Abstract
Dilatation of the colon and the rectum, which is not attributable to aganglionosis, is a rare finding and can be the result of intractable chronic constipation. We report a rare case of a 29-year-old male patient with impressive megacolon, in whom Hirschsprung’s or Chagas disease was ruled out. In the present case, dilatation of the colon was most likely due to a behavioral disorder with habitual failure of defecation. Chronic stool retention led to a bizarre bulging of the large bowel with displacement of the other abdominal organs and severe occult blood loss. Because of two episodes of life-threatening gastrointestinal bleeding despite conventional treatment of constipation, a surgical approach for bowel restoration was necessary. Temporary loop ileostomy had to be performed for depressurization of the large bowel and the subsequent possibility for effective antegrade colonic lavage to remove impacted stools. Shortly after the operation, the patient was healthy and could easily manage the handling of the ileostomy. However, the course of the megacolon in this young adult cannot be predicted and the follow-up will have to reveal if regression of this extreme colonic distension with reestablishment of regular rectal perception will occur.
Keywords: Gastrointestinal bleeding, Malabsorption, Habitual megacolon
INTRODUCTION
Occult gastrointestinal bleeding is a frequent actuality in human beings, likewise is a temporary absence after drinking beer on the “Oktoberfest” in Munich. We report the case of a young male with the unusual combination of both conditions.
CASE REPORT
A 29-year-old male patient collapsed at the “Oktoberfest” after consumption of a small beer and was admitted to our emergency department. The patient was pale and displayed hemoglobin of 30 g/L despite normal blood pressure and heart rate. On clinical examination, cachexia and an obvious distension of the abdomen with slight pain in the epigastrium and the periumbilical region were noted. The digital rectal exam revealed black stools with positive guaiac testing, but the patient denied gross rectal bleeding in the past. The patient has seldom bowel movements (every third day) and denotes the absence of the urge for defecation. He has recently lost his job as a janitor because of permanent fatigue and decreasing tolerance to work. Furthermore, he reported an unclassified “bowel disease” since early childhood and a “dilatation” of the colon which had been performed during infancy. Two years ago, iron deficiency anemia had been treated at another hospital but repeated attempts for colonoscopy had failed because of stool residues in the colon despite lavage for several days at that time.
After transfusion, a diagnostic procedure was performed in addition to the severe anemia and the laboratory tests revealed significant iron deficiency with a ferritin level of 6 µg/L and transferrin saturation of 4.5%. Serum potassium and albumin were decreased to 2.13 mmol/L and 28 g/L, respectively. The abdominal CT scan showed massive dilatation of the rectum and the left-sided colon (Figures 1A and B) with displacement of the other organs. A colonoscopy could not be performed because of persistent masses of stools in the colon even after prolonged bowel lavage. An upper gastrointestinal endoscopy demonstrated regular mucosa without evidence for celiac disease or a bleeding source in the proximal gastrointestinal tract. A radionuclide bleeding scan was negative for an apparent bleeding source. Rectal manometry demonstrated regular arbitrary contraction and a normal reflectory relaxation of the anal sphincter. A dynamic MR defecography revealed again a massive dilatation of the distal colon with complete failure of emptying on command. The histological examination of a rectal biopsy demonstrated chronic proctitis with pseudomelanosis and explicit verification of submucous ganglions excluding Hirschsprung’s disease (aganglionosis). Chagas’ disease was ruled out by serology. A pathological H2-glucose breath test showed signs for a bacterial overgrowth of the small bowel and significant osteopenia was documented by measurement of the bone density by dual X-ray densitometry.
Figure 1.
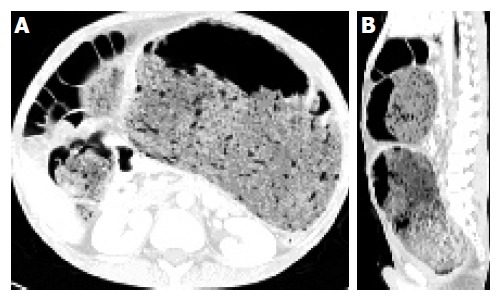
A: Axial CT image of the abdomen; B: Saggital CT reconstruction of the abdomen.
