,416 persons with SCI reported to the NSCID between September 2005 and September 2014 when external causes of injury were documented. After excluding 8 individuals with unknown etiology of injury, a total of 6,408 persons from 21 SCI Model Systems Centers were eligible for the analysis. Twenty nine percent (n = 1,877) of them were injuries caused by falls. Table 1 summarizes the demographic, injury, and medical characteristics of these 1,877 study participants, as compared with 4,531 individuals with SCI of non-fall etiologies (vehicular accidents, 55%; acts of violence, 21%; sports, 12%; medical/surgical complications, 7%; and others, 5%).
Table 1 .
Characteristics of 1,877 study participants as compared with those of non-fall etiologies (n = 4,531)
| Fall group |
Non-fall group |
||||
|---|---|---|---|---|---|
| Characteristics* | n | (%) | n | (%) | P value |
| Age (years) | |||||
| 0–15 | 8 | (0.4) | 69 | (1.5) | <0.001 |
| 16–30 | 239 | (12.7) | 2,052 | (45.3) | |
| 31–45 | 329 | (17.5) | 1,015 | (22.4) | |
| 46–60 | 664 | (35.4) | 945 | (20.9) | |
| 61 and above | 637 | (33.9) | 450 | (9.9) | |
| Age (years), mean ± standard deviation | 52.9 | ± 17.0 | 36.6 | ± 16.6 | <0.001 |
| Sex | |||||
| Male | 1,490 | (79.4) | 3,607 | (79.7) | 0.80 |
| Female | 387 | (20.6) | 921 | (20.3) | |
| Race/ethnicity | |||||
| White | 1,272 | (69.7) | 2,657 | (59.6) | <0.001 |
| Black | 335 | (18.4) | 1,207 | (27.1) | |
| Hispanic | 149 | (8.2) | 455 | (10.2) | |
| Other | 68 | (3.7) | 139 | (3.1) | |
| Day of injury | |||||
| Monday | 295 | (15.7) | 573 | (12.7) | <0.001 |
| Tuesday | 226 | (12.0) | 514 | (11.3) | |
| Wednesday | 232 | (12.4) | 536 | (11.8) | |
| Thursday | 268 | (14.3) | 528 | (11.7) | |
| Friday | 258 | (13.8) | 635 | (14.0) | |
| Saturday | 314 | (16.7) | 881 | (19.4) | |
| Sunday | 284 | (15.1) | 864 | (19.1) | |
| Month of injury | |||||
| January | 131 | (7.0) | 332 | (7.3) | 0.07 |
| February | 133 | (7.1) | 274 | (6.1) | |
| March | 141 | (7.5) | 390 | (8.6) | |
| April | 150 | (8.0) | 401 | (8.6) | |
| May | 157 | (8.4) | 430 | (9.5) | |
| June | 160 | (8.5) | 385 | (8.5) | |
| July | 177 | (9.4) | 495 | (10.9) | |
| August | 166 | (8.8) | 399 | (8.8) | |
| September | 158 | (8.4) | 384 | (8.5) | |
| October | 171 | (9.1) | 353 | (7.8) | |
| November | 172 | (9.2) | 343 | (7.6) | |
| December | 161 | (8.6) | 345 | (7.6) | |
| Work-related | |||||
| Yes | 299 | (16.1) | 268 | (6.0) | <0.001 |
| No | 1,559 | (83.9) | 4,223 | (94.0) | |
| Associated injury | |||||
| Yes | 416 | (24.4) | 1,863 | (46.1) | <0.001 |
| No | 1287 | (75.6) | 2,182 | (53.9) | |
| Vertebral injury | |||||
| Yes | 1,208 | (70.9) | 3,339 | (82.5) | <0.001 |
| No | 497 | (29.1) | 710 | (17.5) | |
| Level of injury | |||||
| Cervical | 1,112 | (66.3) | 2,194 | (53.6) | <0.001 |
| Thoracic | 402 | (24.0) | 1,483 | (36.2) | |
| Lumbar | 146 | (8.7) | 396 | (9.7) | |
| Sacral | 5 | (0.3) | 11 | (0.3) | |
| Normal | 12 | (0.7) | 11 | (0.3) | |
| AIS grade | |||||
| A | 426 | (24.8) | 1,732 | (41.2) | <0.001 |
| B | 162 | (9.4) | 612 | (14.6) | |
| C | 305 | (17.7) | 608 | (14.5) | |
| D | 814 | (47.4) | 1,244 | (29.6) | |
| E | 12 | (0.7) | 11 | (0.3) | |
AIS = American Spinal Injury Association Impairment Scale
*Records with unknown or missing values were excluded from the analysis
Classification of falls
In addition to the 37 descriptive causes of injury,2 the NSCID utilizes the International Classification of Diseases, 10th revision, Clinical Modification (ICD-10-CM), Chapter 20 External Cause of Injury to further capture how the SCI occurred, the intent (accidental or intentional), place, and activity. The ICD-10-CM is the clinical modification of the WHO's ICD-10, published by the United States government for medical coding and reporting of basic health statistics.14 The ICD-10-CM is composed of codes up to 7 digits. Codes with 3 digits are included as the heading of a category of codes that may be further subdivided by the use of 4th, 5th, 6th or 7th digits, which provide greater specificity. This study utilized the codes W00 – W19 to classify accidental falls (Table 2).
