Abstract
OBJECTIVE:
To determine whether challenging behavior in young children with autism and other developmental disabilities can be treated successfully at lower cost by using telehealth to train parents to implement applied behavior analysis (ABA).
METHODS:
We compared data on the outcomes and costs for implementing evidence-based ABA procedures to reduce problem behavior by using 3 service delivery models: in-home therapy, clinic-based telehealth, and home-based telehealth. Participants were 107 young children diagnosed with autism or other neurodevelopmental disorders, and data analysis focused on the 94 children who completed treatment.
RESULTS:
All 3 service delivery models demonstrated successful reduction of problem behavior by training parents to conduct functional analysis and functional communication training. The mean percentage reduction in problem behavior was >90% in all 3 groups after treatment, and treatment acceptability based on parent ratings was high for all groups. Total costs for implementing treatment were lowest for home telehealth, but both telehealth models were significantly less costly than in-home therapy.
CONCLUSIONS:
This research demonstrated that parents can use ABA procedures to successfully treat behavior problems associated with autism spectrum disorders regardless of whether treatment is directed by behavior consultants in person or via remote video coaching. Because ABA telehealth can achieve similar outcomes at lower cost compared with in-home therapy, geographic barriers to providing access to ABA for treating problem behavior can be minimized. These findings support the potential for using telehealth to provide research-based behavioral treatment to any family that has access to the Internet.
Applied behavior analysis (ABA) is the most widely researched intervention for autism spectrum disorder (ASD), and the majority of evidence-based treatments for ASD use ABA strategies (eg, reinforcement, extinction).1 ABA-based interventions for ASD have typically focused on either (a) skill acquisition through core ABA strategies (eg, discrete trial training,2 pivotal response training3), often performed within a developmental framework (eg, Early Start Denver Model4), or (b) treatment of clinically significant behavior.5 Among ABA methods for treating problem behavior in ASDs, functional communication training (FCT)6 is the most widely used, and previous research has demonstrated that FCT can effectively treat many types of behavior problems across a variety of settings.7
FCT begins with a functional analysis (FA)8 to identify the function that maintains challenging behavior for each child.9 Typical social functions include escape (avoiding a nonpreferred activity), attention (gaining attention from an adult or peer), and tangible (obtaining a desired object or activity). After the function of a problem behavior has been identified, children are taught to use alternative communication strategies that serve the same function as the problem behavior.10 By replacing a child’s problem behavior with appropriate social communication, FCT can help a child adapt to the demands of daily life.
The current study compared the outcomes and costs associated with 3 different models for delivery of FA and FCT to treat problem behavior in young children with ASD and other developmental disabilities (DDs). In all 3 models, parents were coached by behavior consultants to conduct FA and FCT during weekly sessions. Wacker et al5 demonstrated that weekly coaching for parents can identify the social functions of problem behavior and replace these behaviors with alternative communication.11–13 In the initial studies in this series,12,13 behavior consultants traveled to family homes weekly to coach parents in conducting FA and FCT. The same strategies have subsequently been tested via telehealth, initially by having families travel to outpatient clinics near their homes5,11 and later by providing telehealth coaching to parents in their own homes.14 The purpose of the current study was to compare the behavioral outcomes, costs, and family acceptance of in-home telehealth with the results obtained when consultants coached parents in person at home or via telehealth at regional clinics. If these 3 models for delivering FA and FCT can achieve comparable behavioral outcomes, then treatment can be selected based on cost, provider availability, or family preference.
Methods
Participants
Children
Participants were 107 children with ASD or other DD (ages 21–84 months; mean age = 49.95 months) who were treated between 1996 and 2014 for problem behavior. Group 1 included children with ASD (n = 16) or other DD (n = 36) who were treated in their homes by behavior consultants between 1996 and 2009. The consultants trained the child’s parents to conduct FA and FCT to replace problem behavior with appropriate social communication. Group 2 included children with confirmed ASD (n = 23) who were treated in 2009 to 2012 as part of a study to train parents to conduct FA and FCT when coached via telehealth at a regional clinic near their home. Group 3 included children with ASD (n = 32) who were treated in 2012 to 2014 as part of a randomized controlled trial of FCT treatment conducted by parents who received telehealth coaching at home. This trial is ongoing, and all children enrolled in the trial eventually receive FCT treatment.
