Abstract
Objective
To investigate the reliability of ultrasonographic measurement of acromiohumeral distance (AHD) and the effects of shoulder positioning on AHD among manual wheelchair users (MWUs) with spinal cord injury (SCI) and an able-bodied control group.
Methods
Ten MWUs with SCI and 10 able-bodied subjects participated in this study. The ultrasonographic measurements of AHD from each subject were obtained by two raters during passive and active scapular plane arm elevation in neutral, 45°, 90° with and without resistance and in a weight relief raise position. The measurements were recorded again by each rater using the same procedures after a 30-minute time interval. All raters were blinded to each other's measurements.
Setting
University Laboratories and Veteran Affairs Healthcare System.
Results
Intra-rater (intraclass correlation coefficient, ICC > 0.83) and inter-rater (ICC > 0.78) reliability was excellent for both the MWUs with SCI and able-bodied groups across all arm positions except for the 45° position in the control group for one of the raters (intra-rater: ICC < 0.40 and inter-rater: ICC < 0.60). AHD significantly reduced when the shoulder was in the 90° arm elevated positions with or without resistance.
Conclusion
Findings from our study demonstrated that ultrasonography is a reliable means to evaluate AHD in both able bodied and individuals with SCI, who are known to have significant shoulder pathology. This technique could be used to develop reference measures and to identify changes in AHD caused by interventions.
Keywords: Ultrasound, Reliability, Shoulder positioning, Subacromial space, Spinal cord injury, Wheelchair
Introduction
Over 1.2 million individuals are living with a spinal cord injury (SCI) in the United States.1 Among these individuals, shoulder pain has a lifetime prevalence of over 70% and associates with essential repetitive weight bearing activities such as wheelchair transfers, weight relief raises, and wheelchair propulsion.2,3 Individuals with SCI are not able to rest a shoulder that becomes painful because of the reliance on the upper limbs for independence with mobility and other essential daily tasks, which may further perpetuate shoulder dysfunction. Subacromial impingement syndrome (SIS) is the most commonly reported condition related to shoulder dysfunction in individuals with SCI.4–6 SIS refers to the encroachment of the supraspinatus tendon of the rotator cuff as a result of a reduction in the subacromial space.7 The acromiohumeral distance (AHD) is a two-dimensional linear measurement of the subacromial space and a widely recognized marker for rotator cuff disease.8 AHD measurement has been well established in previous studies with able-bodied individuals with healthy shoulders,9–11 athletes,12–15 patients with SIS,16,17 patients with poststroke hemiplegia,11 individuals with different stages of rotator cuff degeneration,18 and patients with rotator cuff tear.8
Ultrasonography has increasingly been used as an imaging modality for measuring the AHD because it is portable, radiation-free, and non-invasive. A recent systematic review study also suggested that the ultrasonographic measurement of AHD is closely aligned with the measurements using radiograph, magnetic resonance imaging (MRI), and computed tomography.19 The reliability of AHD measurement by ultrasound has been assessed in many studies. For example, excellent intra-rater reliability (0.87–0.94) and moderate-to-excellent inter-rater reliability (0.64–0.92) of the AHD have been demonstrated using ultrasound in able-bodied individuals with healthy and impinged shoulders.9,17,20,21 Moderate intra- and inter-observer reliability using unmarked sonograms has also been reported.17 Discriminant validity of the AHD between affected and unaffected shoulders was determined in a hemiplegic population.11 However, no studies have yet examined AHD and the reliability of ultrasonographic measurement among wheelchair users (MWUs). The focus of this study could be important because ultrasound may be useful for quantitatively evaluating the AHD in a MWU population to gain insight into mechanisms of rotator cuff disease and SIS.
Shoulder positioning during ultrasound examination is one of the important factors to consider as it has been shown to impact the reliability of AHD measurement. Previous studies measured AHD with the shoulder in a resting neutral position8,16 as well as active or passive shoulder abduction at 45° and 90° arm elevation.22–24 Such studies have reported that the shoulder position might affect the reliability of AHD measurement.17 Superior humeral migration occurs in healthy individuals as the shoulder abducts from 0 to 90°.22,25 Within this range of shoulder motion, the upward force of the deltoid muscle overwhelms the stabilizing force of the rotator cuff muscles, resulting in a decreased AHD.23 Normal shoulder function is compromised in individuals with SCI due to altered scapulothoracic rhythm, glenohumeral kinematics, and muscle strength weaknesses and imbalances around the shoulder joint.5,26 These abnormalities may lead to greater compression of the subacromial space which could lead to subsequent shoulder impingement disorders. Therefore, the objectives of this study were to:
-
1.
Assess the intra-rater and inter-rater reliability of ultrasonographic measurement of AHD in MWUs with SCI (case) and an age and sex matched able-bodied population (control);
-
2.
Evaluate differences in the AHD as a function of shoulder position and muscle activation;
-
3.
Compare AHD measures between the case and control group.
We hypothesized that (1) ultrasonographic measurement of the AHD would be reliable (intraclass correlation coefficient, ICC > 0.8). (2) Effects of shoulder positions on the AHD changes would be different between MWUs with SCI and able-bodied controls due to the altered shoulder biomechanics and muscle imbalances that follow SCI.
Methods
Study design and general procedures
All participants read and signed the informed consent before participating in this study. The research protocol was approved by the Veteran Affairs Pittsburgh Healthcare System Institution Review Board. Participants were instructed not to perform strenuous activities for 24 hours before the testing sessions. Before starting the reliability session, participants transferred to a Biodex System 4 Isokinetic Dyanometer™ (Biodex Medical Systems, Inc, Shirley, New York) with custom-made adjustable height arm rests (Fig. 1A). Armrests were fitted to each participant to allow participants to pushup from a sitting position with full elbow extension and arms adducted to off-load the buttock tissues (Fig. 1B).
