Abstract
Background:
The current approach in stab wounds of the anterior abdominal wall is still unclear.
Objectives:
The goal of this study was to evaluate serial clinical examinations of patients with abdominal wall stab wounds referred to Poursina Hospital in Rasht.
Patients and Methods:
In a cross sectional study, 100 cases with stab wounds to the anterior abdominal wall were examined serially (admission time, 4, 8, 12, and 24 hours) after wound exploration. Serial hemoglobin test was performed every 8 hours. Laparotomy was performed in cases who were not hemodynamically stable or who showed symptoms of peritonitis. The results were analyzed with SPSS software version 21.
Results:
Ninety-one men (91%) and 9 women (9%) with mean age of 27 ± 10.7 years were included. Coexisting injuries were prevalent in 12 cases. The duration of hospitalization was 1 day in 31%, 2 days in 30%, 3 - 4 days in 32% and more than 5 days in 7%. Late laparotomy was performed 12 hours after admission in 8% of patients due to peritonitis. There was visceral damage in these cases. No mortality occurred. The cost and duration of hospitalization was significantly higher in cases with coexisting injuries and those who underwent laparotomy.
Conclusions:
It seems serial clinical examinations are safe and decrease the cost and duration of hospitalization in stable patients with anterior abdominal wall stab wounds.
Keywords: Abdominal Wall; Wounds, Stab; Clinical Examination
1. Background
Trauma is the fourth leading cause of death in Iran and the most frequent cause of death among the young population (1, 2). Nowadays, the burden of severe economic pressure and rapid social change has led to an increase in social conflict and violent crimes resulting in blunt or penetrating trauma (1-3).
The major approach to blunt trauma is based on non-invasive diagnostic methods such as computerized tomography (CT scan) and sonography (4, 5). Unlike blunt abdominal injuries, the traditional approach to penetrating abdominal injuries has been wound exploration and laparotomy (5).
Sometimes laparotomy is performed unnecessarily and these unnecessary laparotomies could have associated morbidities such as incisional hernia, bowel obstruction and other complications (6). The high rate of unnecessary laparotomies (38% - 40%) is due to the fact that many surgeons still adhere to the traditional mandatory laparotomy concept. These surgeries extend the duration of hospitalization and increase hospital spending (7-9).
In developing countries with limited health care resources, avoiding unnecessary laparotomies may translate to significant hospital savings. Nowadays, due to the high rate of unnecessary laparotomies and morbidities, the treatment of penetrating abdominal injuries has been changing (10, 11).
In penetrating trauma management, patients with the stab wound tract ending before violation of their anterior abdominal fascia, are safe for discharge. However, if the anterior abdominal fascia is penetrated, hemodynamically unstable cases, and patients with peritoneal irritation should undergo immediate laparotomy. The proper approach still remains controversial for other cases with hemodynamic stability and no signs of peritonitis. There are three main approaches in these circumstances namely: Diagnostic peritoneal lavage (DPL), CT scan, and serial clinical examinations (9-11).
There are several studies which have declared that, due to the iatrogenic injuries to internal organs, DPL may result in false positive or false negative reports (12, 13). On the other hand, the use of CT scan and serial clinical examinations can increase the likelihood of detecting significant intra-abdominal injuries before the abdomen is explored and may lower the laparotomy rate (14, 15).
2. Objectives
The goal of this study was to evaluate serial clinical examinations as the first step in the approach to cases with anterior abdominal wall stab wounds. This method could be a safe approach to decrease the morbidity and mortality of unnecessary laparotomies and decrease the hospital spending and hospital stay.
3. Patients and Methods
In this cross-sectional study, all patients with stab wounds to the anterior abdominal wall that had passed through the abdominal fascia, referring to the Poursina Hospital in Rasht, from September 2009 to September 2012, were studied. Patients who were not hemodynamically stable on arrival, those with peritonitis, abdominal pain, or tenderness, bloody rectal clots, and bloody discharges in nasogastric tube (NGT) were excluded from this study. Wound examinations were performed under general anesthesia in the emergency room, and patients were excluded if wound examination revealed that the knife had not penetrated the abdominal cavity. A checklist including demographic features (age, gender), systolic blood pressure, heart rate, clinical findings (on arrival, 4, 8, 12 and 24 hours after hospitalization), delayed laparotomy, coexisting injuries, cost, and duration of hospitalization were collected. All cases were serially examined on arrival, 4, 8, 12 and 24 hours after admission by a senior surgical resident and were examined with respect to certain abdominal symptoms based on peritonitis and they were followed by hemoglobin check every 8 hours. If any patients showed peritonitis symptoms or hemodynamic instability, they were sent to the operating room for laparotomy.