Children whose problem behavior served a “social” function as identified by FA were referred for treatment with FCT. Only children who completed FA and were started in FCT were included in the current analysis. Information on a subsample of children from group 1 was reported previously by Wacker et al.12 Wacker et al5,11 reported selected data from 20 of the participants from group 2, and Suess et al14 described treatment fidelity data from the first 3 participants in group 3. Among the 107 children who started FCT in these 3 groups, 8 discontinued treatment in group 1 (3 with ASD, 5 with other DD), 3 discontinued treatment in group 2, and 2 discontinued treatment in group 3. Rates of treatment completion did not differ significantly across groups.
Parents
Children’s parents (or grandparents) conducted all FA and FCT sessions with coaching from trained behavior consultants. Parent data were available only for groups 2 and 3. Parent ages ranged from 23 to 51 years; educational levels ranged from grade 11 to a doctorate.
Behavior Consultants
Behavior consultants were experienced behavior analysts or advanced graduate students with ≥2 years of experience in behavior analysis. Each week, they reviewed data from FA and FCT sessions with a supervising doctoral-level behavioral psychologist. Family navigators from Iowa’s Child Health Specialty Clinic network assisted families in the Clinic Telehealth group, as described in Wacker et al.5,11
Procedures
Diagnostic Assessment
Research procedures for the protection of human subjects were approved by the University of Iowa Institutional Review Board. Only children with significant behavior problems (aggression, destruction, tantrums, self-injury) were referred for these studies, and this referral process was consistent over time. Diagnoses for participants receiving in-home ABA therapy in group 1 were determined by review of medical records and interviews with parents or caregivers. For both groups receiving telehealth, a diagnosis of ASD was confirmed with the Autism Diagnostic Interview–Revised,15 Autism Diagnostic Observation Schedule,16 and Diagnostic and Statistical Manual of Mental Disorders, Fourth Edition.17 In group 1, 30% of participants had an ASD diagnosis, whereas 100% of children in groups 2 and 3 were diagnosed with ASD. Intellectual disability (ID) was determined based on clinic records for group 1 and standardized assessments of development and adaptive skills for groups 2 and 3.5,14
Functional Analysis
For all 3 study groups, parents were taught to conduct FA within a multielement single-case design based on procedures described by Iwata et al.8 FA sessions were 5 minutes in duration and were recorded for later coding by independent data collectors; typically 3 to 5 sessions were completed during each 60-minute home or telehealth visit. All FA sessions were conducted by the parents with coaching from the behavior consultant according to procedures described in Harding et al.18
Functional Communication Training
Each weekly treatment visit lasted ∼60 minutes; individual sessions during each visit were 5 minutes in duration and were recorded for later data coding. A word/picture card or microswitch with voice output was paired with any preexisting mand (appropriate request) to assist children in overcoming communication difficulties. Requests were reinforced, and engagement in problem behavior was ignored (placed on extinction) or resulted in guided compliance. Treatment was individualized based on the results of the FA. For example, if the FA showed that problem behavior functioned to escape demands, then FCT involved teaching the child to appropriately request breaks after compliance. A small amount of developmentally appropriate work was placed in front of the child. When the task was completed, a word card or microswitch was placed in front of the child, and the child was prompted to request a break. Break activities were matched to a preference assessment.19 Problem behavior resulted in continuation of the task or re-presentation of the task if it occurred during a break. Parents were directed to practice FCT procedures for 10 to 15 minutes daily at home. At the completion of FCT, parents used a 7-point scale to rate the acceptability of treatment by using the first item on the Treatment Acceptability Rating Form–Revised.20
Treatment continued for ≥25 weeks or until problem behavior decreased by ≥80% from baseline over 3 consecutive FCT sessions, the child complied with ≥80% of task requests, and the child made requests independently at appropriate times. Thirteen children who started treatment did not continue in treatment long enough to reach these criteria. In group 1, 5 children discontinued treatment because of changes in parent work schedules that precluded continued treatment; 3 children moved to a different locality and did not maintain contact with the study. In group 2, 1 family determined that problem behavior was no longer a serious concern at home, 1 child moved to a different locality not served by the study, and 1 child discontinued because the parents wanted to focus on verbal communication without using picture cards or microswitches. In group 3, 1 child moved out of state and did not maintain contact with the study, and 1 child could not be managed by parents at home and was referred for out-of-home residential placement.
Settings and Equipment
Homes
Parents conducted sessions in rooms within their homes (eg, bedroom, living room) for groups 1 and 3. For group 1, consultants brought video recording equipment on each visit. For group 3, parents were given a Windows-based laptop, webcam, and Ethernet cable at the time of enrollment if they did not already own the necessary equipment (see Lee et al21). Internet service was also provided to families if needed. For groups 1 and 3, leisure activities and work materials available in the home were used during FA and FCT. Behavior consultants provided families with microswitches and picture cards for FCT.
