Abstract
Objective
Recent literature reports that radical hysterectomy followed by adjuvant radiotherapy has comparable progression-free survival and overall survival compared to radical radiotherapy for International Federation of Gynecology and Obstetrics stage IIB cervical cancer. Now, we evaluate the cost-effectiveness (CE) of these two treatment regimens.
Primary and secondary outcome measures
A decision-tree model was constructed comparing CE between treatment arms using the published studies for overall survival rates and treatment-related toxicity rates for 5 years. The cost data were obtained from the hospital system of the First Affiliated Hospital of Xi’an Jiaotong University. Effectiveness was measured as quality-adjusted life year (QALY). Treatment arms were compared with regard to costs and life expectancy using incremental CE ratio, and the results were presented using costs per QALY.
Results
The mean cost was $10,872 for radical hysterectomy followed by adjuvant radiotherapy versus $5,702 for radical radiotherapy. The incremental CE ratio for surgery-based treatment compared to radiotherapy-based treatment was –$76,453 per QALY.
Conclusion
Radical radiotherapy would be a cost-effective method for FIGO stage IIB cervical cancer and would be favored in settings where resources are limited.
Keywords: cost-effectiveness, cervical cancer, FIGO stage IIB, surgery, radiotherapy
Background
Cervical cancer is the most common gynecological cancer in developing countries with the incidence peaks in the fourth decade of life.1 The treatment of cervical cancer is primarily based on the stage of disease. The appropriate treatment for International Federation of Gynecology and Obstetrics (FIGO) stage IIB cervical cancer has been a controversial issue.2–4 The National Comprehensive Cancer Network guidelines recommend cisplatin-based chemoradiotherapy as a primary treatment for the FIGO stage IIB cervical cancer. However, other guidelines, such as the German Arbeitsgemeinschaft Gynäkologische Onkologie guidelines, recommend radical hysterectomy plus adjuvant radiotherapy as a feasible approach for these patients. It is reported that radical hysterectomy followed by adjuvant radiotherapy has comparable progression-free survival and overall survival (OS) compared to radical radiotherapy for FIGO stage IIB cervical cancer.2–4 Our previous literature reported that radical radiotherapy was associated with fewer treatment-related complications and achieved a comparable survival outcome compared to radical hysterectomy plus adjuvant radiotherapy for FIGO stage IIB disease.5 However, all the previous studies reported only progression-free survival, OS, or toxicities, whereas the costs of treatment have rarely been addressed.
All countries are increasingly aware of the need for efficient use of health care resources. Cervical cancer is a common cancer; however, there have been few cost-effectiveness (CE) studies on this cancer. Furthermore, with the majority of cervical cancer cases occurring in the developing world, treatments that are not cost-effective will be inaccessible. For FIGO stage IIB disease with controversial treatment choice, CE analysis is particularly necessary for clinicians to make a clear choice. With this in mind, we sought to evaluate the relative CE of radical hysterectomy plus adjuvant radiotherapy compared to radical radiotherapy for FIGO stage IIB cervical cancer.
Methods
Model design
A decision-tree model to compare the cost and effectiveness between two primary treatment modalities for FIGO stage IIB cervical cancer patients was constructed using TreeAge Pro software (TreeAge Software Inc., Williamstown, MA, USA) (Figure 1). Treatment arms were compared as defined by Chai et al.5 Surgery-based treatment arm contained 148 patients and consisted of radical hysterectomy combined with adjuvant external beam radiotherapy (EBRT) (1.8 or 2 Gy per fraction, with five fractions administered per week for a total of 25 fractions and 45–50 Gy). Of these patients, 69 patients (46.62%) had one or more risk factors and received TP (paclitaxel and cisplatin) regimen for four cycles. RT-based (radiotherapy-based) treatment arm contained 290 patients who received radical radiotherapy consisted of pelvic EBRT (1.8 or 2 Gy per fraction, with five fractions administered per week for a total of 25 or 28 fractions and 50 or 50.4 Gy) followed by ICRT (intracavitary brachytherapy) (four or five fractions, with a total dose of 24–25 Gy). All the patients in the RT-based treatment arm received one cycle PF (cisplatin and 5-fluorouracil) regimen during pelvic EBRT as a radiosensitizing agent. Patient demographics displayed between the two groups were similar (Table 1). Upon completion of treatment, patients were followed up based on the gynecologic examination every 3 months in the 1st year, every 6 months from the 2nd year until the 5th year, and annually thereafter.
