Abstract
Alcohol dependence (AD) and aggression-impulsivity are both associated with increased suicide risk. There is a need to evaluate clinical tools in order to improve suicide risk assessment of AD patients. The present study consisted of 95 individuals with a diagnosis of AD, consecutively admitted for addiction treatment, compared with 95 healthy controls. Suicidal risk was assessed together with exposure of violence and impulsivity. AD patients reported significantly higher rates of exposure to violence in childhood, as measured by the Karolinska Interpersonal Violence Scale (KIVS), compared to HC. Within the AD group, individuals with history of suicidal ideation and suicidal behavior reported higher levels of violence experience compared to AD individuals without such history. AD patients with previous suicidal ideation scored higher on self-reported impulsivity as assessed by the Barratt Impulsivity Scale (BIS). Our main finding was that experience of trauma and expression of violent behavior, coupled with increased impulsivity are associated with an elevated suicide risk in AD patients. Future longitudinal studies assessing these traits are needed to evaluate their potential role in identifying AD patients at risk of future suicide.
Alcohol dependence (AD) is associated with increased risk of suicide, and this has been demonstrated in several lines of research, including post-mortem studies of suicide cases1,2,3,4 and larger cohort studies5,6. The lifetime risk of suicide in AD patients has been estimated to 7%6, and co-morbid substance use disorder increases the absolute risk of suicide in all mental disorders7. Compared to the general population, individuals with a diagnosis of AD are almost 10 times more likely to die by suicide and those with drug dependence are 14 times more likely to commit suicide8. Suicidal behavior in AD patients has been associated with several risk factors such as severity of disease9,10, family history of AD10,11, family history of suicide attempts9,12, earlier onset of alcohol-related problems10,11 and psychiatric co-morbidity9,10,11,12,13. Although addiction treatment programs are sometimes reluctant to accept patients with recent suicidal behavior, up to 40% of patients seeking treatment for substance dependence report a history of suicide attempts12,14. Thus, suicidal behavior is a significant clinical problem among individuals in addiction treatment and it is important to identify risk factors and develop feasible clinical tools to characterize the AD patients at an elevated risk of future suicide.
The clinical assessment and categorization of suicide-related behaviors are inherently difficult and have been inconsistent across different clinical settings. The Columbia-Suicide Severity Rating Scale (C-SSRS) was developed to address previous inconsistencies, and comprises a clear distinction between suicidal ideation and suicidal behavior respectively15. The FDA recommends using the C-SSRS in clinical trials16, and suicide risk in the present study was operationalized as history of suicidal ideation and suicidal behavior, as assessed by this rating scale.
It is well known that exposure to violence in childhood17 and aggressive behaviors are known risk factors for suicidal behavior18,19. Also, higher level of aggression is associated with non-fatal suicide attempts20 and completed suicide21,22. Previous studies in AD individuals have shown that personality traits such as behavioral disinhibition and aggression are linked to suicidal behavior23,24. Conner et al. (2001) have found that violent behavior in the last year increases the risk of completed suicide in individuals with and without history of alcohol abuse. In a recent study, our co-author (JJ) and colleagues constructed and validated a brief 4-item rating instrument that quantifies exposure to, and expression of, violent acts in childhood and adult life, called the Karolinska Interpersonal Violence Scale (KIVS)25. In a prospective study of 161 recent suicide attempters, KIVS score predicted completed suicide at 4-year follow-up25. To our knowledge, the association between experience of violence measured by the KIVS and suicide risk has previously not been evaluated in treatment seeking AD patients.
Impulsivity, i.e. acting without foresight or an inability to inhibit prepotent responses26, is a personality trait proposed to mediate suicidal behavior. In suicide research, impulsive and aggressive behavior are often combined to one construct entitled “Aggression-Impulsivity”, and is strongly associated with suicidal behavior18,21,22,27. It is well established that AD patients have increased levels of impulsivity compared to healthy controls28,29, but only a few previous clinical studies have investigated the association between impulsivity and suicide risk in this patient population. In a theoretical model proposed by Conner and Duberstein30, aggression-impulsivity has been suggested as a key predisposing factor for suicide in AD patients. Wojnar et al.31 found that performance on a response inhibition task distinguished AD patients with a history of impulsive suicide attempt from those with a non-impulsive suicide attempt. Furthermore, AD patients with previous suicidal behavior scored higher on self-rated trait impulsivity31,32. In the current study we investigated whether impulsivity measured by the widely used Barratt Impulsivity Scale (BIS) is associated with different levels of suicide risk in AD patients.
Addiction treatment facilities may fail to identify patients at an elevated risk of suicide since the treatments primarily focus on substance use. In addition, commonly used suicide risk assessments such as the SAD PERSONS scale33 are aimed at capturing more traditional risk factors (e.g. previous suicide attempt) and do not include items regarding either violence experience or impulsivity. It is thus possible that clinical assessment of violence experience and impulsivity may be critical to identify a subgroup of AD patients at high risk of suicide. In the present study we therefore investigated the association between self-rated impulsivity, experience of violence and suicide risk in AD patients in an outpatient addiction treatment facility.
Methods
Participants
Ninety-five AD patients were recruited consecutively through public advertising and invited to the out patient treatment research clinic at the Stockholm Centre for Dependency Disorders to enroll in treatment studies. Participating AD patients provided informed consent and were explicitly informed that all data they provided would be summarized on group level and considered confidential. All patients underwent physical examination, performed a breathalyzer and urine dip test and were interviewed using the Structured Clinical Interview for DSM IV axis I disorders34 and Time-Line Follow-Back interview35 to assess drinking during the last 90 days. Heredity for AD and suicide in first or second-degree relatives were based on self-report. Inclusion criteria were: Male or female age 18–65, minimum nine years of education and currently fulfilling DSM-IV criteria for AD. Exclusion criteria were: Fulfills DSM-IV criteria for schizophrenia, bipolar disorder, major depression or any other substance dependence (excluding nicotine), previous withdrawal-induced delirium tremens or seizures, current severe somatic illness e.g. liver cirrhosis, use of any narcotics the last 30 days, positive urine dip test for any narcotic substance or positive breathalyzer on day of study participation.
Ninety-five healthy controls (HC) were recruited as part of a study at the Suicide Prevention Clinic at the Karolinska University Hospital, and data from these subjects have been reported previously25. All HC’s provided informed consent and were screened by a psychiatrist to exclude any current and past mental disorder, including suicidal behavior. The studies comprising the AD and HC populations were approved by the regional ethical review board in Stockholm, and conducted in accordance with the Declaration of Helsinki and Good Clinical Practice.
