Summary:
Hand appearance is meaningful to patients because hands are an essential part of human interactions, communication, and social integration. Recent literature indicates that hand aesthetics is an important, measurable patient-reported outcome. In hand surgery, several outcome instruments exist that accurately measure functional outcomes, but aesthetics is often overlooked or imprecisely measured. This makes comparison of disease burden and effectiveness of therapies, as they pertain to aesthetics, difficult. This special topic article outlines the aesthetic features of the hand, how literature is evaluating the appearance of the hand in outcomes research, and proposes a novel approach to assessing hand aesthetics.
Hands are prominently visible to both self and the public, and therefore, patients are cognizant of their appearance.1 Although normal hands go unnoticed, the deformed or diseased hand often draws unwanted attention with psychosocial consequences.2,3 Hands have personal significance and are important for human interactions, nonverbal communication, and social integration.1,4–6 Furthermore, presumptions of health can be inferred from skin appearance, soft-tissue bulk, and joint alignment.4,7,8 For these reasons, patients will have concerns about the appearance of their hands, even when faced with a crippling hand ailment.
Although functionality remains unquestionably the outcome of critical importance in hand surgery, surgeons are beginning to recognize that patients care about hand aesthetics.9 This is evident by the use of hand appearance as a patient-reported outcome in observational research.10–14 Assessing aesthetics can be a powerful method of demonstrating the patients’ perspective on surgical interventions.15–17 For example, Chung et al16 found that hand appearance is a valued outcome for rheumatoid arthritis patients with severe hand deformity undergoing silicone metacarpophalangeal arthroplasty. In fact, aesthetic consideration was the most important outcomes domain over function.16
Understanding the importance of hand appearance to patients requires accurate, reliable assessment methods. Although hand-specific questionnaires exist, many researchers elect to use ad hoc methods to evaluate aesthetics. Having a universal, standardized approach to assessing hand appearance would be ideal to introduce consistency across hand surgery literature and provide guidance to hand surgeons interested in evaluating a patient’s aesthetic concerns. This remains challenging because a patient’s perception of hand appearance is dependent on personal preference and their hand affliction, rather than specific characteristics related to the disease process or surgical intervention.18,19 This special topic article focuses on defining hand aesthetics, its importance in hand surgery, and the need for validated and accurate assessment methods for aesthetic outcomes.
FEATURES AFFECTING HAND APPEARANCE
General hand features including shape, proportions, and landmarks (eg, palmar crease) and typical clinical hand anatomy (eg, joints and digits) contribute to the appearance of a normal hand. The qualities of an aesthetic hand are more subjective. Literature suggests that an aesthetic hand appears youthful, healthy, and has long, but proportionally appropriate, fingers.1,4,5,7 The prominence of veins, feminine or masculine features, skin texture, and pigmentation are features of personal preference.1,5 Satisfaction, or comfort, with hand appearance is highly individualistic and may depend on age, sex, religion, culture, socioeconomic status, and hand affliction.1,4,5 Recognizing the features valued by patients will assist surgeons in providing reconstructive surgery with improved patient satisfaction.
Shape, Proportion, and Length
The shape of the hand often parallels an individual’s body type.1 A historical classification of hand types was adopted from Kretschmer’s20 body habitus classification. The leptosome–asthenic type has a slender form with long fingers; the athletic type is rough, wide, and balanced; and the pyknic-type has a short, wide dorsum with conically formed fingers.1,20 The feature differing these hand types is predominantly finger length. The influence of finger length on appearance is glaring when a digit is traumatically foreshortened (Fig. 1). For this reason, many surgeons advocate distal digit replantation over amputation to conserve hand aesthetics.21,22 An aesthetically superior finger to hand length does not exist, but the golden proportion has been suggested as the model dimension.1,23 The golden proportion, a mathematical ratio of 2 parts represented by “(a + b)/a equals a/b equals 1.618,” has been referred to a proportion of beauty and has been applied in facial aesthetics and rhinology (Fig. 2).24
Fig. 1.

Finger length is a dominant hand feature. Discrepancies in figure length or proportion are easily recognized and result in poor hand aesthetics.
Fig. 2.
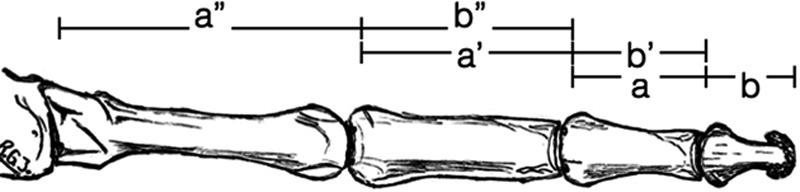
The golden proportion is a mathematical ratio of 2 parts represented as “(a + b)/a equals a/b equals approximately 1.618.” Reprinted with permission from Springer. Jakubietz RG, Jakubietz MG, Kloss D, et al. Defining the basic aesthetics of the hand. Aesth Plast Surg. 2005;29:546–551.
Visual Subunits
Higgins et al25 introduced the concept of hand visual subunits or characteristic regions formed by convexities, concavities, or topographical contrasts of the hand. Similarly, Rehim et al26 subdivided the hand into functional aesthetic units (Fig. 3). When visual subunits are disrupted or become indistinct from adjacent subunits, a deformity is perceived. Higgins et al25 emphasized the importance of reestablishing normal variance between visual subunits in posttraumatic hand deformities, particularly after soft-tissue coverage, with procedures such as partial flap elevation, targeted debulking, and redefining topographic regions. Subunits should also be respected when making a surgical incision, as not to not disfigure their natural borders.27
Fig. 3.
