Abstract
Background
One million neonates die each year in low- and middle-income countries because of neonatal sepsis; group B Streptococcus (GBS) and Escherichia coli are the leading causes. In sub-Saharan Africa, epidemiological data on vaginal GBS and E. coli carriage, a prerequisite for GBS and E. coli neonatal sepsis, respectively, are scarce but necessary to design and implement prevention strategies. Therefore, we assessed vaginal GBS and E. coli carriage rates and risk factors and the GBS serotype distribution in three sub-Saharan countries.
Methods
A total of 430 women from Kenya, Rwanda and South Africa were studied cross-sectionally. Vaginal carriage of GBS and E. coli, and GBS serotype were assessed using molecular techniques. Risk factors for carriage were identified using multivariable logistic regression analysis.
Results
Vaginal carriage rates in reference groups from Kenya and South Africa were 20.2% (95% CI, 13.7–28.7%) and 23.1% (95% CI, 16.2–31.9%), respectively for GBS; and 25.0% (95% CI, 17.8–33.9%) and 27.1% (95% CI, 19.6–36.2%), respectively for E. coli. GBS serotypes Ia (36.8%), V (26.3%) and III (14.0%) were most prevalent. Factors independently associated with GBS and E. coli carriage were Candida albicans, an intermediate vaginal microbiome, bacterial vaginosis, recent vaginal intercourse, vaginal washing, cervical ectopy and working as a sex worker. GBS and E. coli carriage were positively associated.
Conclusions
Reduced vaginal GBS carriage rates might be accomplished by advocating behavioral changes such as abstinence from sexual intercourse and by avoidance of vaginal washing during late pregnancy. It might be advisable to explore the inclusion of vaginal carriage of C. albicans, GBS, E. coli and of the presence of cervical ectopy in a risk- and/or screening-based administration of antibiotic prophylaxis. Current phase II GBS vaccines (a trivalent vaccine targeting serotypes Ia, Ib, and III, and a conjugate vaccine targeting serotype III) would not protect the majority of women against carriage in our study population.
Introduction
One million children die each year in low- and middle-income countries in the first 4 weeks of life because of neonatal sepsis [1]. Early-onset neonatal sepsis (EOS), occurring in the first week of life, accounts for approximately 80% of cases, and is caused by bacteria that are transmitted vertically from the genital tract of the mother to infant before or during delivery [2]. Late-onset neonatal sepsis (LOS) occurs between week 1 and month 2 to 3 of life and may be caused by bacteria acquired vertically or horizontally [3]. Because the transfer of a single species from the maternal genitourinary tract to the neonate before or during delivery is a prerequisite for EOS [4], there are unique opportunities for prevention of EOS.
At present, Streptococcus agalactiae (Group B Streptococcus, GBS) and Escherichia coli are the leading causes of EOS worldwide [5]. Furthermore, GBS and E. coli are associated with preterm birth, very-low-birth-weight delivery and puerperal sepsis [6, 7], which cause substantial morbidity and mortality in sub-Saharan Africa (SSA) [2, 8, 9].
To prevent EOS, efforts have been focusing mainly on GBS and high-income countries, based on two strategies, namely the screening- or risk-based administration of intrapartum antibiotic prophylaxis (IAP) and the development of vaccines [10].
IAP has been shown to reduce the incidence of GBS EOS from 1.7/1000 to 0.6/1000 in the US [11], but is not effective against E. coli EOS, LOS, and adverse perinatal outcomes related to GBS [12, 13]. Furthermore, according to the current universal guidelines (Centers for Disease Control and Prevention, CDC), IAP should be administered to women found positive for GBS at 35–37 weeks of gestation [14]. However, these guidelines are not followed in most health-care facilities in low-income countries. The use of intravaginal washes with chlorhexidine (a wide-spectrum microbicide) during labour and neonatal wipes with chlorhexidine, has been explored in low- and middle-income countries, but is unlikely to prevent vertically acquired neonatal infections in any setting or population [4].
Most GBS vaccines under development aim at eliciting protective antibodies against capsular polysaccharides (CPS), the most important GBS virulence factor of which ten antigenically distinct CPS are known [10], and are attractive as some of the IAP-related problems may be circumvented [10]. However, these vaccines might not be effective in low-income countries because of different serotype distribution [15].