Table 2 .
External causes of fall-induced spinal cord injury documented by three-character ICD-10-CM codes (n = 1,783)
| ICD-10-CM | Description | n | (%) |
|---|---|---|---|
| W00 | Fall due to ice and snow | 38 | (2.1) |
| W01 | Fall on same level from slipping, tripping, and stumbling | 360 | (20.2) |
| W03 | Other fall on same level due to collision with another person | 3 | (0.2) |
| W04 | Fall while being carried or supported by other persons | 1 | (0.1) |
| W05 | Fall from non-moving wheelchair | 2 | (0.1) |
| W06 | Fall from bed | 49 | (2.7) |
| W07 | Fall from chair | 25 | (1.4) |
| W08 | Fall from other furniture | 20 | (1.1) |
| W09 | Fall on and from playground equipment | 5 | (0.3) |
| W10 | Fall on and from stairs and steps | 284 | (15.9) |
| W11 | Fall on and from ladder | 159 | (8.9) |
| W12 | Fall on and from scaffolding | 43 | (2.4) |
| W13 | Fall from, out of or through building or structure | 285 | (16.0) |
| W14 | Fall from tree | 87 | (4.9) |
| W15 | Fall from cliff | 11 | (0.6) |
| W16 | Fall, jump or diving into water | 36 | (2.0) |
| W17 | Other fall from one level to another | 99 | (5.6) |
| W18 | Other slipping, tripping and stumbling and falls | 131 | (7.3) |
| W19 | Unspecified fall | 145 | (8.1) |
ICD-10 coding structure has been applied in injury research since 1994.15–18 In a study that examined the usefulness of ICD-10-CM system in documenting public health diseases, Watzlaf et al. concluded that compared to ICD-9-CM, the ICD-10-CM captures external causes of injury more straightforwardly and clearly.19
Variables and measures
Demographic, injury, and medical characteristics for this study were obtained by trained personnel from hospital admission records and by personal interview. Neurological examinations were performed within 7 days of discharge in accordance with the version of the International Standards for Neurological Classification of SCI that was in use at the time the examinations were performed.20
Based on the International SCI Data Standards,21 vertebral injury was defined as any break, rupture, or crack in any bone that is part of the vertebral column from the occiput to the coccyx. Associated injury referred to the presence of any of the following injuries occurring at the time of SCI: traumatic brain injury (Glasgow Coma Scale ≤ 12), non-vertebral fractures, severe facial injuries affecting sense organs, major chest injury, traumatic amputations of an arm or leg, severe hemorrhaging, and damage to any internal organ requiring surgery.
A work-related case was defined as any injury occurred in the course of employment, according to the ‘Operational Guidelines for Determination of Injury at Work’ developed in 1992 jointly by several United States government agencies.22 Additional NSCID data collection procedures as well as forms and instructions are located on the National SCI Statistical Center web site at https://www.nscisc.uab.edu/.
Data analysis
Descriptive statistics (mean, standard deviation, frequency, and percentage) were used to describe demographic and medical characteristics of study participants across injury etiologies as well as different mechanisms of falls. Student's t-test and χ2 test, as appropriate, were used to assess the differences between the fall and non-fall etiology groups at a statistical significance level of 0.05.
