Abstract
Objectives
The cervical range of motion device (CROM) has been shown to provide reliable forward head position (FHP) measurement when the upper cervical angle (UCA) is controlled. However, measurement without UCA standardization is reflective of habitual patterns. Criterion validity has not been reported. The purposes of this study were to establish: (1) criterion validity of CROM FHP and UCA compared to Optotrak data, (2) relative reliability and minimal detectable change (MDC95) in patients with and without cervical pain, and (3) to compare UCA and FHP in patients with and without pain in habitual postures.
Methods
(1) Within-subjects single session concurrent criterion validity design. Simultaneous CROM and OP measurement was conducted in habitual sitting posture in 16 healthy young adults. (2) Reliability and MDC95 of UCA and FHP were calculated from three trials. (3) Values for adults over 35 years with cervical pain and age-matched healthy controls were compared.
Results
(1) Forward head position distances were moderately correlated and UCA angles were highly correlated. The mean (standard deviation) differences can be expected to vary between 1·48 cm (1·74) for FHP and −1·7 (2·46)° for UCA. (2) Reliability for CROM FHP measurements were good to excellent (no pain) and moderate (pain). Cervical range of motion FHP MDC95 was moderately low (no pain), and moderate (pain). Reliability for CROM UCA measurements was excellent and MDC95 low for both groups. There was no difference in FHP distances between the pain and no pain groups, UCA was significantly more extended in the pain group (P<0·05).
Discussion
Cervical range of motion FHP measurements were only moderately correlated with Optotrak data, and limits of agreement (LOA) and MDC95 were relatively large. There was also no difference in CROM FHP distance between older symptomatic and asymptomatic individuals. Cervical range of motion FHP measurement is therefore not recommended as a clinical outcome measure. Cervical range of motion UCA measurements showed good criterion validity, excellent test–retest reliability, and achievable MDC95 in asymptomatic and symptomatic participants. Differences of more than 6° are required to exceed error. Cervical range of motion UCA shows promise as a useful reliable and valid measurement, particularly as patients with cervical pain exhibited significantly more extended angles.
Keywords: Cervical spine, Posture, Cervical position, Reliability, Criterion validity, Cervical range of motion device
Introduction and Purpose
Cervical pain is common in individuals who work in seated postures1,2 and computer users.2,3 Extreme postural positions such as forward head posture and upper cervical extension angle (which are inter-related) may potentially contribute to stress on the cervical joints and muscles. Forward head position (FHP) is measured as the sagittal distance from C7 to the nose or the angle between C7 and the ear relative to horizontal with most studies reporting FHP as the measurement reflecting head and neck position with respect to the trunk.4–6 A more extended upper cervical angle (UCA) has been suggested to be a response to a FHP position to maintain eye gaze when there is increased anterior translation of the head.6 Although FHP is commonly observed in patients with cervical pain and is frequently reported in studies related to cervical pain,7 the strength of the relationship between FHP and cervical pain is still a topic of discussion. There have been statistically significant differences noted in FHP measurements between asymptomatic and symptomatic groups using the cervical range of motion (CROM) device4 in sitting and using photographs in standing.6 Moderate correlation between FHP measurements and neck disability measures has also been reported.7
The information from previous studies leaves gaps in our current knowledge related to cervical posture in individuals with and without pain. The lack of a reliable and valid tool to be used systematically in the clinical settings complicates research designed to address this question. While clinicians often assess posture during clinical examination, objective measurements are used less frequently. In order to further establish if postural measurements contribute to cervical dysfunction in clinical settings, an instrument which has adequate clinimetric properties is needed.8 Sophisticated quantitative measurement systems9–11 and photographic analysis12–16 provide highly reliable data, but are time consuming, while visual analysis has limited reliability.17–19 The CROM device exhibits good to excellent reliability and criterion validity for range of motion (ROM).20–23 The CROM also has moderate to excellent test–retest and moderate to good inter-rater reliability for FHP measurements.24,25 These reliability studies were conducted in standardized supported sitting and cues were used to adjust UCA position to ensure that the CROM FHP arm was horizontal. However, upper and lower cervical regions often function independently,7,26–28 and, therefore, habitual posture is not reflected if UCA is controlled while measuring FHP anterior translation. Measurements taken in naturally assumed postures without standardization would represent the patient’s actual or habitual postures. Criterion validity compared to sophisticated motion analysis equipment and minimal detectable change (MDC95) – the minimal amount of change needed to reflect true change beyond measurement error at the 95% confidence interval – have not been reported.
The purposes of this study were to establish the following for FHP and UCA measurements in a habitual seated posture: (1) criterion validity and the level of agreement between CROM measurements compared to optoelectronic measurements, (2) test–retest relative reliability and minimal detectable change at the 95% confidence level (MDC95) in asymptomatic (no pain) and symptomatic (pain) groups, and (3) to determine if FHP and UCA measures were significantly different between individuals with and without cervical pain.
Methods
This study was approved by the Human Investigation Committee at Wayne State University and informed consent was obtained from all participants. A within-subject single session design was used with three trials conducted for each participant in both Part 1 (criterion validity study) and Part 2 (reliability study). Data for the patients with pain in Part 2 were obtained from baseline testing data in a registered clinical trial [http://www.clinicaltrials.gov-identifier NCT01999283].
Part 1: criterion validity
Criterion validity and level of agreement of FHP and UCA measurements from the CROM device (deluxe version) (Performance Attainment Associates, Roseville, MN, USA; http://www.spineproducts.com) and the Optotrak Certus motion analysis system (Northern Digital, Inc., Waterloo, ON, Canada) were established.
Part 2: reliability & construct validity
Cervical range of motion FHP and UCA relative reliability measurements and MDC95 were established for age-matched individuals with cervical pain and healthy controls. Forward head position and UCA values were compared between groups.