Figure 1 .
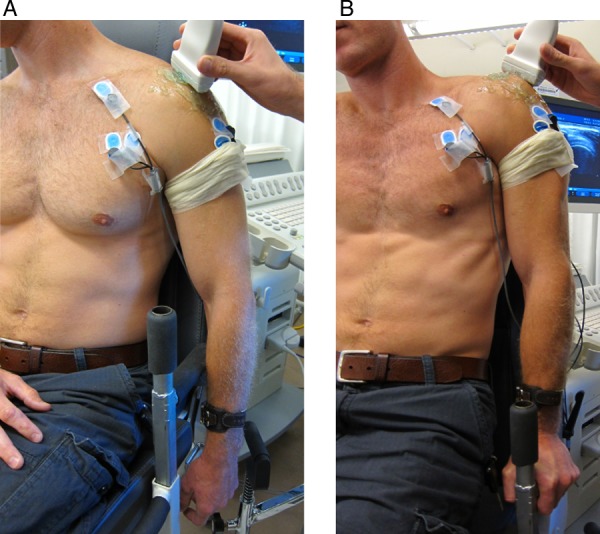
Imaging positions in the neutral resting (A) and weight relief raise position (B).
Age, height, weight, and date of injury/diagnosis were self-reported. Anthropometric data including shoulder circumference and upper arm length were measured before the experiment. The non-dominant side was chosen for all the measures in order to minimize the effects caused by performing activities of daily living on the dominant shoulder. A general questionnaire was used to document medical history including history of shoulder pain and surgery.27 MWUs with SCI completed the Wheelchair Users Shoulder Pain Index (WUSPI). The questionnaire contains 15 items to document shoulder pain during transfer, wheelchair mobility, personal care, and general activities. Each item is scored from 0 (lowest pain) to 10 (worst pain ever experienced) and summed to produce a total score between 0 and 150.
Participants
Two groups of participants were recruited, one being MWUs with SCI and the other one being able-bodied volunteers. The individuals with SCI must have had their injury for more than one year and use a manual wheelchair as their primary means for mobility. Inclusion criteria for both groups were 18 years of age or older, English speaking, and able to complete weight relief raises. Exclusion criteria for both groups included having a history of fractures or dislocations in the shoulder girdle, elbow, and wrist from which the participant had not fully recovered, the presence of implants or pacemakers, and any pain in an upper limb that could interfere with normal function and activity. Convenience sample of MWUs with SCI were recruited through a research registry of MWUs. Able-bodied participants were chosen by matching their sex and age within 5 years of each MWU with SCI.
AHD reliability protocols
The subacromial space was quantified by measuring the AHD using ultrasound techniques as described in a previous study.28 Two ultrasound operators underwent training to learn the techniques and then practiced on healthy volunteers to become familiar with the protocol and measurement procedure before the reliability study. A Philips HD11 1.0.6 ultrasound machine (Philips Healthcare, Andover, MA, USA) with a 5–12 MHz linear transducer was used to scan the shoulder from the anterior aspect of glenoid to the flat segment of posterior scapula to capture the bright reflection of the bony contour of the acromion and humeral head (Fig. 2).
Figure 2 .
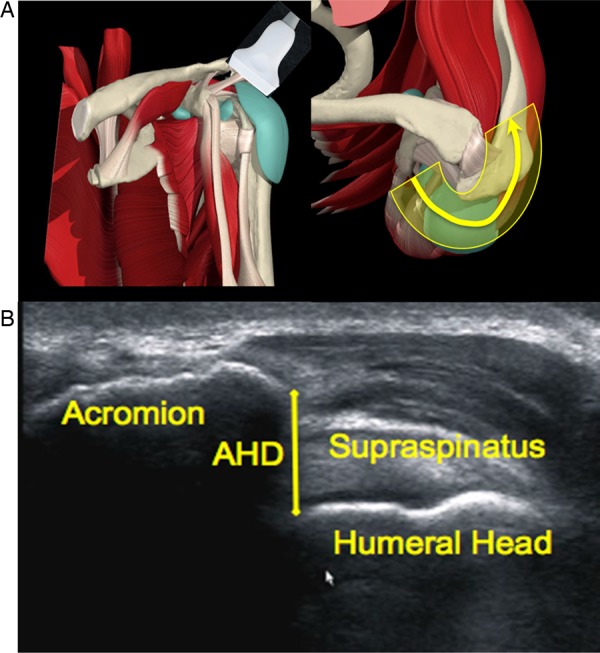
Ultrasonographic probe positioning (Left A) and path (Right A) and one snapshot of the video-based ultrasonographic measurement of the acromiohumeral distance (B).
Ultrasound video was recorded at 10 Hz for the duration of scanning, which took approximately 10 seconds. Each rater recorded the AHD video in randomized order in the following shoulder positions: neutral resting position (neutral), arm abducted at 45° and 90° in scapular plane (with and without resistance), and isometrically holding the weight relief raise position (WR) (Fig. 1B). For the arm abduction trials, participants were instructed to grab the handle of the Biodex which was set to 45° and 90° of arm elevation in the scapular plane (Fig. 3).
Figure 3 .
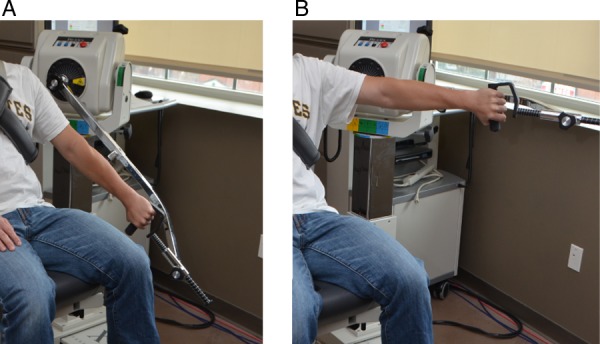
Participants maintained their arm at the prescribed angle of shoulder elevation by grabbing the handle bar of the Biodex. Ultrasound images were collected at 45° (A), and 90° (B) at scapular plane elevation with humeral internal rotation with and without weight.