Figure 1.
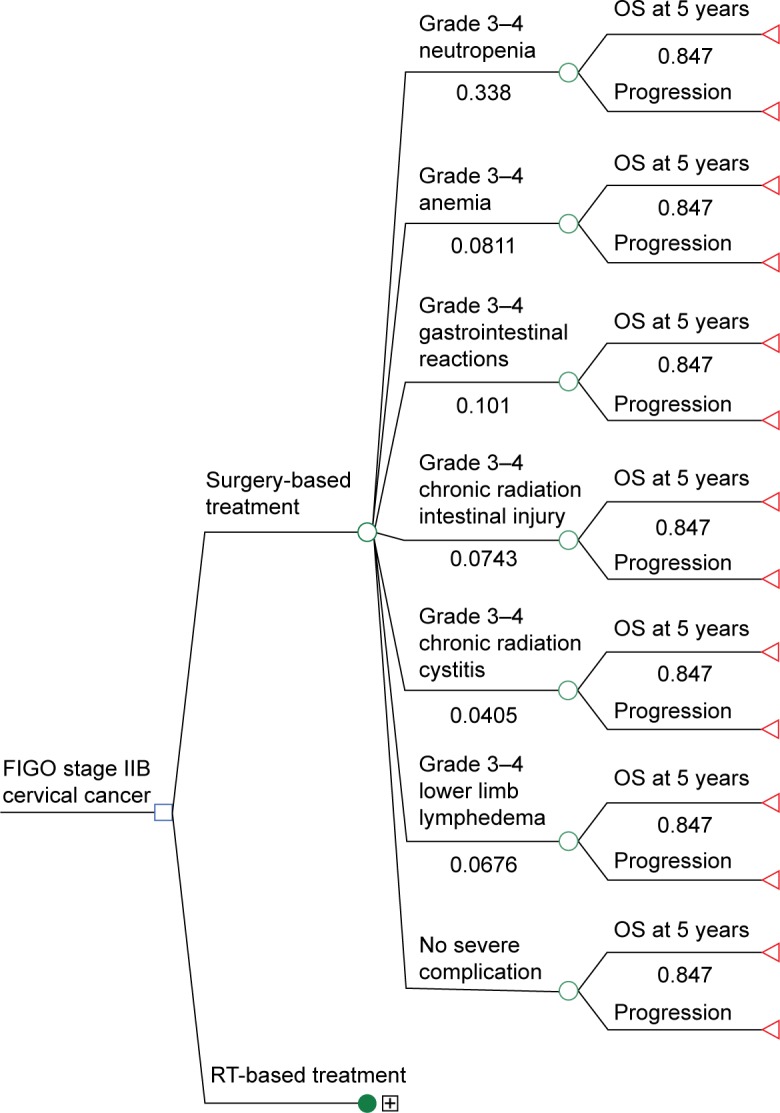
Decision analysis model.
Notes: Cost-effectiveness model. Markov model comparing radical hysterectomy plus adjuvant radiotherapy versus radical radiotherapy for FIGO stage IIB cervical cancer.
Abbreviations: OS, overall survival; RT, radiotherapy.
Table 1.
Patient demographics
| Treatment arm S | Treatment arm R | |
|---|---|---|
| Median age, years (range) | 48 (25–70) | 51 (24–88) |
| Histopathology, n (%) | ||
| Squamous | 136 (92.0) | 272 (93.8) |
| Non-squamous | 12 (8.0) | 18 (6.2) |
| Maximum tumor diameter (mm), n (%) | ||
| >40 | 26 (17.57) | 89 (30.69) |
| ≤40 | 122 (82.43) | 201 (69.31) |
| One or more risk factors | 69 (46.62) | – |
Abbreviations: R, radiotherapy-based; S, surgery-based.
Model parameters
Survival
The study protocol was approved by the Ethics Committee of the First Affiliated Hospital of Xi’an Jiaotong University, and informed consent were obtained from all participants. The OS for the two treatment strategies was based on the analysis reported by Chai et al.5 OS curves were published in the manuscript and were used for the model to best represent the original data and to reduce uncertainty. Five-year OS rates were 84.7% and 86.8% for surgery-based treatment arm and RT-based treatment arm, respectively, without significant statistical difference.
