Abstract
AIM: To investigate the impact of minimum tacrolimus (TAC) on new-onset diabetes mellitus (NODM) after liver transplantation (LT).
METHODS: We retrospectively analyzed the data of 973 liver transplant recipients between March 1999 and September 2014 in West China Hospital Liver Transplantation Center. Following the exclusion of ineligible recipients, 528 recipients with a TAC-dominant regimen were included in our study. We calculated and determined the mean trough concentration of TAC (cTAC) in the year of diabetes diagnosis in NODM recipients or in the last year of the follow-up in non-NODM recipients. A cutoff of mean cTAC value for predicting NODM 6 mo after LT was identified using a receptor operating characteristic curve. TAC-related complications after LT was evaluated by χ2 test, and the overall and allograft survival was evaluated using the Kaplan-Meier method. Risk factors for NODM after LT were examined by univariate and multivariate Cox regression.
RESULTS: Of the 528 transplant recipients, 131 (24.8%) developed NODM after 6 mo after LT, and the cumulative incidence of NODM progressively increased. The mean cTAC of NODM group recipients was significantly higher than that of recipients in the non-NODM group (7.66 ± 3.41 ng/mL vs 4.47 ± 2.22 ng/mL, P < 0.05). Furthermore, NODM group recipients had lower 1-, 5-, 10-year overall survival rates (86.7%, 71.3%, and 61.1% vs 94.7%, 86.1%, and 83.7%, P < 0.05) and allograft survival rates (92.8%, 84.6%, and 75.7% vs 96.1%, 91%, and 86.1%, P < 0.05) than the others. The best cutoff of mean cTAC for predicting NODM was 5.89 ng/mL after 6 mo after LT. Multivariate analysis showed that old age at the time of LT (> 50 years), hypertension pre-LT, and high mean cTAC (≥ 5.89 ng/mL) after 6 mo after LT were independent risk factors for developing NODM. Concurrently, recipients with a low cTAC (< 5.89 ng/mL) were less likely to become obese (21.3% vs 30.2%, P < 0.05) or to develop dyslipidemia (27.5% vs 44.8%, P <0.05), chronic kidney dysfunction (14.6% vs 22.7%, P < 0.05), and moderate to severe infection (24.7% vs 33.1%, P < 0.05) after LT than recipients in the high mean cTAC group. However, the two groups showed no significant difference in the incidence of acute and chronic rejection, hypertension, cardiovascular events and new-onset malignancy.
CONCLUSION: A minimal TAC regimen can decrease the risk of long-term NODM after LT. Maintaining a cTAC value below 5.89 ng/mL after LT is safe and beneficial.
Keywords: Liver transplantation, Minimum tacrolimus, New-onset diabetes mellitus, Immunosuppressants, Allografts failure
Core tip: New-onset diabetes mellitus (NODM) is a common and severe metabolic complication that develops after liver transplantation. It is more prominent in recipients with tacrolimus (TAC)-dominant regimens. In this study, we found that the incidence of NODM is TAC concentration (cTAC)-dependent. Using a receiver operating characteristic curve, we identified that a cutoff cTAC of 5.89 ng/mL was predictive of NODM development after 6 mo after LT. And recipients exposed to low mean cTAC developed less other TAC related complications. The strategy of maintaining cTAC below 5.89 ng/mL after 6 mo after LT is therefore safe and beneficial.
INTRODUCTION
Liver transplantation (LT) has become a standard curative treatment for end-stage liver disease, and the 5-year survival rate of recipients has reached over 70%[1]. However, improved long-term survival is accompanied by increasingly prevalent post-operative metabolic complications[2]. Recent studies have shown that the prevalence of new-onset diabetes mellitus (NODM) after transplantation is approximately 16%-61%, depending on the medical center[3,4]. The development of post-LT NODM is associated with an increased risk of cardiovascular disease, rejection, infection, neuropsychiatric problem, allograft failure and even death[5,6]. Previous studies have found that old age, obesity, non-Caucasian ethnicity, family history of diabetes, hepatitis C virus infection and certain immunosuppressive agents are risk factors for the development of post-LT NODM in Western populations[7].
Tacrolimus (TAC), a calcineurin inhibitor, has become the most commonly used immunosuppressive agent worldwide over the past two decades[8]. Compared to cyclosporine, TAC effectively reduces acute rejection (AR) and increases allograft survival in liver recipients[8,9]. However, prolonged exposure to TAC leads to significant adverse events, including nephrotoxicity, neurotoxicity, and diabetogenic effects[10]. Some studies have suggested that higher trough concentrations of TAC (cTAC) after transplantation are associated with increased risk of complications[11-13], and many LT centers have recommended different minimal TAC regimens[14-16]. According to the current practice, target TAC level falls within the range of 10-15 ng/mL in the first month after transplantation, then is maintained at 5-10 ng/mL[17]. A prospective study has reported that reducing cTAC within the range of 5-8 ng/mL combined with mycophenolate mofetil (MMF) administration early did not increase the risk of rejection within 26 wk[18]. Jia et al[14] proposed that an early cTAC of 5-7 ng/mL would be safe and effective. A previous study performed in our center suggested that cTAC < 8 ng/mL after 1 mo and cTAC < 6 ng/mL after 3 mo are protective against chronic kidney disease (CKD) after LT[19]. However, all target cutoffs or ranges for cTAC are arbitrary, and there are no studies concerning the long-term maintenance of cTAC level after LT and its impact on NODM development. In this study, we aim to identify the risk factors for NODM and to determine the ideal long-term range of cTAC for preventing chronic complications.
MATERIALS AND METHODS
Patient population
We performed a retrospective study of 973 Chinese patients who received liver transplantation between March 1999 and September 2014 in the West China Hospital Liver Transplantation Center. All recipients were followed until June 2015 or until death or withdrawal. We excluded patients who had been diagnosed as diabetics before transplantation; those aged younger than 18 years old at transplantation; and those followed up for less than 6 mo, who died within 6 mo, and who received a cyclosporine-dominant regimen after liver transplantation. Finally, we collected demographic and clinical data of 528 recipients for this study. All liver grafts were voluntarily donated after cardiac death or by living donors. All donations were approved by the West China Hospital Ethics Committee and were in accordance with the ethical principles of the Declaration of Helsinki. Both the West China Hospital Liver Transplantation Center and the China Liver Transplant Registry approved and supported this study and its methods.