Participants grabbed the handle with the arm internally rotated and thumb downward. The Biodex was used to provide a 5-lb weight in the active trials (45A, 90A) and provided no resistance in the passive trials (45P, 90P).22 The weight was determined through pilot testing and was determined to provide adequate muscle activity without causing discomfort to the participant. For the weight relief raises, the participants were instructed to hold the buttocks off the seat with both elbows in locked positions for the entire duration of the scanning (Time 1).29 The AHD videos were recorded again by each rater using the same procedures after a 30-minute time interval (Time 2). All raters were blinded to each other's measurements.
Data analysis
An investigator blinded to the subject's shoulder positions and timing of the video reviewed each frame of the video and marked the most inferior point of acromion and the most superior point of humeral head using a customized Matlab program. The narrowest distance between the bony landmarks was calculated and used for statistical analyses. A subset of the videos (n = 120) were randomly and independently analyzed by a second investigator to access intra- and inter-video reliability of the manual techniques used to post-process the images. Reliability of the post-processing procedures and the ultrasound image data collected by two raters were assessed using ICC (two-way random, absolute agreements). The following ICC interpretation scale was used: almost perfect (0.81–1), excellent (0.61–0.80), moderate (0.41–0.60), and poor to fair (below 0.40).30 The accuracy for each rater was examined using standard error of measurement (SEM) and the minimum detectable difference (MDD). The SEM, a quantitative estimate of the average error of the measurement, was calculated to determine 95% confidence intervals around individual measurements.31 The MDD was computed to describe the smallest threshold to detect true AHD changes beyond the measurement error at a confidence interval of 90%.32 χ2 or independent t-tests depending on the nature of the variable were used to compare demographic differences between the case and control groups. A two-way mixed-design analysis of variance was used to identify differences in the AHD between groups and shoulder positions. Significant main effects in position and interaction effects were further examined using pair-wise statistics. A Bonferroni correction was applied to accommodate adjustment for the bias of 11 pairwise comparisons for examining neutral (N), passive and active muscle conditions (N vs. 45P, N vs. 45A, N vs. 90P, N vs. 90A, N vs. WR, 45P VS. 45A, 45P vs. 90P, 45A vs. 90A, 90P vs. 90A, 45A vs. WR, 90A vs. WR). The alpha corrected level for these comparisons was set to 0.005. Trends in the data were noted for a level of significance under 0.1. Pearson's or Spearman's correlation statistics were used where appropriate to examine the relationships between the AHD measures and subject height, weight, shoulder circumference, arm length, age, years since injury (only case group), and shoulder pain (only case group).
Results
Subjects characteristics
Ten MWUs with a spinal cord injury including nine men and one woman (two with tetraplegia and eight with paraplegia) and ten able-bodied individuals including eight men and two women participated in the study. The demographic data and statistical results are summarized in Table 1. Shoulder circumference was significantly positively correlated with AHD at the 45P (r = 0.74, P = 0.02) and WR (r = 0.65, P = 0.04) positions in the case group only. No other subject characteristics or the WUSPI score as shown in Table 1 was related to the AHD measures.
Table 1 .
Subject characteristics
| Case (n = 10) | Control (n = 10) | P value | |
|---|---|---|---|
| Age | 34.8 ± 10.4 | 35.8 ± 11.5 | 0.84 |
| Range 25–55 | Range 20–53 | ||
| Height (inches) | 68.2 ± 4.9 | 68.8 ± 3.6 | 0.78 |
| Range 60–75 | Range 61–73 | ||
| Weight (lbs) | 152.9 ± 10.4 | 175.1 ± 29.7 | 0.28 |
| Range 101–283 | Range 124–215 | ||
| Years Since Injury (years) | 14.75 | N/A | |
| Range (3–27) | |||
| WUSPI | 17.54 ± 23.13 | N/A | |
| Range (0–65.32) | |||
| Shoulder circumference (cm) | 46.13 ± 7.41 | 46.49 ± 4.24 | 0.27 |
Reliability of ultrasonographic AHD measurement
The intra-rater (ICC > 0.83) and inter-rater (ICC > 0.78) reliability of AHD measurement for each shoulder position was excellent among MWUs with SCI (Table 2). For rater 2, the ICC values for the intra-rater reliability of the AHD measurement were almost perfect in MWUs with SCI (ICC > 0.90) and able-bodied individuals (ICC > 0.81) (Table 2). For the AHD measured by rater 1 in able-bodied, the intra-rater reliability was fair to poor (ICC<0.40) at 45A and excellent for all other positions (ICC>0.85). Inter-rater reliability was excellent to almost perfect (ICC > 0.78) at both time points for the case group at all shoulder positions. Inter-rater reliability was excellent (ICC > 0.75) at both time points for the control group for all shoulder positions except at 45A in time 1 (ICC<0.60). The inter- and intra-video reliability was almost perfect (ICC>0.81) (Table 2).
Table 2 .