Participants
Part 1: criterion validity
Sixteen asymptomatic young adults between 21 and 30 years of age (3 M, 13 F, age: mean (SD) 24 (2) years) were recruited from an urban research university setting. Participants were excluded if they reported a history of neck pain or trauma, surgery, vestibular problems, persistent headaches, or radicular symptoms.
Part 2: reliability & construct validity
Twenty females with cervical pain and 20 age-matched healthy controls (mean age 51 years, range 35–69 years) participated in the second part of the study. Healthy female controls with no pain were recruited as a sample of convenience. Symptomatic participants were matched based on age and sex from a data base collected for baseline measurements for an exercise intervention study. Symptomatic participants were included if they reported an average pain of ≧3/10 for more than 3 months, no symptoms of radiculopathy (numbness, tingling, or weakness), and no history of recent trauma or major medical problems.29 Participants completed the neck disability index (NDI).30
Procedures
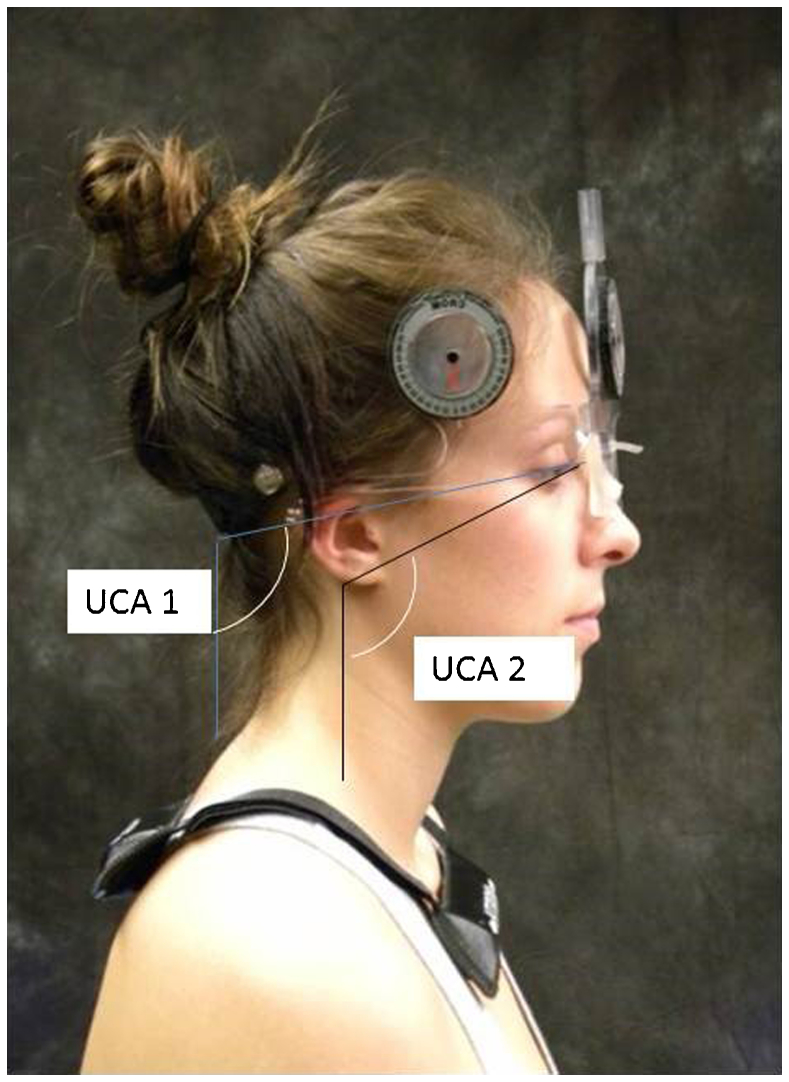
Tester variability was limited by using one tester (Part 1) and by providing at least 20 hours of training for the three testers (Part 2) until consistent procedures were established (Part 2). Participants were seated on a plinth with 90° of hip/knee flexion, both feet placed flat on the floor and hands on top of their legs. They were instructed to: ‘sit in your normal posture and to look straight ahead at a point on the wall’ defined as their habitual posture (Fig. 1) and were asked to stand up in between trials. One practice trial preceded three test trials. The CROM was placed on the bridge of the nose and ears and its location was verified between trials. The vertebral locator arm was placed on C7 which was located by asking participants to flex, and extend followed by cervical rotation while palpating for the most mobile segment in the cervicothoracic junction region.31 The embedded bubble inclinometer on the vertebral locator was used to ensure vertical alignment. The sagittal distance from the bridge of the nose to the intersection of the vertebral locator with the horizontal forward arm was used to measure FHP to the nearest 0·5 cm (Fig. 2). Upper cervical angle was recorded as the degree of flexion/extension using the sagittal inclinometer on the CROM (Fig. 3). Upper cervical angle measurements were transformed to a vertical reference consistent with optoelectronic measurements by adding 90° to provide a continuous scale without the use of negative and positive values relative to horizontal.
Figure 1.
Setup for testing position.
Figure 2.
Cervical range of motion (CROM) device forward head position (FHP) measurement.
Figure 3.
Cervical range of motion (CROM) device and Optotrak upper cervical angle (UCA) 1 and 2 measurement.
Four Optotrak Certus wireless system reflective markers were placed on: (1) the velcro strap of the CROM device under the occipital prominence (OCC), (2) spinous process of C7 (C7), (3) bridge of CROM device level with the nose (N), and (4) ear (E). The CROM device was monitored between trials to ensure that the position of the device remained stable. In addition, data corresponding to the position of the reflective markers placed on the CROM device were examined to confirm that the device remained stable across trials. Data were recorded for 6 seconds for each trial using the Optotrak system. Immediately following the Optotrak measurements the researcher recorded FHP and UCA from the CROM device.