Definition of NODM and other clinical terms
NODM was defined as a composite endpoint consisting of the first occurrence of at least one of four parameters: two occurrences of a fasting plasma glucose level ≥ 7.0 mmol/L more than 30 d apart; oral hypoglycemic agent use for more than 30 consecutive days; insulin therapy for more than 30 consecutive days; or hemoglobin A1c ≥ 6.5%[20]. Arterial hypertension was defined as systolic blood pressure over 140 mmHg or diastolic pressure over 90 mmHg occurring twice at different time points[21]. Dyslipidemia was defined as total plasma cholesterol ≥ 6.22 mmol/L (i.e., hypercholesterolemia), triglyceride ≥ 2.26 mmol/L (i.e., hypertriglyceridemia) or high density lipoprotein cholesterol (HDL-C) < 1.04 mmol/L[21]. Chronic kidney disease (CKD) was defined as an estimated glomerular filtration rate (eGFR) < 60 mL/min per 1.73 m2 for at least 3 consecutive months[22]. AR was defined either by liver biopsy or recovery of liver function via high-dose methylprednisolone pulse therapy. If chronic rejection (CR) was suspected, liver biopsy was performed for confirmation. The Model for End-stage Liver Disease (MELD) score was calculated according to the United Network for Organ Sharing (UNOS) formula for each recipient before LT[23].
Immunosuppression protocol
The mode of initial immunosuppressive therapy was a triple-drug regimen after transplantation consisting of corticosteroids, TAC and MMF. Methylprednisolone was given intravenously at a 200 mg dose on the first day after transplantation, then gradually decreased daily and discontinued after one week. Alternative oral prednisone was also generally discontinued within 3 mo after transplantation. The initial dose of TAC was 0.05-0.10 mg/kg per day and was adjusted according to liver function and TAC trough concentration. MMF was individualized between 1.0 g/d and 1.5 g/d initially and was discontinued when severe side effects occurred and in long-term survivors with stable graft function after 6 mo after LT. Rapamycin was given as an alternative to MMF or an auxiliary for liver tumor at a dose of 1 mg/d.
Monitoring TAC trough concentrations and other clinical parameters
TAC trough concentrations were monitored daily during the first week following transplantation, weekly during the first month after LT, monthly within 3 mo and every 3-6 mo thereafter. The ideal serum trough level of TAC was 5-10 ng/mL during the first 3 mo after LT. Allograft function and cTAC were monitored closely while adjusting the TAC dose. If AR occurred, the prior dosage was reinstated, together with an increase in prednisone or the administration of high-dose methylprednisolone. After 6 mo post-LT, we reduced the TAC dosage very slowly and carefully while closely monitoring allograft function to maintain cTAC as low as possible. After transplantation, the recipients’ fasting plasma glucose level was monitored at 3, 6 and 12 mo, then annually thereafter according to international consensus guidelines[24]. A 2-h 75 g glucose tolerance test was performed in recipients with impaired fasting glucose. We also recorded the weight, blood pressure, serum lipid level, renal function, and chronic complications such as moderate to severe infections, cardio-cerebral vascular events, new-onset malignancy and allograft failures of each recipient at each visit after transplantation.
Statistical analysis
Quantitative descriptive data were expressed as the mean ± SD or median (minimum to maximum). Qualitative descriptive data were expressed as percentages. Univariate analysis using the χ2 and, when appropriate, Fisher’s exact test was performed for qualitative descriptive variables. Quantitative descriptive variables were analyzed by independent sample Student’s t test if the data were normally distributed or by the rank-sum test if the data were non-normally distributed. Survivor curves were analyzed using the Kaplan-Meier method and were compared using the log-rank test. The best cutoff mean cTAC after 6 mo was determined using a receiver operating characteristic (ROC) curve. Independent risk factors for NODM were identified by a stepwise forward Cox regression model. Candidate risk factors with a P value < 0.05 in univariate analysis were included in the multivariate analysis. Statistical analysis was performed using SPSS version 21.0 statistical software (SPSS Company, Chicago, IL, United States). P values of less than 0.05 were considered statistically significant. The statistical methods used in this study were reviewed by Ji-Zheng Qin from West China School of Public Health, Sichuan University.
RESULTS
Recipient and donor characteristics
A total of 973 recipients underwent LT between March 1999 and September 2014 in West China Hospital Liver Transplantation Center. Following the exclusion of ineligible recipients, 528 recipients were included in this study. The demographical and clinical records of recipients meeting the inclusion criteria were reviewed retrospectively. Recipients were followed up for a median of 46 mo (range, 6-173 mo). Recipients were 44.93 ± 9.41 years (range, 18-70 years) old and were predominantly male (87%). HBV (79.5%) was the most common etiology of liver disease; only six recipients had HCV (1.1%), and approximately half of the recipients (50.9%) had liver tumors. The pre-LT baseline included overweight/obesity (BMI ≥ 25) in 110 (20.8%) recipients, hypertension in 12 (2.3%) recipients, and dyslipidemia in 41 (8.2%) recipients. The median MELD score of all recipients was 13 (range, 6-40). MMF was administered in 322 (61%) recipients, and 129 (24.4%) recipients were also treated with Rapamycin. Donors were aged 34.01 ± 8.75 years (range, 5-65 years) old and were more likely to be male (84.5%). The living donor liver transplantation rate was 29.9%.