Columbia-Suicide Severity Rating Scale (C-SSRS)
The C-SSRS is a semi-structured interview that evaluates suicidal ideation and suicidal behavior, respectively15,36. It consists of four constructs evaluating current and lifetime history of: (1) Severity of suicidal ideation rated on a 5-point ordinal scale where 1 = “wish to be dead”, 2 = “nonspecific active suicidal thoughts”, 3 = “suicidal thoughts with methods”, 4 = “suicidal intent”, and 5 = “suicidal intent with plan”; (2) Intensity of suicidal ideation comprised of 5 items: frequency, duration, controllability, deterrents and reasons for ideation. All items were rated on a 5-point scale where higher points indicates greater intensity; (3) Suicidal behavior rated categorically yes/no for actual attempt; aborted attempt; interrupted attempt; preparatory behavior (e.g. writing suicide letter) in contrast to non-suicidal self-injury behavior; (4) Lethality of actual suicide attempts. All C-SSRS interviews were performed by an M.D., and we report lifetime history of suicidal ideation severity and suicidal behavior.
The Karolinska Interpersonal Violence Scale (KIVS)
The KIVS25 consists of 4 subscales assessing exposure to violence and expressed violent behavior in childhood (6–14 years old) and adulthood (15 years or older). Each item is scored from 0–5 where greater score indicates more severe experiences of violence. In the HC, the assessment was done as a semi-structured interview by trained clinicians. The AD patients completed the ratings through self-report. See Table 1 for the complete KIVS items and scoring. The KIVS has previously been shown to have high inter-rater reliability as well as validity25 and has been used in several suicide research studies37,38.
Table 1. The Karolinska Interpersonal Violence Scale (KIVS). Copyright 2010, Jussi Jokinen MD, PhD.
| The Karolinska Interpersonal Violence Scale |
| The steps of this scale are defined by short statements about violent behavior. Based on an interview with the subject; use the highest score where one or more of the statements apply. |
| A. Used violence. |
| As a child (6–14 years) |
| 0 No violence. |
| 1 Occasional fights, but no cause for alarm among grown-ups in school or in the family. |
| 2 Fighter. Been in fights a lot. |
| 3 Often started fights. Hit a comrade who had been bullied. Continued hitting when the other had surrendered. |
| 4 Initiated bullying. Often hit other children, with fist or object. |
| 5 Caused serious physical injury. Violent toward adult(s). Violent behavior that led to intervention by social welfare authorities. |
| As an adult (15 years or older) |
| 0 No violence. |
| 1 Slapped or spanked children on occasion. Shoved or shook partner or another adult. |
| 2 Occasionally smacked partner or child. Fought when drunk. |
| 3 Assaulted partner drunk or sober. Repeated corporal punishment of child. Frequent fighting when drunk. Hit someone when sober. |
| 4 Instance of violent sexual abuse. Repeated battering/physical abuse of child or partner. Assaulted/attacked other persons frequently, drunk or sober. |
| 5 Killed or caused severe bodily harm. Repeated instances of violent sexual abuse. Convicted of crime of violence. |
| B. Victim of violence. |
| Childhood (6 – 14 years) |
| 0 No violence. |
| 1 Occasional slaps. Fights in school, of no great significance. |
| 2 Bullied occasionally for short period(s). Occasionally exposed to corporal punishment. |
| 3 Often bullied. Frequently exposed to corporal punishment. Beaten by drunken parent. |
| 4 Bullied throughout childhood. Battered/beaten up by schoolmates. Regularly beaten by parent or another adult. Beaten with objects. Sexually abused. |
| 5 Repeated exposure to violence at home or in school that resulted at least once in serious bodily harm. Repeated sexual abuse, or sexual abuse that resulted in bodily harm. |
| Adulthood (15 years or older) |
| 0 No violence. |
| 1 Threatened or subjected to a low level of violence on at least one occasion. |
| 2 Beaten by partner on occasion. Victim of purse snatching. Threatened with object. |
| 3 Threatened with a weapon. Robbed. Beaten by someone other than partner. Frequently beaten by partner. |
| 4 Raped. Battered. |
| 5 Repeatedly raped. Repeatedly battered. Severely battered, resulting in serious bodily harm. |
Barratt Impulsivity Scale (BIS)
The Barratt Impulsivity Scale (BIS) was designed to measure the personality construct of impulsivity and is currently in it’s 11th revised form39. It consists of 30 self-report-items (e.g. “I say things without thinking”) each rated using a 4-point ordinal scale where 1 = “Rarely/never”, 2 = “Occasionally”, 3 = “Often” and 4 = “Almost always/always”. Outcomes reported in this study are the total BIS score, as well as the three subscales of attentional impulsivity, motor impulsivity and non-planning impulsivity. The English version of the BIS was translated to Swedish and back-translated by an authorized bilingual translator.
Statistical Analysis
Outcomes are reported using the mean, median, standard deviation and range. The assumption of normality was evaluated using the Shapiro-Wilks test. Between-group comparisons were done using two-tailed students t-test and Fischer’s exact test for continuous and categorical variables, respectively. If data were not normally distributed non-parametric tests were used.
We performed step-wise comparisons of KIVS and BIS (total score and all the subscales) between the following groups: (1) AD patients and HC; (2) AD patients with and without previous suicidal ideation; (3) AD patients with and without previous suicidal behavior; (4) AD patients with and without previous suicide attempt. In order to investigate potential confounding factors, these subgroups of AD patients were also compared regarding clinical characteristics (sex, age) as well as known risk factors for suicidal behavior in AD patients (previous depression, alcohol consumption, dependence severity, heredity for AD and heredity for suicide). Since the KIVS scores were positively skewed, all comparisons between groups were performed using the non-parametric Mann-Whitney U test. The BIS however was normally distributed, and students t-tests were performed to compare groups. Spearman correlation coefficients were calculated to assess correlations between KIVS subscales, as well as KIVS and BIS score. Statistical analyses were performed using SPSS version 21. No missing data was imputed, and analyses include only those subjects who completed all items on each questionnaire or subscale. The alpha level was set to 0.05, uncorrected, two-tailed.
Results
Participants
The AD patients had a mean age of 47 years (SD = 7.3; range 24–58) and 43% (n = 41) were female. The average number of fulfilled DSM IV criteria for AD was 5.2 (SD = 1.2; range 3–7) and 19% (n = 18) had a previous episode of major depressive disorder. In the AD group, 39% (n = 37) and 9.5% (n = 9) had a history of previous suicidal ideation and suicidal behavior, respectively. Among the 9 subjects with previous suicidal behavior, 4 had made previous suicide attempts while the other 5 had a history of aborted attempt and/or preparatory suicidal behavior. In the AD group, 2 subjects did not complete the C-SSRS and they were thus only included in analysis comparing HC and AD regarding KIVS score. In the HC the mean age was 40.2 years (SD = 11; range 18–63) and 60% were female (n = 57). The HC group was younger than the AD group (t(187) = −5.1; p < 0.001) and had more females (p = 0.030). Table 2 provides a summary of experience of violence and impulsivity measures across different levels of suicide risk.
