Summary:
In this article, the authors present a practical surgical technique using the anatomical character of the inferior alveolar nerve to fully expose the mental nerve (MN) in narrowing genioplasty. During the procedure, a rectangular mandibular outer cortex adjacent to the mental foramen is removed before the osteotomy. The objective is to avoid the injury of the MN from the reciprocating saw or bur and offer abundant space for the surgical operation. The technique has a minimal learning curve and will be useful to plastic surgeons to minimize unintentional cutting or pulling injury to the MN in narrowing genioplasty.
The chin is the most prominent feature in the lower third of the face in both the frontal and profile views, which plays an important role in the facial harmony and balance. In many Asian countries, an oversized or broad chin not only gives a squared contour to the face but also shows a muscular appearance. Narrowing genioplasty, the resection of the lateral border of the chin, is one main therapeutic approach used to reduce the width of the chin or to change its shape.1
The mental nerve (MN) exits the mandible through the mental foramen, divides into 3 branches deep to the depressor anguli oris muscle, and supplies the skin and mucous membrane of the lower lip, the skin of the chin, and the vestibular gingiva of the mandibular incisor.2 Because of the location of the MN and the limited distance between the mental foramen and the labial soft tissue, the MN is at risk of unintentional injury with the use of various significantly large and unyielding instruments, such as the reciprocating saw, bur, and retractor for osteotomy, and exposure in the narrowing genioplasty. Westermark et al3 reported paresthesia of the MN in 3.4% and 12% in genioplasty. Hence, in this article, the authors introduce a practical surgical technique to fully expose the nerve and add to its range of extension, to prevent that kind of injury in many cases.
SURGICAL TECHNIQUE
Under general anesthesia, the chin and mandibular body were exposed with a conventional intraoral vestibular incision and subperiosteal dissection. The mental foramen with its exiting nerve is exposed.
A rectangle, the mental foramen as one of its vertices, was marked using a fissure bur at the anterior and inferior mandible (Fig. 1). The upper line is parallel to the occlusal plane through the lower border of the mental foramen; the lower line is the mandibular margin. The distal line is perpendicular to the occlusal plane through the posterior border of the mental foramen; the mesial line is parallel to the distal line, and the distance between them is about 8 mm. Cutting the mandibular outer cortex along these lines and using a chisel to separate the outer cortex from the cancellous bone, the rectangular cortex was removed. The caudal and anterior part of the inferior alveolar nerve (IAN) was relaxed. As a result, the distance between the mental foramen and the labial soft tissue was prolonged, which provides a better exposure of the MN and the chin-body bone (Fig. 2). Then we used the technique of oblique mandibular chin-body osteotomy for the narrowing of the broad chin, which has been previously published from our institution.4
Fig. 1.
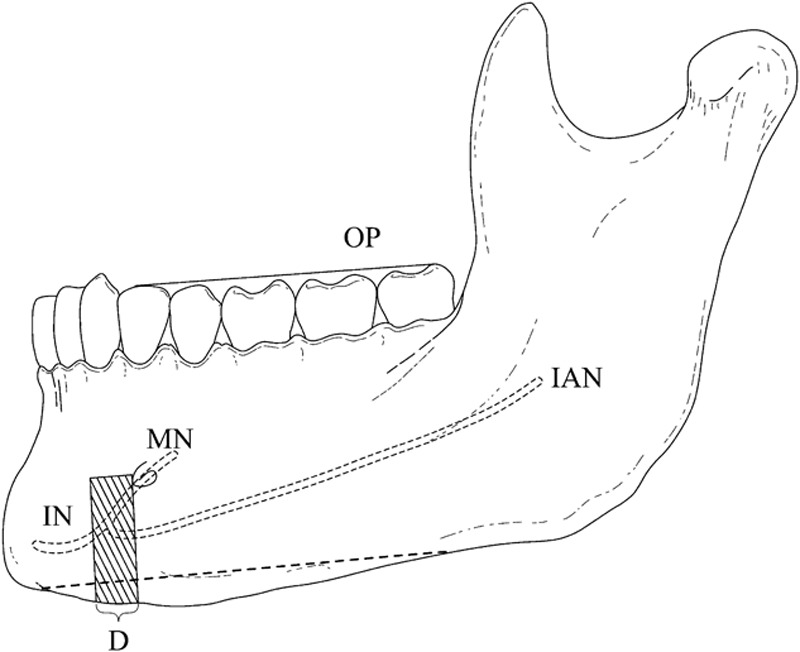
Schematic illustration of the surgical technique. The shaded part is the rectangular mandibular outer cortex to be removed. The dotted line at the inferior border of the mandible is the osteotomy for narrowing genioplasty. The distance (D) between the distal line and the mesial line is about 8 mm. IAN, inferior alveolar nerve; IN, incisive nerve; MN, mental nerve; OP, occlusal plane.
Fig. 2.