Optoelectronic data processing
Posture data were detected from the reflective markers and recorded by four Optotrak CertusTM optoelectronic sensors placed systematically in the testing area. Data were sampled at 100 Hz and planar coordinates corresponding to each marker were recorded using NDI Toolbench software version 1.1. Data recorded using the Optotrak system have been reported to be accurate to the closest 0·1 mm with a resolution of 0·01 mm (http://www.ndigital.com). The system has been reported to have minimal measurement error and good precision, along with excellent repeatability.32
Two seconds of position data corresponding to the most stable range of the 6 second output (between 2 and 4 seconds with less than 5% variation in the output signal) were extracted for each trial.33 Two upper cervical angles, UCA 1 and UCA 2, were calculated. The OCC and N sensors (UCA 1) were used to reflect the position of the CROM device and E and N (UCA 2) to reflect the head inclination. Angles were calculated from a vertical vector projected through the most posterior marker; OCC for UCA 1 and E for UCA 2. All Optotrak angles were calculated from the caudal aspect of the vertical vector.
Statistical analysis
Part 1: criterion validity
Criterion validity of the CROM FHP and UCA measurements was established using intraclass correlation coefficients (ICC2,k), which reflect both degree of correspondence and agreement between measures.34 The means of the three trials from comparable Optotrak distances and angles were used. Limits of agreement (LOA) at the 95% confidence level were calculated from the mean (SD) of the differences between CROM and Optotrak data (Mean (CROM–OP)±2 SD Diff CROM/OP).35,36 The differences between values obtained with the two instruments and the means of the two measurements for each participant were analyzed visually using Bland–Altman plots to determine if there was any systematic bias.35
Part 2: reliability & construct validity
Intraclass correlation coefficients (ICC 3,1)37 were calculated using SPSS PASW 20 to determine test–retest reliability across three trials. Reliability coefficients were interpreted as ICCs below 0·75 indicating poor to moderate reliability, above 0·75 good reliability, and clinically acceptable or excellent reliability as greater than 0·90.34 The MDC95 (the minimum amount of change needed to reflect true change beyond measurement error at the 95% confidence interval) was calculated using the formula: MDC95 = Z × SEM × √2, where Z = 1·96, the score associated with the 95% CI, and √2 is a multiplier to account for added uncertainty when repeated measures are taken of an outcome measure. Standard error of measurement (SEM), which contributed to this calculation, was computed from the square root of the mean square error term from the ICC ANOVA tables. Finally, the FHP and UCA measurements were compared between the no pain and pain groups using independent t-tests with significance set at P<0·05. Post-hoc power analysis was performed with G*Power software to determine the achieved power for the comparisons between those with and without pain using an alpha of 0·05, equal sample sizes and the corresponding means and SD.
Results
Descriptive statistics are presented in Tables 1 and 2. Reliability and MDC95 results are presented in Table 3. For Part 1, 16 (F = 13, M = 3) young healthy individuals (mean age 24 years) participated in the study. In Part 2, 20 females (mean age 51·8 years) with chronic neck pain and 20 age-matched controls (mean age 51·7 years) participated in the study.
Table 2.
Participant demographics, forward head position (FHP) and upper cervical angle (UCA) measured with the cervical range of motion (CROM) device comparison between asymptomatic and symptomatic participants using independent t-tests (Part 2)
| Asymptomatic (n = 20) | Symptomatic (n = 20) | P | |||
|---|---|---|---|---|---|
| Mean (SD) | Range | Mean (SD) | Range | ||
| Demographics | |||||
| Age | 51·7 (8) | 35–69 | 51·8 (8) | 35–69 | P = 0·97 |
| Height (inches) | 64·7 (2) | 61–68 | 65·9 (2·7) | 63–75 | P = 0·14 |
| Weight | 161 (33) | 125–250 | 157·3 (34·9) | 123–250 | P = 0·75 |
| Pain (0–10/10) | 0 | 0 | 4·95 (1·82) | 3–8 | |
| NDI (0/50) | 3·1 (0) | 0–4 | 16·1 (5) | 8–24 | P<0·001 |
| Postural variables | |||||
| A. Forward head position (cm) 1 | 17·5 (3) | 13·5–24·8 | 16·2 (2·7) | 10·2–22 | P = 0·14 |
| B. Upper cervical angle CROM (°) 2 | 93·4 (7·2) | 79·3–106 | 99·1 (6·6) | 85·3–113·3 | P<0·01 |
Forward head measurement in sagittal plane from C7 to the bridge of the nose.
Upper cervical angles are reported with respect to the vertical.
Statistical analysis not possible due to zero value for controls.
Significant at the P<0·01 level.
Table 3.
Test–retest reliability, and minimal detectable change (MDC) for forward head position (FHP) and upper cervical angle (UCA) measured with the cervical range of motion (CROM) device and OPTOTRAK
| Group | ICC3,1 | MDC95 | MDC95 (%) | ||
|---|---|---|---|---|---|
| A. Forward head position (cm) | Optotrak | No pain (young) | 0·93 | 0·9 | 5·1 |
| CROM | No pain (young) | 0·82 | 2·9 | 14·7 | |
| No pain (older) | 0·93 | 2·5 | 13·9 | ||
| Pain (older) | 0·69 | 3·6 | 22·4 | ||
| B. Upper cervical angle (°) | Optotrak UCA 1 (occiput to nose) | No pain (young) | 0·91 | 4 | 4·3 |
| Optotrak UCA 2 (ear to nose) | No pain (young) | 0·91 | 4·1 | 3·2 | |
| CROM UCA | No pain (young) | 0·90 | 4·9 | 5·4 | |
| No pain (older) | 0·94 | 5·2 | 5·6 | ||
| Pain (older) | 0·89 | 6·3 | 6·5 |
Table 1.
