Abstract
Background:
Treatment of forearm fracture nonunion is challenging. Several surgical techniques for the treatment of forearm nonunion have been reported.
Objectives:
The aim of this prospective study was to evaluate the effects of the radial forearm bone graft technique in cases with forearm nonunion.
Patients and Methods:
We treated 7 patients with forearm nonunions via radial forearm bone flap and internal plate fixation. On the preoperative examination and last follow-up, the quick disabilities of the arm, shoulder, and hand (Q-DASH) score, elbow, forearm and wrist arches of motion and grip force were measured. At the final follow-up, radiographic union and patient satisfaction and return to work were assessed.
Results:
The mean follow-up duration was 34 ± 23 months. The Q-DASH scores improved from 70 ± 6 points preoperatively to 13 ± 15 points at final follow-up (P < 0.01). The preopetative range of motion (ROM) was 101 ± 26 degrees; whereas the final forearm ROM was 140 ± 17 (P = 0.01). All nonunions united uneventfully (range 3-6 months). At the last follow-up, the grip force was 83% of uninjured extremity and all patients were satisfied with the outcome of the operation.
Conclusions:
Radial forearm bone flap is a safe, useful and novel technique in cases with forearm nonunion.
Keywords: Forearm, Nonunion, Microsurgery
1. Background
By application of compression plating, an expected union rate of forearm fractures has been greater than 95% (1, 2). However, forearm nonunion is a real challenge for both the patient and the surgeon. Minimal changes in length and alignment, or instability at nonunion site of radius or ulna may distort complex normal relationship at proximal and distal radioulnar joints or along the interosseous membrane and result in a great loss of the forearm range of motion and force and therefore functional impairment (3). Treating these nonunions becomes even more complicated due to the presence of bone necrosis, segmental bone loss, possible concomitant infection, and scar adhesion of the soft tissues (4, 5). An effective surgical intervention in treatment of forearm nonunions should therefore, meet two criteria: first, it should provide a biological environment that promotes bone healing; second, it should provide adequate stability for the fracture at the same time (6).
Regarding several factors such as the size of the bone defect, type of nonunion, the condition of soft tissue envelope and the presence of infection, currently different methods can be used for treatment of forearm nonunion. These treatment options include: open reduction and internal fixation (ORIF) with cancellous bone graft (7), intercalary corticocancellous iliac graft (8-10), nonvascularized fibular strut intercalary autograft (11), free vascularized fibular graft (12, 13), distraction-compression osteogenesis by the Ilizarov method (14) and vascularized bone graft from the ulna (15).
Mullett et al. described the radial forearm bone graft technique for treatment of nonunion of the distal humerus and suggested that this technique can be used in proximal forearm nonunions as well (16).
2. Objectives
The aim of this prospective study was to evaluate the medium-term effects of the radial forearm bone graft technique in cases with forearm nonunion.
3. Patients and Methods
3.1. Patients
After approval of the institutional review board of our center and obtaining a written informed consent from the patients, we conducted the study between October 2007 and December 2013. The study included seven cases of forearm nonunion (5 females and 2 males) with the mean age of 41.3 years (range: 20 - 72 years). Nonunions affected both bones in 4 cases, only ulna in 2 cases and only radius in one case. The initial fracture was isolated radius fracture in one forearm and both radius and ulna fracture in 6 forearms. All fractures were closed except one radius and ulna fracture classified as Gustilo type IIIA; an exceptional case (case 6) presented with infected nonunion by a draining fistula at the site of ulna fracture. Initial treatment consisted of internal fixation with plates and screws in all patients. Two of them underwent a second operation to remove the plates. Neurovascular examination was intact in all cases. Details are presented in Table 1.
