Abstract
Trigeminal neuralgia is a syndrome of unilateral, paroxysmal, stabbing facial pain, originating from the trigeminal nerve. Careful history of typical symptoms is crucial for diagnosis. Most cases are caused by vascular compression of the trigeminal root adjacent to the pons leading to focal demyelination and ephaptic axonal transmission. Brain imaging is required to exclude secondary causes. Many medical and surgical treatments are available. Most patients respond well to pharmacotherapy; carbamazepine and oxcarbazepine are first line therapy, while lamotrigine and baclofen are considered second line treatments. Other drugs such as topiramate, levetiracetam, gabapentin, pregabalin, and botulinum toxin-A are alternative treatments. Surgical options are available if medications are no longer effective or tolerated. Microvascular decompression, gamma knife radiosurgery, and percutaneous rhizotomies are most promising surgical alternatives. This paper reviews the medical and surgical therapeutic options for the treatment of trigeminal neuralgia, based on available evidence and guidelines.
Trigeminal neuralgia (TN) is one of the most common causes of facial pain seen in dental and neurologic practices. This classic neuropathic pain disorder has been known for centuries.1 The International Headache Society (IHS) defines TN as a “unilateral disorder characterized by brief electric shock-like pains, abrupt in onset and termination, and limited to the distribution of one or more divisions of the trigeminal nerve”.2 The age of onset for most idiopathic cases is usually between 40 and 60 years, although onset may occur in the second and third decades, most often in females.3 Epidemiological studies reveal a global incidence of approximately 4-28.9 per 100,000 individuals.4-7 A variety of medical and surgical treatments are available for TN. Antiepileptic drugs (AEDs) are considered first line therapy for TN with different efficacy, and carbamazepine is the drug of choice.6-10 Surgical interventions are reserved for patients who do not respond to adequate medical therapy. Microvascular decompression (MVD), percutaneous trigeminal rhizotomies, and gamma knife radiosurgery (GKRS) are possibly effective in the treatment of TN.11
Etiology and pathogenesis
The cause of TN remains unclear.12,13 However, most cases are caused by compression of the trigeminal nerve root within a few millimeters of entry into the pons.9,14 The nerve impingement is often accompanied by a demyelination of sensory fibres within the nerve root or the root entry zone, or less commonly in the brainstem.15 Vascular compression by an aberrant loop of an artery or vein accounts for 80-90% of idiopathic TN.14 Other compressive causes are benign tumors of the posterior fossa such as acoustic neuroma, meningioma, and epidermoid cyst.9,16
Diagnosis
The diagnosis of TN is usually based on the characteristic clinical picture. The key feature is a sudden and severe lancinating pain, usually unilateral, precipitated by touching facial zones. This pain occurs in paroxysms, within the trigeminal nerve distribution; typically involving the maxillary nerve (V2) or mandibular nerve (V3) distribution and lasts for a fraction of a second to 2 minutes.9
Classification
The IHS divides TN into classic and symptomatic categories based on presumed etiology. Trigeminal neuralgia is termed classic (or idiopathic) when investigation identifies no cause other than a neurovascular compression; and examination shows no clinical evidence of neurological deficit. This accounts for 80-90% of TN cases.14 The classification symptomatic (or secondary) is reserved for patients with TN when major neurological diseases such as MS, skull deformity, or benign compressions in the posterior fossa have been identified.17-19 Neurological examination may show sensory impairment in trigeminal nerve distribution.2
Therapeutic modalities
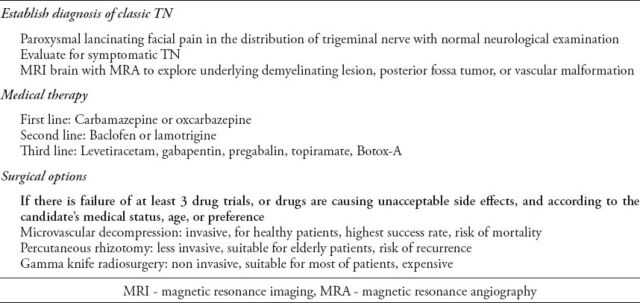
A huge variety of pharmacological and surgical treatments are available for TN. The practice parameters and guidelines published in 2008 from the American Academy of Neurology (AAN), and the European Federation of Neurological Societies (EFNS)11,20 recommend starting treatment with drugs in patients with classic TN (Table 1). Surgical procedures should be reserved for patients who are refractory to medical therapy or when drugs are causing unacceptable adverse effects. There are few studies directly comparing medical and surgical treatments. However, pharmacological therapy for TN has been the subject of several Cochrane systematic reviews,8,21,22 and available evidence shows carbamazepine is the best-studied treatment and drug of choice for initial and long-term management of classical TN.8,9,23 As far as symptomatic TN is concerned, to date, no placebo-controlled trials have evaluated and established effective treatment. However, it is advisable to treat symptomatic TN with the same drugs used in classical TN.
Table 1.
Clinical approach to the management of trigeminal neuralgia (TN).
Pharmacological therapy
Different medication has been considered for treatment of TN. Based on the level of evidence; carbamazepine and oxcarbazepine should be offered as a first line for pain control.11 There is limited evidence for efficacy of different AEDS to treat TN; other medications such as Baclofen and Botulinum toxin A seem promising treatment for this disorder.11
First-line therapy
According to current evidence-based treatment guidelines published in 2008 from the AAN and EFNS,20 carbamazepine is established as effective (level A) and oxcarbazepine is probably effective (level B) for controlling pain in classic TN. These guidelines recommend carbamazepine (200-1200 mg/d) and oxcarbazepine (600-1800 mg/d) as a first-line therapy for classic TN.