Table 2. Demographics of alcohol dependent patients (N = 95) and healthy controls (N = 95).
| Alcohol Dependence (N = 95) | Alcohol Dependence with previous suicidal ideation (N = 37) | Alcohol Dependence with previous suicidal behavior (N = 9) | Alcohol Dependence with previous suicide attempt (N = 4) | Healthy Controls (N = 95) | |
|---|---|---|---|---|---|
| KIVS | |||||
| Experience of violence (KIVS total score) | 3.4 (2.5) | 4.4(2.7) | 6.0(2.6) | 6.8(3.8) | 2.9 (3.0) |
| Expressed violent behavior during childhood | 0.60(0.72) | 0.84(0.87) | 0.67(0.50) | 1.0(0.0) | 0.59(0.77) |
| Expressed violent behavior as adult | 0.52(0.76) | 0.70(0.85) | 1.2(1.1) | 1.5(1.3) | 0.43(0.74) |
| Exposure to violence during childhood | 1.2(1.1) | 1.5(1.1) | 2.4(1.7) | 2.5(2.1) | 0.93(1.2) |
| Exposure to violence as adult | 1.1(1.3) | 1.4(1.4) | 1.7(1.5) | 1.8(2.2) | 0.98(1.4) |
| BIS | |||||
| Impulsivity (BIS total score) | 62.3(10.7) | 66.1(11.6) | 61.1(10.6) | 54.5(7.5) | * |
| Attentional Impulsivity | 15.1(3.5) | 15.8(3.3) | 14.1(2.0) | 13.3(1.7) | * |
| Motor Impulsivity | 21.8(3.8) | 22.8(4.4) | 22.1(5.0) | 19.0(2.2) | * |
| Non-planning Impulsivity | 25.4(5.6) | 27.0(6.3) | 24.9(4.8) | 22.3(4.9) | * |
Experience of violence was measured by the Karolinska Interpersonal Violence Scale (KIVS) and impulsivity was measured using the Barratt Impulsivity Scale (BIS). Values are presented as mean (standard deviations).
*Prevalence of previous suicidal ideation and BIS were not collected in healthy controls.
Experience of violence: Comparison of AD Patients and HC
Since the KIVS scores deviated from the normal assumption (all Shapiro-Wilks tests p < 0.001), comparisons were performed using non-parametric tests. There was a trend toward greater overall violence experience (KIVS total score) in the AD group (n = 95) compared to the HC (n = 95; Z = 1.9; p = 0.052). The rating of exposure to violence during childhood was significantly higher in the AD group (Z = 2.6; p = 0.009) while there were no significant differences regarding the other three subscales (all p > 0.1; Table 3). The different KIVS subscales of exposure to and expression of violence were all significantly correlated in the entire sample (Table 4). Within the AD group, males rated significantly higher regarding expression of violent behavior during childhood compared to females (Z = −3.7; p < 0.001). There were no gender differences in any of the other KIVS subscales (all p > 0.05). Within the HC group, there were no gender differences in any of the KIVS subscales (all p > 0.05).
Table 3. Karolinska Interpersonal Violence Scale (KIVS) ratings of experience of violence in alcohol dependent patients (n = 95) and healthy controls (n = 95).
| Rating | Alcohol Dependence |
Healthy Controls |
Statistic | ||||||
|---|---|---|---|---|---|---|---|---|---|
| Mean | Median | SD | Range | Mean | Median | SD | Range | ||
| Experience of violence (KIVS total score) | 3.41 | 3 | 2.52 | 0–14 | 2.92 | 2 | 2.96 | 0–17 | Z = 1.9 p = 0.052 |
| Expressed violent behavior during childhood (6–14 years old) | 0.60 | 1 | 0.72 | 0–5 | 0.58 | 0 | 0.77 | 0–4 | Z = 0.53 p = 0.60 |
| Expressed violent behavior as adult ( >15 years old) | 0.52 | 0 | 0.76 | 0–3 | 0.43 | 0 | 0.74 | 0–3 | Z = 1.0 p = 0.30 |
| Exposure to violence during childhood (6–14 years old) | 1.23 | 1 | 1.09 | 0–5 | 0.93 | 0 | 1.19 | 0–5 | Z = 2.6 p = 0.009 |
| Exposure to violence as adult (>15 years old) | 1.06 | 1 | 1.27 | 0–5 | 0.98 | 0 | 1.41 | 0–5 | Z = 1.2 p = 0.23 |
Table 4. Correlations between the different subscales of Karolinska Interpersonal Violence Scale (KIVS), measuring exposure to and expression of violent acts in childhood and adulthood, in the entire study sample (n = 190).
| Exposure to violence during childhood | Expressed violent behavior as adult | Exposure to violence as adult | Expressed violence total | |
|---|---|---|---|---|
| Expressed violent behavior during childhood | 0.237** | 0.286*** | 0.258*** | |
| Exposure to violence during childhood | 0.243** | 0.262*** | ||
| Exposure to violence total | 0.386*** |
*p < 0.05; **p < 0.01; ***p < 0.001.
Experience of violence: Comparison of AD patients with and without history of suicidal ideation
AD patients with a history of previous suicidal ideation (1 or more on the C-SSRS lifetime suicidal ideation construct; n = 37) reported significantly greater violence experience (Z = 3.6; p < 0.001; Fig. 1A) as well as all four subscales (all p < 0.05; Fig. 2) compared to AD patients without such history (n = 58). Within the AD group with previous suicidal ideation, there was a significant correlation between severity of suicidal ideation and KIVS total score (r = 0.40; p = 0.01). Among the subscales, there was a significant correlation between severity of suicidal ideation and expression of violence as adult (r = 0.33; p = 0.048), and no significant correlations for any of the three other subscales (all p > 0.1).
Figure 1. Karolinska Interpersonal Violence Scale (KIVS) ratings of experience of violence in alcohol dependent (AD) patients with increasing suicide risk as assessed by the Columbia-Suicide Severity Rating Scale (C-SSRS).
