Abstract
Objective
To identify factors associated with health-care utilization during the first year after inpatient rehabilitation (IR) in individuals with traumatic spinal cord injury (SCI).
Design
Prospective cohort.
Methods
One hundred and sixty-eight patients were prospectively enrolled and followed over 1 year after discharge from an SCI Model System IR program. Telephone follow-up occurred at 3, 6, 9, and 12 months. Participants were grouped into four impairment levels (C1–4 American Spinal Injury Association (ASIA) Impairment Scale (AIS) A–C, C5–C8 AIS A–C, paraplegia AIS A–C, and all AIS D). Three domains of health-care utilization were examined: hospital care, outpatient provider visits, and home services.
Results
Health-care utilization in the first year following IR was high with 45% of subjects reporting re-hospitalization. Twenty percent of patients were initially discharged to a skilled nursing facility (SNF), and an additional 10% required SNF care during this first year. Overall, those with C1–4 AIS A–C used the most services. Participants discharged home used less health care compared to those discharged elsewhere. SCI due to falls (vs. vehicular crashes) was associated with fewer in-home service visits. Age, sex, race, and education were unrelated to higher use.
Conclusion
Those with greater neurological impairment or not discharged home after IR had higher health-care utilization, while age was not associated with utilization. Targeted efforts to reduce genitourinary and respiratory complications may reduce the need for hospital care in the first year after IR.
Keywords: Health-care utilization, Spinal cord injury, Re-hospitalization
Introduction
The individual and societal lifetime economic impact of traumatic spinal cord injury (SCI) is high, despite an incidence of only 25–59 per 1 million persons annually in the USA.1 Physiologic changes resulting from SCI predispose those affected to the development of secondary conditions requiring health-care services, with 95% of patients endorsing at least one associated medical condition.2 Over recent decades, the lengths of stay for acute care and inpatient rehabilitation (IR) phases of initial SCI treatment have greatly decreased. There continues to be an increase in mean age at injury, with growth in the proportion of patients who are elderly at the time of injury and thus have more pre-existing medical comorbidities. These trends make it likely that the need for health-care utilization in the initial period post-discharge is also changing. The aims of this current study were to (1) identify the most common health-care services used in the first year post-discharge from IR for individuals with traumatic SCI, (2) examine characteristics associated with service utilization; and (3) determine rates and reasons for re-hospitalization in this population.
Methods
Participants
This study analyzes data from 168 adults who participated in a randomized controlled trial of a telephone follow-up intervention during the first post-discharge year after traumatic SCI. All patients who were treated for new SCI during 2009–2013 by the Northwest Regional SCI System of Care and meeting criteria for enrollment in the Model Systems National SCI Database were offered enrollment. Briefly, to be included an individual had to have a traumatic SCI, admitted to the center within 1 year of injury, complete IR at the specific SCI Model System center and reside in the center's catchment area following discharge from IR. The primary outcomes of the intervention study included health-care utilization and psychosocial adjustment. During the enrollment period, 80% of eligible patients admitted to the study site agreed to participate. No differences in demographics and outcomes were found between treatment (enhanced telephone follow-up) and control (usual follow-up) condition; therefore, data from both groups were combined for this study. During this time period, no significant changes in health-care delivery occurred within the system.
Participants were enrolled during IR and each participant was followed prospectively with structured phone interviews at 3, 6, 9, and 12 months after discharge from IR. Information about hospital admissions, emergency room (ER) visits, surgeries, imaging studies, primary care and specialist outpatient visits, and home health services (nursing, therapy, and paid attendant care) were obtained for the prior 3 months by an examiner blinded to treatment condition. All study procedures were approved by the UW Human Subjects Review Committee and informed consent was obtained from each participant.
Measures
Demographic and injury characteristics were collected during IR and are summarized in Table 1. Race was grouped as Caucasian vs. other, etiology was grouped as vehicular vs. other, marital status was grouped as married at time of injury vs. other, and education was grouped as high school or general education development (GED) and above vs. less than high school. Neurological classification was determined for the status at the time of IR discharge. The patients were placed into four groups of neurological level of impairment: (1) C1–C4 American Spinal Injury Association (ASIA) Impairment Scale (AIS) A–C, (2) C5–C8 AIS A–C, (3) paraplegia AIS A–C, and (4) all AIS D SCI.
Table 1 .
