Abstract
Objective
To explore rates of screening, and identification, and treatment for behavioral problems using billing data from Massachusetts Medicaid immediately following the start of the state's new court-ordered screening and intervention program.
Design
Retrospective review of the number of pediatric well-child visits, number of screens, and number of screens that identify risk for psychosocial problems, from January 2008 (the month pediatric screening started) to March 2009. During the surrounding 1-year period we also examined the number of claims with a behavioral health evaluation code.
Setting
Massachusetts.
Participants
Massachusetts Medicaid-enrolled children.
Intervention
Funded court-ordered mandate to screen for mental health during Medicaid well-child visits.
Outcome Measures
Percentage of visits with a screen, percentage of screens identified at risk, and number of children seen for behavioral health evaluations.
Results
Major increase from 16.6% of all Medicaid well-child visits coded for behavioral screens in the first quarter of 2008 to 53.6% in the first quarter of 2009. Additionally, the children identified as at risk increased substantially from about 1600 in the first quarter of 2008 to nearly 5000 in quarter 1 of 2009. The children with mental health evaluations increased from an average of 4543 to 5715 per month over a 1-year period.
Conclusions
The data suggest payment and a supported mandate for use of a formal screening tool can substantially increase the identification of children at behavioral health risk. Findings suggest that increased screening may have the desired effect of increasing referrals for mental health services.
Background
Epidemiological studies indicate that many parents come to a primary care visit with concerns about their children's emotional health, and approximately 12 to 13% of 4- to 16-year-olds have significant psychosocial dysfunction.1-3 The Task Force on Mental Health of the American Academy of Pediatrics has recently endorsed mental health screening in primary care as an effective step to prevent mental health disorders for children and adolescents4, joining a number of other prestigious governmental and professional organizations that have advocated for routine screening for the past decade or more.5-11 Screening activities generally involve assessing cohorts of children to determine their risk for a condition. In psychosocial health, there are a variety of validated questionnaires or screening tools for use in conducting these assessments.
Primary care is the one place in the health system that most children visit each year and where other forms of screening (for anemia and hypertension, for example) are expected and routine. Furthermore, mental health and general health are highly linked, making primary care practices a natural setting to screen for and address mental health problems. This linkage also provides a reason to better coordinate and connect services between primary care and mental health care systems.12, 13 There is a shortage of child mental health specialists, and one way of enhancing the capacity of the mental health delivery system is to increase primary care clinicians’ ability to evaluate and triage patients with the aid of screening tools administered in their practices.12 However, primary care clinicians face numerous barriers to screening and management of psychosocial disorders including time limitations, the stigma associated with mental health care, inadequate behavioral and mental health training among pediatricians, lack of reimbursement for screening, and too few referral options, which are confusing to navigate for families and providers.14 Studies indicate that primary care clinicians recognize only about one-half to one-third of the children with substantial dysfunction in their practices 3, 15 and that pediatric referral rates to mental health services range from 1% to 4% of all patients3, thus meeting only a small percentage of the need.
The American Academy of Pediatrics recommends using formal screening tools to identify developmental problems and adolescent depression. 4, 16 Studies indicate that broad use of formal tools is superior to subjective surveillance in detecting these problems in primary care settings.17 Under the Early and Periodic Screening, Diagnosis, and Treatment (EPSDT) statute, all states are required to provide Medicaid-eligible children with screening, “including assessment of both physical and mental health development.”18 Yet in a 2003 study about half of all states (23 in total) had “no specialized behavioral health screening tools and no behavioral health questions or prompts in their comprehensive screening tools.”19(p. 737) This lack of compliance has been the subject of successful lawsuits in several states.20 Despite the prevalence of emotional disorders, guidelines such as Bright Futures, Medicaid regulations, and almost forty years of advocacy by professional associations and federal agencies, screening for psychosocial dysfunction has not been widely implemented in pediatric primary care.