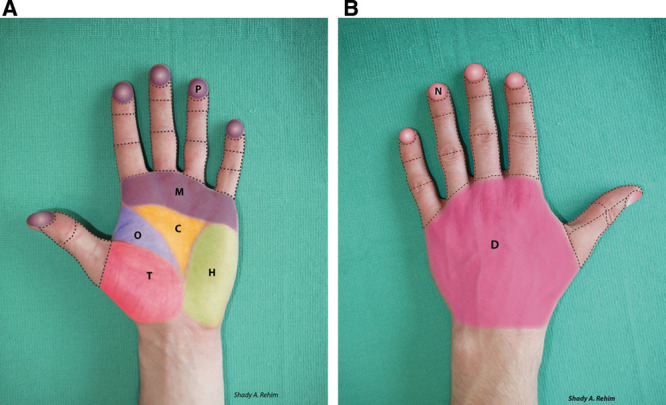
A, Rehim et al26 described the functional aesthetic subunits of the hand. The volar subunits include the thenar (T), opposition (O), hypothenar (H), central triangular (C), metacarpal (M), and 3 subunits for each digit (except for the thumb, which has 2). The pulps (p) of digits are topographically the most prominent subunit of the hand. B, The dorsal hand contains the dorsum (D) and 3 subunits for each digit (except for the thumb, which has 2). Reprinted with permission from Wolters Kluwer Health, Inc. Rehim SA, Kowalski E, Chung KC. Enhancing aesthetic outcomes of soft-tissue coverage of the hand. Plast Reconstr Surg. 2015; 135: 413e–428e.
Soft Tissue
The soft tissues of the hand contribute to the topographic variations between visual subunits. The volume and integrity of soft tissues are strong indicators of an individual’s age, health, and body habitus.4,7 For example, edema and skin turgor can offer estimation of fluid status, whereas fattiness or cachexia lends insight into nutritional status. Young adult hands are marked by supple, soft tissue and few visible subcutaneous structures.4 Veins, tendons, and muscle are more visible on the dorsal surface, as loose areolar tissue anchors the thin skin to the deep fascial layer.4,23 Male hands appear more masculine and square because they generally have less subcutaneous fat.28 Conversely, feminine hands have more subcutaneous soft tissue, less prominently visible underlying structures, and less hair.28
Skin
Palmar and dorsal skins are aesthetically distinct, as a result of their histological differences and mechanical demands. Palmar skin has a thick dermis and heavily cornified epithelium with papillary ridges that protect against shearing forces.23 An abundance of vertical fibers tether the thick, fibrous palmar fascia to the dermis, making this skin highly durable and less susceptible to age-related changes (eg, wrinkles).23 Deep palmar creases allow joint flexion and permit skin folding.4 The transition from glabrous to nonglabrous skin occurs at the mid-axial line of each digit. In contrast, dorsal skin is thin and soft and the lack of tethering fibers contributes to its pliability.23 On the dorsum of the hand, fine wrinkles are apparent at a young age over joints and allow unrestricted flexion.4,7
Hand Aging
Hand appearance is influenced by physiological changes related to aging. Intrinsic aging affects the subcutaneous tissue and is characterized by dermal and fat atrophy; deepening of intermetacarpal spaces; and marked by prominent tendons, bones, and veins.1,29 Extrinsic aging is a result of pathological changes (eg, actinic keratosis) in dermal and epidermal layers and is a consequence of environmental exposures, such as ultraviolet rays.1 Jakubietz et al4 described the chronological changes in aging by making observations on wrinkle pattern, volume loss, visibility of subcutaneous structures, and trophic changes. Dominant wrinkles are the first signs of aging, generally appreciated in the fourth decade. Wrinkle progression is prominent at the wrist crease and over the metacarpophalangeal joints. Around the sixth decade, epidermal thinning, volume loss (particularly thenar and hypothenar eminences), and prominent dorsal veins are more apparent.4 As dorsal skin becomes less elastic, finger flexion no longer results in complete emptying of incompetent dorsal veins.4 Muscular atrophy, visible tendons, dorsal wrinkles, and hand pathology (eg, osteoarthritic joint deformities and skin lesions) are characteristic of elderly hands.
HAND APPEARANCE AS AN OUTCOME OF INTEREST
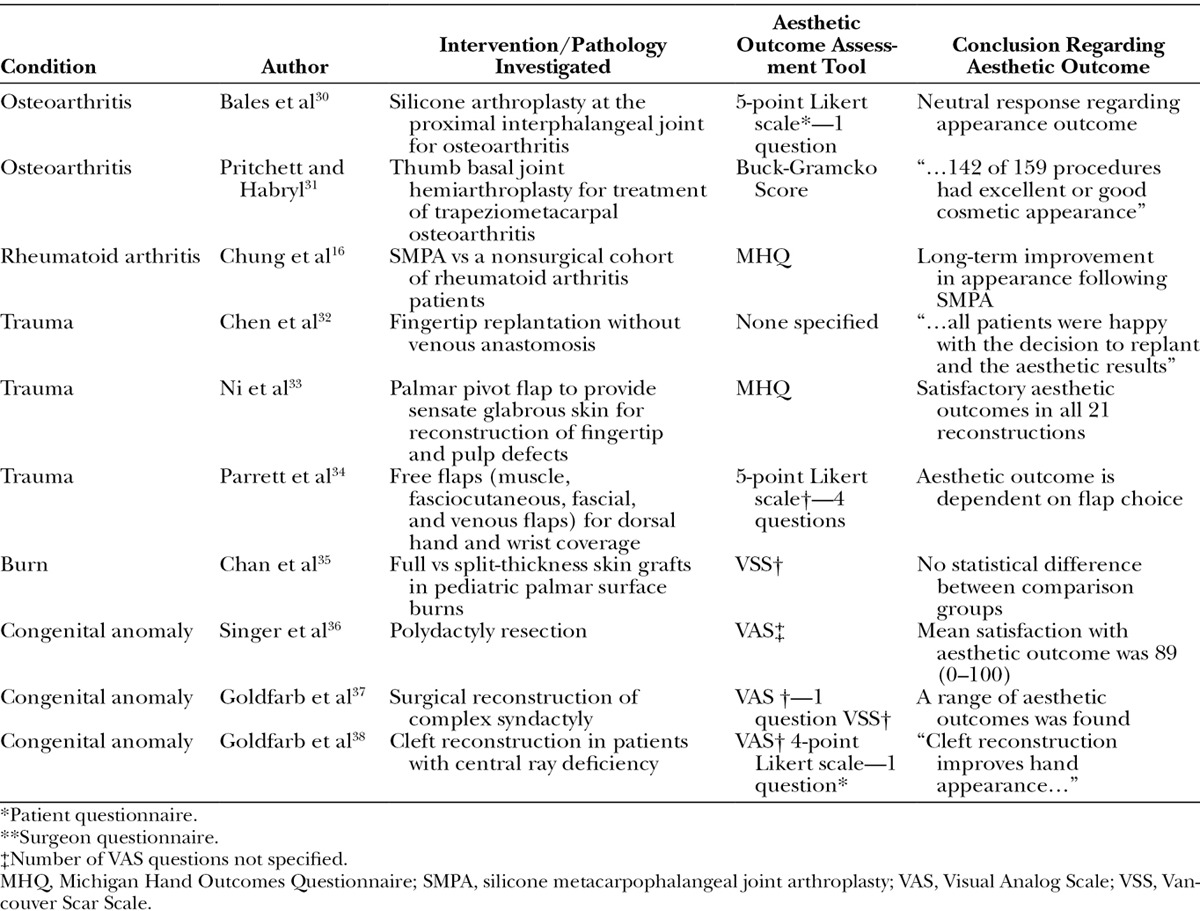
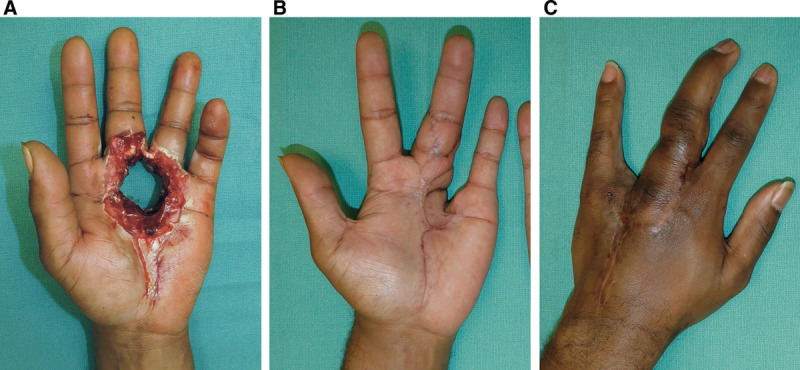
Hand aesthetics can be an important factor in determining the morbidity of pathological hand conditions and the effectiveness of interventions. Here, we provide examples of pathological conditions in which hand appearance has been used as an outcome of interest. Table 1 supplements our discussion by providing examples of publications that have used aesthetics as an outcome.
Table 1.
Examples of Publications That Have Used Aesthetics as an Outcome in Hand Surgery Literature
Degenerative and Inflammatory Joint Disease
Hand features, such as digit length and alignment, can be profoundly affected in degenerative and inflammatory joint diseases. Common osteoarthritic hand deformities include bony enlargement, soft-tissue swelling, Heberden’s nodes, Bouchard’s nodes, and squaring of the hand at the carpometacarpal joint (Fig. 4).39 Hodkinson et al39 found that aesthetic discomfort is a major concern for patients with hand osteoarthritis and is associated with depression, anxiety, and poor health-related quality of life. Hand appearance is also frequently included as an outcome measurement when investigating the surgical management of inflammatory joint diseases. For example, Bogoch et al40 showed that hand appearance is a strong motivator for rheumatoid arthritis patients undergoing metacarpophalangeal joint arthroplasty, and that patients reported greater improvement in appearance than function or pain relief.