Telehealth Center
For groups 2 and 3, consultants provided remote coaching from the telehealth center at the University of Iowa Children’s Hospital.5,11 Telehealth workstations were equipped with a Windows-based PC, video monitor, webcam, and headset.21 For group 2, existing videoconferencing software was used at the hospital site.5,11 This software allowed the consultant to record the telehealth sessions for subsequent data collection. For group 3, parent permission was obtained to use general-use videoconferencing software (ie, Skype), and no privacy issues were encountered during the study.
Regional Clinics
Parents conducted sessions at regional clinics for group 2. Each clinic site had access to high-speed Internet and videoconferencing software.5,11 Parent assistants managed the equipment at the clinic sites. The behavior consultants provided parents in group 2 with leisure activities, microswitches, and picture cards to use in the clinic.
Data Analysis
Single-Subject Analyses
Data for all participants were obtained within single-subject designs, and observation sessions were recorded for each FA and FCT visit. Each 5-minute session was divided into 50 6-second intervals, and problem behavior was coded if present in each interval.5,11 Interobserver agreement was obtained for 30% of sessions and averaged >95% agreement. The percentage reduction in problem behavior was determined by comparing the number of 6-second intervals that included problem behavior at baseline with the end of FCT. Similar data on increases in manding and task completion were available only for groups 2 and 3.
Comparisons Between Treatment Delivery Models
The treatment groups were compared with analysis of variance (ANOVA) for continuous variables and χ2 or Fisher’s exact test (to adjust for small cell sizes) for categorical variables. When the ANOVA was significant, post hoc testing with the Tukey honest significant difference test determined which groups differed significantly. Although the sample size in each treatment group was limited by the number of children receiving each treatment, the study had ≥80% power to detect a between-group difference of ≥9 percentage points on the primary outcome variable (ie, percentage reduction in problem behavior). In estimating costs for implementing FA and FCT procedures, staff costs, facility costs, and family costs were examined separately (in 2014 dollars) and estimated for clinical use when grant funds were not available to cover expenses.
Staff costs included salaries and benefits for behavior consultants ($30 per hour, 1.75 hours per child per week), doctoral-level psychologists ($50 per hour, 0.25 hours per child per week), family navigators ($22 per hour, 1.5 hours per child per week), and data coders ($20 per hour, 1 hour per child per week). Consultant mileage ($0.56 per mile) for travel to family homes was also included.
Facility costs included annual expenses for room space (with utilities and maintenance) of $25 per square foot. The use of rooms was allocated using a per-hour rate (assuming a 40-hour week) derived from the annual cost rate for a teleconferencing room of 100 square feet, an office area (with conference table and data coding desk) of 200 square feet, and a large regional clinic room of 200 square feet. Computer costs were estimated by determining hourly costs based on annual expenses for computer purchase and maintenance. These costs included $0.96 per hour for teleconferencing computers (with webcam, monitor, and software) at the hospital and the regional clinics, $0.72 per hour for use of a computer for data coding and graphing, and $0.58 per hour for a laptop computer for a traveling consultant to record sessions during home visits.
Family costs were calculated based on the use of a general purpose computer (with webcam and software) that would be used for FA and FCT ≤5 hours per week. Costs would include a computer ($2.90 per week) and Internet ($2.00 per week) for group 3 or travel to a regional clinic ($0.235 per mile) for group 2. The cost of parent time was estimated at the 2014 US average hourly wage ($24.63 per hour22), with time in session of 1 hour per week and practice time of 1 hour per week for all groups, plus travel time of 0.75 mile per minute for group 2. Also, $100 was needed for each family to cover the cost of microswitches and picture cards during treatment.
Results
Participant Characteristics
Table 1 lists characteristics of the participants who completed treatment in each of the 3 groups. The children did not differ in age between groups, averaging 48 to 52 months of age at the beginning of treatment. ASD was the primary diagnosis for all children in groups 2 and 3 and for 30% of the children in group 1. Intellectual disability was present in most children in group 1 and half of the children in groups 2 and 3. All 3 groups included more boys than girls, especially the groups with only participants with ASD. As expected, children in group 1 lived closer to the Children’s Hospital than those in either telehealth group. All participants showed ≥1 social function, and most had >1. The frequency of an attention function was especially low in the groups restricted to children with ASD.
TABLE 1.