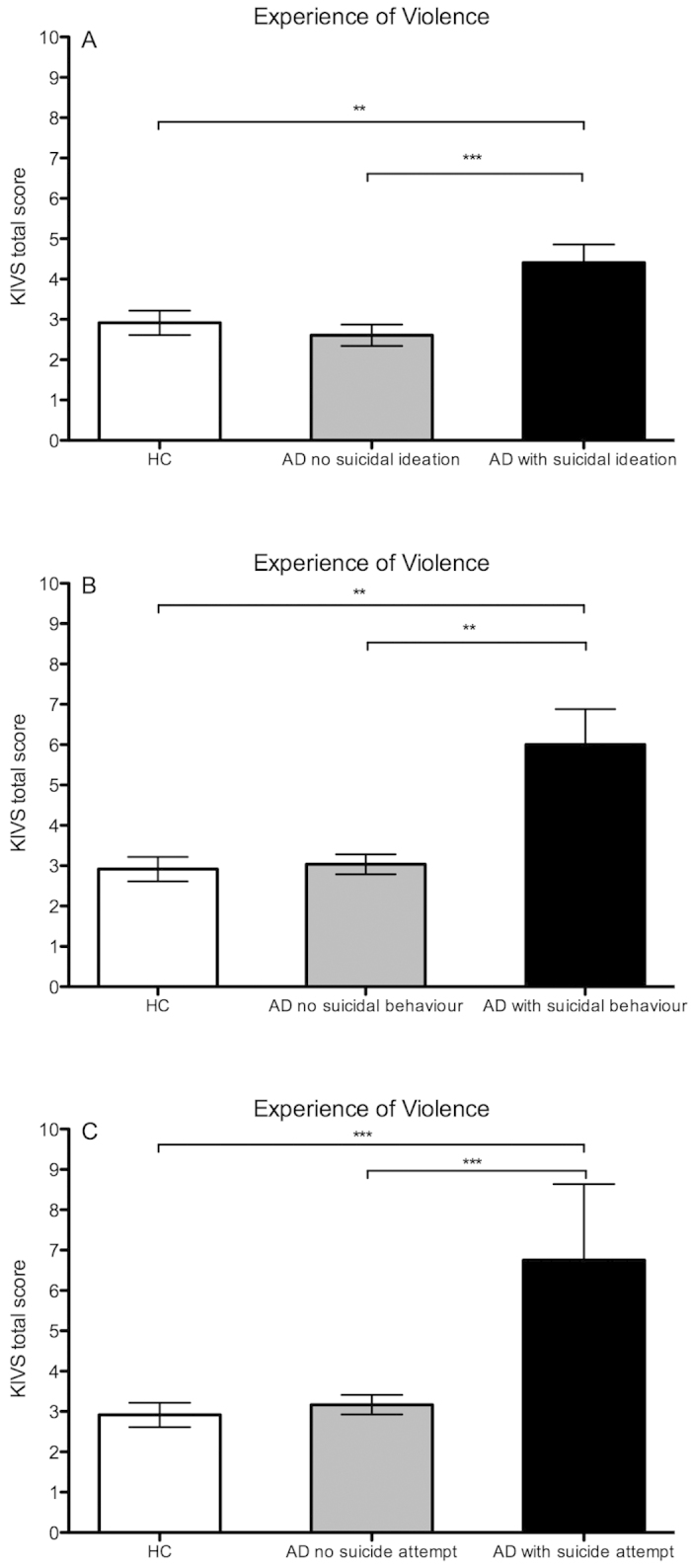
(A) HC (n = 95) versus AD patients without suicidal ideation (n = 58) versus AD patients with suicidal ideation (n = 37); (B) HC versus AD patients without suicidal behavior (n = 86) versus AD patients with suicidal behavior (n = 9); (C) HC versus AD patients without suicide attempt (n = 91) versus AD patients with suicide attempt (n = 4). *p < 0.05; **p < 0.01; ***p < 0.001.
Figure 2.
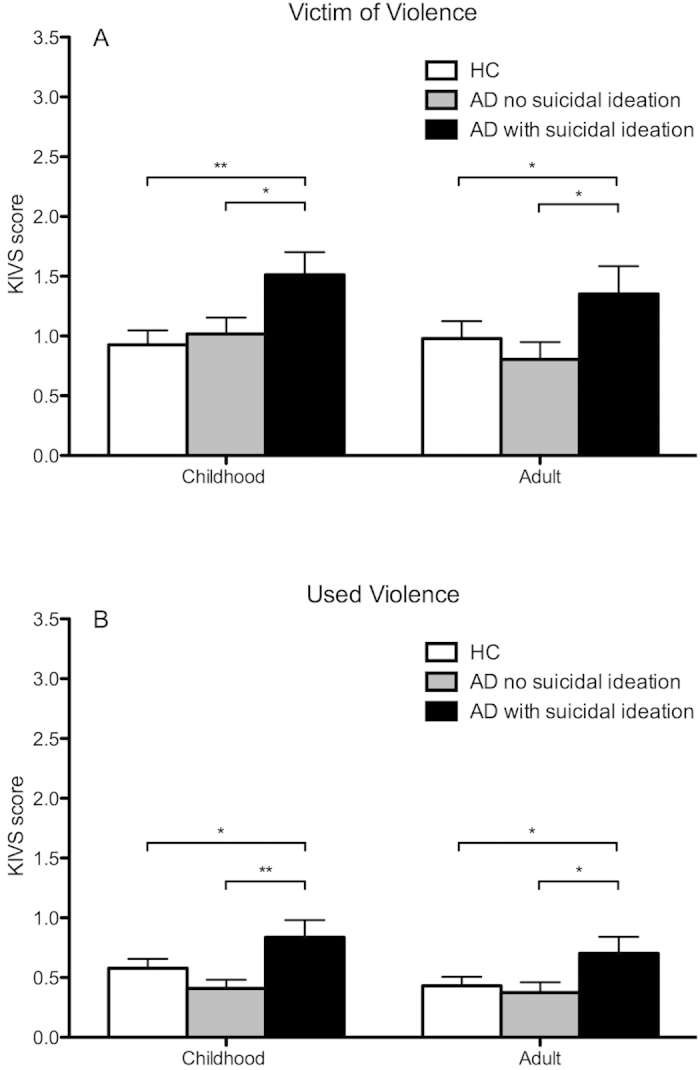
Karolinska Interpersonal Violence Scale (KIVS) subscale scores measuring exposure to (A) and expression of (B) violent acts in childhood and adulthood respectively, in alcohol dependent patients (AD) with (n = 37) and without (n = 58) history of suicidal ideation and healthy controls (HC; n = 95). *p < 0.05; **p < 0.01; ***p < 0.001.
There was no difference in overall violence experience between HC and AD patients without previous suicidal ideation (Z = −0.05; p = 0.96), while AD patients with previous suicidal ideation scored significantly higher than HC on total KIVS score (Fig. 1A) as well as all the subscales (Fig. 2).
There was no statistically significant difference between AD patients with and without history of suicidal ideation regarding number of drinks consumed the last 90 days (t(88) = 0.63; p = 0.53), age (t(90) = 1.0; p = 0.32), sex (p = 0.67) heredity for AD (p = 0.17) or heredity for suicide (p = 0.75). The AD patients with previous suicidal ideation fulfilled more DSM-IV AD criteria (mean 5.5 vs 5.0;t(88) = −2.1; p = 0.038) and had to a higher degree a previous depressive episode (35% vs 9%; p = 0.030) compared with those without previous suicidal ideation.
Experience of violence: Comparison of AD patients with and without history of suicidal behavior
AD patients with a history of suicidal behavior (n = 9; responding yes to any item on the C-SSRS suicidal behavior construct excluding non-suicidal self-injury) reported significantly greater overall violence experience (Z = 3.4; p < 0.001; Fig. 1B), including subscales of expressed violence as adult (Z = 2.5; p = 0.014; Fig. 3B) and exposure to violence in childhood (Z = 2.7; p = 0.006; Fig. 3A), compared to AD patients without such history (n = 86).