Demographic characteristics by neurological level
| Total | AIS A–C (C1–C4) | AIS A–C (C5–C8) | AIS A–C (paraplegia) | AIS D (any level) | P | |
|---|---|---|---|---|---|---|
| N (% total) | 168 | 36 (22%) | 23 (14%) | 47 (28%) | 61 (37%) | |
| Age, mean (SD) | 41 (16) | 40 (16) | 37 (15)A | 36 (14)B | 48 (15)AB | 0.004 |
| Sex N (% male) | 133 (79%) | 27 (75%) | 20 (87%) | 34 (72%) | 51 (84%) | 0.458 |
| Acute care LOS* mean (SD) | 17 (15) | 16 (12) | 22 (16) | 20 (19) | 14 (13) | 0.079 |
| Rehab LOS mean (SD) | 47 (41) | 65 (29)ABC | 51 (19)AE | 45 (33)BF | 35 (54)CEF | <0.001 |
| Race N (% Caucasian) | 138 (83%) | 29 (81%) | 20 (87%) | 39 (83%) | 50 (83%) | 0.385 |
| Etiology N (% vehicular) | 65 (39%) | 16 (44%) | 7 (30%) | 18 (38%) | 24 (39%) | 0.875 |
| Discharge FIM** mean (SD) | 53 (24) | 23 (9)ABC | 41 (15)ADE | 60 (19)BDF | 70 (17)CEF | <0.001 |
| Discharge to SNF*** N (%) | 30 (18%) | 9 (25%) | 6 (26%) | 8 (17%) | 6 (10%) | 0.054 |
| Discharge home N (%) | 134 (80%) | 25 (69%) | 17 (74%) | 38 (81%) | 54 (89%) | |
| Discharge other N (%) | 4 (2%) | 2 (6%) | 0 (0%) | 1 (2%) | 1 (2%) | |
| Married at time of injury N (%) | 59 (35%) | 12 (33%) | 8 (35%) | 15 (32%) | 24 (39%) | 0.522 |
| Education N (% HS/GED or above) | 146 (88%) | 34 (94%) | 21 (95%) | 38 (81%) | 52 (87%) | 0.198 |
Letters, pairwise comparison is significant at the Bonferroni-corrected α = 0.05 (i.e. 0.0083).
*LOS, length of stay.
**FIM, functional independence measure.
***SNF, skilled nursing facility.
Health-care utilization domains
A modified version of the Cornell Services Index was used to collect data on health-care utilization. The original 22-item instrument measures use of mental health services, but includes information about more general health-care use in an adult population.3 Some items related to mental health care (e.g. types of psychotherapy) were deleted, and some additional questions were added specific to SCI care such as whether the participant required surgery, stayed overnight in a skilled nursing facility (SNF), or was seen by a rehabilitation medicine physician. For the current study, data were grouped into three main health-care utilization domains: hospital-based care, outpatient services, and home services. The hospital care domain included any hospitalizations, ER or urgent care visits, or any surgeries (including day procedures). The outpatient services domain included visits to a primary care provider (PCP), rehabilitation medicine or other specialist physician or mid-level provider (physician assistant or nurse practitioner), nursing clinic visit, mental health professional (psychiatrist and psychologist), as well as others. The home services domain included home health (nursing and therapy) visits as well as paid attendant care use.
Statistical analysis
Descriptive statistics were used to compare demographic and injury characteristics across neurological level of impairment. Poisson regression models were run for each of the three health-care utilization domains with neurologic classification, age, sex, race, etiology of injury, discharge location (home or not home), marital status, and education as predictor variables in the model using SPSS version 17 (SPSS Inc., Chicago, IL, USA). The advantage of using this model is to account for multiple incidents, or count of incidents, within each domain (e.g. allow for more than one hospitalization per person), rather than limit to a binary response (i.e. hospitalized or not, used home services or not, etc.). Outcome was modeled as 12-month counts, which were calculated as the sum of the ‘over the previous 3 months' estimates provided at each of the four outcome assessments. Counts for missed assessments were estimated with a pre-rated average based on the known assessments (rounded to the nearest integer to accommodate the Poisson model). As long as a subject provided at least one outcome assessment, they were included in the analysis. We performed unweighted analyses despite the fact that some subjects contributed more information than others.
Results
Table 1 shows demographic characteristics of participants. Individuals with AIS D injuries tended to be older, have the shortest rehabilitation length of stay and the highest discharge functional independence measure scores.