Carbamazepine
Carbamazepine acts by inhibiting voltage-gated sodium channels, thereby reducing the excitability of neural membranes. Carbamazepine has also been shown to potentiate gamma aminobutyric acid (GABA) receptors made up of alpha1, beta2, and gamma2 subunits. This may be relevant to its efficacy in neuropathic pain.24 In newly diagnosed cases of TN, the usual starting dose is 100 to 200 mg twice daily. The daily dose should be increased by 100 mg every other day until sufficient pain relief is attained or until intolerable side effects prevent further upward titration. The typical total maintenance dose is 300-800 mg/d, given in 2-3 divided doses. The maximum suggested total dose is 1200 mg/d. With appropriate dose adjustments, pain can be controlled in around 75% of patients.6,25 The dose may be tapered once pain is controlled, since remission may occur. Extended release carbamazepine is useful as a night dose in patients with pain attacks during sleep, as drug levels do not fall. This not only keeps patients pain free during sleep, but may reduce side effects, as high serum peaks are not achieved.26,27 Common side effects include sedation, dizziness, nausea, vomiting, diplopia, memory problems, ataxia, elevation of hepatic enzymes, and hyponatremia, which may contraindicate it for elderly patients. Potentially serious but uncommon side effects are carbamazepine-induced leucopenia, aplastic anemia, allergic rash, systemic lupus erythematosus, hepatotoxicity, and Stevens-Johnson syndrome (SJS). It is advisable to order complete blood count, serum sodium, and liver function tests within several weeks after starting therapy to detect any complications quickly.9,15
Oxcarbazepine
Oxcarbazepine is a keto-analogue of carbamazepine that is rapidly converted into its pharmacologically active 10-monohydroxy metabolite. The keto derivative of carbamazepine does not pass through the liver cytochrome system, resulting in an improved side effect profile and fewer drug interactions than with carbamazepine.28-30 Oxcarbazepine is an acceptable alternative to carbamazepine, which may have provided pain relief but has caused unacceptable adverse effects. Better tolerability can also be considered an advantage over carbamazepine.31 A systematic review from the American Academy of Neurology / European Federation of Neurological Societies (AAN/EFNS)11 identified several randomized controlled trials that compare oxcarbazepine with carbamazepine in patients with classic TN. Oxcarbazepine can be started at 150 mg twice daily. The dose can be increased as tolerated in 300 mg increments every third day until pain relief occurs. Maintenance doses range between 300-600 mg twice daily.26 The maximum suggested total dose is 1800 mg/d. The risk of allergic cross reactivity between carbamazepine and oxcarbazepine is around 25%, so oxcarbazepine is best avoided when carbamazepine allergy is evident.9
Second-line therapy
Second-line treatment is based on very little evidence. Three drugs are included in this class - lamotrigine, baclofen, and pimozide. Each drug has been studied in single trials,32-34 and per AAN/EFNS guidelines, are possibly effective (level C) for controlling pain in patients with classic TN.20
Lamotrigine
This AED has been used in only one small, double-blind, placebo-controlled trial34 investigating 14 patients with TN who were refractory to carbamazepine, where adjunct therapy with lamotrigine (400 mg/d) was beneficial and more effective than placebo. While in an open-label study, 11 of 15 patients with TN found pain relief with 400 mg of lamotrigine.35 The initial dose of lamotrigine is 25 mg twice daily, and can be increased gradually to a maintenance dose of 200-400 mg/d in 2 divided doses.15 The dosage required for adequate pain relief varied widely from 100-400 mg/d.35 Common side effects are sleepiness, dizziness, headache, vertigo, and ataxia. Some (7-10%) of patients report a skin rash during the first 1-2 months of treatment that most often resolves with continued therapy.36 Stevens-Johnson syndrome can occur in one in 10,000 patients taking lamotrigine.15 Such adverse reactions can be prevented by slower titration of the drug.
Baclofen
Baclofen, a skeletal muscle relaxant, is a GABA analogue that activates GABAB receptors and thus depresses excitatory neurotransmission.26 It is effective in controlling pain in TN at a dose of 60-80 mg/d. Baclofen can be used alone or in combination with carbamazepine. Studies have supported its benefit in both conditions.37 The initial dose is 10 mg/d for 3 days, which can be increased to 10-20 /d every 3 days if needed. The maximum tolerated dose is 60-80 mg/d, administered 3-4 times per day.37 If baclofen is an add-on therapy with carbamazepine, it is advisable to reduce the dose of carbamazepine to 500 mg/d to maintain a putative synergistic effect.38 Typical side effects of baclofen include drowsiness, dizziness, weakness, fatigue, nausea, hypotension, and constipation. Abrupt discontinuation of baclofen can cause withdrawal symptoms (hallucinations and seizures).15 Patients with MS and trigeminal neuralgia obtain additional benefits with baclofen because it is a muscle relaxant.39 To date, baclofen has the strongest evidence for efficacy in the treatment of TN after carbamazepine.15
Pimozide
Pimozide, a dopamine receptor antagonist, is used mainly in the management of Tourette syndrome. It was found effective in a randomized, double-blind crossover trial 40 of 48 patients with refractory TN. In this trial, pimozide achieved pain control in all 48 patients. While displaying encouraging results, pimozide, at a dose of 2-12 mg/d in TN treatment, is seldom used clinically because it has multiple potential serious side effects, including, arrhythmias, acute extrapyramidal symptoms, and Parkinsonism.