Intra- and inter-class correlation coefficients
| MWUs with SCI (n = 10) |
Able-bodied subjects (n = 10) |
|||
|---|---|---|---|---|
| Intraclass correlation coefficients | ||||
| Position | Rater 1 | Rater 2 | Rater 1 | Rater 2 |
| Neutral | 0.83 (0.33–0.96) | 0.98 (0.93–0.99) | 0.94 (0.74–0.98) | 0.95 (0.78–0.99) |
| 45A | 0.94 (0.72–0.0.99) | 0.93 (0.72–0.98) | 0.24 (−3.06–0.82) | 0.96 (0.83–0.99) |
| 45P | 0.92 (0.68–0.98) | 0.97 (0.88–0.99) | 0.69 (−0.08–0.92) | 0.85 (0.38–0.96) |
| 90A | 0.90 (0.62–0.98) | 0.97 (0.88–0.99) | 0.88 (0.54–0.97) | 0.81 (0.24–0.95) |
| 90P | 0.92 (0.69–0.98) | 0.90 (0.62–0.98) | 0.97 (0.87–0.99) | 0.92 (0.68–0.98) |
| WR | 0.93 (0.70–0.98) | 0.93 (0.73–0.98) | 0.85 (0.41–0.96) | 0.96 (0.86–0.99) |
| Interclass correlation coefficients | ||||
| Position | Time 1 | Time 2 | Time 1 | Time 2 |
| Neutral | 0.78 (0.19–0.94) | 0.92 (0.67–0.98) | 0.85 (0.38–0.96) | 0.95 (0.82–0.99) |
| 45A | 0.93 (0.72–0.98) | 0.95 (0.83–0.99) | 0.52 (−1.25–0.89) | 0.88 (0.50–0.97) |
| 45P | 0.84 (0.34–0.96) | 0.95 (0.80–0.99) | 0.84 (0.30–0.96) | 0.66 (−0.42–0.92) |
| 90A | 0.86 (0.41–0.97) | 0.94 (0.76–0.99) | 0.75 (−0.08–0.94) | 0.84 (0.36–0.96) |
| 90P | 0.94 (0.79–0.99) | 0.93 (0.70–0.98) | 0.83 (0.26–0.96) | 0.94 (0.73–0.98) |
| WR | 0.89 (0.59–0.97) | 0.97 (0.88–0.99) | 0.75 (−0.08–0.94) | 0.89 (0.52–0.97) |
| Intra-video reliability | Inter-video reliability | |||
| 0.81 (0.71–0.87) | 0.85 (0.78–0.90) | |||
Data are given as average-measure values (lower-upper bound 95% confidence interval).
Time: Time order of recorded ultrasound video.
Neutral: neutral resting position; 45A, 45P: Arm fully extension with humeral internal rotation at 45° in scapular plane with and without resistance; 90A, 90P: Arm fully extension with humeral internal rotation at 90° in scapular plane with and without resistance; WR: Holding the weight relief raise position
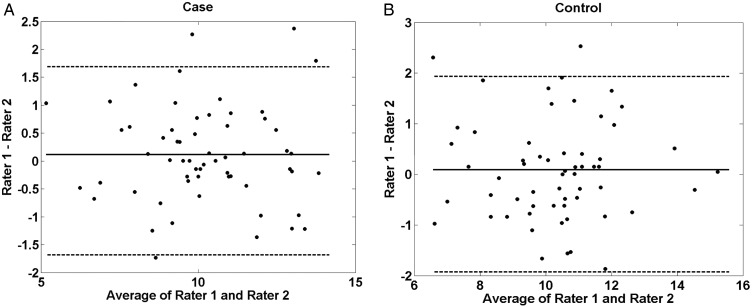
Fig. 4 shows the agreement among raters for the AHD measurements across all shoulder positions in both groups. The Bland–Altman plots were used to compare the individual differences in the AHD for both raters. Most of the differences were within the limits of agreement and differences between two raters were small and close to 0. The variability was random and uniform throughout all six shoulder positions in the case (Fig. 4A) and control groups (Fig. 4B). The AHD measurements for both groups are shown in Table 3.
Figure 4 .
Bland–Altman plot of average rater 1 and 2 of the AHD measurement in MWUs with SCI (A) and able-bodied (B). Dotted line represents 1.96 standard deviations above and below the mean difference.
Table 3 .
Ultrasonographic measurement of acromiohumeral distance in six shoulder positions (averaged across both time points)
| AHD (mm) | MWUs with SCI (n = 10) |
Able-bodied subjects (n = 10) |
||
|---|---|---|---|---|
| Position | Rater 1 | Rater 2 | Rater 1 | Rater 2 |
| Neutral | 11.43 ± 1.59*,** | 11.13 ± 1.51*,** | 11.38 ± 1.71*,** | 11.41 ± 1.73*,** |
| 45A | 10.07 ± 1.91 | 9.90 ± 2.18 | 9.72 ± 1.16 | 9.75 ± 2.08 |
| 45P | 10.97 ± 1.92** | 10.77 ± 2.06** | 11.60 ± 1.75** | 11.36 ± 1.46** |
| 90A | 9.24 ± 2.38* | 9.25 ± 1.93* | 8.94 ± 1.44* | 8.58 ± 1.38* |
| 90P | 9.78 ± 2.35** | 9.78 ± 2.40** | 9.50 ± 2.23** | 9.49 ± 1.67** |
| WR | 10.18 ± 1.46* | 10.17 ± 1.96* | 10.60 ± 1.14* | 10.61 ± 1.45* |
*AHD at 90A was significantly narrower than the neutral and WR positions (P < 0.001).
**AHD at 90P was significantly narrower than neutral and 45P (P ≤ 0.004).
Neutral: neutral resting position; 45A, 45P: Elbow fully extended with humeral internal rotation (thumb down) at 45° in scapular plane with and without resistance, respectively; 90A, 90P: Elbow fully extended with humeral internal rotation (thumb down) at 90° in scapular plane with and without resistance, respectively; WR: Holding the weight relief raise position.