All data were analyzed with SPSS software version 21. To determine the rate of laparotomy in clinical examinations, confidence interval of 95% and chi square test were used. Confidence interval of 95% was also used to determine the rate of mortality, the mean duration of hospitalization, and the mean hospital spending in nonsurgical methods. All quantitative data followed normal distribution with Kolmogorov-Smirnov’s test. For comparison of abdominal symptoms, chi square test and the independent t-test were used. The significance was set at P < 0.005.
4. Results
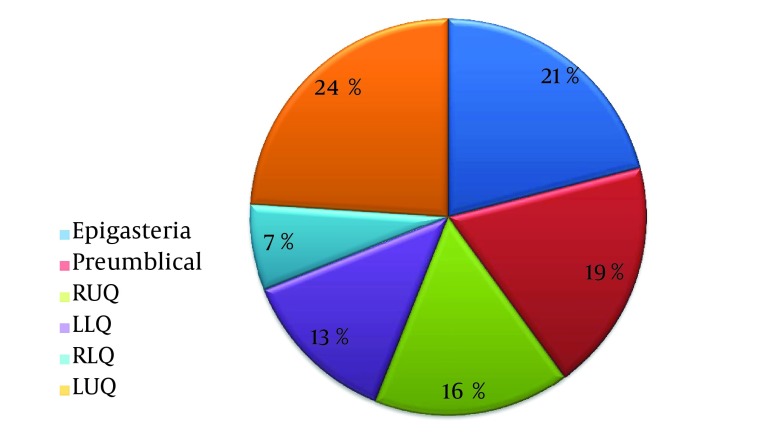
This study was conducted on 100 patients, 91 males and 9 females. The youngest patient was 16 years old and the oldest was 75 years. The mean age of patients was 29.9 ± 10.7 years old. The distribution of stab wound locations is presented in Figure 1.
Figure 1. The Distribution of Stab Wound Locations.
Most injuries were on the left lower quadrant and epigastrium. On arrival, only two cases presented abdominal tenderness, and no one showed classic findings of peritonitis or severe abdominal pain.
Coexisting injuries were present in 12 cases: 2 cases with neck trauma, 1 case with left hand tendon rupture, 1 case with ear rupture, 1 case with forearm laceration, 1 case with blunt abdominal trauma, and 1 case with forearm fracture.
Duration of hospitalization in 31, 30, 32 and 7 cases were 1, 2, 3 - 4, and more than 5 days, respectively. No mortality occurred among our cases.
Based on the findings obtained from clinical examinations, 8 patients (7 men and 1 woman) developed peritonitis, 1 case after 4 hours, 2 cases after 8 hours and 5 cases after 12 hours (Table 1). These were treated with delayed laparotomy. The causes of peritonitis in these 8 cases were: 3 patients with gastric rupture, 3 cases with colon rupture, and 2 patients with rupture of the small intestine.
Table 1. Cross Tabulation Based on Fisher Exact Test Between Sex and Delayed Laparotomy a,b.
| Delayed Laparotomy | Gender | Total | |
|---|---|---|---|
| Female | Male | ||
| Yes | 1 (12.5) | 7 (87.5) | 8 (100) |
| No | 8 (8.7) | 84 (91.3) | 92 (100) |
| Total | 9 (9.0) | 91 (91.0) | 100 (100) |
a Data are presented as No. (%).
b P value was equal to 0.543.