Fig. 4.

Osteoarthritis causing a deformity of the right ring proximal interphalangeal joint (Bouchard’s node).
Trauma and Burns
Several aesthetic considerations exist when treating traumatic injuries and burns to the hand. Treatment of hand trauma involves aggressive debridement of devitalized tissue, reconstruction of osteotendinous and neurovascular defects, and soft-tissue reconstruction.41 Although a surgeon’s primary objective is to maximize functional recovery, patients will have concerns about hand disfigurements. Therefore, without sacrificing the structural reconstructive efforts, surgeons should consider the aesthetic outcomes of surgical interventions.
The following case report illustrates how hand appearance can be important to patients with complex traumatic injuries:
A healthy 32-year-old male laborer sustained a metal press injury to his left nondominant hand (Fig. 5). This resulted in a circular, punched-out wound with complete loss of the ring and long finger metacarpophalangeal joints and associated composite structures. Both digits remained vascularly intact, but only the long finger retained partial sensation. After careful counseling, the patient realized the impact his injury would have on hand functionality. Interestingly, when discussing surgical options to maximize his functional outcome, the patient and his family were equally concerned with aesthetic outcomes. They were apprehensive about the appearance of amputated digits, a cleft hand, skin grafting, and the visibility of surgical incisions.
Fig. 5.
Traumatic injury with complete loss of the ring and long finger metacarpophalangeal joints (A). Palmar (B) and dorsal (C) views after a vascularized pedicled transfer of the ring finger proximal interphalangeal joint to reconstitute the long finger metacarpophalangeal joint with like-to-like reconstruction of glabrous and nonglabrous skin.
Surgical reconstruction included a vascularized pedicled transfer of the ring finger proximal interphalangeal joint to reconstitute the metacarpophalangeal joint of the long finger (Fig. 5). Using this “spare-parts” technique, soft tissue from the ring finger was used as coverage for the wound defect. This like-to-like reconstruction of glabrous and nonglabrous skin enhanced the aesthetic result, as other forms of flap reconstruction would undoubtedly have lead to discrepancies in contour, texture, and pigmentation of the palmar and dorsal surfaces. Although the reconstruction required amputation of the insensate ring finger, the long finger was salvaged and a cleft hand was avoided.
When treating traumatic hand injuries, decisions regarding digit reconstruction (vs amputation) and soft-tissue coverage often have the greatest aesthetic implications.41 Because a deficiency in finger length is easily recognized, distal replantation (performed at centers specializing in replantation) is recommended for patients interested in restoring the length and improving the appearance of an amputated digit.32,42 Important aesthetic parameters in reconstructing hand soft tissue include pigmentation, contour, volume, glabrous skin matching, and incision placement.26 Palmar skin is distinct, and thus, soft-tissue coverage is preferably obtained from the hand to optimize functional, sensory, and aesthetic outcomes.41 When glabrous skin is not available, several soft-tissue reconstructive techniques exist, such as partial toe transplant, pedicled abdominal flaps, cross-finger flap, reverse digital artery flap, reverse dorsal digital island flap, and V-Y advancement flap.33,35,43–46
Hand Tumors
Hand tumors, arising from skin, soft tissue or osseous structures, may present as an unsightly lesion or deforming mass. Skin lesions (eg, actinic keratosis, pyogenic granulomas, and keratoacanthomas), benign soft tissue (eg, lipomas, ganglion cysts, schwannomas, glomus tumors, and neurofibromas), and vascular tumors (eg, hemangiomas) are often amenable to topic treatments, electrocautery, cryotherapy, or simple resection.47 These lesions are typically inconsequential to hand appearance, although aesthetic outcomes after management may be of interest depending on lesion size, side effects of nonsurgical treatment (eg, hypopigmentation from sclerotherapy), and location of surgical incisions.