Toxicity
Major adverse events were defined as any hospitalizations including hospitalization for grade 3–4 anemia, neutropenia, acute gastrointestinal reactions, chronic radiation intestinal injury and chronic radiation cystitis, and lower limb lymphedema. The rates of treatment-related toxicity were obtained directly from the report published by Chai et al.5 The overall rates of grade 3–4 acute adverse events were similar for the two treatment arms (52.01% for surgery-based treatment arm vs 49.98% for RT-based treatment arm, P>0.05), while the incidence of acute grade 3–4 gastrointestinal reactions was significantly higher for the surgery-based group compared to the RT-based group (10.1% vs 4.48%, P=0.036). The frequencies of grade 3–4 chronic radiation intestinal injury and cystitis were similar (P=0.144 and P=0.378, respectively). The incidence of severe lower limb edema in surgery-based treatment arm was significantly higher than RT-based treatment arm (6.76% vs 2.07%, P=0.017).
Costs
The average currency exchange rate in 2012 was approximately 6.3 Yuan ¥/US $. Costs in 2012 US $, shown in Table 2, were estimated from the hospital system of the First Affiliated Hospital of Xi’an Jiaotong University and included hospital and professional costs associated with radical hysterectomy and pelvic lymphadenectomy, EBRT, ICRT, chemotherapy drugs, and treatment of toxicities and complications. The average treatment cost is $3,500 for EBRT of 3D-CRT, $2,742 for radical hysterectomy and pelvic lymphadenectomy, $688 for ICRT, $1,021 for PF regimen, and $2,182 for TP regimen (Table 2). The costs of each adverse event were based on the clinical experience. The average treatment costs for grade 3–4 toxicities are as follows: $523 for anemia, $1,109 for neutropenia, $408 for acute gastrointestinal reactions, $718 for chronic radiation intestinal injury, $628 for chronic radiation cystitis, and $313 for lower limb lymphedema (Table 2).
Table 2.
Model costs (year 2012, US $) and outcomes
| Clinical parameter | Treatment arm S | Treatment arm R |
|---|---|---|
| 5-year overall survival | 84.7% | 86.8% |
| Treatment cost (per patient) ($) | ||
| Surgery | 2,742 | 0 |
| EBRT | 3,500 | 3,500 |
| ICRT | 0 | 688 |
| PF regimen | 0 | 1,021 |
| TP regimen | 2,182 | 0 |
| Treatment cost for toxicity (per patient) ($) | ||
| Grade 3–4 anemia | 523 | 523 |
| Grade 3–4 neutropenia | 1,109 | 1,109 |
| Grade 3–4 GI toxicity | 718 | 718 |
| Grade 3–4 GU toxicity | 628 | 628 |
| Grade 3–4 lower limb lymphedema | 313 | 313 |
Abbreviations: EBRT, external beam radiotherapy; GI, gastrointestinal; GU, genito urinary; ICRT, intracavitary brachytherapy; PF, cisplatin and 5-fluorouracil; R, radiotherapy-based; S, surgery-based; TP, paclitaxel and cisplatin.
Cost-effectiveness analysis and sensitivity analysis
Cycle length was 6 months. Time horizon for analysis was 5 years. Effectiveness was measured as quality-adjusted life year (QALY). The costs were discounted at 3% yearly. A payer perspective was used: treatment arms were compared with regard to costs and life expectancy using the incremental CE ratio (ICER), and the results were presented using costs per QALY. ICER is a numerical value indicating how much it would cost to gain a unit in effectiveness. The numerator was the difference in costs, whereas the denominator was the difference in the QALYs. A structural sensitivity analysis was then conducted (Figure 2).
Figure 2.