Effects of shoulder positioning and group type on the AHD
The AHD was the widest in the neutral resting position and narrowest in the 90A position. The SEM and MDD were less than 0.73 and 1.71 mm, respectively (Table 4). There was a significant main effect of arm position (P < 0.001). The AHD was significantly narrower at 90P compared with neutral and 45P (P ≤ 0.004). We found that AHD at 90A was significantly narrower than at neutral and WR (P < 0.001). There were no interaction effects (P = 0.484, small effect d = 0.23) among shoulder positions and groups.
Table 4 .
Standard error of measurement (SEM) and minimum detectable difference (MDD) of AHD measurement in six shoulder positions
| MWUs with SCI (n = 10) |
Able-bodied subjects (n = 10) |
|||
|---|---|---|---|---|
| SEM (mm) | MDD (mm) | SEM (mm) | MDD (mm) | |
| Rater 1 | ||||
| Neutral | 0.66 | 1.53 | 0.42 | 0.98 |
| 45A | 0.47 | 1.09 | 1.01 | 2.35 |
| 45P | 0.54 | 1.27 | 0.97 | 2.27 |
| 90A | 0.75 | 1.76 | 0.50 | 1.16 |
| 90P | 0.66 | 1.55 | 0.39 | 0.90 |
| WR | 0.39 | 0.90 | 0.44 | 1.03 |
| Rater 2 | ||||
| Neutral | 0.21 | 0.50 | 0.39 | 0.90 |
| 45A | 0.58 | 1.35 | 0.42 | 0.97 |
| 45P | 0.36 | 0.83 | 0.56 | 1.32 |
| 90A | 0.33 | 0.78 | 0.60 | 1.40 |
| 90P | 0.76 | 1.77 | 0.47 | 1.10 |
| WR | 0.52 | 1.21 | 0.29 | 0.68 |
| Inter-rater | ||||
| Neutral | 0.70 | 1.63 | 0.65 | 1.52 |
| 45A | 0.53 | 1.23 | 1.08 | 2.51 |
| 45P | 0.77 | 1.80 | 0.62 | 1.44 |
| 90A | 0.78 | 1.82 | 0.66 | 1.55 |
| 90P | 0.58 | 1.35 | 0.77 | 1.81 |
| WR | 0.56 | 1.31 | 0.61 | 1.43 |
Discussion
To our knowledge, this is the first study to quantify the subacromial space in manual MWUs using ultrasound techniques. In addition, the narrowest AHD was determined by sorting through a sequence of images collected using video-based methods versus relying on a single “snap-shot” image taken during the course of scanning.33 While our methods matched up well (or better in some cases) compared with prior studies, our results also indicate that rater training and practice are more important to ensuring that the AHD is reliable.
Reliability of ultrasonographic AHD measurement
The results showed excellent intra-rater and inter-rater reliability among individuals with SCI. The inter-rater reliability in the able-bodied population is moderate to excellent and consistent with previous studies.16,17 However, the intra-rater reliability at 45° arm elevation with humeral internal rotation for rater 1 was poor to fair. Pijls et al. reported high to excellent inter-rater reliability but moderate intra-rater reliability in individuals with impingement at 60° abduction without restricting the humeral internal and external rotation. It is unclear how the intra-rater reliability of AHD measurement was influenced by humeral internal rotation in 45° abduction in the scapular plane as other studies have not reported this data. Because intra-rater ICC's were almost perfect for both raters in this shoulder position for the case group, it may be due to a learning effect since most control subjects were tested before the case subjects. Our study found that the reliability of the AHD measurement in MWUs with SCI, whose shoulders are prone to shoulder instability, pathologies, and altered kinematics, is consistent with those reported in control groups, subjects with impingement, and poststroke hemiplegia.9,11,17
The SEM of AHD measured in the shoulder neutral position was smaller than that in recent findings (e.g. 0.60 and 0.66 mm for intra-observer and 0.85 mm for intra-observer repeatability) in healthy male subjects.10 The maximum MDD found in our case group (1.82 mm) and our control group (2.51 mm) were similar to the range reported for the unaffected (1–3 mm) and affected shoulder (2–4 mm) among individuals with poststroke hemiplegia.11 The MDD describes the smallest threshold to detect true AHD changes beyond the measurement error. On an individual basis, knowing this threshold could help identify patients who improve after a treatment or intervention designed to increase the size of the subacromial space. Future studies are needed to determine the amount of change beyond the MDD that is clinically meaningful.
Ultrasonographic bone surfaces are less affected by gain, depth, focal zones, or slight tilting or translation from the ultrasound probe due to the dramatic difference in acoustic impedance between bone and soft tissue. Therefore, we expected rater scanning errors to be minimized.34 In fact, we found that sources of variability in our ultrasound technique were more likely to stem from the video analysis and selection of the 2D slice. There was some uncertainty with the selection of the narrowest distance from the sequence of images collected by the video and the manual determination of the feature points on the acromion and humeral head within and between the video observers. The sub-analysis of the post-processing technique on the 120 videos, however, showed excellent intra- and inter-video reliability (ICC > 0.81) for the methods used.
Effects of shoulder positioning
Consistent with previous studies, greater AHD narrowing was found during scapular plane elevation with humeral internal rotation in healthy subjects.22 Maenhout et al. reported similar AHD reduction in 29 elite athletes and 33 recreational athletes using sonographic elevation during the first 45° active shoulder abduction.21 However, no information was provided on the actual AHD at 90° of abduction in these populations. Our findings are also consistent with a previous MRI study that found the co-contraction imbalance between deltoids and shoulder depressors was most prominent around 90° abduction, resulting in a narrower subacromial space.35 Giphart et al. studied the AHD during arm elevation starting from 20° to 150° using dynamic in vivo biplane fluoroscopy in eight healthy male subjects. They reported the shortest AHD was 2.6 ± 0.8 mm, located between the supraspinatus footprint and the greater tuberosity during scapular plane elevation at 72° ± 12°.36,37 However, the shortest AHD in our study was 8.58 ± 1.38 mm at 90°. The results from biplane videography methods are not comparable with ours since the positioning of the subjects during movement and the determination of the anatomic distance may be factors influencing AHD. Although biplane videography is known as the most accurate in vivo and non-invasive method for measuring joint movement and AHD in three-dimensional space, this method poses a risk on subjects to radiation exposure and is difficult for clinicians to use. Moreover, the modality is not widely available in rehabilitation clinics.