Third-line therapy
The newer AEDs tested within the past few years are gabapentin, pregabalin, topiramate, and levetiracetam.26
Gabapentin
Gabapentin, a GABA receptor agonist, acts primarily on presynaptic calcium channels of neurons to inhibit the release of excitatory neurotransmitters. Gabapentin has been used in randomized control trials (RCTs) of neuropathic pain and was proven effective.40 Its use and effectiveness were also reported in several TN studies.41,42 Gabapentin showed adequate efficacy in only one RCT, where it was used in combination with ropivacaine.43 This combination was found to be safe and effective. Gabapentin also has demonstrated effectiveness with sustained relief in TN, especially in patients with MS.43 Treatment can be started at a dose of 300 mg/d, and may be gradually increased by 300 mg every 2-3 days as tolerated. For maximum efficacy, the dose can be increased to 1800 mg/d.15,44 Gabapentin has many advantages, including faster titration, no known drug interactions, no known idiosyncratic skin reactions, and a favorable side-effect profile, with mild somnolence, dizziness, headache, confusion, nausea, and ankle edema.29 Hyperlipidemia is an important side effect to watch for with gabapentin therapy.29
Pregabalin
Pregabalin is an analog of GABA, structurally related to gabapentin. It acts by interacting with the alpha-2-delta (α2-δ) subunit of voltage-gated calcium channels.45 Although a potentially useful drug for neuropathic pain in some patients, evidence is scant in TN. It has been tested and found effective only in a single open-label study.46 In this well-designed cohort study, pregabalin (150-600 mg/d) was tested in 53 patients over one year, and proved to be effective in reducing TN pain by more than 50-74% of patients.46 Side effects are similar to other AEDs but less marked; most common are dizziness and sleepiness.40
Topiramate
The exact mechanism of action of topiramate is unknown. However, its pain-modulating effect might be related to its property of blockage of the voltage-gated sodium channel and an augmentation of GABA activity by binding to a non benzodiazepine site on the GABAA receptor.15 Topiramate (100-400 mg/d) was found effective in 75% of patients in one study of 8 patients with classic TN.47 A recent meta-analysis48 evaluated the effectiveness and safety of topiramate with carbamazepine in the treatment of classic TN. In this analysis, 6 RCTs involving 354 patients were included. A meta-analysis of these studies showed the overall effectiveness and tolerability of topiramate did not seem to differ from carbamazepine in the treatment of classic TN. In this analysis the results were limited due to the poor methodological quality of these RCTs. The most frequently registered side effects of topiramate were dizziness, somnolence, cognitive impairment, and weight loss.29
Levetiracetam
Levetiracetam is a newer AED that has been tried in TN. The exact mechanism by which it acts is unknown, but it is thought to target high-voltage, N-type calcium channels as well as the synaptic vesicle protein 2A (SV2A); by this, it impedes impulse conduction across synapses.49 Its evidence in TN is scant. Recently, 2 pilot, open-label studies investigated the efficacy and tolerability of levetiracetam in patients with TN. One study with 10 patients reported an improvement of 50-90%.49 Another study with 23 patients reported a 62% reduction in number of daily attacks in patients receiving levetiracetam as add-on therapy.50 The effective dose range of levetiracetam in TN is 1000-4000 mg/d. Levetiracetam has advantages, including no need for routine blood tests, less drugs interactions,11 the absence of auto-induction effect, nasopharyngitis, sleepiness, headaches, and irritability are side effects when starting levetiracetam.29,51 Although evidence suggests good efficacy and safety for levetiracetam in medical treatment of TN, a wide-range of randomized and placebo-controlled trials are warranted before making any definitive claim.
Botulinum toxin A
Botulinum toxin A (BTX-A) has been thoroughly studied as a potential tool in the treatment of several pain syndromes, such as migraine, tension headache, occipital, and postherpetic neuralgias.52,53 The BTX-A’s mechanism of analgesic effect is still unclear, but it is postulated it causes local release of anti-nociceptive neuropeptides such as substance P, glutamate, and calcitonin-gene related peptide, inhibiting central and possibly peripheral sensitization.54 Its therapeutic efficacy and safety has been reviewed recently.55 In this systemic review, they identified one double-blind RCT study56 and 5 prospective open-labelled studies.57-61 This systemic review found subcutaneous or mucosal injection of BTX-A effective for adult TN patients, and the results of the 2 RCTs showed significant benefit over placebo. Response was achieved in approximately 70-100% of patients, and mean pain intensity and frequency were reduced by approximately 60-100% at 4 weeks after injection in most studies. In one study,58 47% of patients didn’t need further treatment, 33% patients required nonsteroidal anti-inflammatory drugs to alleviate pain, while 20% responded to the AED after receiving a BTX-A injection. The most commonly used dose of BTX-A was 20-75U, however, patients also showed significant reduction in intensity of pain at lower doses (6-9U).57 Based on this available limited evidence, BTX-A seems promising treatment of TN. However, well-designed RCT studies are required to determine the therapeutic efficacy, optimal dose, time, and indications for repeat injections of BTX-A.
Other drugs
A number of other drugs have been tried in treating TN, showing limited benefit such as phenytoin and intravenous phenytoin, fosphenytoin, clonazepam, valproic acid, misoprostol, tocainide, topical capsaicin cream, intranasal lidocaine, tizanidine, sumatriptan, and amitriptyline.62-66
Surgical treatment
Surgical interventions are reserved for the candidate with incapacitating symptoms of TN despite a trial of at least 3 drugs in sufficient dosage or where medications caused unacceptable adverse effects.67 Relapse of symptoms might also be another strong factor in opting for surgical treatment. It is estimated that up to 50% of patients with TN will require some form of surgery sooner or later.25,68 According to practice parameters from the AAN and EFNS,11 microvascular decompression (MVD), percutaneous rhizotomy on the Gasserian ganglion, and gamma knife radiosurgery (GKRS) may possibly be effective in the treatment of TN, while evidence for peripheral neurectomy is inconclusive.