Results
Participant characteristics: fall vs non-fall etiologies
Statistically significant differences were found between the fall and non-fall groups with regard to demographic and injury profile (Table 1). Persons with fall-induced SCI tended to be older, of white race, less likely to have associated injury (24% vs 46%) and vertebral injury (71% vs 83%), but more likely to have cervical injury (66% vs 54%) and American Spinal Injury Association Impairment Scale (AIS) D injury (43% vs 28%). Work-relatedness was also more common in the fall group than in the non-fall group (16% vs 6%).
Mechanisms of falls
After excluding 94 individuals with missing or incomplete ICD-10-CM codes, 1,783 participants with accidental fall injuries were classified into 19 mechanisms of falls (Table 2). Among them, fall on the same level from slipping, tripping, and stumbling (W01) was most common (20%), followed by fall from building (W13, 16%), stairs and steps (W10, 16%), and ladder (W11, 9%). Other slipping, tripping, and stumbling and falls (W18, 7%) was also a common cause, including fall from or off toilet, fall in (into) shower or empty bathtub, and fall on same level due to stepping on an object.
Circumstances surrounding the falls further specified by the 4th, 5th or 6th digits of the ICD-10-CM codes were shown in Table 3. Approximately 54% of the falls on same level from slipping, tripping, and stumbling involved subsequently striking against an object. Fall from the roof and balcony accounted for about 59% of the falls from, out of or through buildings.
Table 3 .
Further specification of the most common mechanisms of falls
| Mechanisms of fall | n | (%) |
|---|---|---|
| Fall on same level from slipping, tripping, and stumbling (n = 360) | ||
| Without subsequent striking against object (W01.0) | 111 | (30.8) |
| With subsequent striking against object | ||
| - Against sharp object (W01.11) | 2 | (0.6) |
| - Sharp glass (W01.110) | 1 | (0.3) |
| - Power tool or machine (W01.111) | 1 | (0.3) |
| - Against other object (W01.19, W01.198) | 98 | (27.2) |
| - Furniture (W01.190) | 25 | (6.9) |
| - No detail or unspecific about the object (W01.1, W01.10) | 67 | (18.6) |
| No detail about subsequent striking against object (W01) | 55 | (15.3) |
| Fall from, out of, or through building or structure (n = 285) | ||
| Balcony (W13.0) | 71 | (24.9) |
| Bridge (W13.1) | 7 | (2.5) |
| Roof (W13.2) | 98 | (34.4) |
| Floor (W13.3) | 9 | (3.2) |
| Window (W13.4) | 19 | (6.7) |
| Other: viaduct, wall, or flag-pole (W13.8) | 47 | (16.5) |
| Building, not otherwise specified (W13.9) | 18 | (6.3) |
| No further information (W13) | 16 | (5.6) |
| Fall on and from stairs and steps (n = 284) | ||
| Escalator (W10.0) | 3 | (1.1) |
| Sidewalk curb (W10.1) | 4 | (1.4) |
| Incline (W10.3) | 3 | (1.1) |
| Other stairs and steps (W10.8) | 148 | (52.1) |
| No detail or unspecified (W10, W10.9) | 126 | (44.4) |
Demographic and injury differences
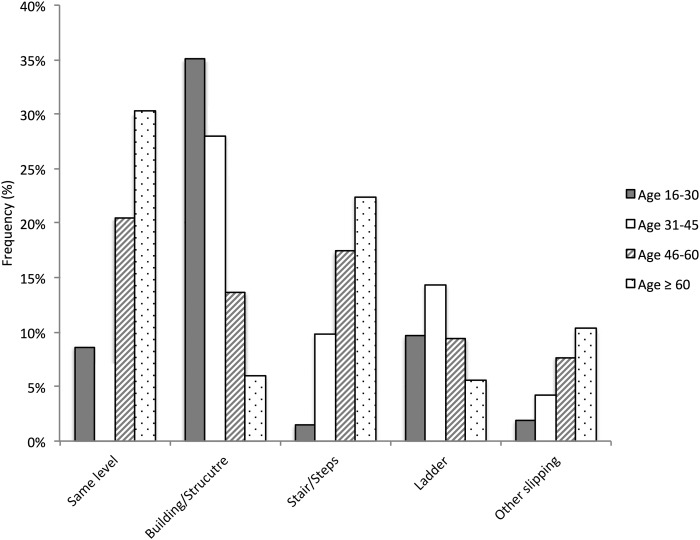
People who were 61 years of age and older had the highest frequency of falls on the same level (30%), from stairs (22%), and other slipping, tripping and stumbling (10%) (Fig. 1). In fact, 40% of the 186 fall-induced SCI cases among persons aged 75 and above occurred on same level from slipping, tripping and stumbling. Among the age 16–30 and 31–45 groups, falls from buildings were the most common mechanism (35% and 28%, respectively), and a substantial number of these falls from buildings were work-related (29% and 43%, respectively). A similar pattern was observed for falls from ladders, work-relatedness accounting for 55% of falls from ladders among persons aged 16–30 and 66% among those aged 31–45.