Table 1. Patients’ Dataa.
| Variables | Case 1 | Case 2 | Case 3 | Case 4 | Case 5 | Case 6 | Case 7 |
|---|---|---|---|---|---|---|---|
| Age, y | 29 | 52 | 72 | 20 | 64 | 24 | 28 |
| Gender | F | F | F | F | M | M | F |
| Mechanism of injury | MVA | MVA | Falling | Falling | Falling | Falling | MVA |
| Primary fracture | RU | RU | RU | RU | RU | RU | R |
| Close/ open fracture | Close | Close | Close | Close | Close | Open | Close |
| Nonunion location | Um / Rm | Um / Rm | Up / Rp | Um /Rm | Ud /Rm | Um /Rm | Rm |
| Occupation | Teacher | House-keeper | - | Clerk | Farmer | Laborer | Clerk |
| Accident to RFBF operation time, m | 15 | 12 | 54 | 66 | 10 | 12 | 12 |
| Operations | 1 - ORIF by Plate, 2-: U: RFBF, R: Re-ORIF + IG, 3-R: PIBF, 4-plate removal | 1- ORIF by plate, 2- U: RFBF | 1- ORIF by plate, 2- plate removal (→Both bone NU), 3- U: RFBF, R: no procedure | 1- ORIF by plate, 2- plate removal (→ U NU), 3- U: RFBF | 1-ORIF by plate, 2- R: RFBF , U: PIBF | 1- ORIF by plate, 2- U: PIBF, 3- R: RFBF, 4- plate removal | 1- ORIF by plate, 2- R: RFBF, 3- Tendon transfer for FPL |
| Union time | 3 | 6 | 4 | 3 | 3 | 4.5 | 3 |
| Preop. Elbow Flex./ext., deg | 145 | 145 | 105 | 145 | 115 | 145 | 145 |
| Postop. Elbow Flex./ext., deg | 145 | 145 | 100 | 145 | 120 | 145 | 145 |
| Preop. Forearm sup./pron., deg | 145 | 100 | 90 | 130 | 80 | 95 | 70 |
| Postop. Forearm sup./pron., deg | 160 | 145 | 110 | 160 | 130 | 145 | 135 |
| Preop. Wrist Flex./ext., deg | 135 | 85 | 95 | 115 | 60 | 95 | 125 |
| Postop. Wrist Flex./ext., deg | 160 | 95 | 95 | 160 | 105 | 135 | 105 |
| Interval between injury and RFBF, mo | 15 | 12 | 54 | 66 | 10 | 12 | 12 |
| Follow-up, mo | 80 | 33 | 32 | 28 | 42 | 18 | 7 |
| Injured/normal grip force, kg | 32 /36 | 24 / 28 | 12 /18 | 20 / 24 | 25 / 32 | 42 / 42 | 23 / 30 |
| Preop./ Final quick-DASH score | 66.6 /9.1 | 75 / 2.3 | 80 / 35 | 61.4/ 11.4 | 68.2 / 0 | 70.4 / 0 | 70.4 /34.1 |
| Return to work | Yes | Yes | Disabled due to medical comorbidity | Yes | Yes | Yes | No |
| General satisfaction | Yes | Yes | Yes | Yes | Yes | Yes | Yes |
| Complication | None | Hypoesthesia in SRNT | None | Radius pain (7 m) | None | None | Hypoesthesia in SRNT |
aAbbreviations: DASH, disabilities of the arm, shoulder and hand; Flex, flexion; FPL, flexor pollicis longus; IG, iliac graft; MVA, motor vehicle accident; NU, nonunion; PIBF, posterior interosseous bone flap; Preop, postoperative, Preop, preoperative; R, radius; RFBF, radial forearm bone flap; Rm, middle third of radius; Rp, proximal third of radius; RU, radioulna; SRNT, superficial radial nerve area; U, ulna; Ud, distal third of ulna; Um, middle third of ulna; Up, proximal third of ulna.
The main objective presentations were disability in hand use (7 cases), limited or painful forearm rotation (5 cases), nonunion site motion (4 cases) and tenderness at the nonunion site (4 cases). Three older (> 50 years old) patients reported no pain but frank instability. The average time between injury and referral was 26 (range: 10 - 66) months. All nonunions were atrophic.
