Summary:
Primary chronic osteomyelitis of the mandible is a rare condition that presents with a long-standing chronic facial swelling over the mandible, pain with mastication, and trismus. With no clinically appreciated acute phase, the aetiology often remains unknown. Many patients achieve adequate symptom control with broad-spectrum antibiotics, hyperbaric oxygen therapy and surgical debridement, or decortication of bone sequestration. However, because of the rarity of primary chronic osteomyelitis and the extensive involvement of the mandible that can result, we present a case of a 32-year-old woman with chronic disease of the left mandible requiring a left hemimandibulectomy and fibular free flap reconstruction. Few such cases have been reported in the literature, which require such extensive resection and reconstruction to control long-standing symptoms.
Primary chronic osteomyelitis (PCO) of the mandible is a rare nonsuppurative inflammatory condition of unknown aetiology. Patients presenting with PCO usually complain of episodic pain, trismus, and facial swelling. Symptoms may last from days to many weeks. The intensity of symptoms can vary with each exacerbation and between episodes, and there may be no clinically significant symptoms. PCO has an insidious onset and may have a subacute or no acute phase of note. Currently, literature suggests that the aetiology of the condition is infection by low virulence microorganisms causing an exaggerated immune response in predisposed individuals.1,2
Standard of care treatment includes long-term empiric intravenous or oral antibiotics with or without adjunctive hyperbaric oxygen treatment. Necrotic bone should be debrided. Rarely do cases of PCO remain resistant to conventional treatments and require larger resection of bone with reconstruction.3,4
Here, we present a case of a 32-year-old woman with a long-standing history of PCO of the mandible requiring hemimandibulectomy and fibular free flab reconstruction of the surgical defect.
CASE PRESENTATION
A 32-year-old white woman with an 8-year history of chronic left mandibular swelling was referred to Otolaryngology—Head and Neck Surgery (OTO-HNS) by her oromaxillofacial surgeon. The patient had experienced a 1-year history of intermittent pain with mastication and facial swelling over the left mandible. She had no history of trauma to the mandible, dental procedures, oral lesions, or constitutional symptoms. On presentation, the patient was a 2 pack per day smoker but denied consumption of alcohol.
Before presentation to OTO-HNS, the patient had undergone bacterial cultures, radiological investigations, and multiple biopsies of the mandible. Computed tomography (CT) scan showed characteristic features of chronic sclerosing osteomyelitis of the mandible including marked enlargement of the left mandible from condylar process to symphysis, multiple sinus tracts through the mandible, and frank disruption of the cortex of the ramus. Moderate flattening of the mandibular condyle and narrowing of the temporomandibular joint were also noted. Bacterial cultures grew scant colonies of Streptococcus viridans, Staphylococcus aureus, and Staphylococcus lugdunensis. Bone biopsy revealed chronic inflammatory markers. After consultation with infectious diseases specialists, the patient was treated with a 6-week course of intravenous ceftriaxone with oral metronidazole and hyperbaric oxygen treatments with no improvement. Because of the long-standing nature of the condition with frequent exacerbations, the patient sought more definitive treatment.
After consultation with OTO-HNS, a resection of the left hemimandible with fibular free flap reconstruction was recommended secondary to the extent of mandibular involvement, worsening symptoms, and failure of conservative therapy. A preoperative CT scan showed diffuse thickening of the left masseter muscle with small areas of hypoattenuation consistent with myositis, without any findings of discreet abscess formation. Bony changes were consistent with findings on the prior CT scan of chronic sclerosing osteomyelitis of the mandible (Fig. 1).
Fig. 1.
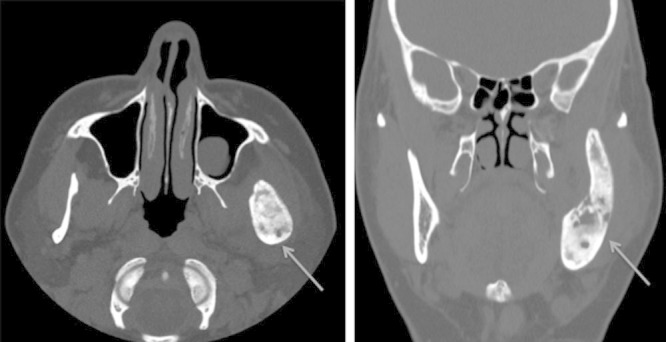
CT images. A and B show axial and coronal images, respectively, illustrating osteitic changes and thickening of the left hemimandible (arrows). Incidental note is made of a mucous retention cyst in the left maxillary sinus.