Figure 1 .
Selected mechanisms of falls by age groups
Among females, more falls occurred on same level from slipping, tripping and stumbling (27% vs 19%) and on/from stairs and steps (27% vs 13%) than their male counterparts, while falls from buildings, ladders, and trees were more common among males than females (34% vs 14%).
Individuals of Hispanic origin had the highest proportion of falls from buildings (26%), ladders (14%) and scaffolding (7%) compared to other racial and ethnic groups (17%, 10%, and 2%, respectively for whites and 10%, 5%, and 1%, respectively for blacks). Most of these falls occurring among persons of Hispanic origin were work-related, including 66% of falls from buildings (n = 23 out of 35) and 74% of falls from ladders (n = 14 out of 19).
Associated injury and vertebral injury occurred frequently among falls from buildings and ladders than other mechanisms of falls (Table 4). High falls, such as falls from buildings and ladders, were more likely to be work-related and result in thoracic and complete injury, while low falls, such as falls on the same level or stairs, were more commonly associated with cervical and AIS D injury.
Table 4 .
Demographic and injury profile of selective mechanisms of falls
| Mechanism of falls |
|||||
|---|---|---|---|---|---|
| Characteristics | Same level (W01) | Building/ Structure (W13) | Stairs/ Steps (W10) | Ladder(W11) | Other slipping (W18) |
| Sample size* | 360 | 285 | 284 | 159 | 131 |
| Age (years), mean | 61.3 | 42.7 | 60.4 | 48.9 | 60.9 |
| Sex, % | |||||
| Male | 73.1 | 87.0 | 66.2 | 94.3 | 77.9 |
| Female | 26.9 | 13.0 | 33.8 | 5.7 | 22.1 |
| Race/ethnicity, % | |||||
| White | 68.5 | 73.7 | 64.6 | 78.1 | 65.6 |
| Black | 25.8 | 11.7 | 24.8 | 9.7 | 22.4 |
| Hispanic | 3.7 | 12.5 | 5.5 | 12.3 | 8.0 |
| Other | 2.0 | 2.2 | 5.1 | 0.0 | 4.0 |
| Work-related: | |||||
| Yes, % | 6.1 | 27.6 | 5.0 | 36.1 | 15.6 |
| Associated injury: Yes, % | 12.0 | 44.5 | 22.3 | 32.1 | 14.3 |
| Vertebral injury: Yes, % | 47.4 | 91.8 | 62.8 | 94.2 | 54.0 |
| AIS grade, % | |||||
| A | 8.4 | 37.7 | 13.1 | 47.0 | 12.6 |
| B | 7.9 | 10.8 | 7.7 | 12.1 | 9.0 |
| C | 22.1 | 19.0 | 17.8 | 13.4 | 12.6 |
| D | 60.7 | 32.1 | 59.9 | 26.9 | 64.0 |
| E | 0.9 | 0.4 | 1.5 | 0.7 | 1.8 |
| Level of injury, % | |||||
| Cervical | 87.8 | 39.2 | 88.2 | 34.3 | 86.0 |
| Thoracic | 7.0 | 46.9 | 6.3 | 45.5 | 8.4 |
| Lumbar | 3.7 | 13.2 | 3.5 | 19.6 | 2.8 |
| Sacral | 0.6 | 0.4 | 0.4 | 0.0 | 0.9 |
| Normal | 0.9 | 0.4 | 1.6 | 0.7 | 1.9 |
AIS = American Spinal Injury Association Impairment Scale
*Records with unknown or missing values were excluded from analysis.
Discussion
Fall vs non-fall etiologies
Our findings on the demographic and injury profile of persons with fall-induced SCI are generally consistent with previous reports, including no sex difference between the fall and non-fall groups.23 A slightly higher percentage of whites were observed in our fall group compared with the non-fall group. However, because these are proportions rather than incidence rates, one cannot draw a conclusion that whites fall more often than non-whites. Moreover, this slightly higher percentage might be partly explained by age rather by race alone (whites in our study population are on average older than non-whites).