Although SSA has the highest rates of neonatal sepsis mortality worldwide, epidemiological data on vaginal GBS and E. coli carriage are very limited but necessary to develop and implement prevention strategies [16, 17]. Therefore, in this multi-country cross-sectional study, we assessed the vaginal GBS and E. coli carriage prevalence, risk factors for GBS and E. coli carriage, and GBS serotype distribution in populations from three countries: Kenya, Rwanda and South Africa.
Patients and Methods
Study design and population
In 2010–2011, we conducted a multi-country follow-up study entitled ‘‘Characterisation of novel microbicide safety biomarkers in East and South Africa”. The main aim of that project was to characterise the vaginal microbiome and the cervicovaginal mucosal immune system in African women and to assess changes of these over time [18–21]. In that study, 430 women were recruited at three study sites, i.e. the International Centre for Reproductive Health Kenya (ICRHK) in Mombasa, Kenya (170 women); the non-governmental organisation Rinda Ubuzima (RU) in Kigali, Rwanda (60 women), and the Wits Reproductive Health and HIV Institute (Wits RHI) in Johannesburg, South Africa (SA) (200 women). The women were recruited into 6 predefined study groups: a reference group of 219 women (adult, non-pregnant, HIV-negative women at average risk of HIV), 60 pregnant women (up to 14 weeks of gestational age as determined by abdominal ultrasound at recruitment), 60 adolescent girls (16–17 years), 31 HIV-negative women engaging in vaginal practices (usage of cloth, lemon juice, or detergents to clean, dry or tighten the vagina on a regular basis), 30 self-acknowledged female sex workers (FSW), and 30 HIV-positive women (on antiretroviral treatment for at least 6 months, asymptomatic and with a CD4 count of more than 350 cells/μl) (Table 1). Participants were eligible for inclusion if they were in good physical and mental health, able and willing to participate in the study as required by the protocol, able and willing to give written informed consent (including written parental or guardian consent for adolescents). Women were excluded if they had never had penetrative vaginal intercourse, if they had a history of hysterectomy or other genital tract surgery in the three months prior to the screening visit, if external and/or internal genital warts were found, if they were enrolled in HIV prevention trials involving investigational products, if they were less than 6 months post-partum at the time of enrolment, if they were HIV-positive (unless for inclusion in the HIV-positive women group), or if they were pregnant (unless for inclusion in the pregnant women group). The study population, followed up for approximately eight months per person over 8 visits, is described in detail by Jespers and coworkers [19].
Table 1. Study population and vaginal GBS and E. coli carriage rates.
| City, Country | Group | n | GBS prevalence % (95% CI) | E. coli prevalence % (95% CI) |
|---|---|---|---|---|
| Mombasa, Kenya | Reference group | 110 | 20.2 (13.7–28.7) | 25.0 (17.8–33.9) |
| Mombasa, Kenya | Pregnant women | 30 | 14.3 (5.7–31.5) | 14.3 (5.7–31.5) |
| Mombasa, Kenya | Adolescents | 30 | 3.6 (0.6–17.7) | 28.6 (15.3–47.1) |
| Kigali, Rwanda | FSW | 30 | 20.0 (9.5–37.3) | 70.0 (52.1–83.3) |
| Kigali, Rwanda | HIV+ women | 30 | 0.0 (0.0–11.4) | 20.0 (9.5–37.3) |
| Johannesburg, SA | Reference group | 109 | 23.2 (16.2–31.9) | 27.1 (19.6–36.2) |
| Johannesburg, SA | Pregnant women | 30 | 10.0 (3.5–25.6) | 33.3 (19.2–51.2) |
| Johannesburg, SA | Adolescents | 30 | 0.0 (0.0–11.4) | 13.3 (5.3–29.7) |
| Johannesburg, SA | Vaginal practices | 31 | 25.8 (13.7–43.2) | 30.0 (16.7–47.9) |
The current study presents one of the tertiary objectives of the above mentioned study, namely to document the vaginal carriage rates of the main pathogens associated with EOS (GBS and E. coli) and the risk factors for their carriage. These analyses are based on the screening visit and the first visit (scheduled soon after the last day (day 9 +/- 2 days) of the menstrual period) from the follow-up study.