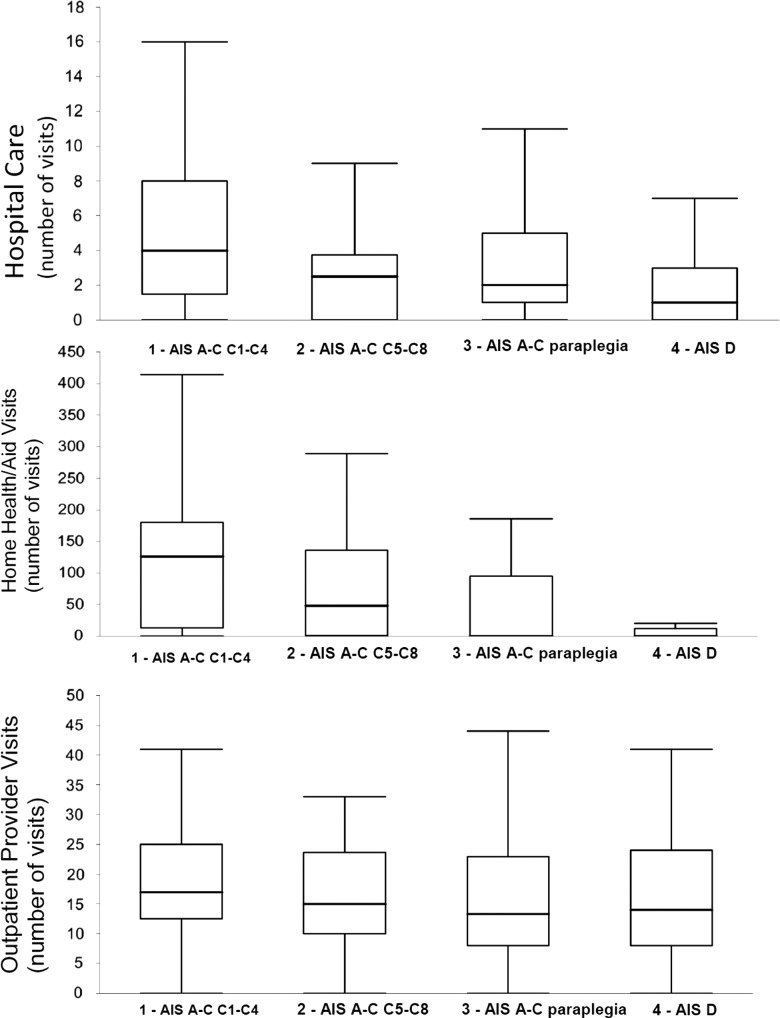
In the first year following IR, 45% of study participants were re-hospitalized, 57% visited an ER, and 26% required surgery. Twenty percent of patients were initially discharged to a SNF, but another 10% required SNF care during this first year. Most (86%) of the subjects reported being treated by a PCP. Overall, those with C1–4 AIS A–C injuries used the most services; they averaged 4 hospital encounters, 125 home care visits, and 17 outpatient visits. By comparison, participants in the AIS D group averaged about 1 hospital encounter, 25 home care visits, and 15 outpatient visits. Figure 1 provides boxplots for the three types of utilization by neurologic category.
Figure 1 .
Health-care utilization by neurologic injury.
Table 2 shows the frequency and duration of re-hospitalizations based on neurological level. The frequency with which those with greatest neurological impairment (C1–4 AIS A–C injuries) had any re-hospitalization was only modestly greater (63%) than for the next lower category of neurological impairment (C–C8 AIS A–C; 43%). However, the mean number of re-hospitalizations was considerably greater (2.4 vs. 1.1 episodes) as was the average re-hospitalization length of stay (19.8 vs. 8.0 days). The majority of participants with C1–C4 AIS A–C and C5–C8 AIS A–C who required re-hospitalization were hospitalized more than once during the 1-year period, while those with lesser neurological impairment who required re-hospitalization were more likely to have only a single episode of re-hospitalization.
Table 2 .