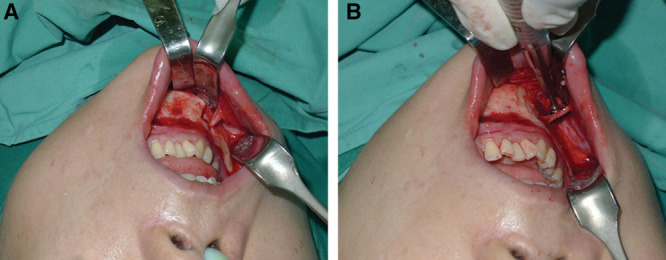
A, The length of the mental nerve before removing the rectangular mandibular outer cortex. B, The distance between the mental foramen and the labial soft tissue was prolonged, and the mobility of the mental nerve was added after removing the rectangular mandibular outer cortex.
DISCUSSION
Narrowing genioplasty involving resection of the lateral border of the chin can effectively reduce the width of the mandibular body and mental region and makes the lower face look attractive from both the anterior and lateral perspectives.4 It is one critical component of the mandibular contouring surgery, which considers the mandibular angle, body, and chin as one aesthetic unit. Technically, because of the obstacle of the MN, the osteotomy space is limited especially when the procedure is performed from posterior to anterior.
Traditionally, the plastic surgeons dissect the MN branches carefully from the periosteum covered with it to add its mobility. Apart from that, during the procedure the Obwegeser or Gimma retractors are often used and strongly retracted with the lips and mucosal stretched for a better exposure of the MN. However, the above measures have not completely addressed the limited space between the mental foramen and the labial soft tissue and may bring about adverse injury to the nerve or mucosal tear. From our experience of consecutive 100 narrowing genioplasty procedures over the last 3 years, the incidence of paresthetic symptoms after this maneuver is much lower than with the traditional technique.
The MN arises from the IAN in the mandibular canal. Hwang et al5 studied 50 dry specimens of Korean origin and reported that the terminal mandibular canal is at an average of 4.5 mm under the mental foramen, advances 5.0 mm anteriorly, loops, and ends at the foramen. However, Mardinger et al6 stated that a 3 mm safety margin from the mental foramen is necessary because the length of the alveolar loop of the IAN was 0.4–2.19 mm, and this has been confirmed by many other studies.2 In view of the anatomical variation of the anterior loop, we adopted 8 mm as the distance between the distal and mesial line. Xu et al7 dissected 80 Chinese adult cadavers and pointed that the length of the mental canal is 4.01 ± 1.20 mm, so the surgical technique we introduced can indeed relax the MN and offer abundant space for the operation.
CONCLUSIONS
Strategically utilizing the alveolar loop of the IAN and removing a rectangular outer cortex of mandible adjacent the mental foramen is an effective surgical technique, which can fully expose the MN and facilitate the operation of various orthognathic instruments and minimize the injury of the MN during the narrowing genioplasty. Additionally, this technique can be applied to all kinds of mandibular contouring surgeries if exposing the MN is necessary.
Footnotes
Disclosure: The authors have no financial interest to declare in relation to the content of this article. The Article Processing Charge was paid for by the authors.
REFERENCES
- 1.Park S, Noh JH. Importance of the chin in lower facial contour: narrowing genioplasty to achieve a feminine and slim lower face. Plast Reconstr Surg. 2008;122:261–268. doi: 10.1097/PRS.0b013e3181774179. [DOI] [PubMed] [Google Scholar]
- 2.Hu KS, Yun HS, Hur MS, et al. Branching patterns and intraosseous course of the mental nerve. J Oral Maxillofac Surg. 2007;65:2288–2294. doi: 10.1016/j.joms.2007.06.658. [DOI] [PubMed] [Google Scholar]
- 3.Westermark A, Bystedt H, von Konow L. Inferior alveolar nerve function after mandibular osteotomies. Br J Oral Maxillofac Surg. 1998;36:425–428. doi: 10.1016/s0266-4356(98)90457-0. [DOI] [PubMed] [Google Scholar]
- 4.Zhang Z, Tang R, Tang X, et al. The oblique mandibular chin-body osteotomy for the correction of broad chin. Ann Plast Surg. 2010;65:541–545. doi: 10.1097/SAP.0b013e3181d37770. [DOI] [PubMed] [Google Scholar]
- 5.Hwang K, Lee WJ, Song YB, et al. Vulnerability of the inferior alveolar nerve and mental nerve during genioplasty: an anatomic study. J Craniofac Surg. 2005;16:10–14; discussion 14. doi: 10.1097/00001665-200501000-00004. [DOI] [PubMed] [Google Scholar]
- 6.Mardinger O, Chaushu G, Arensburg B, et al. Anterior loop of the mental canal: an anatomical-radiologic study. Implant Dent. 2000;9:120–125. doi: 10.1097/00008505-200009020-00003. [DOI] [PubMed] [Google Scholar]
- 7.Xu Y, Suo N, Tian X, et al. Anatomic study on mental canal and incisive nerve canal in interforaminal region in Chinese population. Surg Radiol Anat. 2015;37:585–589. doi: 10.1007/s00276-014-1402-7. [DOI] [PubMed] [Google Scholar]