Forward head position (FHP) and upper cervical angle (UCA) measured with the cervical range of motion (CROM) device and Optotrak for younger asymptomatic participants (Part 1)
| CROM | Optotrak | ||||
|---|---|---|---|---|---|
| Mean (SD) | Range | Mean (SD) | Range | ||
| A. Forward head position (cm) 1 | 19·75 (2·3) | 15·3–3·3 | 18·27 (1·2) | 16·18–20·3 | |
| B. Upper cervical angle (°) 2 | UCA 1 (Occiput–nose) | 90·7 (5·3) | 80–97·3 | 92·4 (4·7) | 82·7–100 |
| UCA 2 (ear–nose) | 128·3 (4·9) | 120·9–138·5 | |||
Forward head measurement in sagittal plane from C7 to the bridge of the nose.
Upper cervical angles are reported with respect to the vertical.
Part 1: criterion validity
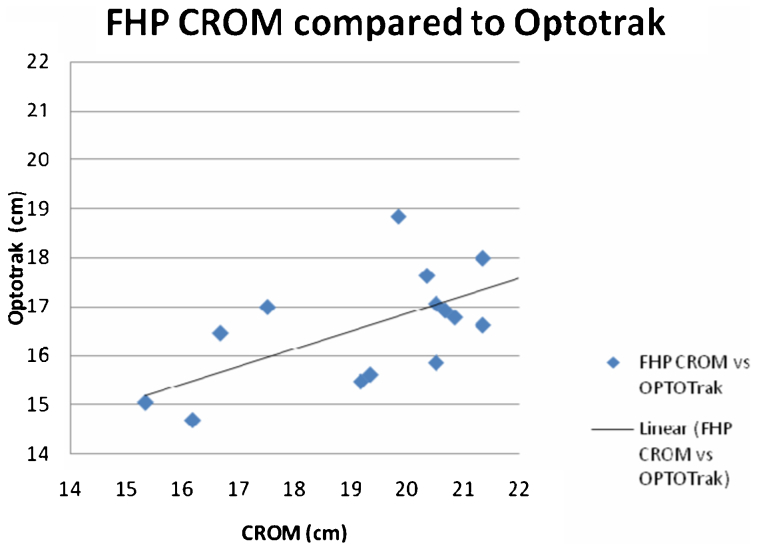
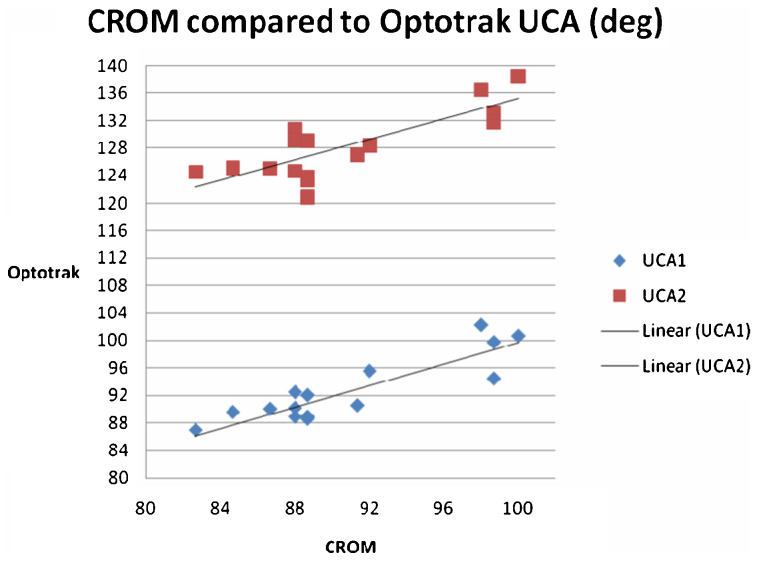
Cervical range of motion and Optotrak FHP distance means were moderately correlated in the young asymptomatic participants (ICC2,k = 0·72) (Fig. 4). Means for UCA angles were highly correlated (UCA 1 ICC2,k = 0·94, UCA 2 ICC2,k = 0·89) indicating that angles calculated from markers placed on the CROM (UCA 1) and on the head (UCA 2) were similarly associated with Optotrak measurements (Fig. 5).
Figure 4.
Part 1: Criterion validity study comparison of forward head position (FHP) measurements recorded from the cervical range of motion (CROM) device compared to the Optotrak. (1) CROM and Optotrak measurements moderately correlated (ICC2,k = 0·72). (2) Measurements corresponding to distance from C7 to the nose in the sagittal plane measured in centimeters.
Figure 5.
Part 1: Criterion validity study comparison of upper cervical angle (UCA) measurements recorded from the cervical range of motion (CROM) device compared to the Optotrak. (1) CROM and Optotrak UCA angle measurements were highly correlated (UCA 1 ICC2,k = 0·94, UCA 2 ICC2,k = 0·89). (2) Optotrak UCA 1 calculated from markers on the occiput, nose relative to a vertical vector from the occipital marker analogous to the position of the CROM, UCA 2 calculated from markers on occiput, ear relative to the same vertical vector analogous to the head inclination.