In Massachusetts, one of the states to experience such an EPSDT mental health legal challenge, the court-ordered remedy has led to the implementation of an array of enhancements and new services for children's behavioral health under MassHealth, the state Medicaid program. As a part of the remedy of a class-action lawsuit (Rosie D. v. Romney; later, Rosie D. v. Patrick)21, 22 the state implemented new regulations requiring primary care providers to screen for developmental and behavioral problems at all well-child visits or at parent request, for all MassHealth members under the age of 21. Providers are required to use validated, standardized screening tools from a list provided by the state 23 (Table) and are currently reimbursed approximately $10 for each screening test performed24 and an additional $25 for face to face evaluation and management time for a positive screen. Prior to these regulations, even the mandated screening under EPSDT did not require the use of specified tools and was not a distinct uniformly reimbursable service.
Table.
Assessment Toolsa
| Tool | Abbreviation | Age Range |
|---|---|---|
| Ages and Stages Questionnaire: Social-Emotional | ASQ:SE | 3-60 months |
| Brief Infant and Toddler Social and Emotional Assessment | BITSEA | 12-36 months |
| Child Behavior Checklist/Youth/Adult Achenbach System of Empirically Based Assessment | CBCL | 1.4 to 20 years |
| Car, Relax, Alone, Forget, Friends, Trouble (specific to substance/alcohol use) | CRAFFT | 14-18 years |
| Parents’ Evaluation of Developmental Status | PEDS | 0-8 years |
| Modified Checklist for autism in Toddlers (specific to autism) | M-CHAT | 16 -30 months |
| Patient Health Questionnari-9 (specific to depression) | PHQ-9 | 18-20 years |
| Pediatric Symptom Checklist http://www2.massgeneral.org/allpsych/psc/psc_home.htm |
PSC YPSC |
4-16 years 11+ years |
Adapted from MassHealth-Approved Standardized Behavioral Health Screening Tools for Children Under the Age of 21.23
In addition to providing reimbursement, the state launched a substantial effort to inform primary care practices about the requirement and to provide educational and technical resources to support clinical and practice-management issues related to the requirement. Information was distributed through pediatric and family practice networks and the local news media, as well as through conventional notices to MassHealth providers and, through MassHealth's managed care organizations, to the networks of the managed care organizations. The state also sponsored regional educational forums for provider staff, and made available free telephone consultation from two physician experts in behavioral health screening; notices were also sent to MassHealth members informing them about the new screening rules. The regulations requiring well-child screening went into effect on December 31, 2007.
This paper examines rates of screening and identification of behavioral problems for children with Medicaid coverage in Massachusetts during the months immediately following the Rosie D. ruling and reports on the combined impact of a court order, thoughtful implementation efforts, and distinct reimbursements for psychosocial screening services.
Methods
Samples
For the whole Massachusetts Medicaid population, we obtained the number of pediatric well child visits, the number of screens (procedure code 96110), and the number of screens that identify risk for psychosocial problems (with U2 as a modifier of the procedure code that indicates a positive screen). These data come from the plaintiff's attorney (S. Schwartz, written communication, December 31, 2009) and were prepared by Massachusetts Department of Medical Assistance staff for the purpose of reporting to Judge Ponsor on the implications of the court-ordered remedy. They cover the period from January 2008 (the month screening became mandatory) to December 2009 two years later. In a separate data report provided by MassHealth, also obtained from the Massachusetts Executive Office of Human Services a spreadsheet provided data on the number of children with MassHealth for whom claims were submitted each month with a behavioral health evaluation procedure code (90801) for the period from September 2008 to November 2009.
Variables
We computed the percentages of well child visits of Medicaid enrolled children with screens and the percent of screens with identified as at risk by quarter from January 2008 to March 2009 for the Medicaid Population.
Analyses
For the whole Medicaid population, we graph the change in the percentage of visits with a screen and the percentage of screens with an outcome of “identified as at risk.” These data are presented by quarter. We also show numbers of children with behavioral health evaluations for September through November 2008 vs. September through November 2009.