Conversely, malignant lesions, including basal cell carcinoma, squamous cell carcinoma, melanoma, and soft-tissue sarcomas, may require extensive resections with dramatic aesthetic consequences (Fig. 6).48 Sarcomas are aggressive hand tumors, historically treated with radial resection and amputations.49 Current literature recommends limb salvage when feasible, as this offers no difference in long-term survival but provides the potential of improved functional and aesthetic outcomes.49
Fig. 6.
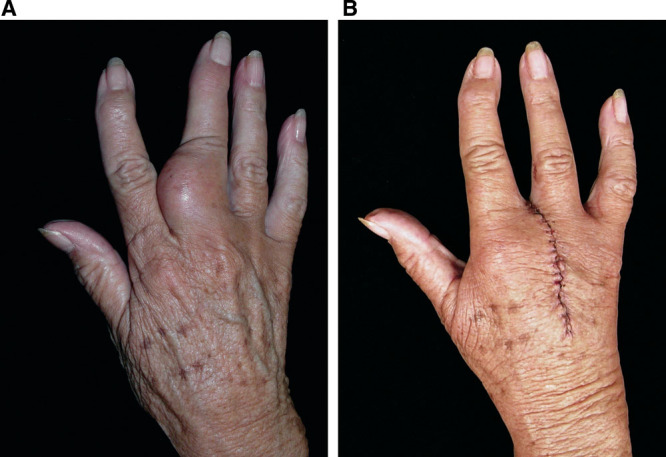
Malignant tumor of the long finger proximal phalanx (A) requiring digit amputation (B).
Congenital Deformities
Hand appearance as a clinical outcome is relevant in congenital deformities because an abnormal hand may impact a child’s psychological, emotional, and social development.50,51 For example, aesthetics is often the primary indication for surgical correction of ulnar polydactyly, as this condition is rarely associated with function disabilities (Fig. 7).36 Literature has shown that children with congenital hand deformities experience low self-esteem, stress, social anxiety, and depression when they become aware of physical disfigurements.3,50,51 Hermansson et al52 reported that children with upper-limb reduction deficiency more often experienced withdrawn behavior when compared with standardized norms.
Fig. 7.
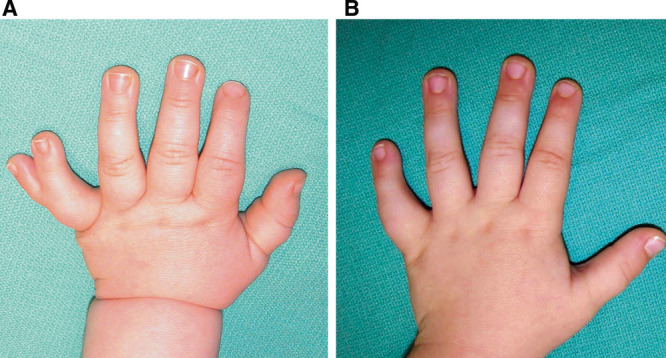
Ulnar polydactyly (A) with excellent aesthetic outcome 18 months after surgical resection (B).
Decision making regarding reconstructive surgery for hand anomalies is difficult for parents, who provide consent for invasive, complex procedures. Therefore, demonstrating the aesthetic benefits of surgical interventions can provide reassurance that surgical correction of deformities is worth pursuing. Unfortunately, there are unique challenges in assessing aesthetic outcomes of surgeries for congenital hand deformities. First, given the burden of disease, normal appearing hands may not be attainable (Fig. 8), and second, psychological factors (eg, guilt) may influence a parent’s subjective assessment of aesthetic outcomes.
Fig. 8.
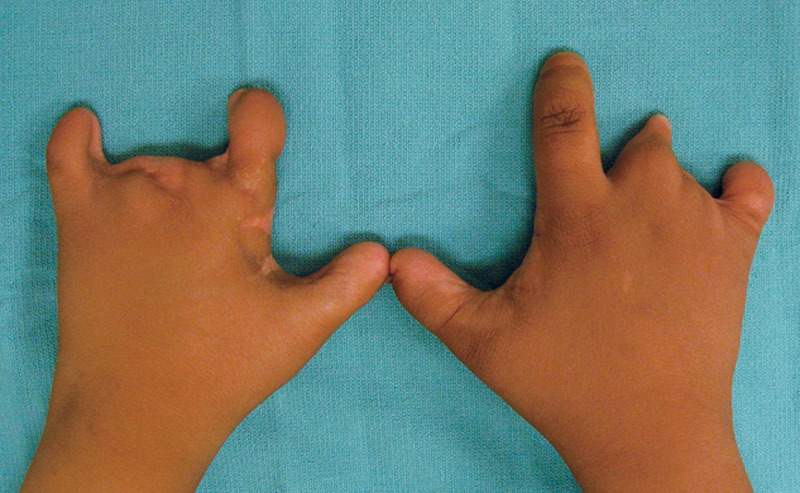
Amniotic band syndrome.
Aging
Bains et al. showed that people can estimate the age of an individual based on hand appearance.7 Cosmetic surgeons have also observed that patients notice the discrepancy between rejuvenated facial appearance and senile hands.8 Therefore, antiaging hand treatments (eg, laser therapy for photoaging pathology) have gained interest.29 More invasive therapies directed at masking age-related changes include sclerotherapy for tortuous veins and autologous fat grafts or dermal fillers for soft-tissue restoration.8 Because antiaging procedures are relatively new, elective, commercially influenced, and privately funded, there is less interest in objectively evaluating outcomes. Regardless, patients will query hand surgeons on the effectiveness of procedures as interest grows.