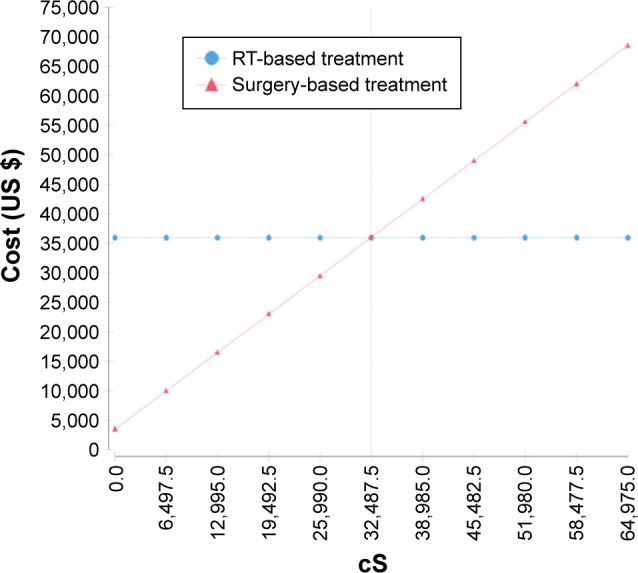
Sensitivity analysis.
Abbreviation: RT, radiotherapy.
Consent
Written informed consent was obtained from each patient for the publication of this report and any accompanying images.
Results
The average cost for surgery-based treatment is $10,872, whereas the average cost for RT-based treatment is $5,702. The results of the CE analysis are shown in Table 3. The base case model revealed that RT-based treatment arm had a reduced cost of $5,169 per patient with an incremental effectiveness of 0.07 QALYs. When compared to the surgery-based treatment, the ICER for RT-based treatment is –$76,453/QALY. This suggests that RT-based treatment is cost-effective compared to the surgery-based treatment. We then evaluated the impact of the cost of surgery on the CE by sensitivity analysis. In this analysis, the total cost is highly affected by the cost of surgery.
Table 3.
Results of the CE model
| Treatment arm | Cost | Incremental cost | Effectiveness (QALYs) | Incremental effectiveness (QALYs) | Incremental CE |
|---|---|---|---|---|---|
| Surgery-based treatment | $10,872 | $5,173 | 4.37 | −0.07 | –$76,453 |
| RT-based treatment | $5,702 | NA | 4.44 | NA | NA |
Abbreviations: CE, cost-effectiveness; NA, not available; RT, radiotherapy; QALYs, quality-adjusted life years.
Discussion
FIGO stage IIB cervical cancer has traditionally been treated by radical hysterectomy plus adjuvant radiotherapy or radical radiotherapy with similar survival outcomes.2–4 The decision regarding treatment options for stage IIB disease is complex. Competing factors that arise from the perspective of cancer control (survival), treatment toxicity, quality of life, and geographic location of the patient (related to access to specific health care resources), all play a role in the ultimate decision to radical radiotherapy or radical surgery plus with adjuvant radiotherapy. Proponents of radical radiotherapy argue that many patients treated surgically will subsequently require adjuvant radiotherapy, thereby increasing the adverse event rate, while the proponents of radical hysterectomy cite the potential to preserve ovarian and vaginal function and to avoid brachytherapy-related complications.6,7 However, no study was conducted from the perspective of the CE analysis.
As health care costs and expenditures continue to grow, there has been an increased awareness of the CE of regimens. Worldwide, cervical cancer is the second most common cause of cancer death in developing countries,8 and the cost of cervical cancer treatment is compounded by substantially higher rates of patients with lower socioeconomic status. With the burden of cervical cancer treatment primarily affecting indigent populations, therapies must be cost-effective, otherwise they may be unobtainable for patients.
For FIGO stage IIB cervical cancer, we have published an article discussing treatment outcomes of radical radiotherapy or primary radical hysterectomy with tailored adjuvant therapy.5 The article revealed that radical radiotherapy was associated with less treatment-related complications and achieved comparable survival outcomes for patients with FIGO stage IIB cervical cancer compared to radical hysterectomy followed by postoperative radiotherapy.5 Now in this study, we compared the two treatment methods from the perspective of the CE analysis. We constructed a decision-tree model to determine which of two common treatment strategies is more cost-effective. The results of our model suggest that RT-based treatment is potentially cost-effective, with a reduced cost of $5,169, an incremental effectiveness of 0.07 QALYs, and the ICER of –$76,453/QALY. In other words, compared with surgery-based treatment, RT-based treatment had a higher survival benefit and lower cost.