Prevalence of NODM and other post-LT complications
Eventually, 24.8% of the study population (131 cases) developed NODM during the follow-up period. The cumulative incidence of NODM increased progressively, and the 1-, 3-, 5- and 10-year incidence rates were 15.1%, 24.4%, 30.7% and 34.2%, respectively (Figure 1). We compared the 26 demographical and clinical parameters between recipients with and without NODM, as shown in Table 1. Common post-LT TAC-related complications included overweight/obesity (BMI ≥ 25) in 128 (24.2%) recipients, hypertension in 67 (12.7%) recipients, dyslipidemia in 175 (33.1%) recipients, and CKD in 91 (17.2%) recipients. There were 58 (11%) and 20 (3.8%) recipients with AR and CR, respectively. Predictably, we found that NODM recipients experienced more cardio-cerebral vascular events (7.6% vs 2.0%, P < 0.05), moderate to severe infections (36.7% vs 25.2%, P < 0.05), and allograft failures (15.3% vs 8.1%, P < 0.05) than non-NODM recipients. The 1-, 5-, and 10-year overall survival rates ( 86.7%, 71.3%, and 61.1% vs 94.7%, 86.1%, and 83.7%, P < 0.05) and allograft survival rates (92.8%, 84.6%, and 75.7% vs 96.1%, 91%, and 86.1%, P < 0.05) in the NODM group were significantly lower than in the non-NODM group, as shown in Figure 2.
Figure 1.
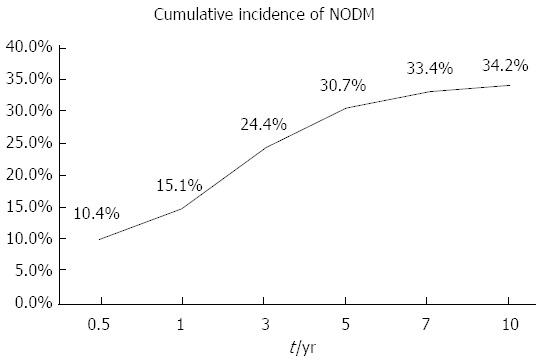
Cumulative incidence of new-onset diabetes mellitus over a 10-year period after liver transplantation. NODM: New-onset diabetes mellitus.
Table 1.
Demographic and clinical characteristics of recipients with and without new-onset diabetes millitus after liver transplantation (n = 528) n (%)
| Characteristics | Total (n = 528) | NODM group (n = 131) | Non-NODM group (n = 397) | P value |
| Recipient characteristics | ||||
| Age (yr) | 44.93 ± 9.41 | 46.24 ± 9.54 | 44.50 ± 9.34 | 0.068 |
| Gender (male) | 446 (84.5) | 144 (87.0) | 332 (83.6) | 0.352 |
| Child-Pugh (A/B/C) | 136/223/169 | 39/44/48 | 97/179/121 | 0.069 |
| MELD Score | 13 (6-40) | 15 (6-40) | 13 (6-40) | 0.010 |
| BMI ≥ 25 pre-LT | 110 (20.8) | 36 (27.5) | 74 (18.6) | 0.006 |
| Hypertension pre-LT | 12 (2.3) | 7 (5.3) | 5 (1.3) | 0.017 |
| Dyslipidemia pre-LT | 41 (8.2) | 15 (11.5) | 26 (6.5) | 0.069 |
| Indications for LT | ||||
| Hepatitis B virus disease | 420 (79.5) | 102 (77.9) | 318 (80.1) | 0.582 |
| Hepatitis C virus disease | 6 (1.1) | 1 (0.8) | 5 (1.3) | > 0.990 |
| Alcoholic cirrhosis | 16 (3.0) | 7 (5.3) | 9 (2.3) | 0.137 |
| Tumors | 269 (50.9) | 56 (42.7) | 213 (53.7) | 0.030 |
| Mean cTAC (ng/mL) | 5.26 ± 2.91 | 7.66 ± 3.41 | 4.47 ± 2.22 | < 0.001 |
| Rapamycin administration | 129 (24.4) | 30 (22.9) | 99 (24.9) | 0.638 |
| MMF administration | 322 (61.0) | 78 (59.5) | 244 (61.5) | 0.696 |
| Complications post-LT | ||||
| BMI ≥ 25 post-LT | 128 (24.2) | 40 (30.5) | 88 (22.2) | 0.053 |
| Hypertension post-LT | 67 (12.7) | 22 (16.8) | 45 (11.3) | 0.104 |
| Dyslipidaemia post-LT | 175 (33.1) | 63 (48.1) | 112 (28.2) | < 0.001 |
| Cardio-cerebral events post-LT | 18 (3.4) | 10 (7.6) | 8 (2.0) | 0.005 |
| CKD post-LT | 91 (17.2) | 28 (21.4) | 63 (15.9) | 0.148 |
| AR post-LT | 58 (11.0) | 20 (15.3) | 38 (9.6) | 0.071 |
| CR post-LT | 20 (3.8) | 9 (6.9) | 11 (2.8) | 0.062 |
| Infection post-LT | 165 (28.7) | 65 (36.7) | 100 (25.2) | 0.042 |
| Graft failure | 52 (9.8) | 20 (15.3) | 32 ( 8.1) | 0.016 |
| Donor characteristics | ||||
| Age (yr) | 34.01 ± 8.75 | 33.62 ± 8.33 | 34.13 ± 8.89 | 0.559 |
| Gender (male) | 443 (84.5) | 108 (82.4) | 335 (84.4) | 0.600 |
| Donor type (LDLT) | 158 (29.9) | 34 (26.0) | 124 (31.2) | 0.252 |
NODM: New-onset diabetes mellitus; Age: Age at transplantation; MELD: Model for end-stage liver disease; BMI: Body mass index; LT: Liver transplantation; cTAC: Tacrolimus trough concentration; MMF: Mycophenolate mofetil; CKD: Chronic kidney disease; AR: Acute rejection; CR: Chronic rejection; LDLT: Living donor liver transplantation.
Figure 2.
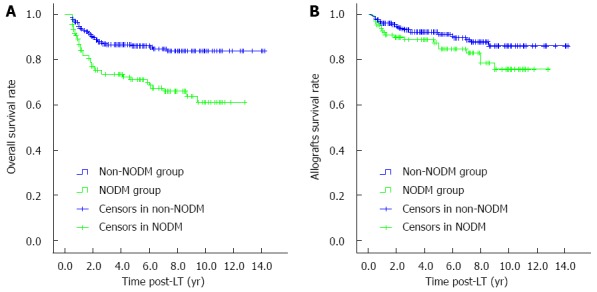
Survival rates of liver recipients in non-new-onset diabetes mellitus and new-onset diabetes mellitus groups. A: Overall survival rates (P < 0.05); B: Allograft survival rates (P < 0.05). NODM: New-onset diabetes mellitus; LT: Liver transplantation.