EVALUATING HAND AESTHETICS
The use of hand aesthetics as a patient-reported outcome in clinical research has influenced the indications and demonstrated the effectiveness of surgical interventions in hand surgery.10,16,40,53 Although, quantifying aesthetic improvement may influence treatment decisions, obtaining these data relies on appropriate outcome assessment instruments. Several outcome instruments exist in hand surgery research, but hand aesthetics is infrequently explicitly included. For example, the Disabilities of the Arm, Shoulder, and Hand instrument assesses the construct of “function,” but this only implicitly evaluates hand appearance.14,54 Conversely, the Michigan Hand Outcomes Questionnaire is a validated and reliable tool widely used in hand research that includes a domain dedicated to hand appearance.12 Table 2 provides a list of outcomes instruments (or strategies) commonly employed in hand surgery research.
Table 2.
Methods Used to Assess Hand Aesthetics in Literature
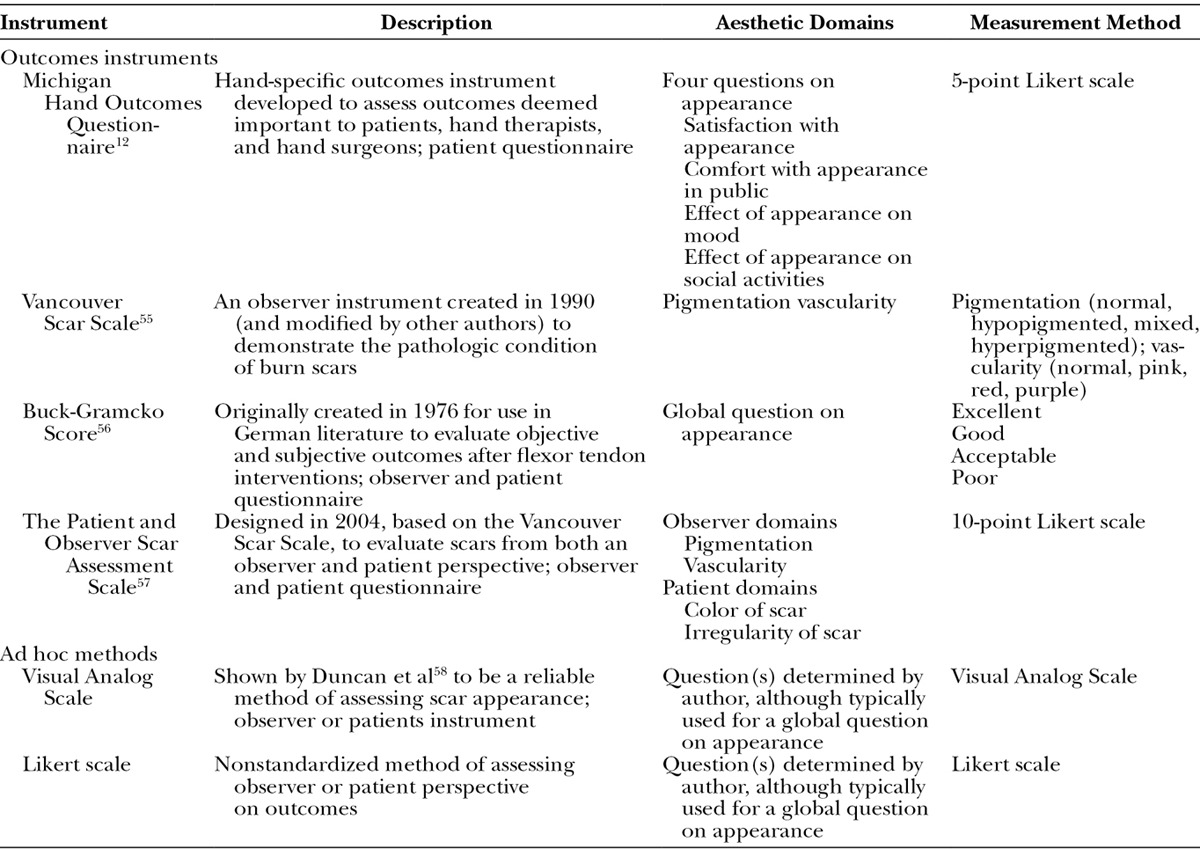
In lieu of a validated instrument, many researchers utilize ad hoc questions with visual analog scales, Likert scales, or available scar scales to assess hand appearance.11 Tyack et al18 performed a systematic review of available scar scales, and of 18 investigated instruments, the Patient and Observer Scar Assessment Scale and Vancouver Scar Scale were the most robustly validated.21,55,57 Unfortunately, both of these instruments were deemed to have intermediate quality clinimetric properties (eg, validity and reproducibility). Furthermore, the applicability of scar scales to hand aesthetics has not been robustly investigated.
FUTURE DIRECTION IN EVALUATING HAND AESTHETICS
Measuring and reporting “what matters” to patients is fundamental to understanding and communicating the burden of disease or success of health-care interventions.59 Theoretically, a universally accepted, standardized aesthetic assessment instrument would allow for accurate comparison of outcomes across literature.60,61 Further research is needed to demonstrate the quality of currently available aesthetic assessment instruments, as the particular instrument used is less important than demonstrating the validity (and responsiveness), reliability, interpretability, feasibility, and minimal clinically important difference of the tool.15,18,62 Alternatively, efforts can be directed at designing a universal assessment tool dedicated to hand aesthetics.
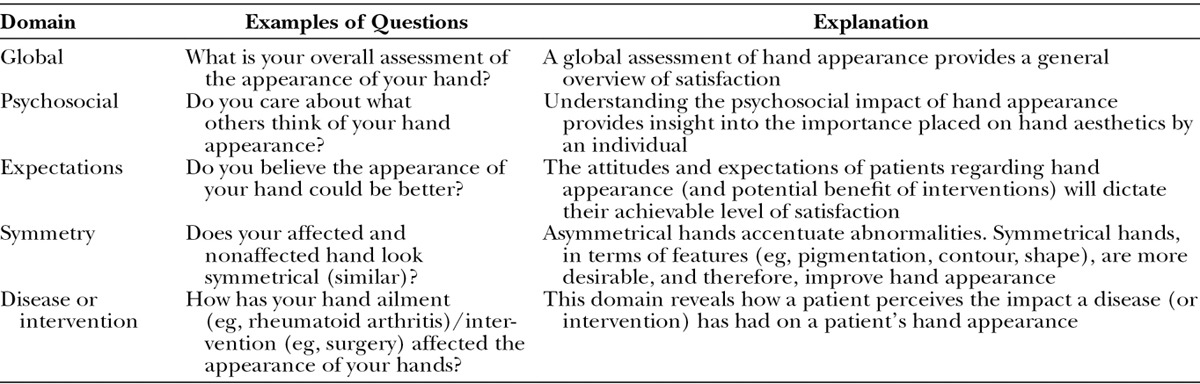
We present a simple approach to evaluating a patient’s perception of hand appearance. Through our literature review, we conclude that hand appearance is (1) unique to each patient with influences from age, sex, culture, and occupation; (2) dependent on the hand pathology; (3) related to the chronicity of disease; and (4) may be of variable importance. Furthermore, a patient’s opinion of their hand appearance may be adversely influenced by social perceptions. Hand aesthetics, therefore, is best understood as a self-concept that is dynamic and responsive to biopsychosocial factors. Table 3 refers to 5 domains that evaluate a patient’s perceptions of hand appearance. Our approach captures a patient’s global assessment, interest, and expectations of hand aesthetics in the context of a disease or surgical intervention. These domains can provide the foundation for creating a future assessment tool or be used by health-care providers to evaluate an individual’s perspective of hand appearance.