Microvascular decompression
Among all surgical procedures, MVD is the most invasive surgery, but offers the highest success rate of pain-free status in patients with classic TN.20,69 Generally it is reserved for the patient with TN who is otherwise, healthy and has no other major medical problems, or for patients who may have failed less invasive procedures such as radiosurgery and rhizotomy. It is carried out under general anesthesia (GA), involves retrosigmoid craniotomy and microsurgical exploration of the posterior fossa. A systemic review by AAN/EFNS identified 5 studies on MVD for TN.20 The studies concluded 90% of patients experience initial pain relief; more than 80% are still pain free after one year, with 75% pain free after 3 years, and 73% after 5 years.11,26 In this review, the most common complication was aseptic meningitis (11%), followed by long-term hearing loss (10%), and sensory loss (7%). Major adverse events were noted in 4% of patients in the form of cerebrospinal fluid leaks, infarction, or hematoma. Although complication rates were low, this surgical option has a small risk of death (around 0.20-0.4%).68
Percutaneous rhizotomy on the Gasserian ganglion
There are 3 common percutaneous rhizotomies: radiofrequency thermal rhizotomy (that creates a lesion through application of heat), chemical rhizotomy (by injecting 0.1 to 0.4 mL of glycerol into the trigeminal cistern), and mechanical rhizotomy or micro compression (by inflating a balloon into Meckel’s cave to compress the Gasserian ganglion). These techniques are performed by passing a cannula through the foramen ovale, followed by controlled lesion of the trigeminal ganglion or root.68 The goal of these rhizotomies is selective destruction of pain fibers (A-delta and C-fibers) while preserving touch fibers (A-alpha, and beta fibers) in the trigeminal nerve.67 The systemic review by the AAN/EFNS identified 4 uncontrolled case studies of these percutaneous procedures,11 and concluded initial pain relief is achieved in 90% of patients, but pain free rates decline gradually in successive years, and after 5 years only 50% of patients are pain free. The most common complication reported are trigeminal distribution sensory loss (50%), followed by dysesthesias (6%), anesthesia dolorosa (4%), characterized by persistent, painful anesthesia, or hypesthesia in the denervated region, corneal numbness with risk of keratitis (4%), aseptic meningitis (0.2%), and extremely low mortality.11,20 Percutaneous procedures are less invasive and have relative advantages and disadvantages.25 They are used to a greater extent in patients with high operative risks such as in elderly or ill patients or as a partially diagnostic procedure in atypical disease.9 All these procedures are associated with significant risk of recurrence.70,71
Gamma knife radiosurgery
The GKRS has recently been established as an effective treatment for TN.72 It is a noninvasive outpatient procedure in which a high dose (70-90 Gy) of a highly focused52 beam of radiation is delivered at the trigeminal root entry zone, which over time causes axonal degeneration and necrosis and thus interrupts pain signals.73 The success of GKRS demands a very accurate stereotactic system. The AAN/EFNS systemic review11 identified 3 case series of GKRS that used independent outcome assessment,74-76 revealing 69% of patients are pain free at one year after radiosurgery, and 52% are still pain free at 3 years. Pain relief can be delayed (mean one month) with this procedure. Side effects are facial numbness (9-37%), which improves over time, and bothersome sensory loss or paresthesia (6-13%) that may develop with a delay of up to 6 months. Quality of life improves by 88%.77 The non invasive nature of GKRS provides many advantages, and makes it available for patients who cannot opt for MVD because of multiple medical comorbidities, are on anticoagulation therapy, or are unwilling to take anticonvulsants.67 The treatment is expensive, which limits its widespread use.
In conclusion, TN is one of the most painful, but readily treatable conditions, whose diagnosis is based purely on clinical grounds by characteristic symptoms and signs. Many medical and surgical treatments are available; however, only a few of them have proven their efficacy to modern evidence-based medicine standards. The AEDs form the mainstay of treatment, among them carbamazepine is the gold standard. Newer drugs such as gabapentin, pregabalin, topiramate, levetiracetam, and botulinum toxin-A are promising and effective with fewer side effects, better efficacy, and tolerability. However, there is still no existing evidence to use them as first-line therapy. Medically refractory cases and patients who cannot tolerate the side effects of medication may benefit from surgical management. Microvascular decompression remains the best approach in patients when MRI shows a loop of the aberrant vessel. Other options are percutaneous ablative procedure and GKRS. The selection of the surgical procedure needs to be individualized, depending upon patient’s preference, age, underlying pathology, and comorbidities. There is a need for wide-ranged randomized and placebo-controlled trials with long-term-follow up to establish the stepwise, standardized medical regimen after failure of first-line medical therapy, to compare surgical and medical therapies, and to determine the optimal timing for surgical intervention.
Footnotes
Related articles
Erbagci H, Kizilkan N, Sirikci A, Yigiter R, Aksamoglu M. Computed tomography based measurement of the dimensions of foramen ovale and rotundum in trigeminal neuralgia. Neurosciences 2010; 15: 101-104.
Ganz J. Gamma Knife Surgery for Epilepsy and Trigeminal Neuralgia. Neurosciences 2004; 9: S39.
Reda WA, Moharem H, Hamad H, Hay AA. Treatment of idiopathic trigeminal neuralgia: Comparison of outcome after radiofrequency rhizotomy and microvascular decompression. Neurosciences 2003; 8: 23-25.