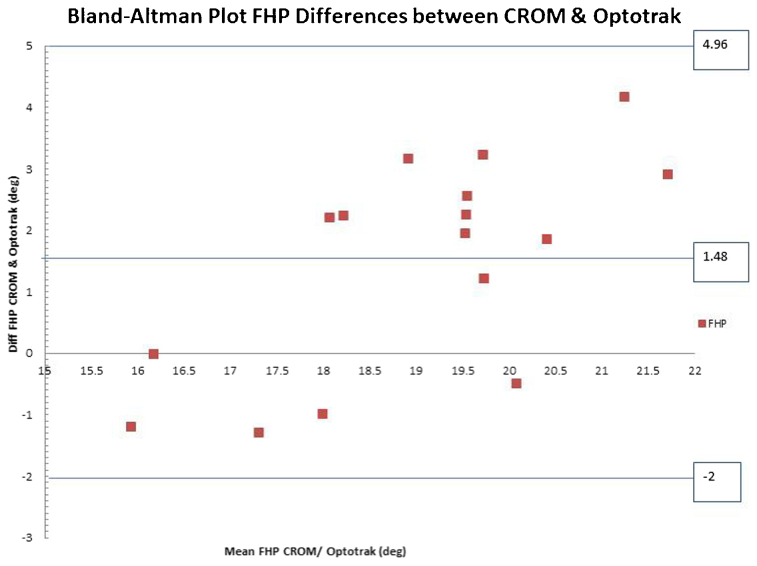
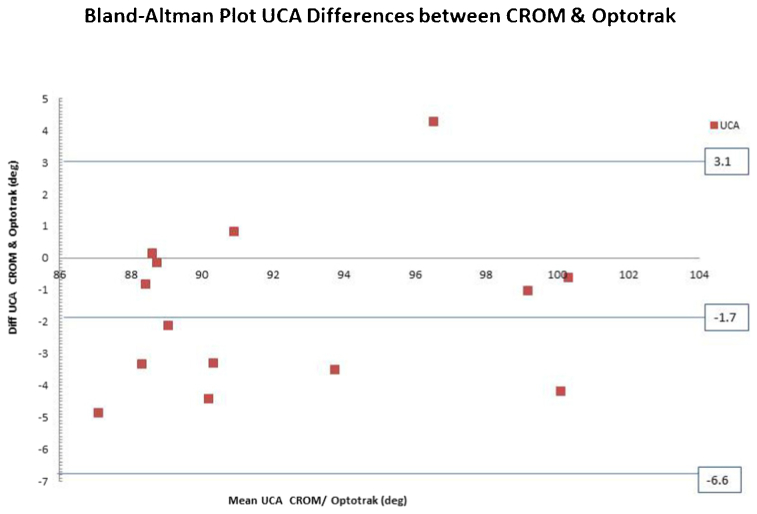
The mean (SD) of the FHP difference scores between the CROM compared to the Optotrak data were 1·48 (1·74) cm with the 95% LOA equal to −2–4·94 cm. While there was no systematic bias observed on the Bland–Altman plot, CROM FHP measurements were greater than Optotrak measurements in some participants (Fig. 6). The mean (SD) difference in scores between instruments for UCA 1 was −1·73(2·46)° with a 95% LOA of −6·65–3·19° (Fig. 7). The CROM angular measurements were slightly more flexed than the Optotrak UCA values, but the LOA were within acceptable ranges and there was no systematic bias.
Figure 6.
Bland–Altman plot – differences between cervical range of motion (CROM) device and Optotrak forward head position (FHP) distance measurements related to the mean of the CROM device/Optotrak FHP measurements.
Figure 7.
Bland–Altman Plot – difference between cervical range of motion (CROM) device and Optotrak upper cervical angle (UCA) compared to mean of CROM device/Optotrak UCA 1.
Part 2: reliability (Table 3)
Test–retest relative reliability of FHP CROM measurements was good to excellent for asymptomatic (ICC3,1 = 0·82 {Part 1 young}, = 0·93 {Part 2 older}) and only moderate for symptomatic older adults (ICC3,1 = 0·69). Cervical range of motion UCA reliability was excellent for both asymptomatic ICC3·1 = 0·90 {young}, = ICC3·1 = 0·94 {older}, and symptomatic participants (ICC3·1 = 0·89 {older}). The Optotrak measurements exhibited excellent reliability (OP FHP ICC3,1 = 0·93; UCA 1 & 2 ICC3,1 = 0·91).
Part 2: minimal detectable change (Table 3)
Cervical range of motion FHP MDC95/MDC95% for the young asymptomatic participants was feasible (2·9 cm, 14·7%), but was three times larger than the distance required to exceed error for Optotrak FHP (0·9 cm, 5·1%). Forward head position MDC95 distance was 1 cm larger in the symptomatic older participants (3·6 cm, 22·4%), compared to the asymptomatic participants (2·5 cm, 13·9%).
MDC95/MDC95% for CROM UCA measurements were low and feasible for participants without pain (4·9–5·2°/5·4–5·6%) and similar to Optotrak values (4°/4·3%). The MDC95 values for participants with pain only differed by a degree (6·3°/6·5%).
Part 2: differences in asymptomatic and symptomatic groups
There was no difference in FHP distances between the older participants with and without pain. Post hoc power analysis of FHP results using the means and SD listed in Table 2 revealed an effect size of d = 0·45 considered to be medium (Cohen’s d) and rendered a power of 0·30. The UCA measurements in these same participants were however, significantly more extended in the older participants with pain than those without pain (P<0·01). The effect size for UCA (d = 0·71) can be considered large (Cohen’s d) and rendered a power of 0·72.
Discussion
The purposes of this study were to establish (1) criterion validity of FHP and UCA CROM compared to optoelectronic measurements, (2) test–retest relative reliability and MDC95 in asymptomatic and symptomatic groups, and (3) if FHP and UCA measures differed between individuals with and without neck pain.
The CROM FHP measurements did not provide sufficient concurrent criterion validity relative to the comparable Optotrak FHP distances to be considered as a suitable alternative to the optoelectronic measurements. Positive correlations between CROM and Optotrak FHP distances (ICC2,k = 0·72) were only moderate. The FHP LOA at the 95% CI was also large for a measure with physiological range limits (2–4·94 cm). It is possible that FHP measurements were influenced by angulation of the instrument with UCA adjustments or anatomical variations. If the CROM FHP arm was slanted, there was difficulty reading the intersection of the vertebral locator between the divisions which could have contributed to error. The CROM increments of measurement (0·5 cm) may not reflect subtle postural changes, a limitation of the instrument discussed by other authors.24,25 Although the newer model of the CROM has 1° increments for ROM measurement, the FHP divisions have not been changed. The reference point for the CROM on the head should be considered a limitation for measurement of FHP.