Table 3.
Assessing Hand Aesthetics With 5 Core Domains
CONCLUSIONS
Evaluating hand appearance can demonstrate the impact of hand pathology and the effectiveness of therapeutic interventions. Although functionality remains the mainstay of determining the success of surgical interventions in hand surgery, aesthetics should be regarded as a pertinent outcome, worthy of being measured and monitored. Currently, available outcome instruments lack detailed, precise assessments of aesthetic discomfort. Therefore, a common method of assessing appearance is with ad hoc questioning, which makes comparison of outcomes across literature difficult. Further research is required to investigate how hand appearance can be accurately and thoroughly assessed. We propose 5 important domains to capture when evaluate hand appearance including a global assessment, symmetry, expectations, psychosocial influences, and disease-specific morbidity.
Footnotes
Disclosure: The authors have no financial interest to declare in relation to the content of this article. Research reported in this publication was supported by the National Institute of Arthritis and Musculoskeletal and Skin Diseases of the National Institutes of Health under Award Number 2 K24-AR053120-06. Article Processing Charge was paid for by the authors.
REFERENCES
- 1.Jakubietz RG, Jakubietz MG, Kloss D, et al. Defining the basic aesthetics of the hand. Aesthetic Plast Surg. 2005;29:546–551. doi: 10.1007/s00266-005-0100-6. [DOI] [PubMed] [Google Scholar]
- 2.Van Loey NE, Van Son MJ. Psychopathology and psychological problems in patients with burn scars: epidemiology and management. Am J Clin Dermatol. 2003;4:245–272. doi: 10.2165/00128071-200304040-00004. [DOI] [PubMed] [Google Scholar]
- 3.Andersson GB, Gillberg C, Fernell E, et al. Children with surgically corrected hand deformities and upper limb deficiencies: self-concept and psychological well-being. J Hand Surg Eur Vol. 2011;36:795–801. doi: 10.1177/1753193411412869. [DOI] [PubMed] [Google Scholar]
- 4.Jakubietz RG, Kloss DF, Gruenert JG, et al. The ageing hand. A study to evaluate the chronological ageing process of the hand. J Plast Reconstr Aesthet Surg. 2008;61:681–686. doi: 10.1016/j.bjps.2007.12.028. [DOI] [PubMed] [Google Scholar]
- 5.Kościński K. Determinants of hand attractiveness–a study involving digitally manipulated stimuli. Perception. 2011;40:682–694. doi: 10.1068/p6960. [DOI] [PubMed] [Google Scholar]
- 6.Pillet J. And thus, the hand revealed its beauty. Moving toward aesthetics. J Hand Ther. 1997;10:258–261. doi: 10.1016/s0894-1130(97)80039-7. [DOI] [PubMed] [Google Scholar]
- 7.Bains RD, Thorpe H, Southern S. Hand aging: patients’ opinions. Plast Reconstr Surg. 2006;117:2212–2218. doi: 10.1097/01.prs.0000218712.66333.97. [DOI] [PubMed] [Google Scholar]
- 8.Butterwick KJ. Rejuvenation of the aging hand. Dermatol Clin. 2005;23:515–527, vii. doi: 10.1016/j.det.2005.04.007. [DOI] [PubMed] [Google Scholar]
- 9.Manske PR. Aesthetic hand surgery. J Hand Surg Am. 2002;27:383–384. doi: 10.1053/jhsu.2002.33938. [DOI] [PubMed] [Google Scholar]
- 10.Chung KC, Kotsis SV, Kim HM, et al. Reasons why rheumatoid arthritis patients seek surgical treatment for hand deformities. J Hand Surg Am. 2006;31:289–294. doi: 10.1016/j.jhsa.2005.10.005. [DOI] [PubMed] [Google Scholar]
- 11.Alderman A, Chung KC. Measuring outcomes in aesthetic surgery. Clin Plast Surg. 2013;40:297–304. doi: 10.1016/j.cps.2012.10.005. [DOI] [PubMed] [Google Scholar]
- 12.Chung KC, Pillsbury MS, Walters MR, et al. Reliability and validity testing of the Michigan Hand Outcomes Questionnaire. J Hand Surg Am. 1998;23:575–587. doi: 10.1016/S0363-5023(98)80042-7. [DOI] [PubMed] [Google Scholar]
- 13.Badalamente M, Coffelt L, Elfar J, et al. American Society for Surgery of the Hand Clinical Trials and Outcomes Committee. Measurement scales in clinical research of the upper extremity, part 1: general principles, measures of general health, pain, and patient satisfaction. J Hand Surg Am. 2013;38:401–406; quiz 406. doi: 10.1016/j.jhsa.2012.11.028. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Badalamente M, Coffelt L, Elfar J, et al. Measurement scales in clinical research of the upper extremity, part 2: outcome measures in studies of the hand/wrist and shoulder/elbow. J Hand Surg Am. 2013;13:407–412. doi: 10.1016/j.jhsa.2012.11.029. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.van der Wal MB, Verhaegen PD, Middelkoop E, et al. A clinimetric overview of scar assessment scales. J Burn Care Res. 2012;33:e79–e87. doi: 10.1097/BCR.0b013e318239f5dd. [DOI] [PubMed] [Google Scholar]