Results
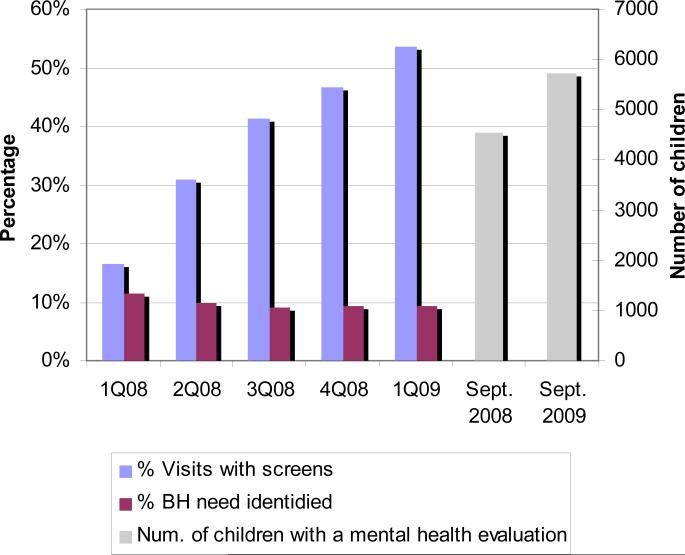
Figure 1 shows the sharp increase from 16.6% of all Medicaid well child visits that have screens in the first quarter of 2008 (just after the start of the Rosie D regulations) to 53.6% in the first quarter of 2009 one year later. This reflects an increase from 20 334 screens in the first quarter of 2008 to 63 555 in the first quarter of 2009 or a tripling of the number of screens and an increase of over 40 000 more screens.
Figure 1.
Percentage of Medicaid-enrolled children with screens for mental health (blue), percent of “modified” screens with behavioral health (BH) problems identified (red), and number of children with a mental health evaluation (grey).
The number of children identified as at risk increased substantially from about 1600 in quarter 1 of 2008 to nearly 5000 in quarter 1 of 2009. Extrapolating these figures to an annual number suggests that if the first-quarter figures in 2009 held steady about 20 000 children would have been identified in 2009. If the first quarter of 2008 suggests a level of identification close to that prior to the Rosie D. regulations, about 5800 children would have been screened annually (a rough estimate of the levels prior to Rosie D.). This suggests that under the new Rosie D. regulations about 14 200 children would be identified as at risk for behavioral health problems who would not have been identified if screening and identification rates remained at the levels they were in the first quarter of 2008. The percentage of children with an identified behavioral health risk based on the screening actually decreased slightly over this period (from 11.6 to 9.2% of those screened) but because the large increase in screening, the number of children identified was still much higher in the last quarter than in the first quarter studied.
Data from the Commonwealth of Massachusetts also show that the number of children with a behavioral health evaluation increased about 25%, from an average of 4543 to an average of 5715 per month for the quarter starting in September 2008 vs the quarter starting in September 2009.
Comment
These data show a remarkable 3-fold increase in the number of pediatric screens and the percentage of well child visits with screens following implementation of a small payment and a comprehensive statewide program supporting routine behavioral health screening as a part of pediatric well child visits covered by EPSDT in the state of Massachusetts. With a reimbursement of just $10 per screen, there were an estimated 40 000 additional screens and 3500 more positive screens in the first quarter of 2009 than there had been in the first quarter of 2008. These data suggest that a small payment and a well-supported mandate for use of a formal screening tool can substantially improve the identification of children at behavioral health risk.
Despite the major increase in screening, a large number and proportion (nearly half) of well child visits still do not have identified behavioral health screening, even though MassHealth requires primary care providers to screen for behavioral health conditions, provides payment for these behavioral health screenings, and has conducted extensive educational outreach and technical assistance to primary care practices. We do not yet understand all the factors affecting screening implementation, or steps that would further increase behavioral health screening rates.
The percentage of screens identified as at risk decreased slightly over the first year of implementation. We speculate that screening was more selectively targeted at individual children with suspected risk initially when screening rates were low. In the later quarters, as screening rates ranged around 50%, it is likely that more children with low risk were screened and thus fewer of the screens identified risk. Despite this slight decrease in the percentage of well-child visits with screens with identified risk, the numbers screened as at risk still increased markedly. We estimate a substantial increase in Medicaid-enrolled children who were identified as at risk 2009 than would have been identified if 2008 first quarter rates remained steady. These are children whose risk profile likely went undetected prior to the increase in screening.