Study procedures
At the screening visit, blood, vaginal, endocervical and urine samples were taken for diagnostic testing of HIV, HSV-2, syphilis, Neisseria gonorrheae (NG), Chlamydia trachomatis (CT), Trichomonas vaginalis (TV), urinary tract infection (UTI), pregnancy, cervical dysplasia (by Pap smear), bacterial vaginosis (BV) (Amsel criteria), and vaginal candidiasis. Treatment was provided according to national guidelines, voluntary HIV counseling was offered, and condoms were provided free-of-charge.
At visit 1, two sterile Copan flocked® vaginal swabs (Copan Diagnostics, Inc., Murrieta, CA), to be used for the molecular detection of GBS and E. coli, were brought into the vaginal vault by the study clinician, rotated against the vaginal wall at the midportion of the vault, gently dipped in the posterior fornix and carefully removed to prevent contamination with the microbiome of the vulva and introitus. The swab heads were collected into two 1.5 ml cryovials, labelled and immediately frozen at -80°C until shipment to the central laboratory at the Institute of Tropical Medicine (ITM, Antwerp, Belgium) using temperature-monitored dry shippers filled with liquid nitrogen. One Amies swab (Copan Diagnostics, Inc.) for culturing was taken in a likewise manner, placed in the Amies tube, and transported at 4°C in a temperature-monitored cooler to the local laboratory, where it was processed immediately. At both visits, women were interviewed during face-to-face interviews about their general and sexual health, vaginal habits and sociodemographic characteristics. A physical examination including speculum and bimanual pelvic examination was carried out by a clinician. At each visit, participants were compensated for their time and transportation.
Diagnosis of genital infections
At the local laboratories, tests for HIV, HSV-2, syphilis, CT and NG were performed. For immediate detection of Candida cells and hyphae, TV, and clue cells, wet mount microscopy was used. For the purpose of this study, a commercially available TV InPouchTM system (BioMed Diagnostics, White City, Oregon) was used. For this, a vaginal swab was inoculated according to the manufacturer’s instructions and InPouch cultures were monitored on a daily basis. InPouch bags with no growth at the end of five days were considered negative. BV diagnosed according to the Amsel criteria was used for immediate treatment. For research, vaginal smears were made and sent to ITM for Gram staining and Nugent scoring, a scoring system to diagnose BV. Briefly, smears from vaginal swabs were prepared by rolling the swab onto a glass slide. Slides were air-dried and fixed using 70% ethanol. For the Gram-staining at ITM, the fixed smear was covered with crystal violet for 1 minute, washed with water, flooded with Lugol’s iodine for 1 minute, washed with water, and then decolorized with acetone-alcohol for 2–3 seconds. The smears were rinsed quickly under running water to stop the decolorisation and then counterstained with safranin for 1 minute. All reagents were from Becton Dickinson (BD). All smears were examined microscopically with the 40X objective to check the staining and the distribution of the material, and then assessed under oil immersion objective (1000x magnification) using the grading system described by Nugent and co-workers [22]. The Nugent score is calculated by assessing for the presence of Lactobacillus cell types, small Gram-variable coccobacilli, and curved Gram-variable rods. A score of 0–3 is considered as normal (BV-negative); a score of 4–6 as an intermediate vaginal microbiome; and a score of 7–10 as BV-positive.
DNA extraction
For the molecular detection of GBS and E. coli, DNA extraction from the two Copan swabs of each subject was carried out at ITM by thawing the swabs at room temperature for 30 minutes. After adding 1200 μL of diluted PBS, each swab was gently vortexed for 15 seconds, and 1 mL of each swab suspension was pooled into a final volume of 2 mL. An aliquot of 250 μL was extracted using the Abbott m24sp automated extraction platform (Abbott, Maidenhead, UK), according to the manufacturer’s instructions, and 200 μl of eluted DNA—to be used in the quantitative PCR (qPCR) assays—was stored at– 80°C.