- 16.Chung KC, Burns PB, Kim HM, et al. Long-term followup for rheumatoid arthritis patients in a multicenter outcomes study of silicone metacarpophalangeal joint arthroplasty. Arthritis Care Res (Hoboken) 2012;64:1292–1300. doi: 10.1002/acr.21705. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Pearl RA, Belcher HJ. Three-dimensional assessment of hand outcome. Ann R Coll Surg Engl. 2013;95:421–426. doi: 10.1308/003588413X13629960048190. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Tyack Z, Simons M, Spinks A, et al. A systematic review of the quality of burn scar rating scales for clinical and research use. Burns. 2012;38:6–18. doi: 10.1016/j.burns.2011.09.021. [DOI] [PubMed] [Google Scholar]
- 19.Chung KC. Clinical research in hand surgery. J Hand Surg Am. 2010;35:109–120. doi: 10.1016/j.jhsa.2009.09.012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Kretschmer E. Physique and Character. 2nd ed. New York, NY: Harcourt, Brace & Company; 1925. [Google Scholar]
- 21.Sebastin SJ, Chung KC. A systematic review of the outcomes of replantation of distal digital amputation. Plast Reconstr Surg. 2011;128:723–737. doi: 10.1097/PRS.0b013e318221dc83. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Matsuzaki H, Yoshizu T, Maki Y, et al. Functional and cosmetic results of fingertip replantation: anastomosing only the digital artery. Ann Plast Surg. 2004;53:353–359. doi: 10.1097/01.sap.0000137136.09890.18. [DOI] [PubMed] [Google Scholar]
- 23.Neligan PC. Plastic Surgery. 3rd ed. Philadelphia, PA: Saunders; 2012. [Google Scholar]
- 24.Danikas D, Panagopoulos G. The golden ratio and proportions of beauty. Plast Reconstr Surg. 2004;114:1009. doi: 10.1097/01.prs.0000138702.13724.26. [DOI] [PubMed] [Google Scholar]
- 25.Higgins JP, Seruya M. Visual subunits of the hand: proposed guidelines for revision surgery after flap reconstruction of the traumatized hand. J Reconstr Microsurg. 2011;27:551–557. doi: 10.1055/s-0031-1285987. [DOI] [PubMed] [Google Scholar]
- 26.Rehim SA, Kowalski E, Chung KC. Enhancing aesthetic outcomes of soft-tissue coverage of the hand. Plast Reconstr Surg. 2015;135:413e–428e. doi: 10.1097/PRS.0000000000001069. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Watt AJ, Chung KC. Surgical exposures of the hand. Hand Clin. 2014;30:445–457, vi. doi: 10.1016/j.hcl.2014.07.004. [DOI] [PubMed] [Google Scholar]
- 28.Garrett JW. The adult human hand: some anthropometric and biomechanical considerations. Hum Factors. 1971;13:117–131. doi: 10.1177/001872087101300204. [DOI] [PubMed] [Google Scholar]
- 29.Fabi SG, Goldman MP. Hand rejuvenation: a review and our experience. Dermatol Surg. 2012;38(7 Pt 2):1112–1127. doi: 10.1111/j.1524-4725.2011.02291.x. [DOI] [PubMed] [Google Scholar]
- 30.Bales JG, Wall LB, Stern PJ. Long-term results of Swanson silicone arthroplasty for proximal interphalangeal joint osteoarthritis. J Hand Surg Am. 2014;39:455–461. doi: 10.1016/j.jhsa.2013.11.008. [DOI] [PubMed] [Google Scholar]
- 31.Pritchett JW, Habryl LS. A promising thumb Basal joint hemiarthroplasty for treatment of trapeziometacarpal osteoarthritis. Clin Orthop Relat Res. 2012;470:2756–2763. doi: 10.1007/s11999-012-2367-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Chen YC, Chan FC, Hsu CC, et al. Fingertip replantation without venous anastomosis. Ann Plast Surg. 2013;70:284–288. doi: 10.1097/SAP.0b013e3182321b81. [DOI] [PubMed] [Google Scholar]
- 33.Ni F, Appleton SE, Chen B, et al. Aesthetic and functional reconstruction of fingertip and pulp defects with pivot flaps. J Hand Surg Am. 2012;37:1806–1811. doi: 10.1016/j.jhsa.2012.05.003. [DOI] [PubMed] [Google Scholar]
- 34.Parrett BM, Bou-Merhi JS, Buntic RF, et al. Refining outcomes in dorsal hand coverage: consideration of aesthetics and donor-site morbidity. Plast Reconstr Surg. 2010;126:1630–1638. doi: 10.1097/PRS.0b013e3181ef8ea3. [DOI] [PubMed] [Google Scholar]
- 35.Chan QE, Barzi F, Harvey JG, et al. Functional and cosmetic outcome of full- versus split-thickness skin grafts in pediatric palmar surface burns: a prospective, independent evaluation. J Burn Care Res. 2013;34:232–236. doi: 10.1097/BCR.0b013e31826fc53d. [DOI] [PubMed] [Google Scholar]
- 36.Singer G, Thein S, Kraus T, et al. Ulnar polydactyly - an analysis of appearance and postoperative outcome. J Pediatr Surg. 2014;49:474–476. doi: 10.1016/j.jpedsurg.2013.06.029. [DOI] [PubMed] [Google Scholar]
- 37.Goldfarb CA, Steffen JA, Stutz CM. Complex syndactyly: aesthetic and objective outcomes. J Hand Surg Am. 2012;37:2068–2073. doi: 10.1016/j.jhsa.2012.06.033. [DOI] [PubMed] [Google Scholar]
- 38.Goldfarb CA, Chia B, Manske PR. Central ray deficiency: subjective and objective outcome of cleft reconstruction. J Hand Surg Am. 2008;33:1579–1588. doi: 10.1016/j.jhsa.2008.05.010. [DOI] [PubMed] [Google Scholar]
- 39.Hodkinson B, Maheu E, Michon M, et al. Assessment and determinants of aesthetic discomfort in hand osteoarthritis. Ann Rheum Dis. 2012;71:45–49. doi: 10.1136/ard.2011.153965. [DOI] [PubMed] [Google Scholar]
- 40.Bogoch ER, Escott BG, Ronald K. Hand appearance as a patient motivation for surgery and a determinant of satisfaction with metacarpophalangeal joint arthroplasty for rheumatoid arthritis. J Hand Surg Am. 2011;36:1007–1014.e1. doi: 10.1016/j.jhsa.2011.02.002. [DOI] [PubMed] [Google Scholar]