In a partially overlapping time frame, the number of children with Medicaid who received behavioral health evaluation visits increased by just over 1000 visits per month from the end of 2008 to the end of 2009. This finding suggests that the increased screening in pediatrics may be having the desired effect of increasing mental health services for at least some children. But because the data come from different data sets, there is no way to know the extent to which the increased behavioral health referrals were due to pediatric screens or vice versa.
We also do not know the extent to which children received other types of mental health services (eg, traditional mental health services or counseling provided by a social worker or through a school). We also lack information about referrals for other types of services. For example, other desired outcomes of positive screening in pediatrics in Massachusetts could include more time and counseling with the pediatrician and/or referral to any of a number of community based services like wrap-around, that were made available as a part of the Rosie D. remedy implementation.
As alluded to earlier, in addition to screening, Rosie D. also led to the implementation of the Children Behavioral Health Initiative, which directed major changes in the service landscape for children and adolescents with emotional behavioral health needs on Medicaid, with a focus on community-based care. These changes included enhanced emergency services, with new mobile crisis teams focused on stabilizing children in their natural environments when possible, and the ability to remain to remain engaged with the child and family for up to 72 hours. Additional new services included Intensive Care Coordination using the Wraparound model for youth with complex needs, availability of family partners to families in need of peer support and guidance on navigating the system, and new in-home therapy teams. The Children's Behavioral Health Initiative also forged connections between existing mental health services across the state. These enhancements and new services rolled out following the implementation of screening, over the period from June 30 to November 30, 2009. Patients are connected to these services either through self-referral or referral by primary care providers, school officials, or social workers. Once referred, a comprehensive behavioral health assessment is completed for the patient by a mental health provider, and a family-driven treatment plan is formed. Primary care providers often contact the Massachusetts Child Psychiatry Access Project (MCPAP) to facilitate these referrals.
The MCPAP25 is a system of 6 regional children's mental health consultation teams each staffed with a child psychiatrist, a psychologist or social worker, and a care coordinator. The program provides free, immediate, telephone or in-person clinical consultation to primary care practices serving children, irrespective of insurance status of the child. The MCPAP also “closes the loop” with primary care physicians by providing follow-up information regarding patients who are further referred to mental health services outside of the primary care physician's office, including services through the Children's Behavioral Health Initiative. The MCPAP program is funded by the state Department of Mental Health and was in full operation by the end of 2005. The MCPAP also provides information about screening tools and requirements for screening patients enrolled in Medicaid through its Web site. These changes may have helped promote the increase in screening since providers have new options for providing services to those identified as at risk. Physician surveys by MCPAP demonstrate that providers felt better able to meet the needs of patients with mental health problems after MCPAP was established. The volume of calls increased after December 2007 when the mandate for screening under Rosie D. became effective,26 although the effect of the mandate is difficult to separate from the trend of increased call volume over time generally. The MCPAP also may have helped increase the use of follow-up services either directly (children using these services) or indirectly (freeing up other services for children).
This study is subject to several limitations. First, all data are dependent on having services coded. We do not know the extent to which changes in the rate of coding influence these trends. We further do not know about mental health services provided in settings where a code would not be generated such as the public health sector or schools. All data are based on encounters not individual children. We are unable to determine whether the right children are receiving the right services or whether these services resulted in improvements in children's well-being. This information will be important to assess in the future. We also lack true baseline data, from the period before the implementation of the Rosie D. decision. Further limitations include any unreported administrative difficulties that discouraged offices from submitting complete data (bias to underreporting or even from billing at all).
In Massachusetts, the combination of a clear mandate, some training efforts, a modest increase in referral options and distinct reimbursement were able to overcome many of the longstanding barriers to psychosocial/developmental screening that had kept Massachusetts from full compliance with EPSDT regulations. If our nation truly seeks to leave no child left behind, finding ways to accelerate broad adoption of high-quality care is important. Efforts described in this paper appear to be an effective first step toward improving mental health services for children. But, access does not equal improved clinical outcomes without the ability to create and carry out care plans that meet families’ needs. If followed by appropriate further evidence- and community-based evaluation and services, routine psychosocial/developmental screening could be the start of a substantial improvement in the well-being of America's children.