References
- 1.Adams F, editor. The extant works of Aretaeus, the Cappadocian. London (UK): Sydenhem Society; 1856. [Google Scholar]
- 2.Headache Classification Subcommittee of the International Headache Society. The International Classification of Headache Disorders: 2nd edition. Cephalalgia. 2004;24:9–160. doi: 10.1111/j.1468-2982.2003.00824.x. [DOI] [PubMed] [Google Scholar]
- 3.Childs AM, Meaney JF, Ferrie CD, Holland PC. Neurovascular compression of the trigeminal and glossopharyngeal nerve: three case reports. Arch Dis Child. 2000;82:311–315. doi: 10.1136/adc.82.4.311. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Dieleman JP, Kerklaan J, Huygen FJ, Bouma PA, Sturkenboom MC. Incidence rates and treatment of neuropathic pain conditions in the general population. Pain. 2008;137:681–688. doi: 10.1016/j.pain.2008.03.002. [DOI] [PubMed] [Google Scholar]
- 5.Koopman JS, Dieleman JP, Huygen FJ, de Mos M, Martin CG, Sturkenboom MC. Incidence of facial pain in the general population. Pain. 2009;147:122–127. doi: 10.1016/j.pain.2009.08.023. [DOI] [PubMed] [Google Scholar]
- 6.Katusic S, Williams DB, Beard CM, Bergstralh EJ, Kurland LT. Epidemiology and clinical features of idiopathic trigeminal neuralgia and glossopharyngeal neuralgia: similarities and differences, Rochester, Minnesota, 1945-1984. Neuroepidemiology. 1991;10:276–281. doi: 10.1159/000110284. [DOI] [PubMed] [Google Scholar]
- 7.Hall GC, Carroll D, McQuay HJ. Primary care incidence and treatment of four neuropathic pain conditions: a descriptive study 2002-2005. BMC Fam Pract. 2008;9:26. doi: 10.1186/1471-2296-9-26. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Wiffen PJ, McQuay HJ, Moore RA. Carbamazepine for acute and chronic pain. Cochrane Database Syst Rev. 2005;3:CD005451. doi: 10.1002/14651858.CD005451. [DOI] [PubMed] [Google Scholar]
- 9.Bennetto L, Patel NK, Fuller G. Trigeminal neuralgia and its management. BMJ. 2007;334:201. doi: 10.1136/bmj.39085.614792.BE. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Wiffen PJ, Derry S, Moore RA, McQuay HJ. Carbamazepine for acute and chronic pain in adults. Cochrane Database Syst Rev. 2011;1:CD005451. doi: 10.1002/14651858.CD005451.pub2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Gronseth G, Cruccu G, Alksne J, Argoff C, Brainin M, Burchiel K, et al. Practice parameter: the diagnostic evaluation and treatment of trigeminal neuralgia (an evidence-based review): report of the Quality Standards Subcommittee of the American Academy of Neurology and the European Federation of Neurological Societies. Neurology. 2008;71:1183–1190. doi: 10.1212/01.wnl.0000326598.83183.04. [DOI] [PubMed] [Google Scholar]
- 12.Devor M, Amir R, Rappaport ZH. Pathophysiology of trigeminal neuralgia: the ignition hypothesis. Clin J Pain. 2002;18:4–13. doi: 10.1097/00002508-200201000-00002. [DOI] [PubMed] [Google Scholar]
- 13.Zakrzewska JM, Linskey ME. Trigeminal neuralgia. BMJ Clin Evid. 2009;2009:1207. [PMC free article] [PubMed] [Google Scholar]
- 14.Love S, Coakham HB. Trigeminal neuralgia: pathology and pathogenesis. Brain. 2001;124:2347–2360. doi: 10.1093/brain/124.12.2347. [DOI] [PubMed] [Google Scholar]
- 15.Hassan S, Khan NI, Sherwani OA, Bhatt W, Asif S. Trigeminal neuralgia: an overview of literature with emphasis on medical management. Int Research J Pharmcol. 2013;3:235–238. [Google Scholar]
- 16.El Otmani H, Moutaouakil F, Fadel H, Slassi I. [Familial trigeminal neuralgia] Rev Neurol (Paris) 2008;164:384–387. doi: 10.1016/j.neurol.2007.10.010. French. [DOI] [PubMed] [Google Scholar]
- 17.Ali FM, Prasant M, Pai D, Aher VA, Kar S, Safiya T. Peripheral neurectomies: A treatment option for trigeminal neuralgia in rural practice. J Neurosci Rural Pract. 2012;3:152–157. doi: 10.4103/0976-3147.98218. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Cruccu G, Truini A. Refractory trigeminal neuralgia. Non-surgical treatment options. CNS Drugs. 2013;27:91–96. doi: 10.1007/s40263-012-0023-0. [DOI] [PubMed] [Google Scholar]
- 19.Nurmikko TJ, Eldridge PR. Trigeminal neuralgia--pathophysiology, diagnosis and current treatment. Br J Anaesth. 2001;87:117–132. doi: 10.1093/bja/87.1.117. [DOI] [PubMed] [Google Scholar]
- 20.Cruccu G, Gronseth G, Alksne J, Argoff C, Brainin M, Burchiel K, et al. AAN-EFNS guidelines on trigeminal neuralgia management. Eur J Neurol. 2008;15:1013–1028. doi: 10.1111/j.1468-1331.2008.02185.x. [DOI] [PubMed] [Google Scholar]