Surgical resection of the mandible required a modified apron incision from the mastoid process extending to a lip-split incision between the lower 2 central incisors. The marginal mandibular nerve and facial artery were identified and preserved. Several enlarged perifacial and external-jugular lymph nodes were removed and sent for pathology. Dissection was carried out from the midline symphysis to the left glenoid fossa, encompassing the entirety of the left mandible. The disk of the temporomandibular joint was sclerosed to the head of the condyle and therefore was left intact and removed en bloc. Figure 2 shows the gross specimen. The hemimandibulectomy was well tolerated and reconstruction followed.
Fig. 2.

Gross pathological specimens. Sagittal view of the thickened ramus.
A bone-only fibular free flap was selected for reconstruction. The fibula was harvested in the typical fashion by dissecting the peroneal artery and vena comitantes and preserving the peroneal nerve. Using a rough template of the resected mandibulectomy specimen, it was determined that 2 bone segments would be required. The proximal bone segment (from glenoid fossa to the angle of the mandible) was approximated at 7 cm, and the body of the mandible (from the angle to the symphysis) was also approximated at 7 cm. A wedge osteotomy was performed and allowed the 2 bone segments to form an angled mandibular reconstruction. The fibular-to-fibular fixation and mandibular fixation were accomplished with 2.0 mm 4-hole compression plates. The facial artery was used as the recipient vessel for the peroneal artery, and 1 vena comitante was selected for anastomosis to the common facial vein with 9-0 nylon sutures. The fibular donor site, oropharyngeal, alveolar ridge, and lip wounds were all closed in typical fashion. The patient tolerated the reconstruction well and had an uncomplicated postoperative course. The patient was discharged home 11 days postoperatively on a soft diet.
Postsurgical mandibular specimens sent for pathology showed thickened cortical and trabecular bone with decreased intertrabecular space and no bone marrow formation. Final diagnosis of primary chronic sclerosing osteomyelitis was made. Lymph nodes sent for pathology were negative for malignancy, showing only reactive inflammatory changes.
On 4-week follow-up, the patient had a clean and well-healing incision site, full range of motion of her jaw, excellent occlusion, and no difficulties in swallowing. Postoperative panoramic x-ray imaging shows stability of the reconstruction at 5 months (Fig. 3). The patient is now preparing for left sided mandibular dental implants.
Fig. 3.

Panoramic X-ray image. Five-month follow-up x-ray image shows stability of patient’s bony fibular reconstruction.
Footnotes
Disclosure: The authors have no financial interest to declare in relation to the content of this article. The Article Processing Charge was paid for by the Division of Otolaryngology - Head and Neck Surgery at Dalhousie University.
REFERENCES
- 1.El-Shanti HI, Ferguson PJ. Chronic recurrent multifocal osteomyelitis: a concise review and genetic update. Clin Orthop Relat Res. 2007;462:11–19. doi: 10.1097/BLO.0b013e3180986d73. [DOI] [PubMed] [Google Scholar]
- 2.Marx RE, Baltensperger M, Eyrich GK. Osteomyelitis of the Jaws. Berlin: Springer Science & Business Media; 2008. [Google Scholar]
- 3.Montonen M, Iizuka T, Hallikainen D, et al. Decortication in the treatment of diffuse sclerosing osteomyelitis of the mandible. Retrospective analysis of 41 cases between 1969 and 1990. Oral Surg Oral Med Oral Pathol. 1993;75:5–11. doi: 10.1016/0030-4220(93)90397-m. [DOI] [PubMed] [Google Scholar]
- 4.Schmutz J. Osteomyelitis of the Jaws. Berlin: Springer; 2009. Osteomyelitis therapy–hyperbaric oxygen as an adjunct in treatment of osteomyelitis of the jaws. pp. 191–204. [Google Scholar]