Same-day test–retest reliability of CROM FHP measurements for asymptomatic participants was good to excellent (ICC3,1 = 0·82, 0·93), but only moderate for the older participants with pain (ICC3,1 = 0·69). The CROM FHP test–retest reliability in the young no pain group (ICC3,1 = 0·82) was similar to results to those reported by Hickey et al.25 for young asymptomatic participants (mean age 25 years) (ICC2,1 = 0·77). These results suggest that reliability in young asymptomatic participants, in both supported and unsupported seated testing positions, is consistent. In this study, the reliability of CROM FHP measurements in the older participants with pain (ICC3,1 = 0·69) was lower than the reliability reported for participants of similar age with cervical and shoulder dysfunction by Garrett et al. (ICC1,1 = 0·93).24 Differences may be related to the fact that habitual postures were used in the present study compared to using standardized postures in Garrett et al.24 The good test–retest reliability without standardization indicates that asymptomatic individuals appear to assume unsupported habitual postures with some degree of repeatability. The slightly lower test–retest reliability and larger measurement error noted in older individuals with pain (in this study between 35 and 69 years old) is of interest, and postural variability in the presence of pain in this age group is worthy of future investigations.
MDC95 is a useful indicator for clinicians and researchers to gage individual improvement which exceeds variability due to error. MDC95 and MDC95% for CROM FHP measurement in young asymptomatic participants (2·9 cm/14·7%), was larger than the Optotrak FHP values, which were less than 1 cm (0·9 cm/5·1%). The FHP MDC95% in the older participants with pain was larger and the amount of change required to exceed measurement error was large particularly as there are physiological end range limits (3·6 cm/22%). The results from this study do not support the use of CROM FHP measurements in naturally assumed seated postures based on moderate criterion validity and reliability and MDC95 values which are likely to be difficult to achieve in older individuals with pain.
The CROM UCA, however, provided measurements which were extremely comparable to Optotrak angles reflecting both the position of the CROM and the participant (ICC2,k = 0·94, 0·89). The LOA between the instruments was feasible (−6·7−3·2°) and consistent with previous ROM criterion validity.21,22 Test–retest reliability in individuals with and without pain was excellent (ICC3,1>0·90) with feasible MDC95 (4–5°/3–5%). Previous studies using the CROM have standardized the UCA to achieve 0° flexion/extension24,25 and used the back of the chair to ensure a horizontal position of the FHP arm, however, the habitual or natural position used in this study demonstrated good UCA repeatability. This finding supports the use of the instrument in clinical settings when no instructions or external supports are provided.
There is limited research comparing UCA between individuals with and without neck pain and these studies did not find statistical significant differences between groups.6,38 In this study, older individuals with pain exhibited a significantly more extended UCA than age-matched asymptomatic individuals without pain (P<0·05) while there were no differences in FHP distances between the groups. Increased upper cervical extension might represent natural adjustments to compensate for mobility restrictions in the lower cervical or thoracic regions, or alterations in the deep flexor39–41 and extensor42,43 postural muscle support. Prolonged or maximal upper cervical extension required to maintain eye gaze may contribute to increased loading of the upper cervical joints. Elliott et al.42 observed increased use of the superficial extensor muscles and less activity of the small deep cervical extensors with craniocervical extension in prone at low levels of muscle contraction in normal individuals. While numerous studies have implicated the deep neck flexors as being inhibited in patients with cervical pain,39–41 less research has focused on possible contributions from the extensor muscles or distinguished between upper and lower cervical region adjustments. Further investigation of UCA in individuals with chronic neck pain is needed.
The relationship and function of the upper and lower cervical spine are inter-related7,26–28 but may also be influenced by adjustments in lumbar,44 upper thoracic,18 and shoulder position.2 This study provides preliminary support for the use of UCA as a measurement of postural position using the CROM in habitual posture rather than standardized positions, with the acknowledgment that other spinal postural combinations may influence UCA position.
The reliability of postural measurements will be influenced by tester and participant variability, consistency of instructions, or the measurement device itself. Tester variability was limited by using one tester (Part 1) or training (Part 2), while consistency of instructions was ensured. In order to establish the level of agreement between the CROM and Optotrak devices, concurrent measurement was conducted. As the Optotrak provided highly reliable results with low measurement error, the moderate agreement between the CROM and the Optotrak measurements suggests that error contributions from the CROM instrument or the tester were more likely than individual participant variation between trials.
Limitations related to this study need to be acknowledged. This cross-sectional study included only females within a specific age range. The results may not extrapolate to males, or to those outside the age ranges studied. While MDC is an important consideration, determining clinically important differences requires longitudinal study of the measures.
Conclusions
Cervical range of motion FHP measurements, although demonstrating good reliability in asymptomatic participants, were only moderately correlated with Optotrak data, and LOA and MDC95 were relatively large. There was also no difference in CROM FHP distance between older symptomatic and asymptomatic individuals. Cervical range of motion FHP is, therefore, not recommended as a clinical outcome measure.
Cervical range of motion UCA measurements showed good criterion validity, excellent test–retest reliability, and achievable MDC95 in asymptomatic and symptomatic participants. Differences of more than 6° are required to exceed measurement error. Participants with cervical pain exhibited a significantly more extended UCA. Cervical range of motion UCA shows promise as a useful reliable and valid measurement option.
Disclaimer Statements
Contributors All authors contributed to concept and design of the study and approved the final version. Joseph Neil PT, DPT and Allison Tallon PT, DPT performed data collection and analysis for Part 1. Kim Dunleavy PhD, PT, OCS was the primary investigator for the data collected in Part 2. Kim Dunleavy PhD, PT, OCS and Diane Adamo PhD, OT contributed statistical analysis, and interpretation of data.