Higher complication rates are experienced when the patients receive both radical surgery and radiotherapy compared to radical radiotherapy alone.9,10 Patients with FIGO stage IIB cervical cancer usually exhibit high-risk pathological factors following radical hysterectomy such as positive pelvic nodes, parametrial invasion, or a positive surgical margin. For these individuals, postoperative adjuvant chemotherapy (four cycles of TP regimen) is inevitable. These patients experienced longer treatment duration, including 2 weeks to 1 month for surgery, 7 weeks for EBRT, and for patients with higher risk factors at least 3 months for TP regimens. This would not only have a negative impact on patients’ confidence of treatment success, but also result in higher chemotherapy-related complication rates, more treatment cost, more income lost, more transportation costs, more labor charges, etc. In addition, the incidence of chronic lower extremity lymphedema in surgery-based group is higher than that in RT-based group. This is related to lymph node dissection and lymphatic destruction in surgery. Patients with severe lower extremity lymphedema may have different thickness of bilateral lower extremity and cannot buy the right shoes and pant, which produced mental inferiority and seriously affect their quality of life. Therefore, opting for radical radiotherapy instead of radical surgery, especially for patients exhibiting risk factors for the development of severe late stage toxicities,11,12 may provide more benefits.
There are some limitations in our study. First, indirect costs such as income lost, transportation costs, labor charges, and the quality of life information were not incorporated into the model because of the retrospective nature of the research. Additionally, newer cervical cancer treatment strategies such as the use of intensity-modulated radiation therapy,13–15 or the use of neoadjuvant chemotherapy,16,17 which have been reported to improve treatment effectivity and reduce toxicity rate, were not evaluated in our study. These strategies may not be feasible in geographic locations in which health care resources are limited because of their expensive costs, although their use would possibly increase the effectiveness and reduce the rate of toxicity. However, in the case of medical resources fully, these effective new treatments should be considered in treatment decisions.
It is important to remember that a CE analysis should never supercede sound clinical judgment and patient preference. Furthermore, the goal of a decision analysis is to evaluate interventions that are cost-effective when only limited resources are available. A CE analysis is unable to reflect all relevant factors used in treatment decisions. Therefore, it should only serve as an adjunct to policy makers.
Conclusion
As health care expenses continue to rise, it is crucial to develop the most cost-effective treatments for women with FIGO stage IIB cervical cancer. In this model, we conclude that radical radiotherapy would be a cost-effective method for FIGO stage IIB cervical cancer. Radical radiotherapy appears to be a cost-effective strategy to manage these patients and would be favored in settings where resources are limited.
Acknowledgments
We are grateful to the patients for participating in this study. This research received no specific grant from any funding agency in the public, commercial or not-for-profit sectors.
Footnotes
Disclosure
The authors report no conflicts of interest in this work.
References
- 1.Jemal A, Bray F, Center MM, Ferlay J, Ward E, Forman D. Global cancer statistics. CA Cancer J Clin. 2011;61(2):69–90. doi: 10.3322/caac.20107. [DOI] [PubMed] [Google Scholar]
- 2.Kasamatsu T, Onda T, Sawada M, Kato T, Ikeda S. Radical hysterectomy for FIGO stage IIB cervical cancer: clinicopathological characteristics and prognostic evaluation. Gynecol Oncol. 2009;114(1):69–148. doi: 10.1016/j.ygyno.2009.03.026. [DOI] [PubMed] [Google Scholar]
- 3.Yamashita H, Nakagawa K, Tago M, et al. Comparison between conventional surgery and radiotherapy for FIGO stage I–II cervical carcinoma: a retrospective Japanese study. Gynecol Oncol. 2005;97(3):834–839. doi: 10.1016/j.ygyno.2005.03.017. [DOI] [PubMed] [Google Scholar]