- 21.Wiffen P, Collins S, McQuay H, Carroll D, Jadad A, Moore A. Anticonvulsant drugs for acute and chronic pain. Cochrane Database Syst Rev. 2005;3:CD001133. doi: 10.1002/14651858.CD001133.pub2. [DOI] [PubMed] [Google Scholar]
- 22.Wiffen PJ, McQuay HJ, Edwards JE, Moore RA. Gabapentin for acute and chronic pain. Cochrane Database Syst Rev. 2005;3:CD005452. doi: 10.1002/14651858.CD005452. [DOI] [PubMed] [Google Scholar]
- 23.Zakrzewska JM, Lopez BC. Trigeminal neuralgia. Clin Evid. 2005;14:1669–1677. [PubMed] [Google Scholar]
- 24.Granger P, Biton B, Faure C, Vige X, Depoortere H, Graham D, et al. Modulation of the gamma-aminobutyric acid type A receptor by the antiepileptic drugs carbamazepine and phenytoin. Mol Pharmacol. 1995;47:1189–1196. [PubMed] [Google Scholar]
- 25.Joffroy A, Levivier M, Massager N. Trigeminal neuralgia. Pathophysiology and treatment. Acta Neurol Belg. 2001;101:20–25. [PubMed] [Google Scholar]
- 26.Obermann M. Treatment options in trigeminal neuralgia. Ther Adv Neurol Disord. 2010;3:107–115. doi: 10.1177/1756285609359317. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Devor M, Wood I, Sharav Y, Zakrzewska JM. Trigeminal neuralgia during sleep. Pain Pract. 2008;8:263–268. doi: 10.1111/j.1533-2500.2008.00214.x. [DOI] [PubMed] [Google Scholar]
- 28.Ferrell PB, Jr, McLeod HL. Carbamazepine, HLA-B*1502 and risk of Stevens-Johnson syndrome and toxic epidermal necrolysis: US FDA recommendations. Pharmacogenomics. 2008;9:1543–1546. doi: 10.2217/14622416.9.10.1543. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.George M, Selvarajan S, Indumathi C. Drug therapy for trigeminal neuralgia. e-Journal of Dentistry. 2011;1:28–31. [Google Scholar]
- 30.Martinez W, Ingenito A, Blakeslee M, Barkley GL, McCague K, D’Souza J. Efficacy, safety, and tolerability of oxcarbazepine monotherapy. Epilepsy Behav. 2006;9:448–456. doi: 10.1016/j.yebeh.2006.04.022. [DOI] [PubMed] [Google Scholar]
- 31.Beydoun A. Safety and efficacy of oxcarbazepine: results of randomized, double-blind trials. Pharmacotherapy. 2000;20:152S–158S. doi: 10.1592/phco.20.12.152s.35254. [DOI] [PubMed] [Google Scholar]
- 32.Fromm GH, Terrence CF, Chattha AS. Baclofen in the treatment of trigeminal neuralgia: double-blind study and long-term follow-up. Ann Neurol. 1984;15:240–244. doi: 10.1002/ana.410150306. [DOI] [PubMed] [Google Scholar]
- 33.Lechin F, van der Dijs B, Lechin ME, Amat J, Lechin AE, Cabrera A, et al. Pimozide therapy for trigeminal neuralgia. Arch Neurol. 1989;46:960–963. doi: 10.1001/archneur.1989.00520450030015. [DOI] [PubMed] [Google Scholar]
- 34.Zakrzewska JM, Chaudhry Z, Nurmikko TJ, Patton DW, Mullens EL. Lamotrigine (lamictal) in refractory trigeminal neuralgia: results from a double-blind placebo controlled crossover trial. Pain. 1997;73:223–230. doi: 10.1016/S0304-3959(97)00104-8. [DOI] [PubMed] [Google Scholar]
- 35.Lunardi G, Leandri M, Albano C, Cultrera S, Fracassi M, Rubino V, et al. Clinical effectiveness of lamotrigine and plasma levels in essential and symptomatic trigeminal neuralgia. Neurology. 1997;48:1714–1717. doi: 10.1212/wnl.48.6.1714. [DOI] [PubMed] [Google Scholar]
- 36.Wiffen PJ, Rees J. Lamotrigine for acute and chronic pain. Cochrane Database Syst Rev. 2007;2:CD006044. doi: 10.1002/14651858.CD006044.pub2. [DOI] [PubMed] [Google Scholar]
- 37.Fromm GH, Terrence CF, Chattha AS, Glass JD. Baclofen in trigeminal neuralgia: its effect on the spinal trigeminal nucleus: a pilot study. Arch Neurol. 1980;37:768–771. doi: 10.1001/archneur.1980.00500610048007. [DOI] [PubMed] [Google Scholar]
- 38.Parekh S, Shah K, Kotdawalla H. Baclofen in carbamazepine resistant trigeminal neuralgia - a double-blind clinical trial. Cephalalgia. 1989;9:392–393. [Google Scholar]
- 39.Leandri M. Therapy of trigeminal neuralgia secondary to multiple sclerosis. Expert Rev Neurother. 2003;3:661–671. doi: 10.1586/14737175.3.5.661. [DOI] [PubMed] [Google Scholar]
- 40.Zakrzewska JM. Medical management of trigeminal neuropathic pains. Expert Opin Pharmacother. 2010;11:1239–1254. doi: 10.1517/14656561003767449. [DOI] [PubMed] [Google Scholar]
- 41.Cheshire WP., Jr Defining the role for gabapentin in the treatment of trigeminal neuralgia: a retrospective study. J Pain. 2002;3:137–142. doi: 10.1054/jpai.2002.122944. [DOI] [PubMed] [Google Scholar]