Our study did not find significant narrowing of the subacromial space between the neutral and WR position for either subject group. This result opposes the common belief among clinical practitioners that the push-up position prompts humeral head migration and compression of the rotator cuff.38 During the WR raise, the scapula may change orientation in such a way as to protect the space.29 A previous electromyography study also reported that the shoulder depressors (sternal pectoralis major, infraspinatus) and scapulothoracic (serratus anterior) muscles were active at 10–29% of their maximal voluntary contraction levels while holding the weight relief raise.39 Better glenohumeral alignment, altered positioning of the scapula and activation of depressor and scapular-thoracic muscles may all serve as protective mechanisms for preventing the humeral head from migrating into the joint during WR.39
Numerous studies have found that working above shoulder height increases risk of pain and injury (see CPG recommendation 5b). We also found that a greater amount of narrowing occurred in the 90A and 90P positions compared with the WR position. These results agree with a previous study that found when the arm is below shoulder height, the humeral head can be aligned better with the glenoid cavity, which enhances joint stability, minimizes the effects of external forces acting on the joint, and reduces the amount of muscle force needed for stabilization.40 Our results point to over-shoulder positioning posing a greater risk for impingement than WR push-ups among MWUs. Overhead activities should be avoided to help protect the subacromial space from impingement syndrome.
AHD differences between case and control
The mean AHD measures obtained in our control group are similar to published data from a previous study utilizing ultrasound imaging technique (mean: 10.9 mm, range: 5.9–19.6 mm).9 There were no significant differences in the AHD between healthy individuals and MWUs with SCI. The lack of group differences may be because asymptomatic shoulders were recruited in both groups. The results may not be generalized to MWUs with SCI and with shoulder pain. Previous studies have reported that AHD tended to show more pronounced dynamic narrowing among persons with SIS compared to those without impingement.16 Similar group differences were also found in athlete populations, where the AHD was narrower during 45A in recreational athletes compared with elite handball athletes.21 The etiological mechanisms responsible for this reduction in space are unclear. Possible explanations for these mechanisms include glenohumeral instability, humeral translations and decreased scapular posterior tipping and upward rotation reported during scapular plane humeral elevation in previous studies among persons with SIS.41 Future studies are needed to investigate the associations between scapular and humeral kinematics and the AHD.
Study considerations
The lack of a difference between the case and control group could be attributed to the small sample size or enrollment of MWUs with low levels of shoulder pain. Although the results showed excellent inter- and intra-rater reliability of the AHD measurement, the accuracy of the ultrasonographic measurement was not examined in this study. Azzoni et al., however, compared the accuracy of sonographic measurements with radiographic measurements of AHD and found both measurements were highly correlated, with a concurrent validity was 0.77–0.85.18,42 In addition, high correlation has also been demonstrated between AHD measurements taken from radiographs and MRI (r = 0.81).43 As mentioned earlier, in our study the narrowest distance was determined from manual selection of a single frame from the video clip and the manual determination of the feature points on the acromial and humeral head. While the inter- and intra-video reliability was excellent, it may be possible to improve it further by averaging the narrowest distances found for several sequential snapshots or with an automated post-processing technique. While there is certainly room for improvement in these techniques, rater-scanning reliability appears to be a greater issue affecting the AHD measure. In this study, controls were tested before cases and the ordering of shoulder positions within each group were not randomized. It is possible that the lower values of reliability found in this study are explained by a learning effect. Thus, training and practice are essential for achieving the highest degree of reliability with ultrasound techniques.
Conclusions
Findings from our study demonstrate that ultrasonography is a reliable means to evaluate the subacromial space in manual MWUs with SCI and can provide reference measures (e.g. MDD) for identifying meaningful differences in future interventional type studies. Video-based ultrasonographic measurement of AHD showed excellent intra- and inter-observer reliability and qualifying it a potential technique to investigate the mechanism of subacromial space narrowing. Our findings have increased our understanding of the effects of greater scapular arm elevation on the subacromial space narrowing among individuals with SCI. Future studies are needed to further evaluate the relationship between subacromial space narrowing and other activities of daily living such as wheelchair transfers, wheelchair propulsion, and overhead activities.
Acknowledgements
The authors thank Nathan Hogaboom for his help with data collection and thank Janine Carlock for the proofreading. This material is based upon work supported by the Department of Veterans Affairs Rehabilitation Research and Development Service (Grant Number: B6789C). This material is the result of work supported with resources and the use of facilities at the Human Engineering Research Laboratories, VA Pittsburgh Healthcare System. The contents of this abstract do not represent the views of the Department of Veterans Affairs or the United States Government.
Disclaimer statements
Contributors Y-SL, MLB and AMK provided concept/idea/research design. Y-SL and KAD provided data acquisition and analysis. Y-SK and AMK provided data interpretation. MLB provided consultation, project management, and facilities/equipment.
Conflicts of interest None.
Ethics approval This study received the approval from the institutional review board of Veteran Affairs Pittsburgh Healthcare System.
Funding VA Rehabilitation R&D Center of Excellence, Project B6789C, Department of Veterans Affairs.