3.2. Surgical Technique
All operations were done by the first author. The Allen test was done preoperatively to guarantee sufficient hand circulation from the ulnar artery. Nonunion site of the radius or ulna was exposed by volar Henry and dorsal approaches, respectively. In case number 6 which presented an episode of acute on chronic infection, irrigation and debridement was also performed via a wide exposure. Except for case 6, in which resection of the infected bone was done circumferentially, the sclerotic bones were excised from half of the bone surface area at nonunion site until normal bone could be visualized. The other side of the nonunion site was not manipulated to maintain the length. The medulla was opened by drilling. If the existing previous plate and screws were stable and sufficient, they were left (case 7 by previous LCDCP); but if the hardware was insufficient, broken or absent, the nonunion site was bridged by a new Locking Plate (LCP) and held by bone clamp to ensure the proper length and the rotation of bone. Previous plating holes of the bones were good guides for the length and rotation when the bones were completely unstable.
A regional antegrade Radial Forearm Bone Flap (RFBF) was then harvested by the same Henry approach for radius and by an additional Henry approach for ulna nonunions. Briefly, in the plane between Flexor Carpi Radialis (FCR) and brachioradialis, radial artery and its branches to the radius bone were identified. At least 1 centimeter proximal to the radiocarpal joint, the desired length of bone (equal to or slightly greater than the length of the defect) was marked on the radial part of volar side of distal radius metaphysis. Meticulous removal of the graft was easier by making several holes using a small smooth k-wire that was drilled in the perimeter of the graft. Reducing the temperature of the drilling pin and surrounding bone by continuous irrigation could prevent iatrogenic burning of delicate tissues. The width and thickness of the graft were selected on the basis of recipient site, maximally one third of radius width for the former and 1 centimeter for the latter. A thin and narrow osteotome was used to remove the vascularized bone graft with the beveled end in association with its overlying soft tissue pedicle which contained periosteum, some parts of brachioradialis insertion, intact sheath of radial artery and veins and their bone branches. The radial artery and vein was ligated distal to the graft and then dissected proximally as needed to reach the recipient site without acute angulation (Figures 1 and 2).
Figure 1. Intraoperative pictures of case 7. The pedicled radial bone forearm flap was harvested and released proximally to rotate and reach the defect at the nonunion site of the radius (A). The graft was fixed under the previous stable LCDCP by two screws (B). The donor site was obvious at the distal end of the incision. The pedicle is depicted by arrows.
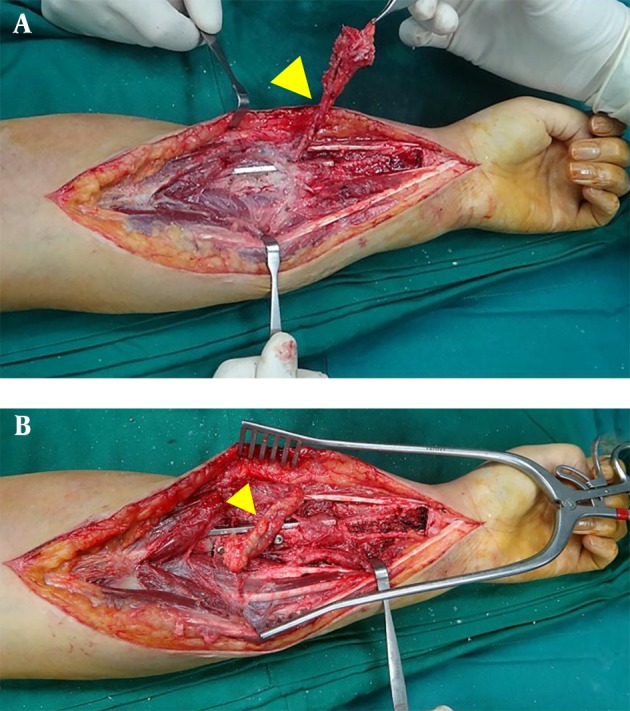
Figure 2. The Recipient Site of the Ulna in Another Case (Case 1) and the Matched Harvested Pedicled Radial Bone Flap Before Fixation.