Definition of the cutoff mean cTAC after 6 mo
In our center, cTAC was measured and recorded at each visit. The mean cTAC was calculated and determined in the year when diabetes was diagnosed in the NODM group and in the last year of follow-up in the non-NODM group. Our study suggested that the mean cTAC was higher in the NODM group (7.66 ± 3.41 ng/mL) than in the non-NODM group (4.47 ± 2.22 ng/mL, P < 0.05; Table 1). A cutoff cTAC of 5.89 ng/mL was identified as predictive of post-LT NODM using an ROC curve (Figure 3). The diagnostic value showed that the area under the curve (AUC) was 0.815 (95%CI: 0.770-0.859, P < 0.05) with a sensitivity of 0.733 and a specificity of 0.809. All liver recipients were divided into two groups: a low mean cTAC (< 5.89 ng/mL) group (n = 356) and a high mean cTAC (≥ 5.89 ng/mL) group (n = 172).
Figure 3.
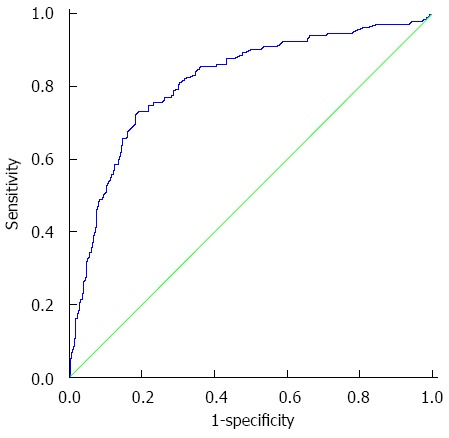
Receiver operating characteristic curve for mean cTAC after 6 mo to predict new-onset diabetes mellitus after transplantation.
To evaluate the impact of different mean cTAC levels on the long-term survival of the recipients after LT, we compared the common post-LT complications between the two cTAC groups (Table 2). We found that recipients in the high mean cTAC group were more frequently overweight/obese (30.2% vs 21.3%), and were more likely to develop dyslipidemia (44.8% vs 27.5%), CKD (22.7% vs 14.6%), and moderate to severe infection (33.1% vs 24.7%) than recipients in the low mean cTAC group (P < 0.05). However, there was no significant difference in other complications between the two groups. Kaplan-Meier survive curves suggested that recipients in the low mean cTAC group had higher 1-, 5-, and 10-year allograft survival rates (96.8%, 92.3%, and 87.4%) than recipients in the high mean cTAC group (92.0%, 82.9%, and 72.0%, P < 0.05; Figure 4A). The low mean cTAC group also exhibited higher 1-, 5-, and 10-year overall survival rates (93.7%, 83.8%, and 78.3% vs 90.5%, 78.6%, and 71.8%), but the difference was not statistically significant (P = 0.129; Figure 4B).
Table 2.
Clinical complications associated with mean tacrolimus trough concentration n (%)
| Complications post-LT | Low-cTAC group (n = 356) | High-cTAC group (n = 172) | P value |
| Overweight/obesity (BMI ≥ 25) | 76 (21.3) | 52 (30.2) | 0.026 |
| Hypertension | 48 (13.5) | 19 (11.0) | 0.431 |
| Dyslipidaemia | 98 (27.5) | 77 (44.8) | < 0.001 |
| Cardio-cerebral events | 12 (3.4) | 6 (3.5) | 0.944 |
| CKD | 52 (14.6) | 39 (22.7) | 0.021 |
| AR | 34 (9.6) | 24 (14.0) | 0.129 |
| CR | 10 (2.8) | 10 (5.8) | 0.090 |
| Infection | 88 (24.7) | 57 (33.1) | 0.042 |
| New-onset malignance | 8 (2.2) | 1 (0.6) | 0.304 |
cTAC: Tacrolimus trough concentration; BMI: Body mass index; LT: Liver transplantation; CKD: Chronic kidney disease; AR: Acute rejection; CR: Chronic rejection.
Figure 4.
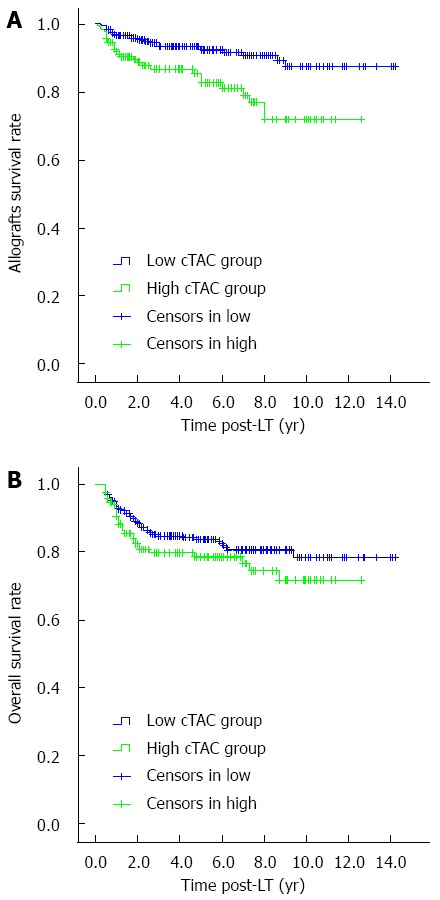
Survival rates of recipients in low and high mean tacrolimus trough concentration groups (P < 0.05). A: Allograft survival rates; B: Overall survival rate (P = 0.129). Low mean cTAC group: mean cTAC < 5.89 ng/mL; High cTAC group: mean cTAC ≥ 5.89 ng/mL. cTAC: Tacrolimus trough concentration; LT: Liver transplantation.
Risk factors for post-LT NODM
We examined more than 20 parameters to identify risk factors for NODM by univariate Cox regression analysis (Table 3). We chose all statistically significant factors as candidates for multivariate Cox regression analysis. As a result, recipient’ age at the time of LT (age > 50 years), pre-LT hypertension, and high mean cTAC (≥ 5.89 ng/mL) after 6 mo were deemed independent risk factors for post-LT NODM (Table 4).
Table 3.