References
- 1.Anonymous. Paralysis Facts and Figures. Christopher & Dana Reeve Foundation [accessed 2 May 2014]. Available from: http://www.christopherreeve.org/site/c.mtKZKgMWKwG/b.5184189/k.5587/Paralysis_Facts__Figures.htm
- 2.Dalyan M, Cardenas DD, Gerard B. Upper extremity pain after spinal cord injury. Spinal Cord 1999;37(3):191–5. [DOI] [PubMed] [Google Scholar]
- 3.Collinger JL, Boninger ML, Koontz AM, Price R, Sisto SA, Tolerico ML, et al. Shoulder biomechanics during the push phase of wheelchair propulsion: a multisite study of persons with paraplegia. Arch Phys Med Rehabil 2008;89(4):667–76. [DOI] [PubMed] [Google Scholar]
- 4.Bayley JC, Cochran TP, Sledge CB. The weight-bearing shoulder. The impingement syndrome in paraplegics. J Bone Joint Surg Am 1987;69(5):676–8. [PubMed] [Google Scholar]
- 5.Lee TQ, McMahon PJ. Shoulder biomechanics and muscle plasticity: implications in spinal cord injury. Clin Orthop 2002;403Suppl:S26–36. [DOI] [PubMed] [Google Scholar]
- 6.Dyson-Hudson TA, Kirshblum SC. Shoulder pain in chronic spinal cord injury, part I: epidemiology, etiology, and pathomechanics. J Spinal Cord Med 2004;27(1):4–17. [DOI] [PubMed] [Google Scholar]
- 7.Michener LA, McClure PW, Karduna AR. Anatomical and biomechanical mechanisms of subacromial impingement syndrome. Clin Biomech (Bristol, Avon.) 2003;18(5):369–79. [DOI] [PubMed] [Google Scholar]
- 8.Cholewinski JJ, Kusz DJ, Wojciechowski P, Cielinski LS, Zoladz MP. Ultrasound measurement of rotator cuff thickness and acromio-humeral distance in the diagnosis of subacromial impingement syndrome of the shoulder. Knee Surg Sports Traumatol Arthrosc 2008;16(4):408–14. [DOI] [PubMed] [Google Scholar]
- 9.Schmidt WA, Schmidt H, Schicke B, Gromnica-Ihle E. Standard reference values for musculoskeletal ultrasonography. Ann Rheum Dis 2004;63(8):988–94. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Cheng SC, Hulse D, Fairbairn KJ, Clarke M, Wallace WA. Comparison of dynamic ultrasound and stress radiology for assessment of inferior glenohumeral laxity in asymptomatic shoulders. Skeletal Radiol 2008;37(2):161–8. [DOI] [PubMed] [Google Scholar]
- 11.Kumar P, Bradley M, Gray S, Swinkels A. Reliability and validity of ultrasonographic measurements of acromion-greater tuberosity distance in poststroke hemiplegia. Arch Phys Med Rehabil 2011;92(5):731–6. [DOI] [PubMed] [Google Scholar]
- 12.Maenhout A, Van Eessel V, Van Dyck L, Vanraes A, Cools A. Quantifying acromiohumeral distance in overhead athletes with glenohumeral internal rotation loss and the influence of a stretching program. Am J Sports Med 2012;40(9):2105–12. [DOI] [PubMed] [Google Scholar]
- 13.Wang H-K, Lin J-J, Pan S-L, Wang T-G. Sonographic evaluations in elite college baseball athletes. Scand J Med Sci Sports 2005;15(1):29–35. [DOI] [PubMed] [Google Scholar]
- 14.Girometti R, De Candia A, Sbuelz M, Toso F, Zuiani C, Bazzocchi M. Supraspinatus tendon US morphology in basketball players: correlation with main pathologic models of secondary impingement syndrome in young overhead athletes. Preliminary report. Radiol Med 2006;111(1):42–52. [DOI] [PubMed] [Google Scholar]
- 15.Silva RT, Hartmann LG, De Souza Laurino CF, Biló JPR. Clinical and ultrasonographic correlation between scapular dyskinesia and subacromial space measurement among junior elite tennis players. Br J Sports Med 2010;44(6):407–10. [DOI] [PubMed] [Google Scholar]
- 16.Desmeules F, Minville L, Riederer B, Cote CH, Fremont P. Acromio-humeral distance variation measured by ultrasonography and its association with the outcome of rehabilitation for shoulder impingement syndrome. Clin J Sport Med 2004;14(4):197–205. [DOI] [PubMed] [Google Scholar]
- 17.Pijls BG, Kok FP, Penning LIF, Guldemond NA, Arens HJ. Reliability study of the sonographic measurement of the acromiohumeral distance in symptomatic patients. J Clin Ultrasound 2010;38(3):128–34. [DOI] [PubMed] [Google Scholar]
- 18.Azzoni R, Cabitza P, Parrini M. Sonographic evaluation of subacromial space. Ultrasonics 2004;42(1–9):683–7. [DOI] [PubMed] [Google Scholar]
- 19.McCreesh KM, Crotty JM, Lewis JS. Acromiohumeral distance measurement in rotator cuff tendinopathy: is there a reliable, clinically applicable method? A systematic review. Br J Sports Med 2015;49(5):298–305 [DOI] [PubMed] [Google Scholar]
- 20.Kumar P, Bradley M, Swinkels A. Within-day and day-to-day intrarater reliability of ultrasonographic measurements of acromion-greater tuberosity distance in healthy people. Physiother Theory Pract 2010;26(5):347–51. [DOI] [PubMed] [Google Scholar]
- 21.Maenhout A, van Cingel R, De Mey K, Van Herzeele M, Dhooge F, Cools A. Sonographic Evaluation of the Acromiohumeral Distance in Elite and Recreational Female Overhead Athletes. Clin J Sport Med 2013;23(3):178–83. [DOI] [PubMed] [Google Scholar]