Figure 3.
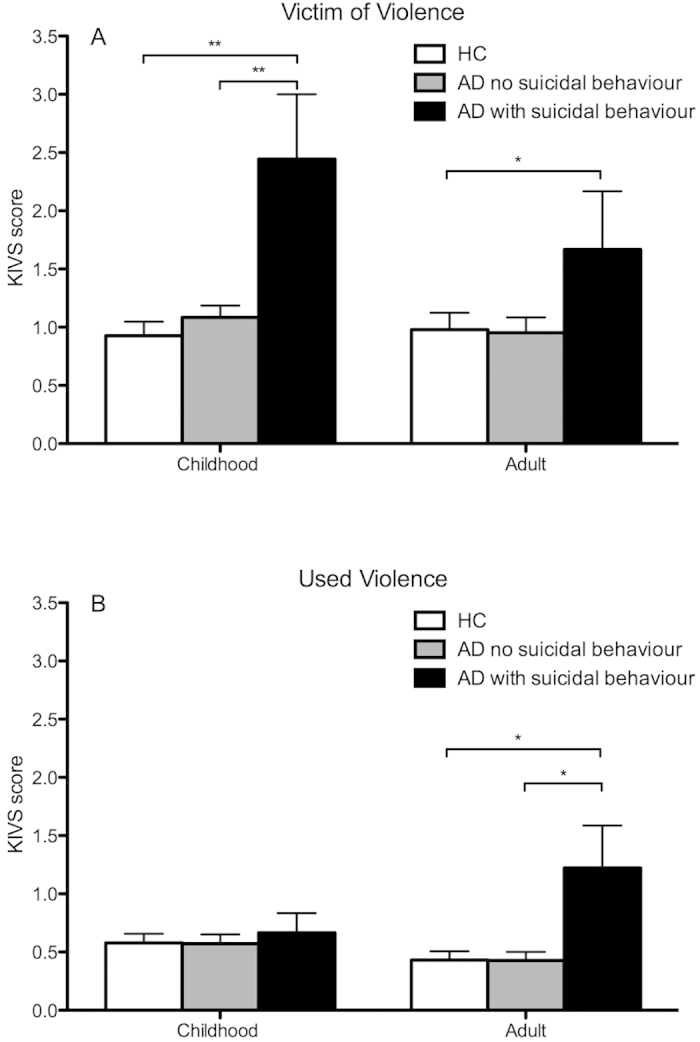
Karolinska Interpersonal Violence Scale (KIVS) subscale scores measuring exposure to (A) and expression of (B) violent acts in childhood and adulthood respectively, in alcohol dependent patients (AD) with (n = 9) and without (n = 86) history of suicidal behavior and healthy controls (HC). *p < 0.05; **p < 0.01; ***p < 0.001.
There was no difference in overall violence experience between HC and AD patients without previous suicidal behavior (Z = −1.1; p = 0.27), while the AD patients with previous suicidal behavior scored significantly higher than HC regarding overall violence experience (Fig. 1B), including all the subscales except using violence in childhood (Fig. 3).
There was no statistically significant difference between AD patients with and without history of suicidal behavior regarding number of DSM-IV AD criteria (t(88) = 0.41; p = 0.69), drinks consumed the last 90 days (t(88) = 0.67; p = 0.50, age (t(90) = 0.23; p = 0.82), sex (p = 1.0), heredity for AD (p = 1.0) or heredity for suicide (p = 1.0). The AD patients with previous suicidal behavior had to a higher degree a previous depressive episode (44% vs 17%; p = 0.072) compared to those without previous suicidal behavior.
Experience of violence: Comparison of AD patients with and without history of suicide attempt
Only four patients had a history of previous suicide attempt, and this group reported significantly greater overall violence experience compared to AD patients without any previous suicide attempt (Z = 2.3; p = 0.021) as well as the HC group (Z = 2.3; p = 0.019; Fig. 1C). No statistically significant difference in any of the subscales was observed (data not shown; p > 0.1 for all subscales).
Violence Experience: Sensitivity Analyses
Since the HC were significantly younger and to a higher degree female, compared to AD patients, the following sensitivity analysis was performed: The youngest females in the HC group (n = 15) and the oldest males in the AD group (n = 15) were removed from analysis. After removal of these subjects, there was no significant difference between the remaining AD and HC regarding age (HC: 43.5; AD: 45.7; t(156) = −1.7; p = 0.085) or sex (p = 0.94). Analysis of KIVS score yielded similar results as the original analysis. The AD patients scored significantly higher on KIVS total score (Z = 2.0; p = 0.046) and on the rating of exposure to violence during childhood (Z = 2.9; p = 0.004) while no significant difference was found for the other three subscales (all p > 0.1).
Since history of depressive episodes was more frequent in subjects with previous suicidal ideation and behavior, an additional sensitivity analysis was done. After excluding all subjects with history of major depression, the remaining subjects with history of suicidal ideation (Z = 3.1; p = 0.001) as well as behavior (Z = 2.4; p = 0.014) reported significantly greater overall violence experience compared to subjects without such history.
Since all AD patients with previous suicidal behavior also scored positive regarding previous suicidal ideation, an additional analysis was done to investigate whether these subjects alone drove the observed association. All AD patients were subdivided into the following three groups based on their most severe level of suicidality: 1) No previous suicidal ideation or behavior (n = 56; KIVS total score = 2.6); 2) Previous suicidal ideation but no suicidal behavior (n = 28; KIVS total score = 3.9) and 3) Previous suicidal ideation and previous suicidal behavior (n = 9; KIVS total score = 6.0). In line with the original analysis, both group 3(p < 0.001) and group 2(p = 0.014) reported significantly greater violence experience compared to both group 1.
Impulsivity and suicide risk in AD patients
A subset of AD patients completed the Barratt Impulsivity Scale (BIS). AD patients with a history of suicidal ideation (n = 28) reported significantly higher overall impulsivity (BIS total score; mean: 66.1 vs 59.9; t(73) = 2.5; p = 0.014) compared to AD patients without such history (n = 47). Among the BIS subscales, the AD patients with previous suicidal ideation scored significantly higher on non-planning impulsivity (mean 27.0 vs 24.3; t(75) = 2.0; p = 0.046) and a trend was observed for motor impulsivity (22.8 vs 21.2; t(74) = 1.8; p = 0.071), but no difference in attentional impulsivity (mean 15.8 vs 14.6; t(76) = 1.4; p = 0.16). However, when comparing AD patients with (n = 8) and without previous suicidal behavior (n = 67) we found no significant difference regarding overall impulsivity (mean 61.1 vs 62.3; t(73) = −0.29; p = 0.77) or any of the subscales measuring non-planning (mean 24.9 vs 25.4; t(75) = −0.25; p = 0.80), motor (mean 22.1 vs 21.8; t(74) = 0.23; p = 0.82) and attentional impulsivity (mean 14.1 vs 15.2; t(76) = −0.82; p = 0.41). No difference was found between AD patients with (n = 4) and without (n = 71) previous suicide attempt (data not shown; All p > 0.1 for total BIS score and all subscales).