Funding Funding for data collection for the participants with neck pain was provided by the Physical Therapy Program, Wayne State University and by the Eugene Applebaum College of Pharmacy and Health Sciences Faculty Research Award.
Conflicts of interest Data collection for Part 1 and for the normal participants in Part 2 was conducted in partial fulfillment for entry-level doctoral research requirements for the Physical Therapy Program at Wayne State University, Detroit, MI, USA in the Motion Analysis Laboratory. Thanks to Nicole Widak PT, DPT who provided assistance with Optotrak data processing for Part 1. Thanks to Katherine Vezina PT, DPT, Nicole Widak PT, DPT, Julie Khoung PT, DPT, Elana Bodzin PT, DPT, Amanda Rowley PT, DPT who assisted with participant recruitment and data collection for Part 2.
Ethics approval Research for all components of the data presented in this paper was approved by the Wayne State University Institutional Review Board.
References
- 1.Rossignol AM, Morse EP, Summers VM, Pagnotto LD. Video display terminal use and reported health symptoms among Massachusetts clerical workers. J Occup Med. 1987;29:112–8. [PubMed] [Google Scholar]
- 2.Szeto GP, Straker L, Raine S. A field comparison of neck and shoulder postures in symptomatic and asymptomatic office workers. Appl Ergon. 2002;33:75–84. [DOI] [PubMed] [Google Scholar]
- 3.Szeto GP, Straker LM, O'Sullivan PB. A comparison of symptomatic and asymptomatic office workers performing monotonous keyboard work–2: neck and shoulder kinematics. Man Ther. 2005;10:281–91. [DOI] [PubMed] [Google Scholar]
- 4.Haughie L, Fiebert I, Roach K. Relationship of forward head posture and cervical backward bending to neck pain. J Man Manip Ther. 1995;3:91–7. [Google Scholar]
- 5.Shiau YY, Chai HM. Body posture and hand strength of patients with temporomandibular disorder. J Craniomandibular Pract. 1990;8:244–51. [DOI] [PubMed] [Google Scholar]
- 6.Silva AG, Punt TD, Sharples P, Vilas-Boas JP, Johnson MI. Head posture and neck pain of chronic nontraumatic origin: a comparison between patients and pain-free persons. Arch Phys Med Rehabil. 2009;90:669–74. [DOI] [PubMed] [Google Scholar]
- 7.Yip CH, Chiu TT, Poon AT. The relationship between head posture and severity and disability of patients with neck pain. Man Ther. 2008;13:148–54. [DOI] [PubMed] [Google Scholar]
- 8.Fortin C, Feldman DE, Cheriet F, Labelle H. Clinical methods for quantifying body segment posture: a literature review. Disabil Rehabil. 2011;33:367–83. [DOI] [PubMed] [Google Scholar]
- 9.Keshner EA. Head-trunk coordination during linear anterior–posterior translations. J Neurophysiol. 2003;89:1891–901. [DOI] [PubMed] [Google Scholar]
- 10.Keshner EA. Head-trunk coordination in elderly subjects during linear anterior–posterior translations. Exp Brain Res. 2004;158:213–22. [DOI] [PubMed] [Google Scholar]
- 11.Zabjek KF, Leroux MA, Coillard C, Rivard CH, Prince F. Evaluation of segmental postural characteristics during quiet standing in control and Idiopathic Scoliosis patients. Clin Biomech (Bristol, Avon). 2005;20:483–90. [DOI] [PubMed] [Google Scholar]
- 12.Armijo-Olivo S, Jara X, Castillo N, Alfonso L, Schilling A, Valenzuela E,. et al A comparison of the head and cervical posture between the self-balanced position and the Frankfurt method. J Oral Rehabil. 2006;33:194–201. [DOI] [PubMed] [Google Scholar]
- 13.Edmondston SJ, Sharp M, Symes A, Alhabib N, Allison GT. Changes in mechanical load and extensor muscle activity in the cervico-thoracic spine induced by sitting posture modification. Ergonomics. 2011;54:179–86. [DOI] [PubMed] [Google Scholar]
- 14.Grimmer-Somers K, Milanese S, Louw Q. Measurement of cervical posture in the sagittal plane. J Manipulative Physiol Ther. 2008;31:509–17. [DOI] [PubMed] [Google Scholar]
- 15.Lau KT, Cheung KY, Chan KB, Chan MH, Lo KY, Chiu TT. Relationships between sagittal postures of thoracic and cervical spine, presence of neck pain, neck pain severity and disability. Man Ther. 2010;15:457–62. [DOI] [PubMed] [Google Scholar]
- 16.van Niekerk SM, Louw Q, Vaughan C, Grimmer-Somers K, Schreve K. Photographic measurement of upper-body sitting posture of high school students: a reliability and validity study. BMC Musculoskelet Disord. 2008;9:113. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Fedorak C, Ashworth N, Marshall J, Paull H. Reliability of the visual assessment of cervical and lumbar lordosis: how good are we? Spine (Phila Pa 1976). 2003;28:1857–9. [DOI] [PubMed] [Google Scholar]
- 18.Gadotti I, Armijo-Olivo S, Silveira A, Magee D. Intra and inter-rater reliability of the craniocervical posture – photogrammetry vs visual assessment. World Conference of Physiotherapy; Amsterdam, Netherlands; 2011. [DOI] [PubMed] [Google Scholar]
- 19.Silva AG, Punt TD, Johnson MI. Reliability and validity of head posture assessment by observation and a four-category scale. Man Ther. 2010;15:490–5. [DOI] [PubMed] [Google Scholar]