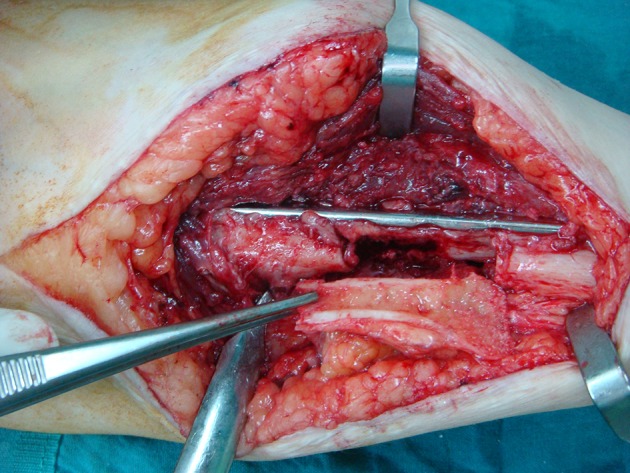
For nonunions of the radius the graft and its pedicle were rotated backwards on the defect in the same exposure and for ulna nonunions the graft wass transferred beneath the skin around the radial side of the forearm from the volar Henry incision to the dorsal incision.
After placing the bone flap, a locking plate was fixed to the bone with at least 2 screws at each side. The bone flap was fixed either under the plate (4 cases) or by one or two screws (3 cases). Only in one case, the RFBF was associated with a concomitant iliac graft.
3.3. Postoperative Rehabilitation Program
A splint was applied to the forearm for 1 week. Heavy activities were advised to be avoided for 6 weeks. IV antibiotic (cefazolin 1 g/6 h) was given for 24 hours. In one case with acute infection, a gentamicin pad was applied at the time of operation and IV antibiotic continued for 48 hours then orally for one week.
3.4. Assessments
At the preoperative examination and last follow-up, the following assessments were conducted. The elbow, forearm and wrist range of motion were measured by a goniometer. All of the patients were assessed with quick disabilities of the arm, shoulder and hand (quick DASH) score (17) and grip force measured using a Jamar hydraulic pinch gauge (Patterson Medical, Bolingbrook, IL, USA). All patients were followed clinically and radiologically by anteroposterior, lateral, and 2 oblique views every 6 weeks until radiographic union could be detected and then at the final follow-up. We defined radiographic union as trabeculation of at least 3 out of 4 cortices detected on two orthogonal radiographic views.
3.5. Statistical Analysis
Statistical analysis was performed using descriptive statistics, t-test and chi-square test with SPSS version 22 (SPSS Inc., Chicago, Illinois, USA).
4. Results
Regional antegrade RFBF was performed for nonunion of 4 ulnar and 3 radial bones. Donor site of the flap on the radius was filled by cortico-cancellous bone graft from the iliac bone only in the first three patients. The average length of the graft was 39 (range: 30- 45) millimeters. The mean duration of follow-up was 34 (range: 7 - 80) months. All of nonunions united in an average time of 3.8 (range: 3 - 6) months (Figure 3).
Figure 3. Preoperative anteroposterior (A) and lateral (B) X-rays of case 7 of a nonunion of the previous isolated radius fracture 12 months ago. Three months after radial fixation, the bone flap united. Anteroposterior (C), lateral (D) X-rays at the final follow-up (7 months after surgery) demonstrated complete healing of both fracture site and donor site.
The mean loss of forearm supination and pronation decreased from 26° (range: 0 - 45°) and 22° (0 - 40°), preoperatively, to 6° (range: 0 - 25°) and 7° degrees (range: 0 - 20°), postoperatively. Also, the average of wrist flexion and extension loss changed from preoperative values of 19° (range: 0 - 50°) and 24° (range: 10 - 35°) to 9° (0 - 25°) and 11⁰ (0 - 25°), postoperatively. The elbow ROM was full preoperatively except for two cases; both had nearly the same preoperative flexion contracture in the final follow-up.