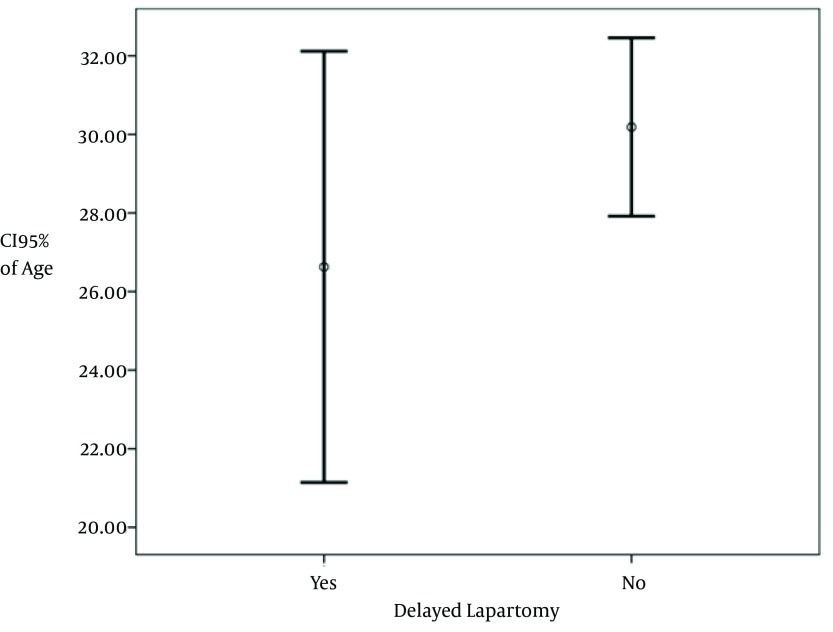
The mean age of patients treated with delayed laparotomy and those treated without invasive treatment were 26.62 ± 6.56 and 30.18 ± 10.94 respectively. This difference in age was not statistically significant (P = 0.369), (Figure 2). Delayed laparotomy according to injury location in order of frequency was: Pre-umbilical (15.8%), epigastria (14.3%) and left upper quadrant (8.3%), (Table 2).
Figure 2. Group Statistics Based on Independent T-Test Between Age and Delayed Laparotomy.
Table 2. Cross Tabulation Between Location of Wound and Delayed Laparotomy a.
| Location of Wound | Delayed Laparotomy | Total | |
|---|---|---|---|
| No | Yes | ||
| RUQ | 16 (100) | 0 (0) | 16 (100) |
| RLQ | 7 (100) | 0 (0) | 7 (100) |
| LUQ | 22 (91.7) | 2 (8.3) | 24 (100) |
| LLQ | 13 (100) | 0 (0) | 13 (100) |
| Epigastria | 18 (85.7) | 3 (14.3) | 21 (100) |
| Pre Umbilical | 16 (84.2) | 3 (15.8) | 19 (100) |
| Total | 92 (92.0) | 8 (8.0) | 100 (100) |
a Data are presented as No. (%).
Distribution of the mean frequency and standard deviation (SD) of systolic blood pressure (mmHg) and heart rate (/min) in all cases and its relation with delayed laparotomy are presented in Figure 2. The distribution of the mean frequency and SD of Hemoglobin titer were: 13.55 ± 1.04 on arrival, 14.22 ± 1.18 at 8 hours, and 13.12 ± 1.04 at 16 hours after admission. There was no significant differences between systolic blood pressure in two groups treated with and without laparotomy, but there was a significant difference in heart rate at 8 and 12 hours after admission with higher heart rates in cases with laparotomy (P = 0.001 and P = 0.001), (Table 3).
Table 3. Group Statistics Between Mean Systolic Blood Pressure and Heart Rate and Delayed Laparotomy.