- 42.Serpell MG Neuropathic pain study group. Gabapentin in neuropathic pain syndromes: a randomised, double-blind, placebo-controlled trial. Pain. 2002;99:557–566. doi: 10.1016/S0304-3959(02)00255-5. [DOI] [PubMed] [Google Scholar]
- 43.Khan OA. Gabapentin relieves trigeminal neuralgia in multiple sclerosis patients. Neurology. 1998;51:611–614. doi: 10.1212/wnl.51.2.611. [DOI] [PubMed] [Google Scholar]
- 44.Backonja M, Glanzman RL. Gabapentin dosing for neuropathic pain: evidence from randomized, placebo-controlled clinical trials. Clin Ther. 2003;25:81–104. doi: 10.1016/s0149-2918(03)90011-7. [DOI] [PubMed] [Google Scholar]
- 45.Rodríguez MJ, Díaz S, Vera-Llonch M, Dukes E, Rejas J. Cost-effectiveness analysis of pregabalin versus gabapentin in the management of neuropathic pain due to diabetic polyneuropathy or post-herpetic neuralgia. Curr Med Res Opin. 2007;23:2585–2596. doi: 10.1185/030079907X233151. [DOI] [PubMed] [Google Scholar]
- 46.Obermann M, Yoon MS, Sensen K, Maschke M, Diener HC, Katsarava Z. Efficacy of pregabalin in the treatment of trigeminal neuralgia. Cephalalgia. 2008;28:174–181. doi: 10.1111/j.1468-2982.2007.01483.x. [DOI] [PubMed] [Google Scholar]
- 47.Domingues RB, Kuster GW, Aquino CC. Treatment of trigeminal neuralgia with low doses of topiramate. Arq Neuropsiquiatr. 2007;65:792–794. doi: 10.1590/s0004-282x2007000500011. [DOI] [PubMed] [Google Scholar]
- 48.Wang QP, Bai M. Topiramate versus carbamazepine for the treatment of classical trigeminal neuralgia: a meta-analysis. CNS Drugs. 2011;25:847–857. doi: 10.2165/11595590-000000000-00000. [DOI] [PubMed] [Google Scholar]
- 49.Jorns TP, Johnston A, Zakrzewska JM. Pilot study to evaluate the efficacy and tolerability of levetiracetam (Keppra) in treatment of patients with trigeminal neuralgia. Eur J Neurol. 2009;16:740–744. doi: 10.1111/j.1468-1331.2009.02585.x. [DOI] [PubMed] [Google Scholar]
- 50.Mitsikostas DD, Pantes GV, H Avramidis TG, Karageorgiou KE, Gatzonis SD, Stathis PG, et al. An observational trial to investigate the efficacy and tolerability of levetiracetam in trigeminal neuralgia. Headache. 2010;50:1371–1377. doi: 10.1111/j.1526-4610.2010.01743.x. [DOI] [PubMed] [Google Scholar]
- 51.Brodie MJ, Perucca E, Ryvlin P, Ben-Menachem E, Meencke HJ Levetiracetam Monotherapy Study Group. Comparison of levetiracetam and controlled-release carbamazepine in newly diagnosed epilepsy. Neurology. 2007;68:402–408. doi: 10.1212/01.wnl.0000252941.50833.4a. [DOI] [PubMed] [Google Scholar]
- 52.Frampton JE. OnabotulinumtoxinA (BOTOX®): a review of its use in the prophylaxis of headaches in adults with chronic migraine. Drugs. 2012;72:825–845. doi: 10.2165/11208880-000000000-00000. [DOI] [PubMed] [Google Scholar]
- 53.Porta M, Camerlingo M. Headache and botulinum toxin. J Headache Pain. 2005;6:325–327. doi: 10.1007/s10194-005-0222-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Aoki KR. Review of a proposed mechanism for the antinociceptive action of botulinum toxin type A. Neurotoxicology. 2005;26:785–793. doi: 10.1016/j.neuro.2005.01.017. [DOI] [PubMed] [Google Scholar]
- 55.Hu Y, Guan X, Fan L, Li M, Liao Y, Nie Z, et al. Therapeutic efficacy and safety of botulinum toxin type A in trigeminal neuralgia: a systematic review. J Headache Pain. 2013;14:72. doi: 10.1186/1129-2377-14-72. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Wu CJ, Lian YJ, Zheng YK, Zhang HF, Chen Y, Xie NC, et al. Botulinum toxin type A for the treatment of trigeminal neuralgia: results from a randomized, double-blind, placebo-controlled trial. Cephalalgia. 2012;32:443–450. doi: 10.1177/0333102412441721. [DOI] [PubMed] [Google Scholar]
- 57.Piovesan EJ, Teive HG, Kowacs PA, Della Coletta MV, Werneck LC, Silberstein SD. An open study of botulinum-A toxin treatment of trigeminal neuralgia. Neurology. 2005;65:1306–1308. doi: 10.1212/01.wnl.0000180940.98815.74. [DOI] [PubMed] [Google Scholar]
- 58.Bohluli B, Motamedi MH, Bagheri SC, Bayat M, Lassemi E, Navi F, et al. Use of botulinum toxin A for drug-refractory trigeminal neuralgia: preliminary report. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 2011;111:47–50. doi: 10.1016/j.tripleo.2010.04.043. [DOI] [PubMed] [Google Scholar]