The mean of Quick DASH score demonstrated a clinically significant decrease from 70 (range 61 - 80) preoperatively to 13 (range 0 - 35) at final visit (P < 0.01). At final follow-up, postoperative grip strength in the affected hand was on average 25.42 kg (range: 12 to 42) and in unaffected hand was 30 kg (range: 18 to 42). Five patients returned to their previous jobs. All patients were satisfied with the surgical results. Results are presented in Table 1.
4.1. Complications
Two cases complained of hypoesthesia in the area of the superficial radial nerve that resolved in one of them after 5 months. In another case there was transient pain at the donor site of the radius for 7 months (Table 1).
5. Discussion
Restoration of the exact anatomy of the ulna and radius and their three dimensional relationship and also improving the biological state at the nonunion site are the principals which make the treatment of forearm nonunion difficult and challenging (7, 11, 18, 19). Infection and bone defects, because of primary segmental bone loss or intraoperative removal of bone sclerosis at the nonunion site and scarred soft tissues, further complicate treatment (5).
Nicoll described a technique of bridging gaps (up to 3 inches long) in long bones by the use of solid blocks of cancellous graft combined with internal fixation and successfully treated 23 cases including 14 forearm nonunions (7). Although acceptable outcome has been accomplished by the Nicoll’s method or its modifications (8, 9, 20), a nonvasculrizad graft would not be in general, an appropriate option for associated infection, severe soft-tissue damage, extensive scar tissue, and long (> 6 cm) bone defects (8, 9, 21, 22). Several techniques other than Nikoll’s have been introduced either to fulfill its shortcomings or to solve the problem inherent to other possible approaches. Faldini et al. found full union and acceptable functional outcome with no complication in 20 aseptic nonunions treated by a metal plate and fibular intercalary autograft in long-term follow-up (11). In contrast, fibula graft harvesting and grafting could result in additional morbidity in other parts of the body (23). The results of application of bone morphogenic proteins to treat nonunion have been uncertain and these products do not work reliably in atrophic or infected nonunions (16, 24).
Theoretically, it seems that none of the above-mentioned methods could solve the problem of conventional bone grafting to treat infected nonunion or those with a large bone defect; possibly because the surrounding soft tissue cannot provide adequate vasculature for graft incorporation and, even if successful, results only in slow revascularization of the dead graft by creeping substitution (12). Conversely, Prasarn et al. (5) reported successful treatment in 15 patients with infected nonunions of the diaphysis of the radius or ulna by a protocol that combines aggressive surgical debridements with definitive fixation after 7 - 14 days, tri-cortical iliac crest bone grafting for segmental defects, leaving wounds open to heal by secondary intention, 6 weeks of culture-specific intravenous antibiotics, and early active range of motion exercises 5. Bone transport by Ilizarov or other types of external fixators have provided alternatives for the reconstruction of composite skeletal and soft-tissue defects and infected nonunion; nonetheless, such procedures are complex and lengthy and have been associated with many difficulties for patients (14, 25-27). Another option is vascularized bone grafts, in which viable bone (osteocytes in the graft survive) is transferred; which is capable of participating in the healing process using a mechanism similar to fracture union rather than bone graft incorporation. Therefore, more rapid bone union can be obtained irrespective of the length of the graft (28). The vascularized bone graft can transport the immune system agents and antibiotics directly to the site of infected nonunion, therefore it could theoretically increase the possibility of treating infection efficiently (22). The most frequently applied vascularized bone graft for treating infected nonunion of forearm or those with large defects have been the free vascularized fibula which seems to be the final option to obviate these obstacles to union. Reasonable outcomes have been gained by this flap (13, 28). Free vascularized fibula harvest is technically a highly demanding and time-consuming procedure and requires microsurgical anastomosis and bears a risk of related complications.