Frequency of re-hospitalizations by neurologic level of injury
| Overall (N = 169) |
Neurologic level |
|||||
|---|---|---|---|---|---|---|
| C1–C4 AIS A, B, C (N = 36) | C5–C8 AIS A, B, C (N = 23) | Paraplegia AIS A, B, C (N = 47) | AIS D (N = 61) | |||
| Subjects re-hospitalized | 73/163 (45%) | 22/35 (63%) | 10/23 (43%) | 23/45 (51%) | 17/58 (29%) | |
| Mean number of re-hospitalizations | 1.1 | 2.4 | 1.1 | 1.1 | 0.5 | |
| Number of re-hospitalizations (pro-rated counts are rounded to nearest integer) | N | Avg. days of hospitalization | N | N | N | N |
| 1 | 36 | 9.3 | 5 | 4 | 15 | 11 |
| 2 | 13 | 14.8 | 4 | 3 | 3 | 3 |
| 3 | 6 | 49.3 | 4 | 0 | 1 | 1 |
| 4 | 9 | 31.9 | 3 | 2 | 2 | 2 |
| 5 | 2 | 34.0 | 2 | 0 | 0 | 0 |
| 6 or more | 7 | 42.6 | 4 | 1 | 2 | 0 |
| Average re-hospitalization LOS | 9.1 | 19.8 | 8.0 | 5.8 | 5.8 | |
Health-care utilization correlations
Table 3 summarizes the results of the Poisson regression analysis. The values represent the percent expected frequency for individuals in the specific condition as compared to the alternative group(s) (vehicular vs. all other etiologies, white vs. non-white, discharge location of home vs. not, married vs. not, high school education and above vs. less than high school, and high tetraplegia vs. all other neurologic levels). For example, in the hospital care model, a subject who was discharged home would be expected to have 57% of the hospitalization rate of a subject who was not discharged home, i.e. 43% fewer hospitalizations. Being discharged home (vs. SNF) was significantly associated with a lower frequency of hospital care (including re-hospitalization, surgery, and ED visits). Falls (vs. vehicular crashes) as a cause for SCI was associated with lower use of in-home services. Married subjects attended significantly more outpatient visits compared to unmarried subjects. However, no difference was noted here in the amount of outpatient services utilized by each neurologic group. Age, sex, race, and education were unrelated to frequency of health-care utilization.
Table 3 .
Poisson regression results across health-care utilization type
| Hospital care | Home care | Outpatient provider | |
|---|---|---|---|
| Etiology | |||
| Violence (vs. vehicular) | 0.83 | ||
| Fall (vs. vehicular) | 0.10*** | ||
| Other (vs. vehicular) | 0.88 | ||
| Discharged home | 0. 57** | ||
| Married | 1.33** | ||
| Neurologic level | |||
| C5–C8 (vs. C1–C4) | 0.70 | 0.80 | |
| Paraplegia (vs. C1–C4) | 0.60* | 0.45*** | |
| D (vs. C1–C4) | 0.38** | 0.25*** |
Other factors used in the regression model included age, sex, race, and education; no significant difference among the health-care utilization domains were found.
*P < 0.05.
**P < 0.01.
***P < 0.001.
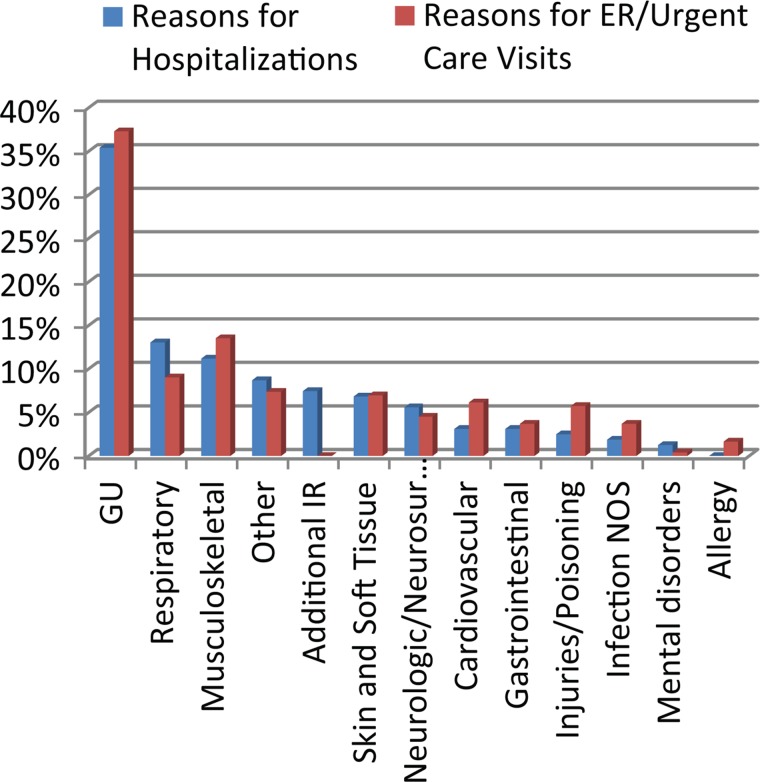
Reasons for re-hospitalization and emergency department/urgent care use
Figure 2 presents the proportion of encounters for re-hospitalization and ER/urgent care visits grouped by body system/cause. The most common diagnoses associated with re-hospitalization in the first year after IR were genitourinary causes, including urinary tract infection (35%), followed by respiratory conditions (12%). Additional IR was cited as the reason for re-hospitalization in 12% of the study population. Genitourinary and musculoskeletal conditions (including pain complaints) were the most common reasons for ER or urgent care visits.