- 22.Graichen H, Bonel H, Stammberger T, Eeglmeier KH, Reiser M, Eckstein F. Subacromial space width changes during abduction and rotation – A 3-D MR imaging study. Surg Radiol Anat 1999;21(1):59–64. [DOI] [PubMed] [Google Scholar]
- 23.Chopp JN, O'Neill JM, Hurley K, Dickerson CR. Superior humeral head migration occurs after a protocol designed to fatigue the rotator cuff: a radiographic analysis. J Shoulder Elbow Surg 2010;19(8):1137–44. [DOI] [PubMed] [Google Scholar]
- 24.Seitz AL, McClure PW, Finucane S, Ketchum JM, Walsworth MK, Boardman ND, et al. The scapular assistance test results in changes in scapular position and subacromial space but not rotator cuff strength in subacromial impingement. J Orthop Sports Phys Ther 2012;42(5):400–12. [DOI] [PubMed] [Google Scholar]
- 25.Lippitt S, Matsen F. Mechanisms of glenohumeral joint stability. Clin Orthop Relat Res 1993;Jun(291):20–8. [PubMed] [Google Scholar]
- 26.Mulroy SJ, Gronley JK, Newsam CJ, Perry J. Electromyographic activity of shoulder muscles during wheelchair propulsion by paraplegic persons. Arch Phys Med Rehabil 1996;77(2):187–93. [DOI] [PubMed] [Google Scholar]
- 27.Boninger ML, Towers JD, Cooper RA, Dicianno BE, Munin MD. Shoulder imaging abnormalities in individuals with paraplegia. J Rehabil Res Dev 2001;38(4):401–8. [PubMed] [Google Scholar]
- 28.Lin YS, Koontz AM, Worobey LA, Boninger ML. Effect of muscle fatiguing tasks on subacromial space in wheelchair users. In: Proceedings of the Rehabilitation Engineering and Assistive Technology Society of North America Conference [CD-ROM]. Baltimore, MD; Jun 28–Jul 3; 2012. [Google Scholar]
- 29.Morrow MMB, Kaufman KR, An KN. Scapula kinematics and associated impingement risk in manual wheelchair users during propulsion and a weight relief lift. Clin Biomech (Bristol, Avon) 2011;26(4):352–7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Landis J, Koch G. The measurement of observer agreement for catagorical data. Biometrics 1977;33(1):159–74. [PubMed] [Google Scholar]
- 31.Portney LG, Watkins MP. Foundations of clinical research applications to practice. 3rd ed. Upper Saddle River, NJ: Pearson Education, Inc.; 2009. [Google Scholar]
- 32.Collinger JL, Gagnon D, Jacobson J, Impink BG, Boninger ML. Reliability of quantitative ultrasound measures of the biceps and supraspinatus tendons. Acad Radiol 2009;16(11):1424–32. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Seitz AL, Michener LA. Ultrasonographic measures of subacromial space in patients with rotator cuff disease: A systematic review. J Clin Ultrasound 2011;39(3):146–54. [DOI] [PubMed] [Google Scholar]
- 34.Sanders RC, Winder TC. Clinical sogography: a practical guideline, 4th ed Baltimore: Lippincott Williams & Wilkins; 2007. [Google Scholar]
- 35.Hinterwimmer S, Von Eisenhart-Rothet R, Siebert M, Putz R, Eckstein F, Vogl T, et al. Influence of Adducting and Abducting Muscle Forces on the Subacromial Space Width. Med Sci Sports Exerc 2003;35(12):2055–9. [DOI] [PubMed] [Google Scholar]
- 36.Giphart JE, van der Meijden OA, Millett PJ. The effects of arm elevation on the 3-dimensional acromiohumeral distance: a biplane fluoroscopy study with normative data. J Shoulder Elbow Surg 2012;21(11):1593–600. [DOI] [PubMed] [Google Scholar]
- 37.Bey MJ, Brock SK, Beierwaltes WN, Zauel R, Kolowich PA, Lock TR. In vivo measurement of subacromial space width during shoulder elevation: technique and preliminary results in patients following unilateral rotator cuff repair. Clin Biomech (Bristol, Avon) 2007;22(7):767–73. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Paralyzed Veterans of America Consortium for Spinal Cord Medicine. Preserving upper limb function in spinal cord injury: a clinical practice guideline for health-care professionals. J Spinal Cord Med 2005;28(5):434–70. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Inman VT, Abbott LC. Observations on the function of the shoulder joint. J Bone Joint Surg 1944;26(1):1–30. [Google Scholar]
- 40.Reyes ML, Gronley JK, Newsam CJ, Mulroy SJ, Perry J. Electromyographic analysis of shoulder muscles of men with low-level paraplegia during a weight relief raise. Arch Phys Med Rehabil 1995;76(5):433–9. [DOI] [PubMed] [Google Scholar]
- 41.Finley MA, Lee RY. Effect of sitting posture on 3-dimensional scapular kinematics measured by skin-mounted electromagnetic tracking sensors. Arch Phys Med Rehabil 2003;84(4):563–8. [DOI] [PubMed] [Google Scholar]
- 42.Azzoni R, Cabitza P. Sonographic versus radiographic measurement of the subacromial space width. Chir Organi Mov 2004;89(2):143–50. [PubMed] [Google Scholar]
- 43.Saupe N, Pfirrmann CWA, Schmid MR, Jost B, Werner CML, Zanetti M. Association between rotator cuff abnormalities and reduced acromiohumeral distance. AJR Am J Roentgenol 2006;187(2):376–82. [DOI] [PubMed] [Google Scholar]