The pedicled regional vascularized bone flap seems to be a good approach and has advantages of the vascularized bone graft in one hand and does not have the shortcomings of other approaches such as the need for difficult microsurgical procedures, disturbing function of other parts of the body or complex and lengthy treatment by an external fixator (15, 16). These types of bone grafts have been successfully (29) used in the upper extremity for scaphoid nonunion. The radial forearm bone flap has been used in a retrograde fashion to fill osseous defects of the hand (30, 31). However, Mullett et al. applied it first in the RFBF in an antegrade fashion for 5 recalcitrant nonunion of the distal humerus (16). All cases had a history of infection and in one of them acute infection was present. Mullett et al. (16) could even harvest a 60 mm length by 10 mm width graft. They suggested that this flap could be harvested as an osteocutaneous flap if necessary. Union was gained in all of their cases with an average time of 17.2 months (range 7 - 23 months) (16) without any significant complication. On the basis of the same concept, we followed 9 cases of forearm nonunion treated by Posterior Interosseous Bone Flap (PIBF) for an average of 21 months. Posterior interosseous bone flap was harvested from the distal third of ulna. The average length of the bone graft was 42.8 mm (range 35 - 55 mm). None of the cases had extensive soft tissue damage or infection. All fractures united uneventfully during 3 months.
In the present study, only half of the area at the nonunion site was excised to prevent shortening of radius or ulna. We relied on vascularized bone graft to bridge the nonunion site. This study demonstrated clinically significant improvement in forearm rotation (supination, 20°; pronation, 15°), wrist flexion and extension (flexion: 9°; extension: 14°) and the Quick DASH score (preoperative: 70; postoperative: 13) when using antegrade RFBF for forearm nonunion. Final union of all 7 cases including the infected one by a mean duration of 3 months shows that RFBF as PIBF could be an effective, less complex and more biologic method for treating forearm nonunion. Notwithstanding pain, hyposthesia or both at donor site in 3 cases was transient in 2 of them, and there were no major complications like vascular compromise, nerve injury, or infection. Mullet et al. harvested a graft with a length of 60 mm (16). The fear of the iatrogenic fracture at donor site may be a cause for a shorter graft; in our cases average graft length was 39mm - 45mm. We discontinued grafting the donor site after 3 patients; We noticed that this pedicle graft can be used in nonunion of the proximal, middle and distal third of the ulna and also middle and proximal third of the radius. It may be possible to do harvest RFBF and PIBF simultaneously or in staged operations for treating nonunion in both bones (Case: 1, 5, and 6).
Insignificant morbidity of donor site, reasonable time of procedure, providing the best biological and mechanical potentials, use of regional anesthesia instead of general anesthesia, and absence of the need for complex microsurgical operations render regional pedicled bone flaps like RFBF an acceptable and interesting method for treating forearm nonunion, even infected ones.
Acknowledgments
The authors would like to thank the residents and staff of Shariati Hospital in Tehran, Iran.
Footnotes
Authors’ Contribution:Reza Shahryar Kamrani: the main surgeon, gathering data, supervise the project and article writing. Amir Reza Farhoud: aiding some operations, following patients, gathering data and article writing. Mohammad Hossein Nabian: article preparation and data analysis. Leila Farhadi: aiding operations, gathering data.