There were no statistically significant correlations between BIS and KIVS total score, nor the different KIVS subscales measuring exposure to and expression of violence (data not shown; All p > 0.1).
Discussion
The main finding of the present study was that AD patients with a history of suicidal ideation and suicidal behavior, report increased levels of experience of violence. We also found that suicidal ideation, but not behavior, was associated with self-rated impulsivity. Collectively our findings indicate that trauma, traits of aggression and impulsivity might be critical factors contributing to the pathogenesis of suicidal behavior in the AD population.
Our findings are corroborated by several previous studies that have shown an association between both violence/aggression and suicide in general among individuals with mental disorders18,20,21,22,27, and specifically in AD patients30,40. In the study by Jokinen et al.25 it was shown that experience of violence as measured by the KIVS, specifically the subscales of victimization of violence in childhood and expression of violence in adulthood, predicted completed suicide in suicide attempters. In the present study AD patients with highest suicide risk, i.e. previous suicidal behavior, scored significantly higher, specifically on the same subscales that have previously been shown to predict completed suicide25. In addition, our results indicate that an overall experience of violence was increased in AD patients with incremental levels of suicide risk. Furthermore, the correlation between suicidal ideation severity and overall violence experience was statistically significant. Taken together these findings indicate that there may be a dose-response relationship between experience of violence and suicide risk in AD patients. The finding collectively provides valuable clinical evidence that in AD patients receiving outpatient addiction care, it is possible to identify individuals at an elevated risk of suicide related behaviors by utilizing the KIVS. It is known that suicide completers do not always communicate their suicidal thoughts and sometimes have no previous suicidal behavior41. It is thus possible that a clinical tool assessing violence experience is able to more accurately identify patients at an elevated risk of suicide who otherwise could be considered as “low-risk” based on traditional suicide risk assessments.
Exposure to violence during childhood was not only elevated in AD patients with increased suicide risk, but it was also the only subscale that differentiated AD patients from HC. It is known that childhood maltreatment, such as physical, emotional and sexual abuse, increases the risk of developing AD42,43. One possible interpretation of our result is that childhood trauma increases risk of developing AD later in life, and that AD itself could act as an independent risk factor for suicide. However, experience of childhood adversities is a known independent risk factor mediating all forms of psychopathology42 as well as suicide attempts44. Furthermore, in a study of 196 AD patients Huang et al.45 found that childhood trauma increased risk of both psychiatric disorders as well as suicide attempts. Thus, it is more likely that experience of childhood trauma acts as a multiple risk factor increasing the risk of AD, other mental disorders as well as suicidal behavior. This illustrates the importance of assessing trauma during childhood, when performing clinical suicide risk assessments in AD patients, and our study suggests that the KIVS is a feasible clinical tool for this purpose.
The neurobiological correlate of our finding is not known, but there is a vast amount of literature indicating an association between serotonergic neurotransmission and both violence and suicide46,47. Recently it was shown that the KIVS subscale measuring experience of violence in childhood was associated with low levels of the serotonin metabolite 5-hydroxyindoleacetic acid (5-HIAA) in cerebrospinal fluid (CSF) in female suicide attempters48. Furthermore, emotional neglect was found to be associated with reduced central serotonergic neurotransmission as measured by a neuroendocrine challenge test in male AD patients49. It is possible that the underlying neurobiological correlate of the association between suicide risk and exposure to childhood trauma observed in the current study is also related to changes in serotonergic neurotransmission. Future studies combining clinical suicide risk assessments with biological samples are needed to investigate to understand the possible pathophysiological mechanism common to AD and suicide.
In the present study, we found significantly elevated levels of self-rated impulsivity in AD patients with previous suicidal ideation, but not in those with previous suicidal behavior or suicide attempt. There are several plausible explanations for this discrepancy. First of all, the variance in self-rated impulsivity was large (range 44–89; mean 62 ± 11) and our limited sample of individuals with suicidal behavior was likely insufficient to detect a difference. Secondly, self-rated impulsivity as a construct may be too heterogeneous to be specific for suicidal behavior. This is substantiated by recent findings that demonstrated that a behavioral measure of impulsivity compared to the self-rated measure more accurately distinguished AD patients with impulsive suicide attempts from those without31. We did not find any correlation between KIVS total score or any of the subscales and self-rated impulsivity, suggesting that these two constructs are separate and could possibly constitute two independent factors important in suicide risk assessment in AD patients.
In order to rule out potential confounding factors that could otherwise explain our findings, we compared clinical characteristics of AD patients with different levels of suicide risk. We found no significant difference between AD patients on the different levels of suicide risk regarding gender, age, alcohol consumption over the last 90 days or heredity for AD and suicide respectively, indicating that these factors did not drive the observed association. However we found that AD patients with previous suicidal ideation fulfilled more DSM-IV AD criteria’s, indicating that the observed association between violence experience and suicide risk could be mediated by severity of diagnosis of AD. With respect to past psychiatric diagnosis, we found that AD patients with previous suicidal ideation and behavior were more likely to have had a past history of a depressive episode. Schwandt et al.50 showed that childhood trauma influenced severity of dependence in a clinical sample of 280 AD patients, and that this association was mediated through neuroticism. In a large retrospective cohort study of 17337 subjects Dube et al.44 found that childhood abuse increased risk of future suicide attempt, and this relationship was partially mediated through both self-reported AD and depression. Our results are in line with previous studies, suggesting that the association between violence experience and suicide risk in AD patients is in part mediated through dependence severity and depressive affect.
There are some important limitations in our study that need to be addressed. First of all, the study sample was of limited size and consisted of cross-sectional data. We emphasize that our findings should be interpreted with caution until replicated, given the limited number of subjects with actual suicidal behavior (n = 9) and suicide attempts (n = 4). Secondly, we did not clinically assess personality disorders in the AD sample. It is possible that e.g. antisocial personality disorder, which is associated with violence51, impulsivity26 and alcohol use disorders52, could confound some of the observed associations. However a recent study in AD patients with history of suicide attempts reported no association with personality disorders with impulsive features such as borderline personality disorder or anti social personality disorder32. Moreover in the current sample of AD patients there was no previous psychiatric diagnosis or treatment of any personality disorder, indicating that unmeasured personality disorders likely did not explain the observed association. Thirdly, the HC and AD group were not matched regarding sex and age. A sensitivity analysis was done which yielded almost identical results as the original analysis, indicating that the mismatched groups did not bias the results. Lastly, in the HC group the KIVS was administered as a semi-structured interview by a trained clinician, while the AD group completed the KIVS rating through self-report, which possibly could bias the result. However, in a study of substance use disorder patients there were convergent correlations between interview and self-report regarding different forms of childhood trauma53. This suggests that the discrepancy in method of administration of the KIVS should not constitute a major bias in the present study.