Participant Characteristics for Children Who Received FA and FCT Treatment via Different Service Delivery Models
| Variables | Group 1: In-Home Therapy, 1996–2009 (n = 44) | Group 2: Clinic Telehealth, 2009–2012 (n = 20) | Group 3: Home Telehealth, 2012–2014 (n = 30) | P |
|---|---|---|---|---|
| Age: mean (SD), mo | 48.20 (15.44) | 50.30 (15.53) | 52.43 (17.45) | .491 |
| Range, mo | 22–83 | 29–80 | 21–84 | |
| Gender | 13 F, 31 M | 1 F, 19 M | 5 F, 25 M | .060 |
| Primary diagnosis, n (%) | ||||
| ASD | 13 (30%)a | 20 (100%)b | 30 (100%)b | <.001c |
| Other DD | 31 (70%) | 0 (0%) | 0 (0%) | |
| ID, n (%) | 42 (95%)a | 10 (50%)b | 15 (50%)b | <.001c |
| Distance from Children’s Hospital | ||||
| Mean (SD), miles | 67.02 (40.33)a | 200.75 (95.25)b | 116.23 (77.85)d | <.001c |
| Range, miles | 3–158 | 39–317 | 3–310 | |
| Social function identified, n (%)e | ||||
| Escape | 36 (82%) | 13 (65%) | 17 (57%) | .056 |
| Tangible | 33 (75%)a | 16 (80%)ab | 29 (97%)b | .035c |
| Attention | 19 (43%)a | 2 (10%)b | 3 (10%)b | .001c |
F, female; M, male.
When there were significant between-group differences, groups with the same superscript in the same row did not differ from each other.
When there were significant between-group differences, groups with the same superscript in the same row did not differ from each other.
Significant differences were based on ANOVA for continuous variables and χ2 (or Fisher’s exact test for small cell sizes) for categorical variables.
When there were significant between-group differences, groups with the same superscript in the same row did not differ from each other.
Children often had >1 social function.
Behavioral Outcomes
The mean percentage reduction in problem behavior achieved through FCT treatment was >90% for all groups and not significantly different between the 3 service models (Table 2). However, the models that delivered services in the home showed slightly greater reductions in problem behavior compared with treatment at the regional clinics, possibly related to more difficulty generalizing treatment effects from clinic to home. These differences might have reached statistical significance if this pattern were maintained in larger samples with greater power to detect small differences in outcome. Both manding and task completion improved in groups 2 and 3, but the groups did not differ and comparable data were not available for group 1. Parent ratings of treatment acceptability were consistently high and did not differ across groups. The number of weekly visits needed to complete FA was similar across treatment groups, but group 1 needed a greater number of FCT visits compared with groups 2 and 3. This difference may have been caused by greater distractions during home visits, more extended testing of methods for maximizing treatment gains in group 1, or greater efficiency in achieving behavior targets in the more recent studies.
TABLE 2.
Behavioral Outcomes and Acceptance by Parents of FA and FCT Treatment via Different Service Delivery Models
| Variables | Group 1: In-Home Therapy (n = 44) | Group 2: Clinic Telehealth (n = 20) | Group 3: Home Telehealth (n = 30) | P |
|---|---|---|---|---|
| Percentage reduction in problem behavior | .074 | |||
| Mean (SD) | 95.76% (8.91) | 91.00% (13.66) | 97.27% (6.00) | |
| Range | 59.07%–100% | 47.40%–100% | 77.01%–100% | |
| Percentage increase in mands (appropriate requests) | N/A | .832 | ||
| Mean (SD) | 78.42% (25.53) | 76.67% (27.48) | ||
| Range | 20.5%–100% | 13.3%–100% | ||
| Percentage increase in task completion | N/A | .301 | ||
| Mean (SD) | 51.53% (30.89) | 61.15% (34.81) | ||
| Range | 13%–100% | 0.6%–100% | ||
| FA weekly visits | ||||
| Mean (SD) | 4.52 (1.57) | 5.30 (1.49) | 4.90 (1.92) | .219 |
| Range | 2–10 | 4–9 | 2–11 | |
| FCT treatment weekly visits | ||||
| Mean (SD) | 17.05 (7.99)a | 9.05 (3.58)b | 9.10 (5.37)b | <.001c |
| Range | 3–39 | 4–18 | 2–23 | |
| Acceptability ratings (Treatment Acceptability Rating Form–Revised; 1–7 scale) | ||||
| Mean (SD) | 6.55 (0.68) | 6.53 (0.61) | 6.25 (0.91) | .457 |
| Range | 5–7 | 5–7 | 4–7 |
ASD diagnosis was confounded with group, but a separate ANOVA based on only subjects with ASD produced similar results to the ANOVA based on the full sample.