| Delayed Laparotomy | Number | Mean ± SD | P Value |
|---|---|---|---|
| On arrival | |||
| Systolic blood pressure, mmHg | 0.668 | ||
| Yes | 8 | 112.50 ± 11.65 | |
| No | 92 | 115.07 ± 16.49 | |
| Heart rate, /min | 0.786 | ||
| Yes | 8 | 85.00 ± 7.56 | |
| No | 92 | 84.35 ± 6.42 | |
| 4 hours after admission | |||
| Systolic blood pressure, mmHg | 0.626 | ||
| Yes | 8 | 113.75 ± 9.16 | |
| No | 92 | 115.73 ± 11.10 | |
| Heart rate, /min | 0.154 | ||
| Yes | 8 | 85.62 ± 6.23 | |
| No | 92 | 82.39 ± 6.10 | |
| 8 hours after admission | |||
| Systolic blood pressure, mmHg | 0.965 | ||
| Yes | 7 | 117.14 ± 9.51 | |
| No | 92 | 116.97 ± 10.17 | |
| Heart Rate, /min | 0.001 | ||
| Yes | 7 | 85.71 ± 5.35 | |
| No | 92 | 78.85 ± 5.05 | |
| 12 hours after admission | |||
| Systolic Blood Pressure, mmHg | 0.964 | ||
| Yes | 4 | 117.50 ± 5.00 | |
| No | 92 | 117.72 ± 9.53 | |
| Heart Rate, /min | 0.0001 | ||
| Yes | 4 | 92.50 ± 5.00 | |
| No | 92 | 77.46 ± 4.53 |
In this study, the mean amount and standard deviation of hospital spending, in terms of 10 thousand Rials, in cases with coexisting injuries and those without, were 928 ± 824 and 434 ± 300 respectively. The difference in duration of hospitalization in cases with or without coexisting injuries was also statistically significant (P = 0.004).
According to the obtained information, the mean hospital spending increased with increased duration of hospitalization. Hospital spending in patients treated with laparotomy was significantly higher (P = 0.0001), (Table 4).
Table 4. Comparison of Hospital Spending in Terms of Delayed Laparotomy a.
| Delayed Laparotomy | Number | Hospital Spending, Rials | 95% Confidence Interval for Mean | Maximum | Minimum | |
|---|---|---|---|---|---|---|
| Upper Bound | Lower Bound | |||||
| Yes | 8 | 10867069.63 ± 8659537.80 | 18106624.40 | 3627514.85 | 28696194 | 832651 |
| No | 92 | 4422340.04 ± 3251830.49 | 5095775.06 | 3748905.02 | 23544692 | 654145 |
| Total | 100 | 4937918.41 ± 4255570.22 | 5782315.87 | 4093520.95 | 28696194 | 654145 |
a P value was equal to 0.0001.
5. Discussion
This was a survey conducted on 100 patients with stab wounds to the anterior abdominal wall referred to Pursina Hospital in Rasht. Many studies have reported that patients suffering from visceral bleeding and internal organs must be immediately transferred to the operating room (16-20). This also existed in our study and hemodynamically unstable patients were excluded from the study and transferred to the operating room. 91 patients were men and 9 were women, similar to the Schmelzer et al. (16) and Tsikitis et al. (17) studies. The subjects in our study were much younger (mean age: 29.9 ± 10.7 years) than those in these two studies.
In our study, delayed laparotomy according to injury location performed for cases with the wounds on the upper quadrants of the abdomen. In other studies (15-20), special attention was given to the upper abdomen, especially left and right upper quadrants and epigastria. It has been mentioned that organ damage in these areas is more likely, especially the stomach and diaphragm (18). Also, we found that the highest frequency of the damages resulted in laparatomy belonged to those happened on the Left upper quadrant and Preumbelical area. The stomach is one of the most vulnerable viscera, and is affected by the time of the last meal (18). Unfortunately, we did not consider the time of trauma as a variable in this survey. During this study, no patients suffered from hemodynamic instability, similar to Cothren et al. (19). Peritonitis was the main factor of delayed laparotomy in the 8 cases treated with laparotomy.
In our study, duration of hospitalization in 93, 61, and 31 percent of subjects was less than 4, 2 and 1 days respectively and it was more than 5 days in just 7% of cases, similar to Thomas et al. with 3.3 days as the mean duration of hospitalization. In this survey, delayed laparotomy was conducted on 8% of patients. In other words, 92% of our cases needed no invasive interventions. The rate of delayed laparotomy in similar studies conducted by Schmelzer et al. (16), Tsikitis et al. (17) and Cothren et al. (19) was high 25%, 11% and 10.7% respectively. Therefore in our study, the success of nonsurgical treatment was more than the mentioned studies. In comparison with Schmelzer et al. (16), the success rate of nonsurgical treatment in our study was less. All 8 cases showed classic peritonitis findings during clinical examinations and all suffered from visceral injuries. In other words, the negative rate of laparotomy was 0% which is lower than Plackett et al. (20) with 18.7%. The maximum delay time in conducting laparotomy was 12 hours which was less than the maximum delay time of Paydar et al. (21) (12 hours versus 17 hours).