In summary, AD patients with increased suicide risk have more experience of violence compared to AD patients with low suicide risk as well as HC. Furthermore, previous suicidal ideation in AD patients was associated with increased self-rated impulsivity. Future studies employing a prospective design are needed to investigate whether clinical assessment of violence experience and impulsivity can predict attempted and completed suicide in AD patients and other substance use disorders.
Additional Information
How to cite this article: Khemiri, L. et al. Suicide Risk Associated with Experience of Violence and Impulsivity in Alcohol Dependent Patients. Sci. Rep. 6, 19373; doi: 10.1038/srep19373 (2016).
Acknowledgments
We thank Professor Johan Franck, Head of Stockholm Dependency Disorder Clinic for access to the patient population and for clinical expertise. We thank research nurses Margareta Gard-Hedander and Else-Britt Hillner, psychologist Angela Stünkel, undergraduate student Maria Östman and project coordinator Camilla Hellspong for excellent assistance in data collection. Funding was provided by the Swedish Research Council (Project numbers: K2009-61P-21304-04-4; K2009-61X-21305-01-1; JJ) and Söderström Königska foundation (SLS 388861; NJL), Swedish Research Council for Health, Working Life and Welfare (2012-0043 and 2013-0071; NJL) and Swedish Society of Medicine, project grant (SLS 409271; NJL).
Footnotes
Author Contributions All authors (L.K., J.J., B.R. and N.J.L.) contributed to the study design, data collection, data analysis and writing of the manuscript. All authors have approved the final manuscript version.
References
- Henriksson M. M. et al. Mental disorders and comorbidity in suicide. Am J Psychiatry 150, 935–940 (1993). [DOI] [PubMed] [Google Scholar]
- Cheng A. T. Mental illness and suicide. A case-control study in east Taiwan. Arch. Gen. Psychiatry 52, 594–603 (1995). [DOI] [PubMed] [Google Scholar]
- Cheng A. T., Chen T. H., Chen C. C. & Jenkins R. Psychosocial and psychiatric risk factors for suicide. Case-control psychological autopsy study. Br J Psychiatry 177, 360–365 (2000). [DOI] [PubMed] [Google Scholar]
- Foster T., Gillespie K., McClelland R. & Patterson C. Risk factors for suicide independent of DSM-III-R Axis I disorder. Case-control psychological autopsy study in Northern Ireland. Br J Psychiatry 175, 175–179 (1999). [DOI] [PubMed] [Google Scholar]
- Harris E. C. & Barraclough B. Suicide as an outcome for mental disorders. A meta-analysis. Br J Psychiatry 170, 205–228 (1997). [DOI] [PubMed] [Google Scholar]
- Inskip H. M., Harris E. C. & Barraclough B. Lifetime risk of suicide for affective disorder, alcoholism and schizophrenia. Br J Psychiatry 172, 35–37 (1998). [DOI] [PubMed] [Google Scholar]
- Nordentoft M., Mortensen P. B. & Pedersen C. B. Absolute risk of suicide after first hospital contact in mental disorder. Arch. Gen. Psychiatry 68, 1058–1064 (2011). [DOI] [PubMed] [Google Scholar]
- Wilcox H. C., Conner K. R. & Caine E. D. Association of alcohol and drug use disorders and completed suicide: an empirical review of cohort studies. Drug Alcohol Depend 76Suppl, S11–19 (2004). [DOI] [PubMed] [Google Scholar]
- Preuss U. W. et al. Comparison of 3190 alcohol-dependent individuals with and without suicide attempts. Alcohol. Clin. Exp. Res 26, 471–477 (2002). [PubMed] [Google Scholar]
- Roy A., Lamparski D., DeJong J., Moore V. & Linnoila M. Characteristics of alcoholics who attempt suicide. Am J Psychiatry 147, 761–765 (1990). [DOI] [PubMed] [Google Scholar]
- Hesselbrock M., Hesselbrock V., Syzmanski K. & Weidenman M. Suicide attempts and alcoholism. J. Stud. Alcohol 49, 436–442 (1988). [DOI] [PubMed] [Google Scholar]
- Roy A. & Janal M. N. Risk factors for suicide attempts among alcohol dependent patients. Arch Suicide Res 11, 211–217 (2007). [DOI] [PubMed] [Google Scholar]
- Whitters A. C., Cadoret R. J. & Widmer R. B. Factors associated with suicide attempts in alcohol abusers. J Affect Disord 9, 19–23 (1985). [DOI] [PubMed] [Google Scholar]
- Roy A. Characteristics of cocaine dependent patients who attempt suicide. Arch Suicide Res 13, 46–51 (2009). [DOI] [PubMed] [Google Scholar]
- Posner K. et al. The Columbia-Suicide Severity Rating Scale: initial validity and internal consistency findings from three multisite studies with adolescents and adults. Am J Psychiatry 168, 1266–1277 (2011). [DOI] [PMC free article] [PubMed] [Google Scholar]
- United States Food and Drug Administration, United States Department of Health and Human Services. Guidance for Industry: Suicidality: Prospective Assessment of Occurrence in Clinical Trials, Draft Guidance. (2012). Date of access 20151013, retrieved from < http://www.fda.gov/downloads/Drugs/Guidances/UCM225130.pdf>.