- 59.Zúñiga C, Díaz S, Piedimonte F, Micheli F. Beneficial effects of botulinum toxin type A in trigeminal neuralgia. Arq Neuropsiquiatr. 2008;66:500–503. doi: 10.1590/s0004-282x2008000400012. [DOI] [PubMed] [Google Scholar]
- 60.Türk U, Ilhan S, Alp R, Sur H. Botulinum toxin and intractable trigeminal neuralgia. Clin Neuropharmacol. 2005;28:161–162. doi: 10.1097/01.wnf.0000172497.24770.b0. [DOI] [PubMed] [Google Scholar]
- 61.Borodic GE, Acquadro MA. The use of botulinum toxin for the treatment of chronic facial pain. J Pain. 2002;3:21–27. doi: 10.1054/jpai.2002.27142. [DOI] [PubMed] [Google Scholar]
- 62.McCleane GJ. Intravenous infusion of phenytoin relieves neuropathic pain: a randomized, double-blinded, placebo-controlled, crossover study. Anesth Analg. 1999;89:985–988. doi: 10.1097/00000539-199910000-00030. [DOI] [PubMed] [Google Scholar]
- 63.Cheshire WP. Fosphenytoin: an intravenous option for the management of acute trigeminal neuralgia crisis. J Pain Symptom Manage. 2001;21:506–510. doi: 10.1016/s0885-3924(01)00269-x. [DOI] [PubMed] [Google Scholar]
- 64.Kanai A, Suzuki A, Kobayashi M, Hoka S. Intranasal lidocaine 8% spray for second-division trigeminal neuralgia. Br J Anaesth. 2006;97:559–563. doi: 10.1093/bja/ael180. [DOI] [PubMed] [Google Scholar]
- 65.Kanai A, Saito M, Hoka S. Subcutaneous sumatriptan for refractory trigeminal neuralgia. Headache. 2006;46:577–582. doi: 10.1111/j.1526-4610.2006.00405.x. discussion 583-584. [DOI] [PubMed] [Google Scholar]
- 66.Yang M, Zhou M, He L, Chen N, Zakrzewska JM. Non-antiepileptic drugs for trigeminal neuralgia. Cochrane Database Syst Rev. 2011;1:CD004029. doi: 10.1002/14651858.CD004029.pub3. [DOI] [PubMed] [Google Scholar]
- 67.Hodaie M, Coello AF. Advances in the management of trigeminal neuralgia. J Neurosurg Sci. 2013;57:13–21. [PubMed] [Google Scholar]
- 68.Pollock BE. Surgical management of medically refractory trigeminal neuralgia. Curr Neurol Neurosci Rep. 2012;12:125–131. doi: 10.1007/s11910-011-0242-7. [DOI] [PubMed] [Google Scholar]
- 69.Bohnstedt BN, Tubbs RS, Cohen-Gadol AA. The use of intraoperative navigation for percutaneous procedures at the skull base including a difficult-to-access foramen ovale. Neurosurgery. 2012;70:177–180. doi: 10.1227/NEU.0b013e3182309448. [DOI] [PubMed] [Google Scholar]
- 70.Udupi BP, Chouhan RS, Dash HH, Bithal PK, Prabhakar H. Comparative evaluation of percutaneous retrogasserian glycerol rhizolysis and radiofrequency thermocoagulation techniques in the management of trigeminal neuralgia. Neurosurgery. 2012;70:407–412. doi: 10.1227/NEU.0b013e318233a85f. discussion 412-413. [DOI] [PubMed] [Google Scholar]
- 71.Koopman JS, de Vries LM, Dieleman JP, Huygen FJ, Stricker BH, Sturkenboom MC. A nationwide study of three invasive treatments for trigeminal neuralgia. Pain. 2011;152:507–513. doi: 10.1016/j.pain.2010.10.049. [DOI] [PubMed] [Google Scholar]
- 72.Gorgulho AA, De Salles AA. Impact of radiosurgery on the surgical treatment of trigeminal neuralgia. Surg Neurol. 2006;66:350–356. doi: 10.1016/j.surneu.2006.03.046. [DOI] [PubMed] [Google Scholar]
- 73.Sheehan J, Pan HC, Stroila M, Steiner L. Gamma knife surgery for trigeminal neuralgia: outcomes and prognostic factors. J Neurosurg. 2005;102:434–441. doi: 10.3171/jns.2005.102.3.0434. [DOI] [PubMed] [Google Scholar]
- 74.Petit JH, Herman JM, Nagda S, DiBiase SJ, Chin LS. Radiosurgical treatment of trigeminal neuralgia: evaluating quality of life and treatment outcomes. Int J Radiat Oncol Biol Phys. 2003;56:1147–1153. doi: 10.1016/s0360-3016(03)00264-5. [DOI] [PubMed] [Google Scholar]
- 75.Régis J, Metellus P, Hayashi M, Roussel P, Donnet A, Bille-Turc F. Prospective controlled trial of gamma knife surgery for essential trigeminal neuralgia. J Neurosurg. 2006;104:913–924. doi: 10.3171/jns.2006.104.6.913. [DOI] [PubMed] [Google Scholar]
- 76.Lopez BC, Hamlyn PJ, Zakrzewska JM. Stereotactic radiosurgery for primary trigeminal neuralgia: state of the evidence and recommendations for future reports. J Neurol Neurosurg Psychiatry. 2004;75:1019–1024. doi: 10.1136/jnnp.2003.018564. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 77.Kondziolka D, Zorro O, Lobato-Polo J, Kano H, Flannery TJ, Flickinger JC, et al. Gamma Knife stereotactic radiosurgery for idiopathic trigeminal neuralgia. J Neurosurg. 2010;112:758–765. doi: 10.3171/2009.7.JNS09694. [DOI] [PubMed] [Google Scholar]