In our study, among those cases treated with laparotomy, 81.5% were male and 12.5% were female and this difference in gender was not statistically significant (P= 0.543). Compared to other studies, only in Tsikitis et al. (17) was there an equal number and in other studies men treated with delayed laparotomy had a higher proportion (15-18). No mortality occurred in our survey which was lower than Plackett et al. (20) 0% versus 0.7%.
According to our findings, the mean hospital spending increased with longer duration of hospitalization and was more in cases with coexisting injuries. Also, similar to Schmelzer et al. (16), the difference between hospital spending in cases with laparotomy treatment and those without, was significant.
According to recent findings and based on the comparison of the obtained results from other studies, it was found that in patients referred to our hospital using the method of clinical examination in hemodynamically stable cases with anterior abdomen stab wounds was an effective and safe approach. Because of reduction in complications of invasive procedures, prevention of negative laparotomies, and decrease in duration of hospitalization and cost reduction, it can be the best and most appropriate approach in these patients.
Based on many studies, one of the earliest approaches to abdominal stab wounds is to explore the wound in emergency room (15-17). Unfortunately, due to special circumstances such as admission at night, no access to a well-trained medical team at that moment, limited lightening, limitations such as patient anxiety, high body mass index (BMI), aggressive mood and poor cooperation, it may be too difficult to examine the wound carefully and explore it in the emergency room. Also, in some cases, little equipment and poor asepsis during wound exploration in the emergency room may lead to wound infections.
Acknowledgments
The authors express their gratitude to Zahra Haghparast Ghadim-Limudahi for critical reading of the manuscript and for her insightful suggestions.
Footnotes
Authors’ Contribution:Writing the manuscript: Mohammad Rasool Herfatkar, Mohammad Reza Mobayen data collection: Mehdi Karimian, Fariba Rahmanzade; draft: Iraj Baghi; analysis: Sadaf Baghernejad Monavar Gilani.
Funding/Support:This study was supported by the Guilan Surgery Research Center in Rasht.
References
- 1.Norouzpour A, Khoshdel AR, Modaghegh MH, Kazemzadeh GH. Prehospital management of gunshot patients at major trauma care centers: exploring the gaps in patient care. Trauma Mon. 2013;18(2):62–6. doi: 10.5812/traumamon.10438. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Sanei B, Mahmoudieh M, Talebzadeh H, Shahabi Shahmiri S, Aghaei Z. Do patients with penetrating abdominal stab wounds require laparotomy? Arch Trauma Res. 2013;2(1):21–5. doi: 10.5812/atr.6617. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Baradaran H, Salimi J, Nassaji-Zavareh M, Rabbani A, Khaji A. Epidemiological study of patients with penetrating abdominal trauma in Tehran-Iran. Acta Med Iranica. 2007;45(4):305–8. [Google Scholar]
- 4.Hsieh TM, Cheng Tsai T, Liang JL, Che Lin C. Non-operative management attempted for selective high grade blunt hepatosplenic trauma is a feasible strategy. World J Emerg Surg. 2014;9(1):51. doi: 10.1186/1749-7922-9-51. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Pallett JR, Sutherland E, Glucksman E, Tunnicliff M, Keep JW. A cross-sectional study of knife injuries at a London major trauma centre. Ann R Coll Surg Engl. 2014;96(1):23–6. doi: 10.1308/003588414X13824511649616. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Katz-Summercorn A, Weaver C, Södergren M, Huf S, Moorthy K. The role of laparoscopy in penetrating abdominal trauma: A retrospective case series from a level 1 major trauma centre. Int J Surg. 2013;11(8):714–5. doi: 10.1016/j.ijsu.2013.06.683. [DOI] [Google Scholar]