Univariate analysis of risk factors for new-onset diabetes mellitus after liver transplantation
| Clinical factor | HR | 95%CI | P value |
| Recipient characteristics | |||
| Elder recipient (age > 50 yr) | 1.568 | 1.096-2.245 | 0.014 |
| Male recipient gender | 0.690 | 0.414-1.150 | 0.155 |
| Child-Pugh (A/B/C) | 0.985 | 0.788-1.232 | 0.895 |
| MELD Score | 1.107 | 0.997-1.037 | 0.088 |
| BMI ≥ 25 pre-LT | 1.616 | 1.100-2.373 | 0.014 |
| Hypertension pre-LT | 4.458 | 2.058-9.659 | < 0.001 |
| Dyslipidaemia pre-LT | 2.064 | 1.201-3.549 | 0.009 |
| Hepatitis B virus disease | 0.955 | 0.632-1.443 | 0.828 |
| Hepatitis C virus disease | 0.699 | 0.098-5.007 | 0.722 |
| Alcoholic cirrhosis | 2.307 | 1.076-4.948 | 0.032 |
| Tumors | 0.961 | 0.676-1.304 | 0.822 |
| With Rapamycin | 1.168 | 0.744-1.761 | 0.459 |
| With MMF | 0.979 | 0.690-1.387 | 0.903 |
| High mean cTAC (cTAC ≥ 5.89 ng/mL) | 8.709 | 5.873-12.915 | < 0.001 |
| BMI ≥ 25 post-LT | 1.345 | 0.927-1.951 | 0.119 |
| Hypertension post-LT | 1.278 | 0.808-2.021 | 0.294 |
| Dyslipidaemia post-LT | 2.014 | 1.429-2.838 | < 0.001 |
| CKD post-LT | 1.140 | 0.925-1.405 | 0.218 |
| AR post-LT | 1.701 | 1.056-2.742 | 0.029 |
| CR post-LT | 2.068 | 1.050-4.074 | 0.036 |
| Donor characteristics | |||
| Donor age at LT (per year) | 0.994 | 0.975-1.015 | 0.590 |
| Male donor gender | 1.202 | 0.766-1.886 | 0.423 |
| Donor type (LDLT) | 0.859 | 0.581-1.270 | 0.446 |
LT: Liver transplantation; MELD: Model for end-stage liver disease; MMF: Mycophenolate mofetil; cTAC: Tacrolimus trough concentration; CKD: Chronic kidney disease; AR: Acute rejection; CR: Chronic rejection; BMI: Body mass index; LDLT: Living donor liver transplantation.
Table 4.
Multivariate analysis of risk factors for new-onset diabetes mellitus after liver transplantation
| Clinical factor | HR | 95%CI | P value |
| Elder recipient (age > 50 yr) | 1.925 | 1.335-2.776 | < 0.001 |
| Hypertension pre-LT | 4.220 | 1.931-9.226 | < 0.001 |
| High mean cTAC (cTAC ≥ 5.89 ng/mL) | 9.474 | 6.357-14.119 | < 0.001 |
cTAC: Tacrolimus trough concentration; LT: Liver transplantation.
DISCUSSION
With improved long-term survival after transplantation, post-operative NODM in recipients has become more prevalent[25]. Our analysis of 528 liver transplant recipients showed that the cumulative incidence of new-onset DM increased after LT. The recipeints with NODM were more likely to develop dyslipidemia, cardio-cerebral vascular events, moderate to severe infections, and allograft loss, which often reduced recipient survival time[26,27]. Inevitably, recipients with NODM had poorer long-term overall and allograft survival than non-NODM recipients[5].
The immunosuppressive regimen employed after LT is important in decreasing the incidence of NODM. Corticosteroids could cause increased gluconeogenesis by inducing insulin resistance[28]. Previous studies have shown that the diabetogenic risks of corticosteroids are cumulative and dose-dependent and that early tapering of corticosteroids decreased the incidence of diabetes at 1 year after LT[29]. In our center, we therefore attempted to discontinue the use of corticosteroids within the first 3 mo of LT. Therefore, we analyzed blood glucose data after 6 mo to avoid the residual effects of corticosteroids on recipient metabolic profiling[30].
TAC dominant therapies remain the first-line immunosuppressive regimen indicated for liver recipients. By inhibiting IL-2 gene transcription, TAC decreases post-LT acute and chronic rejection. However, this mechanism may also contribute to insulin resistance and direct toxicity in pancreatic β-cells[31]. Previous studies have reported that TAC-associated chronic complications, such as metabolic disorders[2], renal dysfunction[11], and hepatocellular carcinoma recurrence[13], are related to TAC concentration. To reduce the TAC related complications, it is recommended that cTAC is reduced to 5-10 ng/mL during the first month[14]. However, the cutoffs or the ranges of cTAC were limited within early stages (4-26 wk) after transplantation and arbitrarily identified with no statistical evidence. Our study focused on the impact of long-term (after 6 mo) cTAC level on post-LT NODM and used an ROC curve to determine the best cutoff mean cTAC to be 5.89 ng/mL. Multivariate analysis showed that exposure to cTAC ≥ 5.89 ng/mL significantly increased the risk of post-LT NODM (HR = 9.474, 95%CI: 6.357-14.119). Similarly, exposure to a high mean cTAC also increased the risk of being overweight or obese, dyslipidemia, CKD, and moderate to severe infection after LT. Fortunately, recipients with a low mean cTAC after 6 mo did not suffer from more acute and chronic rejections. Surprisingly, recipients exposed to a low mean cTAC benefited from longer allograft survival. Thus, we suggest adjusting and maintaining the cTAC below 5.89 ng/mL after 6 mo to reduce chronic complications and improve the overall and allograft survival rates.
Additionally, Cox regression analysis indicated that recipient age (> 50 years) and pre-LT hypertension were independent risk factors in the incidence of post-LT NODM. As we know, increasing age is a significant risk factor for type 2 diabetes in the general population[32]. Correspondingly, diabetes has been a major cause of chronic complications, reduced quality of life and increased incidence of cardiovascular adverse events in the elderly. A UNOS study by Kuo et al[33] reported older age (> 50 years) to be an independent predictor of post-LT NODM, with a 24.1% risk increase in 15463 adult recipients. Otherwise, the prevalence of hypertension is usually high (> 50%) in diabetes patients[34], and hypertension causes a quadruply increase in cardiovascular risk in people with diabetes[35]. It is assumed that insulin resistance and the consequent hyperinsulinemia interacted with increased renal sodium retention, sympathetic tone and renin-angiotensin-aldosterone system activity[36].