When there were significant between-group differences, groups with the same superscript in the same row did not differ from each other.
When there were significant between-group differences, groups with the same superscript in the same row did not differ from each other.
Significant differences were based on ANOVAs; main effects for group are presented because there were no significant group × ID interactions.
Treatment Costs
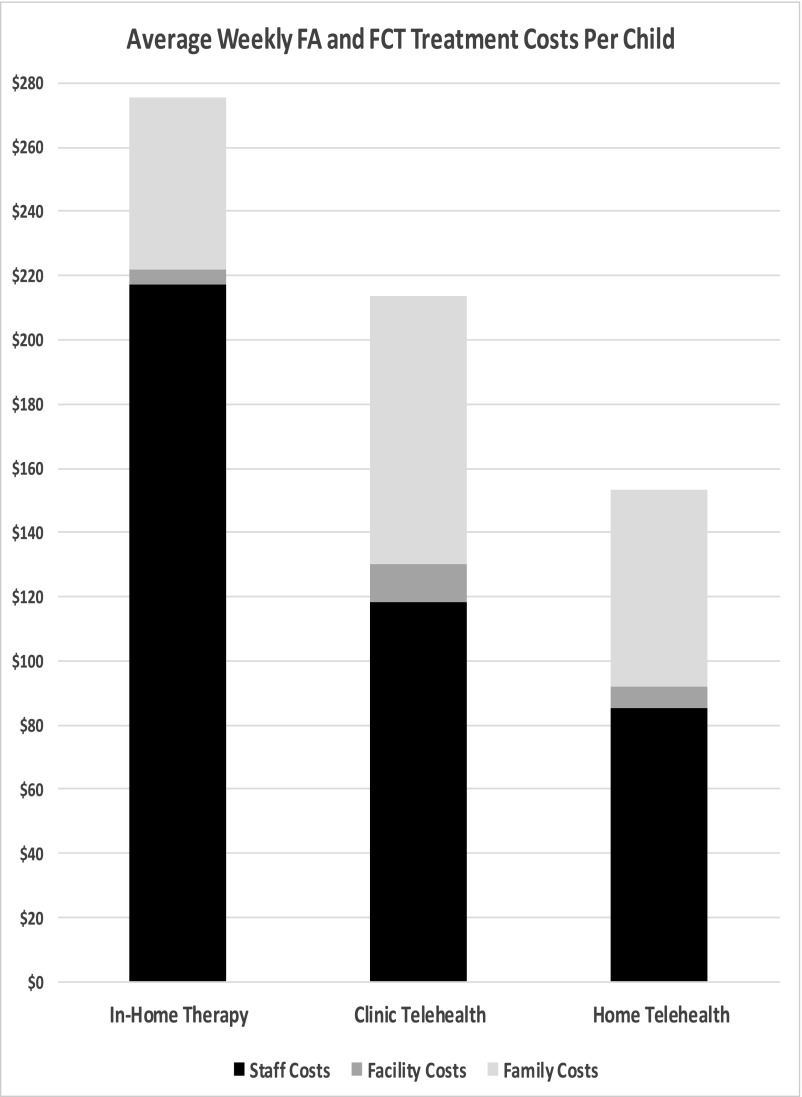
Based on analysis of the procedures and settings involved in providing FA and FCT under the 3 service models, we calculated the staff costs, facility costs, and family costs needed to implement these treatments. Figure 1 shows the relative expenses that contributed to the cost per child per week. Table 3 summarizes the total cost to complete FA and FCT under these delivery systems. Costs were based on the number of weekly visits needed to complete FA and FCT multiplied by the costs per child per week in each of the 3 models. Home telehealth was the least expensive model overall, though not significantly lower than clinic telehealth, primarily because of elimination of staff or parent travel expenses and the costs for the family navigator and additional facilities at the regional clinics. The slightly higher family costs in either of the telehealth models (compared with in-home therapy) were still small and were offset by more efficient use of expensive professional time in the telehealth models.
FIGURE 1.
Average weekly FA and FCT treatment costs per child.
TABLE 3.