More falls occurred on Saturday and Monday, July and November than other days of the week and months of the year. These results are consistent with the overall incidence of SCI.2 Other studies have not found an association between likelihood of SCI due to falls and either day of the week or month of the year.7,24 We did not find any trend with respect to day of week when any specific type of falls occurred.
Mechanisms of falls
There seems to be a lack of international standards to classify falls. Height, nevertheless, has been widely used as a common criterion. The WHO's International Perspectives of SCI report categorizes falls by height using one meter as a cut-off point.12 A previous report suggested defining mechanism of falls by the height from which the person fell, the angle of the fall, the energy absorption of the surface, and the deceleration at the time of impact.6 In DeVivo's study, fall was documented as slipping or tripping on level ground, falling down stairs, and falling off a roof, tree, balcony or ladder. Height was also considered: level ground, 1–5 feet, 6–10 feet, 11–20 feet, 21–50 feet and >50 feet.7
Although the exact height from which the person fell was not documented in this study, the ICD-10-CM coding system provides sufficient information for differentiating high falls from low falls. For example, falls on same level and most falls from stairs are equivalent to falls from heights of less than one meter, while falls from buildings are typically from heights of one meter or more. Besides the height, ICD-10-CM captures further details surrounding the falls, such as the places where falls occur (bridge, roof, winder, escalator, etc.).
Our observation suggests that most fall-induced SCIs occurred at home in women and among the elderly. Falls on same level and from stairs and steps are problematic for both men and women, which are consistent with Buczak-Stec et al's study that used the ICD-10 coding structure to document fall related hospital admissions in the elderly population in Poland.15 In the context of SCI, our study confirms international reports regarding the association of high vs low falls with age, level of injury, and work relatedness.10,12,25 The present study further expands previous studies to document the sex and racial differences in the mechanisms of falls as well as the impact on associated injury and neurologic outcomes.
Fall prevention
In the United States, about 1 in 3 people age 65 and older fall each year. Among elderly people, falls are not only the leading cause of injury death (25,249 reported cases in 2010) but also the most common cause of nonfatal injuries (4,602,665 reported cases) and hospital admissions for trauma.26,27 The medical costs of falls was estimated to be approximately $30.0 billion in 2010.27 Despite the lack of common criteria to define mechanisms of falls, researchers all agree that it is possible and also essential to identify risk factors for sustaining a fall or fall-related injury, so that effective fall-prevention programs can be developed for high-risk population and activities.
There are many established programs aimed at reducing falls. In their review, Rubenstein et al. provided the latest evidence on the efficacy of existing fall interventions and also classified the programs into 5 groups: multidimensional fall risk assessment to reduce risk, exercise intervention, environmental assessment and modification, multifactorial intervention, and institutional interventions.28 In 2010, the Center for Disease Control and Prevention developed a compendium of 22 fall prevention programs with interventions being focused on three main areas: exercise, home modification and multifaceted.26 There are also many randomized controlled trials aiming at reducing falls or fall-risk factors in older people.29,30
Our study results support those fall prevention approaches and recommendations. For example, home safety is crucial in order to reduce falls and ultimately SCIs, especially for women and the elderly. In addition to the home safety checklist,24 we need to improve older people's living environments by removing clutter, loose carpets and uneven floor surface; providing good lighting, hand rails, appropriate toilets and beds; etc.12 For younger adults, especially for the Hispanic population, work place safety is crucial, including proper equipment use and training, safety inspections and testing, as well as environmental modifications.
Limitations
There are several limitations in this study. Study participants were recruited from SCI Model System hospitals and are not population-based. Therefore, our study results might not be applicable to all persons with fall-induced SCI in the United States or other countries. For example, individuals with SCI enrolled in the NSCID tend to be more severely injured. Therefore our study sample might under-represent mild SCI cases among the older adults and falls on the same level.