Many studies have reported that BMI ≥ 25[33,37,38], dyslipidemia[38], and alcoholic cirrhosis[33,39] were independent risk factors for NODM after transplantation, but they were significant only in univariate analysis. HCV-associated liver disease was a high risk factor in previous studies[33,37], but was negative in our study. We assumed that this was due to the low percentage of HCV patients in our center (1.1%), unlike in western countries, where a large number of HCV patients received liver transplants.
In conclusion, some factors are positively related to diabetes progression after LT. Interestingly, mean cTAC is the only controllable factor, so adjusting the dose and trough concentration of TAC is important for preventing post-LT NODM. In accordance with the minimum required tacrolimus dosage early after transplantation, we recommend a decrease in the mean cTAC to < 5.89 ng/mL after 6 mo, as has been practical in Chinese liver transplantation recipients. Limitations of this study are that the data were collected retrospectively and that there was no detailed minimum scheme for timing after transplantation. Therefore, a well-designed prospective clinical trial is needed to confirm our findings and to develop an accepted tacrolimus adjustment protocol.
COMMENTS
Background
New-onset diabetes mellitus (NODM) is a serious metabolic complication after liver transplantation (LT) and is associated with increased rates of cardiovascular disease, rejection, infection and decreased survival. Tacrolimus has strong diabetic effects vs other immunosuppressants and early minimum tacrolimus strategy has been reported to be protective against other complications. The author performed this study to analyze the relationship between tacrolimus concentration (cTAC) and NODM development after 6 mo and to explore the impact of low cTAC on common complications after LT.
Research frontiers
Due to the negative impact of NODM on the long-term outcome of LT, the study about NODM has been important. cTAC is a controlled risk factor for NODM and early (4-26 wk) minimum tacrolimus strategy is safe and beneficial for LT recipients. This retrospective study indicated that reducing cTAC to below 5.89 ng/mL lately (after 6 mo) could prevent recipients from developing NODM and other complications.
Innovations and breakthroughs
Early minimum tacrolimus strategy can decrease the risk of renal dysfunction, dyslipidemia and tumor recurrence. But the cutoffs or the ranges of cTAC were limited within early stages (4-26 wk) after transplantation and arbitrarily identified with no statistical evidence. This study focused on the impact of long-term (6 mo) cTAC level on post-LT NODM and used an ROC curve to determine the best cutoff mean cTAC to be 5.89 ng/mL. And further analysis showed that reducing cTAC to 5.89 ng/mL decreased the incidence of other TAC related complications without increasing rejection.
Applications
Minimizing TAC lately (after 6 mo) to below 5.89 ng/mL is safe and protective against NODM after LT, but multicenter prospective clinical trials are needed to confirm the findings obtained in this study and to develop an accepted tacrolimus adjustment protocol.
Terminology
NODM is defined as diabetes newly diagnosed after LT, occurring in 16%-61% of recipients. Mean cTAC is determined as the average value of cTAC in the year of diabetes diagnosis in NODM recipients or in the last year of the follow-up period in non-NODM recipients.
Peer-review
This manuscript revealed that the risk of the new onset diabetes mellitus after liver transplantation is dependent on high mean tacrolimus. The number of patients is remarkable from a single institute.
Footnotes
Supported by Key Technology Support Program of Sichuan Province, No. 2013SZ0023.
Institutional review board statement: This study was approved by West China Hospital Ethics Committee, Chengdu, China.
Informed consent statement: All study participants, or their legal guardian, provided informed written consent prior to study enrollment.
Conflict-of-interest statement: The authors declare no conflict of interest.
Data sharing statement: Technical appendix, statistical code, and dataset available from the corresponding author at yanlunan688@163.com. Participants gave informed consent for data sharing.
Open-Access: This article is an open-access article which was selected by an in-house editor and fully peer-reviewed by external reviewers. It is distributed in accordance with the Creative Commons Attribution Non Commercial (CC BY-NC 4.0) license, which permits others to distribute, remix, adapt, build upon this work non-commercially, and license their derivative works on different terms, provided the original work is properly cited and the use is non-commercial. See: http://creativecommons.org/licenses/by-nc/4.0/
Peer-review started: September 17, 2015
First decision: October 14, 2015
Article in press: November 19, 2015
P- Reviewer: Hussain S, Inoue K, Tamemoto H S- Editor: Qi Y L- Editor: Ma JY E- Editor: Ma S
References
- 1.Adam R, McMaster P, O’Grady JG, Castaing D, Klempnauer JL, Jamieson N, Neuhaus P, Lerut J, Salizzoni M, Pollard S, et al. Evolution of liver transplantation in Europe: report of the European Liver Transplant Registry. Liver Transpl. 2003;9:1231–1243. doi: 10.1016/j.lts.2003.09.018. [DOI] [PubMed] [Google Scholar]