Costs of Treatment With FA and FCT When Delivered via Different Service Models
| Variables | Group 1: In-Home Therapy (n = 44) | Group 2: Clinic Telehealth (n = 20) | Group 3: Home Telehealth (n = 30) | P |
|---|---|---|---|---|
| Staff costs | ||||
| Mean | $4687.86a | $1693.30b | $1190.00b | <.001c |
| (SD) | (1799.51) | (371.72) | (519.20) | |
| Facility costs | ||||
| Mean | $99.04a | $172.20b | $97.44a | <.001c |
| (SD) | (38.02) | (37.80) | (42.51) | |
| Family costs | ||||
| Mean | $1163.06a | $1202.96a | $858.20b | .002c |
| (SD) | (446.46) | (264.08) | (374.43) | |
| Total cost | ||||
| Mean total cost per child to complete treatment | $5949.97a | $3068.46b | $2145.64b | <.001c |
| (SD) | (2283.99) | (673.60) | (936.15) |
Sensitivity analyses based on 25%–50% higher or lower estimates of staff, facility, and family costs produced changes in total costs for each treatment, but the pattern of relative costs between groups remained similar.
When there were significant between-group differences, groups with the same superscript in the same row did not differ from each other.
When there were significant between-group differences, groups with the same superscript in the same row did not differ from each other.
Significant differences were based on ANOVA.
Discussion
This research demonstrates that parents can successfully use FA and FCT to treat moderate to severe behavior problems associated with ASD regardless of whether treatment is directed by behavior consultants in person or via remote video coaching. The results showed no statistically or clinically significant differences in behavioral outcomes that could be attributed to the service delivery methods. Treatment acceptability based on parent ratings was very high for all 3 groups, and discontinuation of treatment was infrequent for families in all groups. Overall costs for implementing treatment were lowest for home telehealth, but both telehealth models were significantly less costly than in-home therapy.
The current analyses focused only on direct treatment costs expended by clinic staff, treatment facilities, and families, without factoring in societal costs. The clinic telehealth model included salary costs for the family navigators at the regional clinics and family travel costs, whereas costs for behavioral consultants, supervising psychologists, and data coders remained the same across models. For the in-home consultants in the earlier studies, transportation costs (including mileage and salaries during trips) were substantial, and these costs made the in-home therapy model significantly more expensive than the telehealth models. In terms of family costs, additional equipment and Internet costs were included for in-home telehealth, although these expenses were covered by grant funds in the current study. Because time devoted to treatment by individual parents was not tracked, family cost analyses assumed similar time investments for parents in all groups. Although cost analyses for the clinic sites included expenses for equipment, existing teleconferencing equipment was used in the current research.
The findings reported by Suess et al14 demonstrated that parents are able to implement ABA procedures with acceptable fidelity even when a coach is not directly supervising them. Concerns can be raised about whether weekly ABA coaching sessions are frequent enough to produce optimal behavioral outcomes in children with ASD, but when parents are taught to use FCT strategies daily with their children, the intensity of treatment is actually >1 hour per week. This point has been emphasized in other ASD research supporting a similar intensity of direct intervention,23 but we were not able to obtain detailed records from families regarding treatment practice time occurring outside of telehealth sessions.
Potential limitations must be recognized when considering the findings from this study. Enrollment criteria were not identical in selecting participants, the groups were not randomly assigned, and an untreated control group was not included to test these service models. Although both of the telehealth models used gold standard diagnostic procedures to identify participants with ASD, the earlier in-home research was not limited to ASD. All 3 programs included children with significant behavior problems, but we did not use a fixed cutoff score on a measure of behavioral severity as an inclusion criterion. Intellectual abilities of children in the studies ranged from severe ID to above-average ability, and no IQ-based exclusion criteria were used. Although the proportion of children with ID was higher in group 1 than in groups 2 and 3, FCT was generally successful across IQ ranges, and behavioral outcomes were not significantly different between groups. Because the 3 treatment models were not implemented at the same time, it is possible that available services could have changed over time. Also, additional services may have been available for group 1 given the proximity to the Children’s Hospital. However, the fact that all 3 models achieved similar positive outcomes indicates that any differences in services or personnel did not prevent the treatment from achieving targeted goals for most children. Of course, it is critical to recognize that treatment of problem behavior is not sufficient on its own to meet the needs of children with ASD, who still need other health care and educational services. However, effective treatment of challenging behavior can remove a significant barrier to benefiting from therapies and skill acquisition programming.