- 20.Audette I, Dumas JP, Cote JN, De Serres SJ. Validity and between-day reliability of the cervical range of motion (CROM) device. J Orthop Sports Phys Ther. 2010;40:318–23. [DOI] [PubMed] [Google Scholar]
- 21.Tousignant M, de Bellefeuille L, O'Donoughue S, Grahovac S. Criterion validity of the cervical range of motion (CROM) goniometer for cervical flexion and extension. Spine (Phila Pa 1976). 2000;25:324–30. [DOI] [PubMed] [Google Scholar]
- 22.Tousignant M, Smeesters C, Breton AM, Breton E, Corriveau H. Criterion validity study of the cervical range of motion (CROM) device for rotational range of motion on healthy adults. J Orthop Sports Phys Ther. 2006;36:242–8. [DOI] [PubMed] [Google Scholar]
- 23.Fletcher JP, Bandy WD. Intrarater reliability of CROM measurement of cervical spine active range of motion in persons with and without neck pain. J Orthop Sports Phys Ther. 2008;38:640–5. [DOI] [PubMed] [Google Scholar]
- 24.Garrett TR, Youdas JW, Madson TJ. Reliability of measuring forward head posture in a clinical setting. J Orthop Sports Phys Ther. 1993;17:155–60. [DOI] [PubMed] [Google Scholar]
- 25.Hickey E, Rondeau M, Corrente J, Abysath J, Seymour C. Reliability of the cervical range of motion (CROM) device and plumb-line techniques in measuring resting head posture (RHP). J Man Manip Ther. 2000;8:10–7. [Google Scholar]
- 26.Bogduk N, Mercer S. Biomechanics of the cervical spine. I: normal kinematics. Clin Biomech (Bristol, Avon). 2000;15:633–48. [DOI] [PubMed] [Google Scholar]
- 27.Caneiro JP, O'Sullivan P, Burnett A, Barach A, O'Neil D, Tveit O,. et al The influence of different sitting postures on head/neck posture and muscle activity. Man Ther. 2010;15:54–60. [DOI] [PubMed] [Google Scholar]
- 28.Wu SK, Lan HH, Kuo LC, Tsai SW, Chen CL, Su FC. The feasibility of a video-based motion analysis system in measuring the segmental movements between upper and lower cervical spine. Gait Posture. 2007;26:161–6. [DOI] [PubMed] [Google Scholar]
- 29.Dunleavy K, Goldberg A. Comparison of cervical range of motion in two seated postural conditions in adults 50 or older with cervical pain. J Man Manip Ther. 2013;21:33–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.En MC, Clair DA, Edmondston SJ. Validity of the neck disability index and neck pain and disability scale for measuring disability associated with chronic, non-traumatic neck pain. Man Ther. 2009;14:433–8. [DOI] [PubMed] [Google Scholar]
- 31.Palmer M, Epler M. Clinical assessment procedures in physical therapy. New York: J.B. Lippincott; 1990. [Google Scholar]
- 32.States RA, Pappas E. Precision and repeatability of the Optotrak 3020 motion measurement system. J Med Eng Technol. 2006;30:11–6. [DOI] [PubMed] [Google Scholar]
- 33.Adamo DE, Scotland S, Martin BJ. Asymmetry in grasp force matching and sense of effort. Exp Brain Res. 2012;217:273–85. [DOI] [PubMed] [Google Scholar]
- 34.Portney L, Watkins M. Foundations of clinical research: applications to practice, 3rd edn. Upper Saddle River, NJ: Pearson Prentice Hall; 2009. [Google Scholar]
- 35.Bland JM, Altman DG. Statistical methods for assessing agreement between two methods of clinical measurement. Lancet. 1986;1:307–10. [PubMed] [Google Scholar]
- 36.Ottenbacher KJ, Stull GA. The analysis and interpretation of method comparison studies in rehabilitation research. Am J Phys Med Rehabil. 1993;72:266–71. [DOI] [PubMed] [Google Scholar]
- 37.Shrout PE, Fleiss JL. Intraclass correlations: uses in assessing rater reliability. Psychol Bull. 1979;86:420–8. [DOI] [PubMed] [Google Scholar]
- 38.Harrison AL, Barry-Greb T, Wojtowicz G. Clinical measurement of head and shoulder posture variables. J Orthop Sports Phys Ther. 1996;23:353–61. [DOI] [PubMed] [Google Scholar]
- 39.Falla D, O'Leary S, Fagan A, Jull G. Recruitment of the deep cervical flexor muscles during a postural-correction exercise performed in sitting. Man Ther. 2007;12:139–43. [DOI] [PubMed] [Google Scholar]
- 40.Falla D, O'Leary S, Farina D, Jull G. The change in deep cervical flexor activity after training is associated with the degree of pain reduction in patients with chronic neck pain. Clin J Pain. 2012;28:628–34. [DOI] [PubMed] [Google Scholar]
- 41.Falla D, Jull G, Russell T, Vicenzino B, Hodges P. Effect of neck exercise on sitting posture in patients with chronic neck pain. Phys Ther. 2007;87:408–17. [DOI] [PubMed] [Google Scholar]
- 42.Elliott JM, O'Leary SP, Cagnie B, Durbridge G, Danneels L, Jull G. Craniocervical orientation affects muscle activation when exercising the cervical extensors in healthy subjects. Arch Phys Med Rehabil. 2010;91:1418–22. [DOI] [PubMed] [Google Scholar]
- 43.Cagnie B, O'Leary S, Elliott J, Peeters I, Parlevliet T, Danneels L. Pain-induced changes in the activity of the cervical extensor muscles evaluated by muscle functional magnetic resonance imaging. Clin J Pain. 2011;27(5):392–7. [DOI] [PubMed] [Google Scholar]
- 44.Kuo YL, Tully EA, Galea MP. Video analysis of sagittal spinal posture in healthy young and older adults. J Manipulative Physiol Ther. 2009;32:210–5. [DOI] [PubMed] [Google Scholar]