- 2.Bianchi G, Marchesini G, Marzocchi R, Pinna AD, Zoli M. Metabolic syndrome in liver transplantation: relation to etiology and immunosuppression. Liver Transpl. 2008;14:1648–1654. doi: 10.1002/lt.21588. [DOI] [PubMed] [Google Scholar]
- 3.Hanouneh IA, Feldstein AE, McCullough AJ, Miller C, Aucejo F, Yerian L, Lopez R, Zein NN. The significance of metabolic syndrome in the setting of recurrent hepatitis C after liver transplantation. Liver Transpl. 2008;14:1287–1293. doi: 10.1002/lt.21524. [DOI] [PubMed] [Google Scholar]
- 4.Laryea M, Watt KD, Molinari M, Walsh MJ, McAlister VC, Marotta PJ, Nashan B, Peltekian KM. Metabolic syndrome in liver transplant recipients: prevalence and association with major vascular events. Liver Transpl. 2007;13:1109–1114. doi: 10.1002/lt.21126. [DOI] [PubMed] [Google Scholar]
- 5.John PR, Thuluvath PJ. Outcome of patients with new-onset diabetes mellitus after liver transplantation compared with those without diabetes mellitus. Liver Transpl. 2002;8:708–713. doi: 10.1053/jlts.2002.34638. [DOI] [PubMed] [Google Scholar]
- 6.Watt KD, Pedersen RA, Kremers WK, Heimbach JK, Charlton MR. Evolution of causes and risk factors for mortality post-liver transplant: results of the NIDDK long-term follow-up study. Am J Transplant. 2010;10:1420–1427. doi: 10.1111/j.1600-6143.2010.03126.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Wheeler DC, Krentz AJ. New-onset diabetes after transplantation. Br J Hosp Med (Lond) 2007;68:190–194. doi: 10.12968/hmed.2007.68.4.190. [DOI] [PubMed] [Google Scholar]
- 8.A comparison of tacrolimus (FK 506) and cyclosporine for immunosuppression in liver transplantation. The U.S. Multicenter FK506 Liver Study Group. N Engl J Med. 1994;331:1110–1115. doi: 10.1056/NEJM199410273311702. [DOI] [PubMed] [Google Scholar]
- 9.Haddad EM, McAlister VC, Renouf E, Malthaner R, Kjaer MS, Gluud LL. Cyclosporin versus tacrolimus for liver transplanted patients. Cochrane Database Syst Rev. 2006;(4):CD005161. doi: 10.1002/14651858.CD005161.pub2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Wiesner RH, Fung JJ. Present state of immunosuppressive therapy in liver transplant recipients. Liver Transpl. 2011;17 Suppl 3:S1–S9. doi: 10.1002/lt.22410. [DOI] [PubMed] [Google Scholar]
- 11.Rodríguez-Perálvarez M, Germani G, Darius T, Lerut J, Tsochatzis E, Burroughs AK. Tacrolimus trough levels, rejection and renal impairment in liver transplantation: a systematic review and meta-analysis. Am J Transplant. 2012;12:2797–2814. doi: 10.1111/j.1600-6143.2012.04140.x. [DOI] [PubMed] [Google Scholar]
- 12.Karie-Guigues S, Janus N, Saliba F, Dumortier J, Duvoux C, Calmus Y, Lorho R, Deray G, Launay-Vacher V, Pageaux GP. Long-term renal function in liver transplant recipients and impact of immunosuppressive regimens (calcineurin inhibitors alone or in combination with mycophenolate mofetil): the TRY study. Liver Transpl. 2009;15:1083–1091. doi: 10.1002/lt.21803. [DOI] [PubMed] [Google Scholar]
- 13.Vivarelli M, Dazzi A, Zanello M, Cucchetti A, Cescon M, Ravaioli M, Del Gaudio M, Lauro A, Grazi GL, Pinna AD. Effect of different immunosuppressive schedules on recurrence-free survival after liver transplantation for hepatocellular carcinoma. Transplantation. 2010;89:227–231. doi: 10.1097/TP.0b013e3181c3c540. [DOI] [PubMed] [Google Scholar]
- 14.Jia JJ, Lin BY, He JJ, Geng L, Kadel D, Wang L, Yu DD, Shen T, Yang Z, Ye YF, et al. ‘’Minimizing tacrolimus’’ strategy and long-term survival after liver transplantation. World J Gastroenterol. 2014;20:11363–11369. doi: 10.3748/wjg.v20.i32.11363. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Golshayan D, Pascual M. Minimization of calcineurin inhibitors to improve long-term outcomes in kidney transplantation. Transpl Immunol. 2008;20:21–28. doi: 10.1016/j.trim.2008.08.006. [DOI] [PubMed] [Google Scholar]
- 16.Lerut JP, Pinheiro RS, Lai Q, Stouffs V, Orlando G, Juri JM, Ciccarelli O, Sempoux C, Roggen FM, De Reyck C, et al. Is minimal, [almost] steroid-free immunosuppression a safe approach in adult liver transplantation? Long-term outcome of a prospective, double blind, placebo-controlled, randomized, investigator-driven study. Ann Surg. 2014;260:886–91; discussion 891-2. doi: 10.1097/SLA.0000000000000969. [DOI] [PubMed] [Google Scholar]
- 17.Boillot O, Seket B, Dumortier J, Pittau G, Boucaud C, Bouffard Y, Scoazec JY. Thymoglobulin induction in liver transplant recipients with a tacrolimus, mycophenolate mofetil, and steroid immunosuppressive regimen: a five-year randomized prospective study. Liver Transpl. 2009;15:1426–1434. doi: 10.1002/lt.21905. [DOI] [PubMed] [Google Scholar]
- 18.Nashan B, Saliba F, Durand F, Barcéna R, Herrero JI, Mentha G, Neuhaus P, Bowles M, Patch D, Bernardos A, et al. Pharmacokinetics, efficacy, and safety of mycophenolate mofetil in combination with standard-dose or reduced-dose tacrolimus in liver transplant recipients. Liver Transpl. 2009;15:136–147. doi: 10.1002/lt.21657. [DOI] [PubMed] [Google Scholar]
- 19.Shao ZY, Yan LN, Wang WT, Li B, Wen TF, Yang JY, Xu MQ, Zhao JC, Wei YG. Prophylaxis of chronic kidney disease after liver transplantation--experience from west China. World J Gastroenterol. 2012;18:991–998. doi: 10.3748/wjg.v18.i9.991. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.First MR, Dhadda S, Croy R, Holman J, Fitzsimmons WE. New-onset diabetes after transplantation (NODAT): an evaluation of definitions in clinical trials. Transplantation. 2013;96:58–64. doi: 10.1097/TP.0b013e318293fcf8. [DOI] [PubMed] [Google Scholar]