- 4.Ohara K, Sugahara S, Kagei K, et al. Retrospective comparison of clinical outcome between radiotherapy alone and surgery plus postoperative radiotherapy in the treatment of stages IB–IIB cervical squamous cell carcinoma. Radiat Med. 2004;22(1):42–48. [PubMed] [Google Scholar]
- 5.Chai Y, Wang T, Wang J, et al. Radical hysterectomy with adjuvant radiotherapy versus radical radiotherapy for FIGO stage IIB cervical cancer. BMC cancer. 2014;14:63. doi: 10.1186/1471-2407-14-63. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Grigsby PW. Primary radiotherapy for stage IB or IIA cervical cancer. J Natl Cancer Inst Monogr. 1996;21:61–64. [PubMed] [Google Scholar]
- 7.Jewell EL, Kulasingam S, Myers ER, Alvarez Secord A, Havrilesky LJ. Primary surgery versus chemoradiation in the treatment of IB2 cervical carcinoma: a cost effectiveness analysis. Gynecol Oncol. 2007;107(3):532–540. doi: 10.1016/j.ygyno.2007.08.056. [DOI] [PubMed] [Google Scholar]
- 8.Ferlay JSH, Bray F, Forman D, Mathers C, Parkin DM. GLOBOCAN 2008 v1.2, Cancer Incidence and Mortality Worldwide: IARC Cancer-Base No. 10 [webpage on the Internet] Lyon: International Agency for Research on Cancer; 2010. [cited July 20, 2011]. Available from: http://globocan.iarc.fr. [Google Scholar]
- 9.Rotman M, Sedlis A, Piedmonte MR, et al. A phase III randomized trial of postoperative pelvic irradiation in Stage IB cervical carcinoma with poor prognostic features: follow-up of a gynecologic oncology group study. Int J Radiat Oncol Biol Phys. 2006;65(1):169–176. doi: 10.1016/j.ijrobp.2005.10.019. [DOI] [PubMed] [Google Scholar]
- 10.Perez CA, Grigsby PW, Camel HM, Galakatos AE, Mutch D, Lockett MA. Irradiation alone or combined with surgery in stage IB, IIA, and IIB carcinoma of uterine cervix: update of a nonrandomized comparison. Int J Radiat Oncol Biol Phys. 1995;31(4):703–716. doi: 10.1016/0360-3016(94)00523-0. [DOI] [PubMed] [Google Scholar]
- 11.Chen SW, Liang JA, Yang SN, Liu RT, Lin FJ. The prediction of late rectal complications following the treatment of uterine cervical cancer by high-dose-rate brachytherapy. Int J Radiat Oncol Biol Phys. 2000;47(4):955–961. doi: 10.1016/s0360-3016(00)00559-9. [DOI] [PubMed] [Google Scholar]
- 12.Gondi V, Bentzen SM, Sklenar KL, et al. Severe late toxicities following concomitant chemoradiotherapy compared to radiotherapy alone in cervical cancer: an inter-era analysis. Int J Radiat Oncol Biol Phys. 2012;84(4):973–982. doi: 10.1016/j.ijrobp.2012.01.064. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Hasselle MD, Rose BS, Kochanski JD, et al. Clinical outcomes of intensity-modulated pelvic radiation therapy for carcinoma of the cervix. Int J Radiat Oncol Biol Phys. 2011;80(5):1436–1445. doi: 10.1016/j.ijrobp.2010.04.041. [DOI] [PubMed] [Google Scholar]
- 14.Folkert MR, Shih KK, Abu-Rustum NR, et al. Postoperative pelvic intensity-modulated radiotherapy and concurrent chemotherapy in intermediate- and high-risk cervical cancer. Gynecol Oncol. 2013;128(2):288–293. doi: 10.1016/j.ygyno.2012.11.012. [DOI] [PubMed] [Google Scholar]
- 15.Du XL, Tao J, Sheng XG, et al. Intensity-modulated radiation therapy for advanced cervical cancer: a comparison of dosimetric and clinical outcomes with conventional radiotherapy. Gynecol Oncol. 2012;125(1):151–157. doi: 10.1016/j.ygyno.2011.12.432. [DOI] [PubMed] [Google Scholar]
- 16.Gadducci A, Sartori E, Maggino T, et al. Pathological response on surgical samples is an independent prognostic variable for patients with Stage Ib2–IIb cervical cancer treated with neoadjuvant chemotherapy and radical hysterectomy: an Italian multicenter retrospective study (CTF Study) Gynecol Oncol. 2013;131(3):640–644. doi: 10.1016/j.ygyno.2013.09.029. [DOI] [PubMed] [Google Scholar]
- 17.Minig L, Colombo N, Zanagnolo V, et al. Platinum-based neoadjuvant chemotherapy followed by radical surgery for cervical carcinoma international federation of gynecology and obstetrics stage IB2–IIB. Int J Gynecol Cancer. 2013;23(9):1647–1654. doi: 10.1097/IGC.0b013e3182a616d2. [DOI] [PubMed] [Google Scholar]