References
- 1.Chapman MW, Gordon JE, Zissimos AG. Compression-plate fixation of acute fractures of the diaphyses of the radius and ulna. J Bone Joint Surg. 1989;71(2):159–69. [PubMed] [Google Scholar]
- 2.Anderson LD, Sisk D, Tooms RE, Park WI. Compression-plate fixation in acute diaphyseal fractures of the radius and ulna. J Bone Joint Surg Am. 1975;57(3):287–97. [PubMed] [Google Scholar]
- 3.Moss JP, Bynum DK. Diaphyseal fractures of the radius and ulna in adults. Hand Clin. 2007;23(2):143–51. doi: 10.1016/j.hcl.2007.03.002. [DOI] [PubMed] [Google Scholar]
- 4.Ring D, Allende C, Jafarnia K, Allende BT, Jupiter JB. Ununited diaphyseal forearm fractures with segmental defects: plate fixation and autogenous cancellous bone-grafting. J Bone Joint Surg Am. 2004;86-A(11):2440–5. [PubMed] [Google Scholar]
- 5.Prasarn ML, Ouellette EA, Miller DR. Infected nonunions of diaphyseal fractures of the forearm. Arch Orthop Trauma Surg. 2010;130(7):867–73. doi: 10.1007/s00402-009-1016-4. [DOI] [PubMed] [Google Scholar]
- 6.Richard MJ, Ruch DS, Aldridge JM. Malunions and nonunions of the forearm. Hand Clin. 2007;23(2):235–43. doi: 10.1016/j.hcl.2007.02.005. [DOI] [PubMed] [Google Scholar]
- 7.Nicoll EA. The treatment of gaps in long bones by cancellous insert grafts. J Bone Joint Surg Br. 1956;38-B(1):70–82. doi: 10.1302/0301-620X.38B1.70. [DOI] [PubMed] [Google Scholar]
- 8.Davey PA, Simonis RB. Modification of the Nicoll bone-grafting technique for nonunion of the radius and/or ulna. J Bone Joint Surg. 2002;84(1):30–3. doi: 10.1302/0301-620x.84b1.11799. [DOI] [PubMed] [Google Scholar]
- 9.dos Reis FB, Faloppa F, Fernandes HJA, Albertoni WM, Stahel PF. Annals of Surgical Innovation and Research. Ann Surg Innov Res. 2009;3:5. doi: 10.1186/1750-1164-3-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Barbieri C, Mazzer N, Aranda C, Deopinto M. Use of a bone block graft from the iliac crest with rigid fixation to correct diaphyseal defects of the radius and ulna. J Hand Surg J Br Soc Surg Hand. 1997;22(3):395–401. doi: 10.1016/s0266-7681(97)80411-1. [DOI] [PubMed] [Google Scholar]
- 11.Faldini C, Pagkrati S, Nanni M, Menachem S, Giannini S. Aseptic forearm nonunions treated by plate and opposite fibular autograft strut. Clin Orthop Relat Res. 2009;467(8):2125–34. doi: 10.1007/s11999-009-0827-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Safoury Y. Free vascularized fibula for the treatment of traumatic bone defects and nonunion of the forearm bones. J Hand Surg Br. 2005;30(1):67–72. doi: 10.1016/j.jhsb.2004.09.007. [DOI] [PubMed] [Google Scholar]
- 13.Jupiter JB, Gerhard HJ, Guerrero J, Nunley JA, Levin LS. Treatment of Segmental Defects of the Radius with Use of the Vascularized Osteoseptocutaneous Fibular Autogenous Graft*. J Bone Joint Surg. 1997;79(4):542–50. doi: 10.2106/00004623-199704000-00009. [DOI] [PubMed] [Google Scholar]
- 14.Hani EM, Elalfi B, Wasfi K. Functional outcome following treatment of segmental skeletal defects of the forearm bones by Ilizarov application. Acta Orthopaedica Belgica. 2005;71:157–62. [PubMed] [Google Scholar]
- 15.Kamrani RS, Mehrpour SR, Sorbi R, Aghamirsalim M, Farhadi L. Treatment of nonunion of the forearm bones with posterior interosseous bone flap. J Orthop Sci. 2013;18(4):563–8. doi: 10.1007/s00776-013-0395-0. [DOI] [PubMed] [Google Scholar]
- 16.Mullett H, Hausman M, Zaidemberg C. Recalcitrant distal humeral and proximal forearm nonunion: salvage using an extended pedicled radial forearm osseous flap. J Trauma. 2008;64(4):E60–4. doi: 10.1097/01.ta.0000229713.56091.5b. [DOI] [PubMed] [Google Scholar]
- 17.The Disabilities of the Arm, Shoulder and Hand Score (Quick Dash). Available from: http://old.sbmu.ac.ir/SiteDirectory/Orthopedic%20Research%20Center/Pages/asamiketab.aspx.