For the construction of qPCR standard curves, DNA was extracted from overnight cultures of S. agalactiae LMG 14694T on TSA + 5% sheep blood, E. coli ATCC 25922 grown on TSA + 5% sheep blood, and C. albicans ATCC 90028 grown on Sabouraud agar (all BD). All growth was harvested from the plate and resuspended in 1 ml of saline. DNA of this suspension was extracted using the High Pure PCR Template Preparation Kit (Roche Applied Science, Basel, Switzerland) according to the manufacturer’s instructions.
For capsular genotyping of GBS, 1 ml of inoculated Lim Broth medium (see Microbiological culturing) was used for DNA extraction using the High Pure PCR Template Preparation Kit (Roche), according to the the manufacturer’s instructions.
Streptococcus agalactiae qPCR
To detect S. agalactiae in vaginal DNA extracts, a S. agalactiae specific qPCR was carried out, using primers previously described [23]. The qPCR reactions for S. agalactiae were performed in a final volume of 10 μl, containing 5 μl of LightCycler 480® SYBR Green I Master (Roche), 0.5 μM of both forward primer Sip1 (5’-ATCCTGAGACAACACTGACA-3’) and reverse primer Sip2 (5’-TTGCTGGTGTTTCTATTTTCA-3’), 0.3 μM of probe (5’- 6-FAM–ATCAGAAGAGTCATACTGCCACTTC–TAMRA-3’) (Eurogentec, Liège, Belgium) and 2 μl of DNA extract or 2 μl of HPLC water (as negative template control). Cycling conditions were as follows: 95°C for 5 min; 40 cycles of 95°C for 10 s, 58°C for 15 s and 72°C for 20 s. For the standard series, DNA concentration of the extract of S. agalactiae LMG 14694T was determined using the Qubit® Fluorometer (Invitrogen, Auckland, New Zealand) and the genomic concentration was calculated based on the GC% content and genome size of the type strain. A tenfold dilution standard series of S. agalactiae LMG 14694T DNA was prepared by dilution of the DNA stock in HPLC grade water. All standard tenfold dilution series and samples were run in duplicate. Amplification, detection and quantification were carried out using the LightCycler480® platform and the LightCycler® 480 Software Version 1.5 (Roche).
Escherichia coli qPCR
To detect E. coli in vaginal DNA extracts, an E. coli specific qPCR was carried out, using primers targeting the β-glucuronidase encoding gene uidA, previously described [24]. The qPCR reactions were performed in a final volume of 10 μl, containing 5 μl of LightCycler 480® SYBR Green I Master (Roche), 0.3 μM of both forward primer EcoliFW (5’-CAACGAACTGAACTGGCAGA-3’) and reverse primer EcoliRV (5’- CATTACGCTGCGATGGAT -3’) (Eurogentec) and 2 μl of DNA extract or 2 μl of HPLC water (as negative template control). Cycling conditions were as follows: 50°C for 2 min, 95°C for 10 min; 40 cycles of 95°C for 15 s and 60°C for 1 min. A standard series (using E. coli ATCC 25922 grown on TSA + 5% sheep blood (BD)), was constructed as described for S. agalactiae.
Candida albicans qPCR
To detect C. albicans in vaginal DNA extracts, a C. albicans specific qPCR was carried out, using primers targeting the ITS-1 gene (adapted from [25]). The qPCR reactions were performed in a final volume of 10 μl, containing 5 μl of LightCycler 480® SYBR Green I Master (Roche), 0.3 μM of both forward primer CA_FW (5’-CAACGAACTGAACTGGCAGA-3’) and reverse primer CA_RV (5’- CATTACGCTGCGATGGAT -3’) (Eurogentec) and 2 μl of DNA extract or 2 μl of HPLC water (as negative template control). Cycling conditions were as follows: 50°C for 2 min, 95°C for 10 min; 40 cycles of 95°C for 15 s and 60°C for 1 min. A standard series (using C. albicans ATCC 90028 grown on Sabouraud agar (BD)), was constructed as described for S. agalactiae.