- Klomek A. B. et al. Childhood bullying behaviors as a risk for suicide attempts and completed suicides: a population-based birth cohort study. J Am Acad Child Adolesc Psychiatry 48, 254–261 (2009). [DOI] [PubMed] [Google Scholar]
- Mann J. J. et al. Candidate endophenotypes for genetic studies of suicidal behavior. Biol. Psychiatry 65, 556–563 (2009). [DOI] [PMC free article] [PubMed] [Google Scholar]
- Brent D. A. & Mann J. J. Familial pathways to suicidal behavior–understanding and preventing suicide among adolescents. N. Engl. J. Med. 355, 2719–2721 (2006). [DOI] [PubMed] [Google Scholar]
- Oquendo M. A. et al. Prospective study of clinical predictors of suicidal acts after a major depressive episode in patients with major depressive disorder or bipolar disorder. Am J Psychiatry 161, 1433–1441 (2004). [DOI] [PubMed] [Google Scholar]
- Dumais A. et al. Risk factors for suicide completion in major depression: a case-control study of impulsive and aggressive behaviors in men. Am J Psychiatry 162, 2116–2124 (2005). [DOI] [PubMed] [Google Scholar]
- McGirr A. et al. Impulsive-aggressive behaviours and completed suicide across the life cycle: a predisposition for younger age of suicide. Psychol Med 38, 407–417 (2008). [DOI] [PubMed] [Google Scholar]
- Bergman B. & Brismar B. Hormone levels and personality traits in abusive and suicidal male alcoholics. Alcohol. Clin. Exp. Res. 18, 311–316 (1994). [DOI] [PubMed] [Google Scholar]
- Suominen K., Isometsä E., Henriksson M., Ostamo A. & Lönnqvist J. Hopelessness, impulsiveness and intent among suicide attempters with major depression, alcohol dependence, or both. Acta Psychiatr Scand 96, 142–149 (1997). [DOI] [PubMed] [Google Scholar]
- Jokinen J. et al. Karolinska Interpersonal Violence Scale predicts suicide in suicide attempters. J Clin Psychiatry 71, 1025–1032 (2010). [DOI] [PubMed] [Google Scholar]
- Moeller F. G., Barratt E. S., Dougherty D. M., Schmitz J. M. & Swann A. C. Psychiatric aspects of impulsivity. Am J Psychiatry 158, 1783–1793 (2001). [DOI] [PubMed] [Google Scholar]
- Mann J. J., Waternaux C., Haas G. L. & Malone K. M. Toward a clinical model of suicidal behavior in psychiatric patients. Am J Psychiatry 156, 181–189 (1999). [DOI] [PubMed] [Google Scholar]
- Lejuez C. W. et al. Behavioral and biological indicators of impulsivity in the development of alcohol use, problems, and disorders. Alcohol. Clin. Exp. Res. 34, 1334–1345 (2010). [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dick D. M. et al. Understanding the construct of impulsivity and its relationship to alcohol use disorders. Addict Biol 15, 217–226 (2010). [DOI] [PMC free article] [PubMed] [Google Scholar]
- Conner K. R. & Duberstein P. R. Predisposing and precipitating factors for suicide among alcoholics: empirical review and conceptual integration. Alcohol. Clin. Exp. Res. 28, 6S–17S (2004). [DOI] [PubMed] [Google Scholar]
- Wojnar M. et al. Impulsive and non-impulsive suicide attempts in patients treated for alcohol dependence. J Affect Disord 115, 131–139 (2009). [DOI] [PMC free article] [PubMed] [Google Scholar]
- Koller G., Preuss U. W., Bottlender M., Wenzel K. & Soyka M. Impulsivity and aggression as predictors of suicide attempts in alcoholics. Eur Arch Psychiatry Clin Neurosci 252, 155–160 (2002). [DOI] [PubMed] [Google Scholar]
- Patterson W. M., Dohn H. H., Bird J. & Patterson G. A. Evaluation of suicidal patients: the SAD PERSONS scale. Psychosomatics 24, 343–345 348–349 (1983). [DOI] [PubMed] [Google Scholar]
- American Psychiatric Association. Diagnostic and statistical manual of mental disorders (4th ed., text rev.), Washington, DC: American Psychiatric Publishing (2000).
- Sobell L. & Sobell M. In Measuring Alcohol Consumption: Psychosocial and Biological Methods (eds. Litten R. & Allen J.) 41–72 (Humana Press, 1992). [Google Scholar]
- Mundt J. C. et al. Prediction of suicidal behavior in clinical research by lifetime suicidal ideation and behavior ascertained by the electronic Columbia-Suicide Severity Rating Scale. J Clin Psychiatry 74, 887–893 (2013). [DOI] [PubMed] [Google Scholar]
- Stefansson J., Nordström P., Runeson B., Åsberg M. & Jokinen J. Combining the Suicide Intent Scale and the Karolinska Interpersonal Violence Scale in suicide risk assessments. BMC Psychiatry 15, 226 (2015). [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rajalin M., Hirvikoski T. & Jokinen J. Family history of suicide and exposure to interpersonal violence in childhood predict suicide in male suicide attempters. J Affect Disord 148, 92–97 (2013). [DOI] [PubMed] [Google Scholar]
- Patton J. H., Stanford M. S. & Barratt E. S. Factor structure of the Barratt impulsiveness scale. J Clin Psychol 51, 768–774 (1995). [DOI] [PubMed] [Google Scholar]
- Conner K. R. et al. Violence, alcohol, and completed suicide: a case-control study. Am J Psychiatry 158, 1701–1705 (2001). [DOI] [PubMed] [Google Scholar]
- Runeson B. S., Beskow J. & Waern M. The suicidal process in suicides among young people. Acta Psychiatr Scand 93, 35–42 (1996). [DOI] [PubMed] [Google Scholar]
- Kessler R. C., Davis C. G. & Kendler K. S. Childhood adversity and adult psychiatric disorder in the US National Comorbidity Survey. Psychol Med 27, 1101–1119 (1997). [DOI] [PubMed] [Google Scholar]
- Fenton M. C. et al. Combined role of childhood maltreatment, family history, and gender in the risk for alcohol dependence. Psychol Med 43, 1045–1057 (2013). [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dube S. R. et al. Childhood abuse, household dysfunction, and the risk of attempted suicide throughout the life span: findings from the Adverse Childhood Experiences Study. JAMA 286, 3089–3096 (2001). [DOI] [PubMed] [Google Scholar]
- Huang M.-C., Schwandt M. L., Ramchandani V. A., George D. T. & Heilig M. Impact of multiple types of childhood trauma exposure on risk of psychiatric comorbidity among alcoholic inpatients. Alcohol. Clin. Exp. Res. 36, 1099–1107 (2012). [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bortolato M. et al. The role of the serotonergic system at the interface of aggression and suicide. Neuroscience 236, 160–185 (2013). [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mann J. J., Brent D. A. & Arango V. The neurobiology and genetics of suicide and attempted suicide: a focus on the serotonergic system. Neuropsychopharmacology 24, 467–477 (2001). [DOI] [PubMed] [Google Scholar]
- Moberg T. et al. CSF 5-HIAA and exposure to and expression of interpersonal violence in suicide attempters. J Affect Disord 132, 173–178 (2011). [DOI] [PubMed] [Google Scholar]
- Berglund K. J., Balldin J., Berggren U., Gerdner A. & Fahlke C. Childhood maltreatment affects the serotonergic system in male alcohol-dependent individuals. Alcohol. Clin. Exp. Res. 37, 757–762 (2013). [DOI] [PubMed] [Google Scholar]
- Schwandt M. L., Heilig M., Hommer D. W., George D. T. & Ramchandani V. A. Childhood trauma exposure and alcohol dependence severity in adulthood: mediation by emotional abuse severity and neuroticism. Alcohol. Clin. Exp. Res. 37, 984–992 (2013). [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fountoulakis K. N., Leucht S. & Kaprinis G. S. Personality disorders and violence. Curr Opin Psychiatry 21, 84–92 (2008). [DOI] [PubMed] [Google Scholar]
- Grant B. F. et al. Epidemiology of DSM-5 Alcohol Use Disorder: Results From the National Epidemiologic Survey on Alcohol and Related Conditions III. JAMA Psychiatry 72, 757–766 (2015). [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fink L. A., Bernstein D., Handelsman L., Foote J. & Lovejoy M. Initial reliability and validity of the childhood trauma interview: a new multidimensional measure of childhood interpersonal trauma. Am J Psychiatry 152, 1329–1335 (1995). [DOI] [PubMed] [Google Scholar]