Due to ICD-10-CM coding structure constraints, this study is not able to capture every detail surrounding SCI that results from falls. For example, there is no documentation about use of alcohol and drugs and a sequence of events (underlying vs direct mechanism) leading to the SCI. The WHO's International Classification of External Cause of injury has a multi-axial and hierarchical structure, including 7 core modules: mechanism of injury, objects/substances producing injury, place of occurrence, activity when injured, the role of human intent, use of alcohol, and use of (other) drugs. There are also 5 etiology modules: violence, transport, place, sports, and occupational injury so that additional data on special topics can be collected.31 The International Classification of External Cause of injury could be an alternative or supplement for better documenting the multi-dimensional and hierarchical nature of the injury as well as for international comparability across studies, as suggested by previous study.18
Conclusion
This is the first and largest study to date that reports environmental events and circumstances as external causes of fall-induced SCI, using the ICD-10-CM coding structure. This study demonstrates that the mechanisms of falls are different by age, sex and race and also lead to various medical consequences. Future interventions should be developed for high-risk persons, activities and environments. In light of the aging population in the United States, there is an urgent need for effective fall prevention programs among the elderly to reduce SCI.
Disclaimer statements
Contributors All authors have made significant contribution to this project (design, conception, data analysis, or/and interpretation) as well as manuscript preparation and writing.
Funding This work was supported in part by grant #H133A110002 from the National Institute on Disability and Rehabilitation Research, Office of Special Education and Rehabilitation Services, United States Department of Education, Washington DC.
Conflicts of interest No conflict of interest.
Ethics approval Institutional Review Board approval was obtained at the National SCI Statistical Center as well as locally at each participating SCI Model Systems center before data collection.
Reference
- 1.Natio nal Spinal Cord Injury Statistical Center. 2013 Annual Statistical Report for the Spinal Cord Injury Model Systems. [Cited 2014 November 10.] Available from https://www.nscisc.uab.edu/reports.aspx .
- 2.Chen Y, Tang Y, Lawrence CV, DeVivo MJ. Causes of spinal cord injury. Top Spinal Cord Inj Rehabil 2013;19(1):1–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Lovasik D. The older patient with a spinal cord injury. Crit Care Nurs Q 1999;22(2):20–30. [DOI] [PubMed] [Google Scholar]
- 4.Spivak J, Weis M, Cotler J, Call M. Cervical spine injuries in patients 65 and older. Spine 1994;19(20):2302–6. [DOI] [PubMed] [Google Scholar]
- 5.Golob J, Claridge J, Yowler C, Como J, Peerless J. Isolated cervical spine fractures in the elderly: a deadly injury. J Trauma 2008;64(2):311–5. [DOI] [PubMed] [Google Scholar]
- 6.Grimm D, Mion LC. Falls resulting in traumatic injury among older adults: nursing care issues. AACN Advanced Critical Care 2011;22(2):161–8. [DOI] [PubMed] [Google Scholar]
- 7.DeVivo M. Prevention of spinal cord injuries resulting from falls [abstract]. J Spinal Cord Med 2000;23Suppl):15–6.10752869 [Google Scholar]
- 8.Weingarden S, Graham P. Falls resulting in spinal cord injury: patterns and outcomes in an older population. Paraplegia 1989;27(6):423–7. [DOI] [PubMed] [Google Scholar]
- 9.Fayssoux R, Tally W, Sanfilippo J, Stock G, Ratliff J, Anderson G, et al. Spinal injuries after falls from hunting tree stands. Spine J 2008;8(3):522–8. [DOI] [PubMed] [Google Scholar]
- 10.Lee BB, Cripps RA, Fitzharris M, Wing PC. The global map for traumatic spinal cord injury epidemiology: update 2011, global incidence rate. Spinal Cord 2014;52(2):110–6. [DOI] [PubMed] [Google Scholar]
- 11.Hoque M, Hasan Z, Razzak A, Helal S. Cervical spinal cord injury due to fall while carrying heavy load on head: a problem in Bangladesh. Spinal Cord 2012;50(4):275–7. [DOI] [PubMed] [Google Scholar]