Microbiological culturing
At the local laboratories, the Amies swab was inoculated on in-house TMBplus plates (a medium supporting growth of anaerobes and allowing assessment of hydrogen peroxide production of strains) [26], after which the plates were incubated anaerobically as described previously [27]. After 48–72 h, depending on the growth, all biological material of the culture plate was harvested using sterile cotton swabs and stored in cryovials with 1 ml of tryptic soy broth + 5% glycerol at– 80°C until shipment. After shipment to the ITM, bacteria from the cryovial were inoculated in commercial Lim Broth medium (BD)–a selective enrichment medium for GBS–according to the manufacturer’s instructions (5% CO2 at 35°C for 24 hours). The latter procedure was performed only for women found to be positive for vaginal GBS carriage by means of qPCR. DNA extracts of inoculated Lim Broth medium was used for direct molecular capsular typing of GBS.
S. agalactiae molecular capsular typing
To determine the GBS serotype, we used a flowchart described by [28], based on the multiplex PCRs with primers as described by Poyart and co-workers and Imperi and co-workers [29, 30]. The multiplex PCRs were performed directly on DNA extracted from the inoculated Lim Broth medium. The reactions were performed in a final reaction mixture of 20 μl, containing 10 μl of FastStart PCR Master Mix (Roche), 0.2 μM of each primer, and 2 μl of DNA template. Using a Veriti 96-well thermal cycler (Applied Biosystems, Foster City, CA), the following PCR program was run: 94°C for 5 min, 3 cycles of 45 s at 94°C, 2 min at 50°C, 1 min at 72°C, and 30 cycles of 20 s at 94°C, 1 min at 50°C and 1 min at 72°C, with a final extension at 72°C for 7 min. PCR amplification products were visualised under UV light after electrophoresis on 1% agarose gels (30 minutes at 10 V/cm) and staining with ethidiumbromide. Twenty five control strains (covering all GBS serotypes and provided by the Belgian Streptococcus agalactiae reference center (Dr. Pierette Melin, University of Liège, Belgium)) were used as a positive control.
Physiological parameters
Vaginal pH was measured during the speculum examination by pressing commercial pH strips (pH Fix 3.6–6.1, Machery-Nagel) against the vaginal wall.
Detection of prostate-specific antigen (PSA), a marker for sexual intercourse within the past 24 hours [31] in vaginal swab fluid was performed using a chromatographic immune assay (the Seratec® PSA SemiQuant Cassette Test, Seratec, Gottingen, Germany) according to the manufacturer’s instructions. Pregnancy was assessed by testing urine with a rapid hCG test (QuickVue One-Step hCG Test (Kigali, Johannesburg) or Unimed First Sign hCG test (Mombasa)). Leucocytes and erythrocytes in urine were detected using dipsticks according to the manufacturer’s instructions (Siemens Multistix 10 sg in Kigali, Mission® urinalysis strips in Mombasa, and Neotest 4 Urine Dipstick in Johannesburg).
Statistical analysis
Data were analyzed with SPSS software version 22 (SPSS Inc.). Prevalences were reported with their 95% confidence interval. Outcomes for this analysis were vaginal GBS carriage and vaginal E. coli carriage, as determined by a positive qPCR.
Independent variables considered were study site, sociodemographic characteristics, reproductive health characteristics, sexual behavioural factors, vaginal practices characteristics, cervicovaginal signs and symptoms and microbiological characteristics. Variables were analyzed using logistic regression in univariable and multivariable ways, with p-values < 0.05 indicating significance. In order not to overfit our multivariable models, variables were restricted in proportion to the number of cases positive for GBS and E. coli, i.e. maximum one degree of freedom per 10 cases [32]. Variables included in the models were selected as follows [33]: firstly, only variables found to be significantly associated with GBS or E. coli carriage in univariable analysis were considered for inclusion the multivariate GBS or E. coli model, respectively. Subsequently, of correlated variables (e.g. ‘having had recent vaginal intercourse’ and a positive PSA test), only one was kept for further consideration to avoid collinearity. The final selection of variables was based on literature and clinical expertise/relevance. The multivariable models were controlled for possible confounding variables and were validated with bootstrap analysis.