- 18.Schemitsch EH, Richards RR. The effect of malunion on functional outcome after plate fixation of fractures of both bones of the forearm in adults. J Bone Joint Surg Am. 1992;74(7):1068–78. [PubMed] [Google Scholar]
- 19.Hong G, Cong-Feng L, Hui-Peng S, Cun-Yi F, Bing-Fang Z. Treatment of diaphyseal forearm nonunions with interlocking intramedullary nails. Clin Orthop Relat Res. 2006;450:186–92. doi: 10.1097/01.blo.0000214444.87645.75. [DOI] [PubMed] [Google Scholar]
- 20.Gupta DK, Kumar G. Gap nonunion of forearm bones treated by modified Nicoll's technique. Indian J Orthop. 2010;44(1):84–8. doi: 10.4103/0019-5413.58611. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Grace TG, Eversmann WW. The management of segmental bone loss associated with forearm fractures. J Bone Joint Surg. 1980;62(7):1150–5. [PubMed] [Google Scholar]
- 22.Saint-Cyr M, Farkas J, Gupta A. Double-barrel free fibula flap for treatment of infected nonunion of both forearm bones. J Reconstruct Microsurg. 2008;24(8):583–7. doi: 10.1055/s-0028-1090603. [DOI] [PubMed] [Google Scholar]
- 23.Younger EM, Chapman MW. Morbidity at Bone Graft Donor Sites. J Orthopaed Trauma. 1989;3(3):192–5. doi: 10.1097/00005131-198909000-00002. [DOI] [PubMed] [Google Scholar]
- 24.Garrison KR, Shemilt I, Donell S, Ryder JJ, Mugford M, Harvey I, et al. Bone morphogenetic protein (BMP) for fracture healing in adults. Cochrane Database Sys Rev. 2010;(6):CD006950. doi: 10.1002/14651858.CD006950.pub2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Wood MB. Free vascularized bone transfers for nonunions, segmental gaps, and following tumor resection. Orthopedics. 1986;9(6):810–6. doi: 10.3928/0147-7447-19860601-07. [DOI] [PubMed] [Google Scholar]
- 26.Orzechowski W, Morasiewicz L, Dragan S, Krawczyk A, Kulej M, Mazur T. Treatment of non-union of the forearm using distraction-compression osteogenesis. Ortopedia Traumatologia Rehabilitacja. 2006;9(4):357–65. [PubMed] [Google Scholar]
- 27.Liu T, Liu Z, Ling L, Zhang X. Infected forearm nonunion treated by bone transport after debridement. BMC Musculoskelet Disord. 2013;14(1):273. doi: 10.1186/1471-2474-14-273. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Malizos KN, Beris AE, Xenakis TA, Korobilias AB, Soucacos PN. Free vascularized fibular graft: A versatile graft for reconstruction of large skeletal defects and revascularization of necrotic bone. Microsurgery. 1992;13(4):182–7. doi: 10.1002/micr.1920130407. [DOI] [PubMed] [Google Scholar]
- 29.Malizos KN, Dailiana ZH, Innocenti M, Mathoulin CL, Mattar R, Sauerbier M. Vascularized bone grafts for upper limb reconstruction: defects at the distal radius, wrist, and hand. J Hand Surg . 2010;35(10):1710–8. doi: 10.1016/j.jhsa.2010.08.006. [DOI] [PubMed] [Google Scholar]
- 30.Matev I. The osteocutaneous pedicle forearm flap. J Hand Surg J Br Soc Surg Hand. 1985;10(2):179–82. doi: 10.1016/0266-7681(85)90010-5. [DOI] [PubMed] [Google Scholar]
- 31.Cormack GC, Duncan M, Lamberty G. The blood supply of the bone component of the compound osteo-cutaneous radial artery forearm flap—an anatomical study. Br J Plastic Surg. 1986;39(2):173–5. doi: 10.1016/0007-1226(86)90077-9. [DOI] [PubMed] [Google Scholar]