- 7.Leppaniemi A, Salo J, Haapiainen R. Complications of negative laparotomy for truncal stab wounds. J Trauma. 1995;38(1):54–8. doi: 10.1097/00005373-199501000-00016. [DOI] [PubMed] [Google Scholar]
- 8.Demetriades D, Hadjizacharia P, Constantinou C, Brown C, Inaba K, Rhee P, et al. Selective nonoperative management of penetrating abdominal solid organ injuries. Ann Surg. 2006;244(4):620–8. doi: 10.1097/01.sla.0000237743.22633.01. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Ertekin C, Yanar H, Taviloglu K, Guloglu R, Alimoglu O. Unnecessary laparotomy by using physical examination and different diagnostic modalities for penetrating abdominal stab wounds. Emerg Med J. 2005;22(11):790–4. doi: 10.1136/emj.2004.020834. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Khubutiya M, Yartsev PA, Guliaev AA, Levitsky VD, Tlibekova MA. Laparoscopy in blunt and penetrating abdominal trauma. Surg Laparosc Endosc Percutan Tech. 2013;23(6):507–12. doi: 10.1097/SLE.0b013e3182937c37. [DOI] [PubMed] [Google Scholar]
- 11.Sugrue M, Balogh Z, Lynch J, Bardsley J, Sisson G, Weigelt J. Guidelines for the management of haemodynamically stable patients with stab wounds to the anterior abdomen. ANZ J Surg. 2007;77(8):614–20. doi: 10.1111/j.1445-2197.2007.04173.x. [DOI] [PubMed] [Google Scholar]
- 12.Nair MS, Uzzaman MM, Al-Zuhir N, Jadeja A, Navaratnam R. Changing trends in the pattern and outcome of stab injuries at a North London hospital. J Emerg Trauma Shock. 2011;4(4):455–60. doi: 10.4103/0974-2700.86628. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Maxwell R, Trotter C, Verne J, Brown P, Gunnell D. Trends in admissions to hospital involving an assault using a knife or other sharp instrument, England, 1997-2005. J Public Health (Oxf). 2007;29(2):186–90. doi: 10.1093/pubmed/fdm018. [DOI] [PubMed] [Google Scholar]
- 14.Yildiz MK, Ozkan E, Odabasi HM, Eris C, Gunay E, Abuoglu HH, et al. Analysis of 120 patients with abdominal stab wound focusing on diagnostic role of fast. Int J Clin Exp Med. 2014;7(5):1386–90. [PMC free article] [PubMed] [Google Scholar]
- 15.Inaba K, Demetriades D. The nonoperative management of penetrating abdominal trauma. Adv Surg. 2007;41:51–62. doi: 10.1016/j.yasu.2007.05.004. [DOI] [PubMed] [Google Scholar]
- 16.Schmelzer TM, Mostafa G, Gunter OJ, Norton HJ, Sing RF. Evaluation of selective treatment of penetrating abdominal trauma. J Surg Educ. 2008;65(5):340–5. doi: 10.1016/j.jsurg.2008.06.008. [DOI] [PubMed] [Google Scholar]
- 17.Tsikitis V, Biffl WL, Majercik S, Harrington DT, Cioffi WG. Selective clinical management of anterior abdominal stab wounds. Am J Surg. 2004;188(6):807–12. doi: 10.1016/j.amjsurg.2004.08.046. [DOI] [PubMed] [Google Scholar]
- 18.Clarke DL, Allorto NL, Thomson SR. An audit of failed non-operative management of abdominal stab wounds. Injury. 2010;41(5):488–91. doi: 10.1016/j.injury.2009.10.022. [DOI] [PubMed] [Google Scholar]
- 19.Cothren CC, Moore EE, Warren FA, Kashuk JL, Biffl WL, Johnson JL. Local wound exploration remains a valuable triage tool for the evaluation of anterior abdominal stab wounds. Am J Surg. 2009;198(2):223–6. doi: 10.1016/j.amjsurg.2008.11.024. [DOI] [PubMed] [Google Scholar]
- 20.Plackett TP, Fleurat J, Putty B, Demetriades D, Plurad D. Selective nonoperative management of anterior abdominal stab wounds: 1992-2008. J Trauma. 2011;70(2):408–13. doi: 10.1097/TA.0b013e31820b5eb7. discussion 413-4. [DOI] [PubMed] [Google Scholar]
- 21.Paydar S, Salahi R, Izadifard F, Jaafari Z, Abbasi HR, Eshraghian A, et al. Comparison of conservative management and laparotomy in the management of stable patients with abdominal stab wound. Am J Emerg Med. 2012;30(7):1146–51. doi: 10.1016/j.ajem.2011.08.012. [DOI] [PubMed] [Google Scholar]