Ethics statement
Written information and consent forms in the local language were provided to the women or to the Legally Authorized Representatives for their review. After the interview, the participants were asked to express their willingness to participate in the study by signing (or thumb-printing in case they were illiterate) the consent form. In case they were of minor age (age below 18 in Kenya and SA, and below 21 in Rwanda), also the parents or guardians were asked to give consent. The study was approved by the Kenyatta National Hospital Ethical Review Committee, Kenya; the Human Research Ethics Committee (Medical), University of the Witwatersrand, SA; the Rwanda National Ethics Committee, Rwanda; the Institutional Review Boards of the Institute of Tropical Medicine in Antwerp, of Ghent University, and of the University Teaching Hospital in Antwerp, Belgium. In addition, the study was approved by the National Council on Science and Technology in Kenya, and the National AIDS Control Commission in Rwanda. The study is registered at the Trial Registration at the National Health Research Ethics Council South Africa (DOH2709103223) [19].
Results
Vaginal GBS and E. coli carriage and GBS serotype distribution
Of the 430 women enrolled in the study, 424 and 421 vaginal swab DNA extracts were analysed for the presence of GBS and E. coli, respectively. The vaginal GBS and E. coli carriage rates in the different study groups are presented in Table 1.
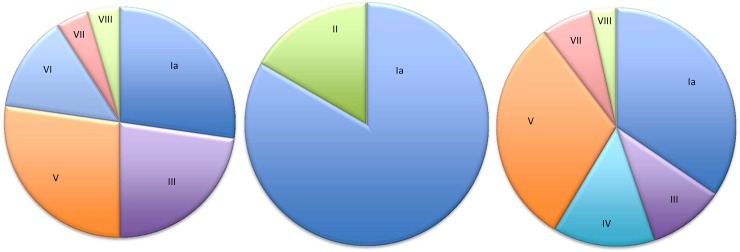
The GBS serotype distribution is presented in Table 2 and Fig 1. For 12 GBS carriers, the serotype could not be determined because samples were no longer available. Serotype distribution was largely comparable between sites. The most prevalent serotypes were Ia (27.3%), V (27.3%), and III (22.7%) in Kenya; Ia (34.5%), V (31.0%), and IV (13.8%) in SA; and Ia (83.3%) and II (16.7%) in Rwanda.
Table 2. Studies reporting GBS serotype distribution of (recto)vaginal isolates in SSA.
| Country | Year | Population | Ia | Ib | II | III | IV | V | VI | VII | VIII | IX | NT | Reference |
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| The Gambia | 1994 | P | 19 | 28 | 6 | 3 | 38 | [34]$ | ||||||
| Malawi | 2011 | P, HIV+, HIV- | 18.2 | 6.2 | 10.3 | 39.0 | 0.3 | 23.9 | 0.8 | 0.8 | 1.5 | [35] | ||
| SA | 2011 | P | 30.1 | 6.7 | 11.3 | 37.3 | 3.7 | 10.2 | [36] | |||||
| SA | 2014 | P | 36.2–41.4 | 3.5–4.6 | 7.2–7.5 | 31.3–34.9 | 2.0–4.0 | 10.3–15.6 | 0.0–3.3 | [37] | ||||
| Kenya | 2015 | P, NP | 27.3 | 22.7 | 27.3 | 13.6 | 4.5 | 4.5 | This study | |||||
| Rwanda | 2015 | NP | 83.3 | 16.7 | This study | |||||||||
| SA | 2015 | P, NP | 34.5 | 10.3 | 13.8 | 31.0 | 6.9 | 3.4 | This study | |||||
| Europe | 2010 | N/A | 18.2 | 12.4 | 14.4 | 28.1 | 3.7 | 14.9 | 0.6 | 0.6 | 0.6 | [38]£ | ||
| US | 2010 | N/A | 26.8 | 8.1 | 10.9 | 24.8 | 1.0 | 15.0 | 0.3 | 0.0 | 0.2 | [38]£ | ||
P, pregnant; NP, non-pregnant
$determined serotypes I-VI (no differentiation between Ia and Ib); N/A, not applicable (review)
£data from meta-analysis but excluding isolates from non-sterile sites and from neonates were excluded.
Fig 1. Distribution of GBS capsular serotypes.
Left, Kenya (n = 22); middle, Rwanda (n = 6); right, South Africa (n = 29).