Figure 2 .
Hospital and ER/urgent care health-care utilization by cause.
Discussion
There is a paucity of US-based studies examining factors that predispose patients with SCI to high levels of health-care use. Jaglal et al.4 found that 27.5% of patients in Canada with SCI were re-hospitalized during the first year post-discharge, and those patients tended to be older, had higher co-morbidity rates, longer mean acute care stay, lived in a rural area, and had 50 or more physician or specialists visits. Munce et al.5 examined physician and emergency department visits among adults with SCI in the first year after injury. Results suggested that women had more visits to their family practitioner compared to men, while men had more visits to a physiatrist. Older age (above 70 years), direct discharge to chronic care, and in-hospital complications were associated with ‘high utilization’ post-discharge.5 The concept of a high utilizer group was explored by Dorsett and Geraghty6 and Samsa et al.,7 who noted that pressure ulcer management and greater health-care use in the first 5 years after injury were related to higher overall use of resources over an average of 10–14 years.
In the US, examination of health-care utilization has primarily focused on re-hospitalization, with the rate in the first year after traumatic SCI among non-veterans administration (VA) cohorts reported as 27.2–33%.8–10 The rate of re-hospitalization in a 5-year VA-based cohort was as high as 90%.7 DeJong et al.9 prospectively examined the reasons for re-hospitalization in 951 patients with acute traumatic SCI and found that genitourinary, respiratory, and diseases of the skin and soft tissue were the most common admission diagnoses, which were similar to an earlier study.10 DeJong et al.9 found that female sex, Medicaid status, and younger age were associated with increased odds of re-hospitalization. In Canada, Dryden et al.11 reported people with traumatic SCI were hospitalized nearly three times more often, had a hospital length of stay 3 days longer, were nearly three times more likely to have outpatient physician contact, and required 30 times as much home care services as age and sex matched controls.
Overall, health-care utilization in the first year after IR was found to differ significantly by neurological level. Persons with tetraplegia, especially high tetraplegia, experienced more frequent hospitalizations and home care visits. Participants with the highest levels and greatest severity of injury (C1–C4 AIS A–C) were the highest users of all health-care services. However, when other variables were included in the regression models, those with C1–C4 AIS A–C did not significantly differ from those with C5–C8 AIS A–C. This suggests that these individuals are more alike in use of health-care services. This finding is consistent with the expectation that greater functional impairment results in greater need for resources and services to meet daily care requirements, and is associated with higher risk for complications requiring medical care, including multiple re-hospitalizations. We also found that those who discharged initially to a SNF used significantly more hospital care services than those discharged to the community. This most likely occurred because those with a higher burden of medical comorbidities required discharge to a SNF rather than to home, and the management of medical comorbidities necessitated greater hospital care service utilization. This finding is consistent with previously reported results.9
It is unclear why those with falls as the injury mechanism (58 subjects, or 34%) utilized fewer in-home services compared to the rest of the group. Falls are the most common etiology of SCI in people over the age of 60 years, and this group is statistically more likely to have more medical comorbidities and may require more home care. Age was not significantly associated with health-care utilization after controlling for neurological impairment. Married participants attended more outpatient services, possibly due to greater availability of support for and transportation to appointments.
Leading reasons for readmission in this study are similar to those described by Cardenas et al.10 and DeJong et al.,9 with diseases of the genitourinary system, diseases of skin and subcutaneous tissue including pressure ulcers, and diseases of the respiratory system being the most common causes. The re-hospitalization rate in the first year after IR in our cohort is slightly higher than the 2012 Model System rate of 36.5%,12 which may be due to the more frequent assessments of health-care use in this study.