- 21.Orlando G, Baiocchi L, Cardillo A, Iaria G, De Liguori Carino N, De Luca L, Ielpo B, Tariciotti L, Angelico M, Tisone G. Switch to 1.5 grams MMF monotherapy for CNI-related toxicity in liver transplantation is safe and improves renal function, dyslipidemia, and hypertension. Liver Transpl. 2007;13:46–54. doi: 10.1002/lt.20926. [DOI] [PubMed] [Google Scholar]
- 22.National Kidney Foundation. K/DOQI clinical practice guidelines for chronic kidney disease: evaluation, classification, and stratification. Am J Kidney Dis. 2002;39:S1–266. [PubMed] [Google Scholar]
- 23.Kamath PS, Wiesner RH, Malinchoc M, Kremers W, Therneau TM, Kosberg CL, D’Amico G, Dickson ER, Kim WR. A model to predict survival in patients with end-stage liver disease. Hepatology. 2001;33:464–470. doi: 10.1053/jhep.2001.22172. [DOI] [PubMed] [Google Scholar]
- 24.Davidson J, Wilkinson A, Dantal J, Dotta F, Haller H, Hernández D, Kasiske BL, Kiberd B, Krentz A, Legendre C, et al. New-onset diabetes after transplantation: 2003 International consensus guidelines. Proceedings of an international expert panel meeting. Barcelona, Spain, 19 February 2003. Transplantation. 2003;75:SS3–S24. doi: 10.1097/01.TP.0000069952.49242.3E. [DOI] [PubMed] [Google Scholar]
- 25.Parekh J, Corley DA, Feng S. Diabetes, hypertension and hyperlipidemia: prevalence over time and impact on long-term survival after liver transplantation. Am J Transplant. 2012;12:2181–2187. doi: 10.1111/j.1600-6143.2012.04077.x. [DOI] [PubMed] [Google Scholar]
- 26.Albeldawi M, Aggarwal A, Madhwal S, Cywinski J, Lopez R, Eghtesad B, Zein NN. Cumulative risk of cardiovascular events after orthotopic liver transplantation. Liver Transpl. 2012;18:370–375. doi: 10.1002/lt.22468. [DOI] [PubMed] [Google Scholar]
- 27.Kim SI. Bacterial infection after liver transplantation. World J Gastroenterol. 2014;20:6211–6220. doi: 10.3748/wjg.v20.i20.6211. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Subramanian S, Trence DL. Immunosuppressive agents: effects on glucose and lipid metabolism. Endocrinol Metab Clin North Am. 2007;36:891–905; vii. doi: 10.1016/j.ecl.2007.07.003. [DOI] [PubMed] [Google Scholar]
- 29.Weiler N, Thrun I, Hoppe-Lotichius M, Zimmermann T, Kraemer I, Otto G. Early steroid-free immunosuppression with FK506 after liver transplantation: long-term results of a prospectively randomized double-blinded trial. Transplantation. 2010;90:1562–1566. doi: 10.1097/TP.0b013e3181ff8794. [DOI] [PubMed] [Google Scholar]
- 30.Li HY, Li B, Wei YG, Yan LN, Wen TF, Zhao JC, Xu MQ, Wang WT, Ma YK, Yang JY. Higher tacrolimus blood concentration is related to hyperlipidemia in living donor liver transplantation recipients. Dig Dis Sci. 2012;57:204–209. doi: 10.1007/s10620-011-1817-5. [DOI] [PubMed] [Google Scholar]
- 31.McAlister VC, Haddad E, Renouf E, Malthaner RA, Kjaer MS, Gluud LL. Cyclosporin versus tacrolimus as primary immunosuppressant after liver transplantation: a meta-analysis. Am J Transplant. 2006;6:1578–1585. doi: 10.1111/j.1600-6143.2006.01360.x. [DOI] [PubMed] [Google Scholar]
- 32.Dunning T, Sinclair A, Colagiuri S. New IDF Guideline for managing type 2 diabetes in older people. Diabetes Res Clin Pract. 2014;103:538–540. doi: 10.1016/j.diabres.2014.03.005. [DOI] [PubMed] [Google Scholar]
- 33.Kuo HT, Sampaio MS, Ye X, Reddy P, Martin P, Bunnapradist S. Risk factors for new-onset diabetes mellitus in adult liver transplant recipients, an analysis of the Organ Procurement and Transplant Network/United Network for Organ Sharing database. Transplantation. 2010;89:1134–1140. doi: 10.1097/TP.0b013e3181d2fec1. [DOI] [PubMed] [Google Scholar]
- 34.Nilsson PM, Cederholm J, Zethelius BR, Eliasson BR, Eeg-Olofsson K, Gudbj Rnsdottir S. Trends in blood pressure control in patients with type 2 diabetes: data from the Swedish National Diabetes Register (NDR) Blood Press. 2011;20:348–354. doi: 10.3109/08037051.2011.587288. [DOI] [PubMed] [Google Scholar]
- 35.Mogensen CE. New treatment guidelines for a patient with diabetes and hypertension. J Hypertens Suppl. 2003;21:S25–S30. [PubMed] [Google Scholar]
- 36.Redon J, Cifkova R, Laurent S, Nilsson P, Narkiewicz K, Erdine S, Mancia G. Mechanisms of hypertension in the cardiometabolic syndrome. J Hypertens. 2009;27:441–451. doi: 10.1097/HJH.0b013e32831e13e5. [DOI] [PubMed] [Google Scholar]
- 37.Li DW, Lu TF, Hua XW, Dai HJ, Cui XL, Zhang JJ, Xia Q. Risk factors for new onset diabetes mellitus after liver transplantation: A meta-analysis. World J Gastroenterol. 2015;21:6329–6340. doi: 10.3748/wjg.v21.i20.6329. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Pérez-Flores I, Sánchez-Fructuoso A, Calvo N, Valga EF, Barrientos A. Incidence and risk factors for the metabolic syndrome and posttransplant diabetes in renal transplant recipients taking tacrolimus. Transplant Proc. 2010;42:2902–2904. doi: 10.1016/j.transproceed.2010.08.005. [DOI] [PubMed] [Google Scholar]
- 39.Schmilovitz-Weiss H, Mor E, Sulkes J, Bar-Nathan N, Shaharabani E, Melzer E, Tur-Kaspa R, Ben-Ari Z. Association of post-liver transplantation diabetes mellitus with hepatitis C virus infection. Transplant Proc. 2003;35:667–668. doi: 10.1016/s0041-1345(03)00090-3. [DOI] [PubMed] [Google Scholar]