Conclusions
This study represents an important step in evaluating the costs and efficiency of alternative models for delivering ABA treatment of challenging behavior. These findings highlight the importance of studying factors that influence the implementation and sustainability of different methods for delivering care in real-world settings.24 By reducing the cost of ABA treatment by nearly half through clinic-based telehealth and by almost two-thirds through home telehealth, these strategies fulfill the health care “triple aim” of enhancing care experiences, improving population health, and reducing costs of care.25 Because telehealth can provide research-based ABA treatment to any family with access to the Internet, barriers to providing access to ABA can be reduced, especially for rural and underserved families. There is a rapidly growing literature on the use of telehealth to deliver a range of ASD interventions,26–30 and future issues regarding the delivery of ABA services via telehealth will need to focus on when to provide services and at what intensity to deliver them in relation to other interventions. These timing and dose issues warrant careful study, as will issues such as the effects of ABA treatment on caregiver stress and parenting and the best ways to ensure generalization of children’s and parents’ newly learned skills. The results of these studies are crucial for informing future decisions about the optimal use of telehealth in delivering ABA services for children with autism.
Acknowledgments
We thank the research assistants and the staff of the University of Iowa Child Health Specialty Clinics for their invaluable contributions to these studies. We appreciate the assistance of Bridget Zimmerman and George Wehby with selected aspects of the data analysis. We are especially grateful to all of the families who have shared their lives with us.
Glossary
- ABA
applied behavior analysis
- ANOVA
analysis of variance
- ASD
autism spectrum disorder
- DD
developmental disability
- FA
functional analysis
- FCT
functional communication training
- ID
intellectual disability
Footnotes
Drs Lindgren and Wacker conceptualized and designed the study, oversaw data collection, analysis, and interpretation, and drafted the initial manuscript; Drs Suess and Schieltz contributed to the data collection and analysis and reviewed and revised drafts of the manuscript; Drs Pelzel and Kopelman contributed to the design of the study, coordinated study implementation and data collection, contributed to data analysis and interpretation, and reviewed and revised drafts of the manuscript; Mr Lee and Dr Romani contributed to data collection and analysis and reviewed drafts of the manuscript; Dr Waldron contributed to the design of the study, supervised staff providing support to families during study implementation and data collection at regional clinics, and provided critical review of the manuscript; and all authors approved the final manuscript as submitted.
FINANCIAL DISCLOSURE: The authors have indicated they have no financial relationships relevant to this article to disclose.
FUNDING: Supported by grants R40 MC22644 from the Maternal and Child Health Bureau of the Health Resources and Services Administration, R01 MH89607 from the National Institute of Mental Health of the National Institutes of Health, and R01 HD029402 from the National Institute of Child Health and Human Development of the National Institutes of Health. The authors have no other financial relationships relevant to this research to disclose. Funded by the National Institutes of Health (NIH).
POTENTIAL CONFLICT OF INTEREST: The authors have indicated they have no potential conflicts of interest to disclose.
References
- 1.Wong C, Odom SL, Hume K, et al. Evidence-Based Practices for Children, Youth, and Young Adults With Autism Spectrum Disorder. Chapel Hill, NC: The University of North Carolina, Frank Porter Graham Child Development Institute, Autism Evidence-Based Practice Review Group; 2014 [Google Scholar]
- 2.Lovaas OI. Behavioral treatment and normal educational and intellectual functioning in young autistic children. J Consult Clin Psychol. 1987;55(1):3–9 [DOI] [PubMed] [Google Scholar]
- 3.Koegel RL, Koegel LK. Generalized responsivity and pivotal behavior. In: Horner R, Koegel R, Dunlap G, eds. Generalization and Maintenance: Lifestyle Changes in Applied Settings. Baltimore, MD: Paul H. Brookes; 1988 [Google Scholar]
- 4.Dawson G, Rogers S, Munson J, et al. Randomized, controlled trial of an intervention for toddlers with autism: the Early Start Denver Model. Pediatrics. 2010;125(1). Available at: www.pediatrics.org/cgi/content/full/125/1/e17 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Wacker DP, Lee JF, Padilla Dalmau YC, et al. Conducting functional communication training via telehealth to reduce the problem behavior of young children with autism. J Dev Phys Disabil. 2013;25(1):35–48 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Carr EG, Durand VM. Reducing behavior problems through functional communication training. J Appl Behav Anal. 1985;18(2):111–126 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Tiger JH, Hanley GP, Bruzek J. Functional communication training: a review and practical guide. Behav Anal Pract. 2008;1(1):16–23 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Iwata BA, Dorsey MF, Slifer KJ, Bauman KE, Richman GS. Toward a functional analysis of self-injury. J Appl Behav Anal. 1994;27(2):197–209 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Durand VM, Carr EG. Self-injurious behavior: motivating conditions and guidelines for treatment. School Psych Rev. 1985;14:171–176 [Google Scholar]