- 41.Chim H, Ng ZY, Carlsen BT, et al. Soft tissue coverage of the upper extremity: an overview. Hand Clin. 2014;30:459–473, vi. doi: 10.1016/j.hcl.2014.08.002. [DOI] [PubMed] [Google Scholar]
- 42.Jazayeri L, Klausner JQ, Chang J. Distal digital replantation. Plast Reconstr Surg. 2013;132:1207–1217. doi: 10.1097/PRS.0b013e3182a3c0e7. [DOI] [PubMed] [Google Scholar]
- 43.Kappel DA, Burech JG. The cross-finger flap. An established reconstructive procedure. Hand Clin. 1985;1:677–683. [PubMed] [Google Scholar]
- 44.Niranjan NS, Armstrong JR. A homodigital reverse pedicle island flap in soft tissue reconstruction of the finger and the thumb. J Hand Surg Br. 1994;19:135–141. doi: 10.1016/0266-7681(94)90149-x. [DOI] [PubMed] [Google Scholar]
- 45.Takeishi M, Shinoda A, Sugiyama A, et al. Innervated reverse dorsal digital island flap for fingertip reconstruction. J Hand Surg Am. 2006;31:1094–1099. doi: 10.1016/j.jhsa.2006.02.029. [DOI] [PubMed] [Google Scholar]
- 46.Atasoy E, Ioakimidis E, Kasdan ML, et al. Reconstruction of the amputated finger tip with a triangular volar flap. A new surgical procedure. J Bone Joint Surg Am. 1970;52:921–926. [PubMed] [Google Scholar]
- 47.Henderson M, Neumeister MW, Bueno RA., Jr Hand tumors: II. Benign and malignant bone tumors of the hand. Plast Reconstr Surg. 2014;133:814e–821e. doi: 10.1097/PRS.0000000000000178. [DOI] [PubMed] [Google Scholar]
- 48.Henderson M, Neumeister MW, Bueno RA. Hand tumors: II. Skin and soft tissue tumors of the hand. Plast Reconstr Surg. 2014;133:154e–164e. doi: 10.1097/01.prs.0000436854.09656.05. [DOI] [PubMed] [Google Scholar]
- 49.Labow BI, Rosen H, Greene AK, et al. Soft tissue sarcomas of the hand: functional reconstruction and outcome analysis. Hand (N Y) 2008;3:229–236. doi: 10.1007/s11552-008-9089-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Franzblau LE, Chung KC, Carlozzi N, et al. Coping with congenital hand differences. Plast Reconstr Surg. 2015;135:1067–1075. doi: 10.1097/PRS.0000000000001047. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Bradbury E. The psychological and social impact of disfigurement to the hand in children and adolescents. Dev Neurorehabil. 2007;10:143–148. doi: 10.1080/17518420701281122. [DOI] [PubMed] [Google Scholar]
- 52.Hermansson L, Eliasson AC, Engström I. Psychosocial adjustment in Swedish children with upper-limb reduction deficiency and a myoelectric prosthetic hand. Acta Paediatr. 2005;94:479–488. doi: 10.1111/j.1651-2227.2005.tb01921.x. [DOI] [PubMed] [Google Scholar]
- 53.Chung KC, Kotsis SV, Kim HM. A prospective outcomes study of Swanson metacarpophalangeal joint arthroplasty for the rheumatoid hand. J Hand Surg Am. 2004;29:646–653. doi: 10.1016/j.jhsa.2004.03.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Hudak PL, Amadio PC, Bombardier C. Development of an upper extremity outcome measure: the DASH (disabilities of the arm, shoulder and hand) [corrected]. The Upper Extremity Collaborative Group (UECG) Am J Ind Med. 1996;29:602–608. doi: 10.1002/(SICI)1097-0274(199606)29:6<602::AID-AJIM4>3.0.CO;2-L. [DOI] [PubMed] [Google Scholar]
- 55.Sullivan T, Smith J, Kermode J, et al. Rating the burn scar. J Burn Care Rehabil. 1990;11:256–260. doi: 10.1097/00004630-199005000-00014. [DOI] [PubMed] [Google Scholar]
- 56.Buck-Gramcko D, Dietrich FE, Gogge S. [Evaluation criteria in follow-up studies of flexor tendon therapy]. Handchirurgie. 1976;8:65–69. [PubMed] [Google Scholar]
- 57.Draaijers LJ, Tempelman FR, Botman YA, et al. The patient and observer scar assessment scale: a reliable and feasible tool for scar evaluation. Plast Reconstr Surg. 2004;113:1960–1965; discussion 1966. doi: 10.1097/01.prs.0000122207.28773.56. [DOI] [PubMed] [Google Scholar]
- 58.Duncan JA, Bond JS, Mason T, et al. Visual analogue scale scoring and ranking: a suitable and sensitive method for assessing scar quality? Plast Reconstr Surg. 2006;118:909–918. doi: 10.1097/01.prs.0000232378.88776.b0. [DOI] [PubMed] [Google Scholar]
- 59.Haywood KL. Patient-reported outcome I: measuring what matters in musculoskeletal care. Musculoskeletal Care. 2006;4:187–203. doi: 10.1002/msc.94. [DOI] [PubMed] [Google Scholar]
- 60.Kosowski TR, McCarthy C, Reavey PL, et al. A systematic review of patient-reported outcome measures after facial cosmetic surgery and/or nonsurgical facial rejuvenation. Plast Reconstr Surg. 2009;123:1819–1827. doi: 10.1097/PRS.0b013e3181a3f361. [DOI] [PubMed] [Google Scholar]
- 61.Maass SW, Bagher S, Hofer SO, et al. Systematic review: aesthetic assessment of breast reconstruction outcomes by healthcare professionals. Ann Surg Oncol. 2015 doi: 10.1245/s10434-015-4434-2. [Epub ahead of print] [DOI] [PubMed] [Google Scholar]
- 62.Yeong EK, Mann R, Engrav LH, et al. Improved burn scar assessment with use of a new scar-rating scale. J Burn Care Rehabil. 1997;18:353–355; discussion 352. doi: 10.1097/00004630-199707000-00014. [DOI] [PubMed] [Google Scholar]