Acknowledgments
Funding/Support: A Fuss Family Fund grant to Newton Wellesley Hospital made the current data analysis and paper writing possible.
Role of the Sponsors: None of the funders participated in the design or conduct of the study; collection, management, analysis, and interpretation of the data; or preparation, review, or approval of the manuscript.
Footnotes
Author Contributions: Dr Kuhlthau had full access to all of the data in the study and takes responsibility for the integrity of the data and the accuracy of the data analysis.
Study concept and design: Kuhlthau, Jellinek, Murphy.
Acquisition of data: Murphy.
Analysis and interpretation of data: Kuhlthau, Jellinek, White, VanCleave, Simons and Murphy.
Drafting of the manuscript: Kuhlthau, Jellinek, White, Simons and Murphy.
Critical revision of the manuscript for important intellectual content: Kuhlthau, Jellinek, VanCleave, Simons and Murphy.
Statistical analysis: Kuhlthau and Murphy.
Obtained funding: Jellinek
Administrative, technical, or material support: Kuhlthau, White and Murphy.
Study supervision: Kuhlthau and Jellinek.
Financial Disclosures: All Massachusetts General Hospital authors except Dr Jellinek received salary or consultation support for secondary data analysis or report writing described in this report. Dr Simons is an employee of the Commonwealth of Massachusetts. Drs Jellinek and Murphy are the authors of the Pediatric Symptom Checklist but they receive no income from this because it is available free in the public domain.
REFERENCES
- 1.Costello EJ, Angold A, Burns B, et al. The Great Smoky Mountains Study of Youth: Goals, design, methods, and the prevalence of DMS III-R disorders. Arch Gen Psychiatry. 1996;53(1129-1136) doi: 10.1001/archpsyc.1996.01830120067012. [DOI] [PubMed] [Google Scholar]
- 2.Jellinek MS, Murphy JM, Burns BJ. Brief psychosocial screening in outpatient pediatric practice. J Pediatr. 1986;109:371–378. doi: 10.1016/s0022-3476(86)80408-5. [DOI] [PubMed] [Google Scholar]
- 3.Kelleher KJ, Childs GE, Wasserman RC, et al. Insurance status and recognition of psychosocial problems. A report from the Pediatric Research in Office Settings and the Ambulatory Sentinel Practice Networks. Archives of Pediatrics & Adolescent Medicine. 1997;151(11):1109–1115. doi: 10.1001/archpedi.1997.02170480039006. [DOI] [PubMed] [Google Scholar]
- 4.American Academy of Pediatrics Task Force on Mental Health Appendix S4: The Case for Routine Mental Health Screening. Pediatrics. 2010;125(S3):S133–139. doi: 10.1542/peds.2010-0788C. [DOI] [PubMed] [Google Scholar]
- 5.US Preventive Services Task Force Screening and treatment for major depressive disorder in children and adolescents: US Preventive Services Task Force recommendation statement. Pediatrics. 2009;123(6):1611. doi: 10.1542/peds.2008-2381. [DOI] [PubMed] [Google Scholar]
- 6.Massachusetts DoMHaDD Behavioral Health Services for Children and Adolescents: Ages 6-17. http://state.tn.us/mental/07BestPractGuide_C&A_.pdf.
- 7.Minnesota DoMHaDD Behavioral Health Services for Children and Adolescents: Ages 6-17. http://state.tn.us/mental/07BestPractGuide_C&A_.pdf.