Limitations of study
Data from this study were collected from a single hospital system from one region of the USA and may not be generalizable more broadly to the entire country. In addition, it is possible that the frequency of data collection (every 3 months), and the use of a self-report method may have introduced recall bias. It would be preferable for utilization to be measured from administrative records such as health insurance claims, but these data were not available for the present study. If data on medical co-morbidities was collected, it may have explained some of the variance in health-care use.
Finally, we do not have specific information on whether health-care use was planned or unplanned. For example, we expect that in most cases, the IR re-admit was planned at the time of discontinuation of spinal bracing or weight bearing precautions, or to learn advanced rehabilitation techniques. However, we did not collect that level of detail on re-hospitalizations.
Conclusion
Better understanding of service utilization in the first year after IR may help providers, policy makers, and patients plan for services that will be required. The findings, especially for individuals with high tetraplegia who are more likely to use more hospital care and home health than individuals with minimal neurological deficit (AIS D), support the need for comprehensive, coordinated IR discharge, and follow-up planning. Rates of re-hospitalization and ER visits could be reduced by specific interventions such as standardized discharge planning (especially for those discharging to a SNF) or by targeted education to reduce genitourinary and respiratory complications.
Disclaimer statements
Contributors The authors would like to thank Jason Barber for his efforts on statistical analysis.
Conflicts of interest None.
Ethics approval This was a secondary analysis of a prospective study; University of Washington IRB was obtained for that study.
Funding The study was done through a model systems center; the SCI model systems grant should be mentioned.
References
- 1.Devivo MJ. Epidemiology of traumatic spinal cord injury: trends and future implications. Spinal Cord 2012;50(5):365–72. [DOI] [PubMed] [Google Scholar]
- 2.Krause JS, Reed KS, McArdle JJ. A structural analysis of health outcomes after spinal cord injury. J Spinal Cord Med 2010;33(1):22–32. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Sirey JA, Meyers BS, Teresi JA, Bruce ML, Ramirez M, Raue PJ, et al. The Cornell Service Index as a measure of health service use. Psychiatr Serv 2005;56(12):1564–9. [DOI] [PubMed] [Google Scholar]
- 4.Jaglal SB, Munce SE, Guilcher SJ, Couris CM, Fung K, Craven BC, et al. Health system factors associated with rehospitalizations after traumatic spinal cord injury: a population-based study. Spinal Cord 2009;47(8):604–9. [DOI] [PubMed] [Google Scholar]
- 5.Munce SE, Guilcher SJ, Couris CM, Fung K, Craven BC, Verrier M, et al. Physician utilization among adults with traumatic spinal cord injury in Ontario: a population-based study. Spinal Cord 2009;47(6):470–6. [DOI] [PubMed] [Google Scholar]
- 6.Dorsett P, Geraghty T. Health-related outcomes of people with spinal cord injury – a 10 year longitudinal study. Spinal Cord 2008;46(5):386–91. [DOI] [PubMed] [Google Scholar]
- 7.Samsa GP, Landsman PB, Hamilton B. Inpatient hospital utilization among veterans with traumatic spinal cord injury. Arch Phys Med Rehabil 1996;77(10):1037–43. [DOI] [PubMed] [Google Scholar]
- 8.Johnson RL, Gerhart KA, McCray J, Menconi JC, Whiteneck GG. Secondary conditions following spinal cord injury in a population-based sample. Spinal Cord 1998;36(1):45–50. [DOI] [PubMed] [Google Scholar]
- 9.DeJong G, Tian W, Hsieh CH, Junn C, Karam C, Ballard PH, et al. Rehospitalization in the first year of traumatic spinal cord injury after discharge from medical rehabilitation. Arch Phys Med Rehabil 2013;944 Suppl:S87–97. [DOI] [PubMed] [Google Scholar]
- 10.Cardenas D, Hoffman J, Kirshblum S, McKinley W. Etiology and incidence of rehospitalization after traumatic spinal cord injury: a multicenter analysis. Arch Phys Med Rehabil 2004;85(11):1757–63. [DOI] [PubMed] [Google Scholar]
- 11.Dryden DM, Saunders LD, Rowe BH, May LA, Yiannakoulias N, Svenson LW, et al. Utilization of health services following spinal cord injury: a 6-year follow-up study. Spinal Cord 2004;42(9):513–25. [DOI] [PubMed] [Google Scholar]
- 12.National Spinal Cord Injury Statistical Center, University of Alabama at Birmingham, 2012 Annual Statistical Report-Complete Public Version. 2012.