Univariable and multivariable analyses
Tables 3 and 4 present the univariable associations of the sociodemographics, sexual behavior, vaginal practices, cervicovaginal signs and symptoms, and microbiological characteristics with vaginal GBS and E. coli carriage, respectively. Because of the low prevalence, CT, NG, TV, and syphilis were not considered for further analysis.
Table 3. Sociodemographic characteristics, reproductive health, sexual behavior, vaginal practices, vaginal signs & symptoms, and microbiological associations with vaginal GBS carriage (univariable analysis).
| n | GBS+ n (%) | Crude OR (95% CI) | p-value* | |
|---|---|---|---|---|
| 424 | 69 (16.3) | |||
| Sociodemographic characteristics | ||||
| City (Country) | ||||
| Mombasa (Kenya) | 165 | 27 (16.4) | 0.89 (0.51–1.53) | 0.665 |
| Kigali (Rwanda) | 60 | 6 (10.0) | 0.50 (0.20–1.26) | 0.142 |
| Johannesburg (SA) | 199 | 36 (18.1) | 1 | - |
| Age (years) | ||||
| <18 | 58 | 1 (1.7) | 0.07 (0.01–0.50) | 0.008 |
| 18–24 | 148 | 23 (15.5) | 0.71 (0.41–1.23) | 0.219 |
| >24 | 218 | 45 (20.6) | 1 | - |
| Educational level | ||||
| Higher educational level£ | 189 | 39 (20.6) | 1 | - |
| Lower educational level££ | 235 | 30 (12.8) | 0.56 (0.33–0.95) | 0.030 |
| Marital status | ||||
| Never married | 242 | 34 (14.0) | 1 | - |
| Married | 148 | 30 (20.2) | 1.55 (0.91–2.67) | 0.109 |
| Separated/divorced/widowed | 34 | 5 (14.7) | 1.06 (0.38–2.91) | 0.918 |
| Socio-economic status# | ||||
| Low | 106 | 17 (13.0) | 1 | - |
| Medium | 163 | 31 (19.0) | 1.23 (0.64–2.36) | 0.533 |
| High | 155 | 21 (13.5) | 0.82 (0.41–1.64) | 0.576 |
| Reproductive health | ||||
| Pregnant | ||||
| No | 366 | 62 (16.9) | 1 | - |
| Yes | 58 | 7 (12.1) | 0.67 (0.29–1.55) | 0.353 |
| Parity | ||||
| 0 | 149 | 18 (12.1) | 1 | - |
| 1–2 | 211 | 42 (19.9) | 1.81 (1.00–3.29) | 0.052 |
| >2 | 64 | 9 (14.1) | 1.19 (0.50–2.81) | 0.690 |
| Gravity | ||||
| 0 | 118 | 14 (11.9) | 1 | - |
| 1–2 | 210 | 38 (18.1) | 1.64 (0.85–3.17) | 0.141 |
| >2 | 96 | 17 (17.7) | 1.60 (0.74–3.44) | 0.230 |
| Regular cycle | ||||
| Yes | 256 | 42 (16.4) | 1 | - |
| No/unknown | 168 | 27 (16.1) | 0.98 (0.58–1.66) | 0.927 |
| Menstrual cycle | ||||
| No cycle | 194 | 33 (17.0) | 1 | - |
| With cycle | 230 | 36 (15.7) | 0.91 (0.54–1.51) | 0.706 |
| Contraceptive | ||||
| None | 73 | 15 (20.5) | 1 | - |
| Condom only | 108 | 10 (9.3) | 0.40 (0.17–0.94) | 0.035 |
| Others (hormones/IUD/sterilisation/pregnant) | 243 | 44 (18.1) | 0.86 (0.44–1.65) | 0.639 |
| Currently breastfeeding | ||||
| No | 390 | 64 (16.4) | 1 | - |
| Yes | 34 | 5 (14.7) | 0.88 (0.33–2.36) | 0.796 |
| Sexual behaviour | ||||
| Age at first sexual encounter (years) | ||||