- 8.U.S. Department of Education, Office of Special Education and Rehabilitative Services, Office of Special Education Programs . 27th Annual Report to Congress on the Implementation of the Individuals with Disabilities Education Act vol. 1. Office of Special Education and Rehabilitative Services U.S. Department of Education; Washington, D.C.: 2005. [Google Scholar]
- 9.U.S. Public Health Service . Report of the Surgeon General's Conference on Children's Mental Health: A National Action Agenda. Department of Health and Human Services; Washington, D.C.: 2000. [PubMed] [Google Scholar]
- 10.U.S. Department of Health and Human Services . Healthy People 2010. 2nd ed. With Understanding and Improving Health and Objectives for Improving Health. 2 vols. U.S. Department of Health and Human Services Office of Disease Prevention and Health Promotion; Washington, DC: 2000. [Google Scholar]
- 11.O'Connell ME, Boat T, Warner KE. Preventing Mental, Emotional, and BehavioralDisorders Among Young People: Progress and Possibilities. Institute of Medicine; National Research Council; 2009. The Committee on the Prevention of Mental Disorders and Substance Abuse Among Children Youth and Young Adults: Research Advances and Promising Interventions. [Google Scholar]
- 12.Institute of Medicine [August 13, 2010];Improving the quality of health care for mental and substance-use conditions: Quality chasm series. 2006 from IOM website: http://www.nap.edu/catalog.php?record_id=11470#toc. [PubMed]
- 13.President's New Freedom Commission on Mental Health [August 12, 2010];Final report to the president. 2003 from Preisdent's New Freedom Commision On Mental Health website: http://www.mentalhealthcommission.gov/reports/FinalReport/downloads/downloads.html.
- 14.Foy JM. Introduction. Pediatrics. 2010;125:S69–S74. doi: 10.1542/peds.2010-0788C. [DOI] [PubMed] [Google Scholar]
- 15.Costello EJ, Edelbrock C, Costello AJ, et al. Psychopathology in pediatric primary care: The new hidden morbidity. Pediatrics. 1988;82:415–424. [PubMed] [Google Scholar]
- 16.Hagan JFJ, Shaw JS, Duncan P, editors. Bright Futures Guidelines for Health Supervision of Infants, Children, and Adolescents - Third Edition. American Academy of Pediatrics; Elk Grove Village, IL: 2008. [Google Scholar]
- 17.Simonian S, Tarnowski K. Utility of the Pediatric Symptom Checklist for behavioral screening of disadvantaged children. Child Psychiatry Hum Dev. 2001;31(4):269–278. doi: 10.1023/a:1010213221811. [DOI] [PubMed] [Google Scholar]
- 18.Adams EK, Graver LJ. Medicaid Providers of Children's Preventive and PSDT Services, 1989 and 1992. Health Care Financing Review. 1998;19(4):5–23. [PMC free article] [PubMed] [Google Scholar]
- 19.Semansky RM, Koyanagi C, Vandivort-Warren R. Behavioral health screening policies in Medicaid programs nationwide. Psychiatr Serv. 2003;54(5):736–739. doi: 10.1176/appi.ps.54.5.736. [DOI] [PubMed] [Google Scholar]
- 20.Perkins J. Fact Sheet: Medicaid EPSDT Litigation. National Health Law Program; Chapel Hill, NC: 2009. [Google Scholar]
- 21.Ponsor MA, ROSIE D, et al. Mitt ROMNEY v., et al. Civil Action No. 01 30199 MAP. Boston, MA: 2006. United States District Court District of Massachusetts, ed. Legal Ruling 410 F.Supp.2d 18. [Google Scholar]
- 22.Smith S. Mentally ill children to get help at home: Judge approves plan to bolster state services. The Boston Globe. 2007 Globe Article. [Google Scholar]
- 23.Massachusetts Executive Office of Human Services MassHealth-Approved Standardized Behavioral Health Screening Tools For Children Under the Age of 21. http://www.mass.gov/Eeohhs2/docs/masshealth/cbhi/mh-approved-screening-tools.pdf.
- 24.Schonwald A. Developmental Screening Tool Kit for Primary Care Providers. http://www.developmentalscreening.org/billing_referring/billing_issues.htm.
- 25.Holt W. The Massachusetts Child Psychiatry Access Project: Supporting Mental Health Treatment in Primary Care. Commonwealth Fund; Boston, MA: 2010. [Google Scholar]
- 26.Sarvet B, Gold J, Bostic JQ, et al. Improving Access to Mental Health Care for Children: The Massachusetts Child Psychiatry Access Project. Pediatrics. 2010 Nov 8; doi: 10.1542/peds.2009-1340. [DOI] [PubMed] [Google Scholar]