- 10.Carr EG. Functional equivalence as a mechanism of response generalization. In: Horner R, Koegel R, Dunlap G, eds. Generalization and Maintenance: Lifestyle Changes in Applied Settings. Baltimore, MD: Paul H. Brookes; 1988 [Google Scholar]
- 11.Wacker DP, Lee JF, Dalmau YC, et al. Conducting functional analyses of problem behavior via telehealth. J Appl Behav Anal. 2013;46(1):31–46 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Wacker DP, Harding JW, Berg WK, et al. An evaluation of persistence of treatment effects during long-term treatment of destructive behavior. J Exp Anal Behav. 2011;96(2):261–282 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Wacker DP, Berg WK, Harding JW, Derby KM, Asmus JM, Healy A. Evaluation and long-term treatment of aberrant behavior displayed by young children with disabilities. J Dev Behav Pediatr. 1998;19(4):260–266 [DOI] [PubMed] [Google Scholar]
- 14.Suess AN, Romani PW, Wacker DP, et al. Evaluating the treatment fidelity of parents who conduct in-home functional communication training with coaching via telehealth. J Behav Educ. 2014;23:34–59 [Google Scholar]
- 15.Rutter M, Le Couteur A, Lord C. ADI-R: Autism Diagnostic Interview–Revised (ADI-R). Los Angeles, CA: Western Psychological Services; 2003 [Google Scholar]
- 16.Lord C, Rutter M, DiLavore P, Risi S. Autism Diagnostic Observation Schedule (ADOS) Manual. Los Angeles, CA: Western Psychological Services; 2001 [Google Scholar]
- 17.American Psychiatric Association Diagnostic and Statistical Manual of Mental Disorders. 4th ed. Washington, DC: American Psychiatric Association; 1994 [Google Scholar]
- 18.Harding JW, Wacker DP, Berg WK, Lee JF, Dolezal D. Conducting functional communication training in home settings: a case study and recommendations for practitioners. Behav Anal Pract. 2009;2(1):21–33 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Roane HS, Vollmer TR, Ringdahl JE, Marcus BA. Evaluation of a brief stimulus preference assessment. J Appl Behav Anal. 1998;31(4):605–620 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Reimers T, Wacker D, Cooper L. Evaluation of the acceptability of treatments for children’s behavioral difficulties: ratings by parents receiving services in an outpatient clinic. Child Fam Behav Ther. 1991;13(2):53–71 [Google Scholar]
- 21.Lee JF, Schieltz KM, Suess AN, et al. Guidelines for developing telehealth services and troubleshooting problems with telehealth technology when coaching parents to conduct functional analyses and functional communication training in their homes. Behav Anal Pract. 2014. 10.1007/s40617-014-0031-2 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Bureau of Labor Statistics Table B-3: average hourly and weekly earnings of all employees. December 2014. US Department of Labor. Available at: www.bls.gov/webapps/legacy/cesbtab3.htm. Accessed February 15, 2015
- 23.Vismara LA, Colombi C, Rogers SJ. Can one hour per week of therapy lead to lasting changes in young children with autism? Autism. 2009;13(1):93–115 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Proctor E, Silmere H, Raghavan R, et al. Outcomes for implementation research: conceptual distinctions, measurement challenges, and research agenda. Adm Policy Ment Health. 2011;38(2):65–76 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Berwick DM, Nolan TW, Whittington J. The triple aim: care, health, and cost. Health Aff (Millwood). 2008;27(3):759–769 [DOI] [PubMed] [Google Scholar]
- 26.Vismara LA, Young GS, Stahmer AC, Griffith EM, Rogers SJ. Dissemination of evidence-based practice: can we train therapists from a distance? J Autism Dev Disord. 2009;39(12):1636–1651 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Vismara LA, Young GS, Rogers SJ. Telehealth for expanding the reach of early autism training to parents. Autism Res Treat. 2012;2012:121878. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Wainer AL, Ingersoll BR. Increasing access to an ASD imitation intervention via a telehealth parent training program. J Autism Dev Disord. 2015;45(12):3877–3890 [DOI] [PubMed] [Google Scholar]
- 29.Machalicek W, O’Reilly MF, Rispoli M, et al. Training teachers to assess the challenging behaviors of students with autism using video tele-conferencing. Educ Train Autism Dev Disabil. 2010;45(2):203–215 [Google Scholar]
- 30.Heitzman-Powell LS, Buzhardt J, Rusinko L, Miller T. Formative evaluation of an ABA outreach program for parents of children with autism in remote areas. Focus Autism Other Dev Disabil. 2013;20:1–16 [Google Scholar]