- 12.Bickenbach J, Officer A., Shakespeare T, von Groote P. International Perspectives on Spinal Cord Injury. World Health Organization; 2013. Available from http://www.who.int/disabilities/policies/spinal_cord_injury/report/en/
- 13.Stover S, DeVivo M, Go B. History, implementation, and current status of the National Spinal Cord Injury Database. Arch Phys Med Rehabil 1999;80(11):1365–71. [DOI] [PubMed] [Google Scholar]
- 14.International Classification of Diseases, Tenth Revision, Clinical Modification (ICD-10-CM). [Cited 2014 November 10.] Available from: http://www.cdc.gov/nchs/icd/icd10cm.htm#icd2015
- 15.Buczak-Stec E, Goryński P. Fall related hospital admissions among seniors in Poland in 2010. Przegl Epidemiol 2013;67(1):57–62. [PubMed] [Google Scholar]
- 16.Davas AA, Durusoy R, Ada S, Kayalar M, Aksu F, Bal E. Epidemiology of injuries treated at a hand and microsurgery hospital. Acta Orthop Traumatol Turc 2010;44(5):352–60. [DOI] [PubMed] [Google Scholar]
- 17.Davas AA, Durusoy R, Bal E, Kayalar M, Ada S, Tanik F. Risk factors for occupational hand injuries: relationship between agency and finger. Am J Ind Med 2012;55(5):465–73. [DOI] [PubMed] [Google Scholar]
- 18.Kozlowski K, Leddy J, Tomita M, Bergen A, Willer B. Use of the ICECI and ICD-10 E-Coding structures to evaluate causes of head injury and concussion from sport and recreation participation in a school population. NeuroRehab 2007;22(3):191–8. [PubMed] [Google Scholar]
- 19.Watzlaf VJM, Garvin JHG, Moeini S, Anania-Firouzan P. The effectiveness of ICD-10-CM in capturing public health diseases. Perspect Health Inf Manag 2007;4:6. [PMC free article] [PubMed] [Google Scholar]
- 20.Kirshblum SC, Burns SP, Biering-Sorensen F, Donovan W, Graves DE, Jha A, et al. International standards for neurological classification of spinal cord injury (revised 2011). J Spinal Cord Med 2011;34(6):535–46. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.DeVivo MJ, Biering-Sorensen F, Charlifue S, Noonan V, Post M, Stripling T, et al. International spinal cord injury core data set. Spinal Cord 2006;44(9):535–40. [DOI] [PubMed] [Google Scholar]
- 22.Operational Guidelines for Determination of Injury at Work. [Cited 2014 November 10.] Available from: http://www.cdc.gov/niosh/docs/2001-129/pdfs/01-129Sapp.pdf .
- 23.Kennedy P, Cox A, Mariani A. Spinal Cord injuries as a consequence of falls: are there differential rehabilitation outcomes? Spinal Cord 2013;51(3):209–13. [DOI] [PubMed] [Google Scholar]
- 24.Akyol AD. Falls in the elderly: what can be done? Int Nurs Rev 2007;54(2):191–6. [DOI] [PubMed] [Google Scholar]
- 25.Correa G, Finkelstein J, Burnier L, Danilla S, Tapia L, Torres V, et al. Work-related traumatic spinal cord lesions in Chile, a 20-year epidemiological analysis. Spinal Cord 2011;49(2):196–9. [DOI] [PubMed] [Google Scholar]
- 26.Tomashek D, Dolski T. Vision and eyeglass use in falls prevention programs: a review of the CDC compendium. Arch Phys Med Rehabil 2012;93(10):e53. [Google Scholar]
- 27.Falls Among Older Adults: An Overview. [Cited 2014 November 10.] Available from: http://www.cdc.gov/HomeandRecreationalSafety/Falls/adultfalls.html
- 28.Rubenstein LZ, Josephson KR. Falls and their prevention in Elderly people: What does the evidence show? Med Clin N Am 2006;90(5):807–24. [DOI] [PubMed] [Google Scholar]
- 29.Vogler CM, Menant JC, Sherrington C, Ogle SJ, Lord SR. Evidence of detraining after 12-week home-based exercise programs designed to reduce fall-risk factors in older people recently discharged from hospital. Arch Phys Med Rehabil 2012;93(10):1685–91. [DOI] [PubMed] [Google Scholar]
- 30.Perula LA, Varas-Fabra F, Rodriguez V, Ruiz-Moral R, Fernandez JA, Dios Cd. Effectiveness of a multifactorial intervention program to reduce falls incidence among community-living older adults: a randomized controlled trial. Arch Phys Med Rehabil 2012;93(10):1677–84. [DOI] [PubMed] [Google Scholar]
- 31.Lee B, Cripps R, Woodman R, Biering-Sørensen F, Wing P, Campbell R, et al. Development of an international spinal injury prevention module: application of the International classification of external cause of injury to spinal cord injury. Spinal Cord 2010;48(6):498–503. [DOI] [PubMed] [Google Scholar]