Initially, we aimed at relieving the chronic constipation by regular administration of polyethylene glycol. However, distention of the colon was even progressive and gastrointestinal bleeding continued. Therefore, a temporary loop ileostomy was performed and about 12 kg of stools could be removed by antegrade colonic lavage. A CT scan 3 wk after surgery demonstrated declining of the colonic dilatation with a marked decrease of abdominal distension. The postoperative course was uneventful and the patient’s fitness improved significantly. He received intravenous iron and vitamin supplementation and due to the bacterial overgrowth antibiotic treatment with metronidazole was initiated. Subsequently lower gastrointestinal bleeding subsided and a repeat colonoscopy showed regular mucosa in the right colon with atrophic appearance of the mucosa in the left colon. The patient was motivated to perform stool training aiming at the establishment of a normal rectal perception.
DISCUSSION
Dilatation of the colon and the rectum, which is not attributable to aganglionosis[1] is a rare finding and can be the result of intractable chronic constipation[2]. Herein we report a rare case of a young adult with impressive megacolon, in whom Hirschsprung’s or Chagas disease was ruled out. In the present case dilatation of the colon is likely to be due to a behavioral disorder with habitual failure of defecation. Chronic stool retention led to a bizarre bulging of the large bowel with displacement of the other abdominal organs. Occult gastrointestinal bleeding has not been described in patients with megacolon, but in our patient dilation of the colonic wall presumably resulted in occult blood loss. The exact bleeding source could not be localized by a radionuclide bleeding scan, thus the intensity of bleeding was supposed to be low. The low hemoglobin value was well tolerated by the patient; therefore, the anemia was most likely due to a chronic blood loss. However, the patient had previously experienced two episodes of life-threatening gastrointestinal bleeding despite conventional treatment of constipation; consequently, a surgical approach for bowel restoration appeared feasible.
A further concern in this patient was the apparent malabsorption with low levels of albumin, severe iron deficiency and osteoporosis. Distension of the colon with subsequent stasis can lead to small bowel bacterial overgrowth, as demonstrated in patients with megacolon due to Chagas disease[3]. Restoration of the small bowel by antibiotic treatment would be a futile approach as long as the underlying stasis of the bowel is not corrected. Therefore, a temporary loop ileostomy was performed for depressurization of the large bowel and the subsequent possibility for effective antegrade colonic lavage to remove impacted stools[4].
In the present case, the indication for surgical intervention was delicate, because ileostomy does not affect the underlying behavioral disorder and includes the risk for a complete unlearning of defecation. Furthermore, the development of a diversion colitis is a possible sequelae[5]. Nevertheless, shortly after the operation the patient was healthy and could easily manage the handling of the ileostomy. However, the course of the megacolon in this young adult cannot be predicted and the follow-up will have to reveal if regression of this extreme colonic distension with re-establishment of regular rectal perception will occur.
Footnotes
Science Editor Guo SY Language Editor Elsevier HK
References
- 1.Puri P, Shinkai T. Pathogenesis of Hirschsprung’s disease and its variants: recent progress. Semin Pediatr Surg. 2004;13:18–24. doi: 10.1053/j.sempedsurg.2003.09.004. [DOI] [PubMed] [Google Scholar]
- 2.Rajagopal A, Martin J. Giant fecaloma with idiopathic sigmoid megacolon: report of a case and review of the literature. Dis Colon Rectum. 2002;45:833–835. doi: 10.1007/s10350-004-6306-x. [DOI] [PubMed] [Google Scholar]
- 3.Guimaraes Quintanilha AG, Azevedo dos Santos MA, Avila-Campos MJ, Saad WA, Pinotti HW, Zilberstein B. Chagasic megacolon and proximal jejunum microbiota. Scand J Gastroenterol. 2000;35:632–636. doi: 10.1080/003655200750023606. [DOI] [PubMed] [Google Scholar]
- 4.Stabile G, Kamm MA, Hawley PR, Lennard-Jones JE. Results of stoma formation for idiopathic megarectum and megacolon. Int J Colorectal Dis. 1992;7:82–84. doi: 10.1007/BF00341291. [DOI] [PubMed] [Google Scholar]
- 5.Edwards CM, George B, Warren B. Diversion colitis--new light through old windows. Histopathology. 1999;34:1–5. doi: 10.1046/j.1365-2559.1999.00624.x. [DOI] [PubMed] [Google Scholar]