| <16 | 80 | 8 (10.0) | 1 | - |
| 16–18 | 197 | 36 (18.3) | 2.01 (0.89–4.5) | 0.093 |
| 19–21 | 104 | 16 (15.4) | 1.64 (0.66–4.04) | 0.286 |
| >21 | 43 | 9 (20.9) | 2.38 (0.85–6.71) | 0.101 |
| Sexually active (last 3 months) | ||||
| No | 55 | 4 (7.3) | 1 | - |
| Yes | 369 | 65 (17.6) | 2.73 (0.95–7.81) | 0.062 |
| Condom use (at last sexual encounter)@ | ||||
| No | 229 | 47 (20,5) | 1.75 (0.94–3.16) | 0.050 |
| Yes | 140 | 18 (12.9) | 1 | - |
| Lifetime n° of sex partners | ||||
| 1 | 112 | 13 (11.6) | 1 | - |
| 2–3 | 186 | 32 (17.2) | 1.58 (0.79–3.16) | 0,194 |
| > 3 | 126 | 24 (19.0) | 1.79 (0.86–3.71) | 0,117 |
| N° of sex partners in the last 3 months | ||||
| 0 | 25 | 0 (0.0) | 1 | - |
| > = 1 | 399 | 69 (17.3) | N/A | 0.010 |
| Recent vaginal sex% | ||||
| No | 343 | 49 (14.3) | 1 | - |
| Yes | 81 | 20 (24.7) | 2.73 (0.95–7.81) | 0.024 |
| Sexual risk taking€ | ||||
| Low | 167 | 25 (15.0) | 1 | - |
| Medium | 155 | 30 (19.4) | 1.36 (0.76–2.44) | 0.297 |
| High | 102 | 14 (13.7) | 0.90 (0.45–1.83) | 0.779 |
| Estimated frequency of sexual encounters in last 3 months@, & | ||||
| 0 | 55 | 4 (7.3) | 1 | - |
| < 10 times | 137 | 18 (13.1) | 1.93 (0.62–5.98) | 0.255 |
| 11–30 times | 129 | 24 (18.6) | 2.91 (0.96–8.84) | 0.059 |
| > 30 times | 98 | 23 (23.5) | 3.91 (1.27–11.98) | 0.017 |
| HIV status partner@, | ||||
| HIV positive | 38 | 3 (7.9) | 1 | - |
| HIV negative | 250 | 52 (20.8) | 3.06 (0.91–10.36) | 0.072 |
| Unknown | 79 | 10 (12.6) | 1.69 (0.44–6.54) | 0.447 |
| Estimated frequency of unprotected sex in last 3 months | ||||
| No sexual contacts | 55 | 4 (7.3) | 1 | - |
| Never unprotected | 104 | 12 (11.5) | 1.66 (0.51–5.42) | 0.399 |
| < 10 times | 88 | 14 (15.9) | 2.41 (0.75–7.75) | 0.139 |
| > = 10 times | 177 | 39 (22.0) | 3.60 (1.23–10.59) | 0.020 |
| New partner (within 3 months) | ||||
| No | 378 | 60 (15.9) | 1 | - |
| Yes | 46 | 9 (19.6) | 1.29 (0.59–2.81) | 0.523 |
| Circumcision status partner@, | ||||
| Circumcised | 240 | 38 (15.8) | 1 | - |
| No/don’t know Not circumcised/don’t know | 129 | 27 (20.9) | 1.41 (0.81–2.43) | 0.222 |
| Female sex worker | ||||
| Yes | 30 | 6 (20.0) | 1 | - |
| No | 394 | 64 (16.2) | 1.03 (0.38–2.97) | 0.952 |
| Vaginal practices | ||||
| Washing inside the vagina when bathing | ||||
| No | 176 | 15 (8.5) | 1 | - |
| Yes | 248 | 54 (21.8) | 2.99 (1.63–5.49) | <0.001 |
| Drying the vagina before sex | ||||
| Yes | 10 | 4 (40.0) | 1 | - |
| No | 414 | 65 (15.7) | 3.58 (0.98–13.04) | 0.053 |
| Washed inside the vagina recently (morning or evening before study visit) | ||||
| No | 231 | 28 (12.1) | 1 | - |
| Yes | 193 | 41 (21.2) | 1.96 (1.16–3.30) | 0.012 |
| Products to wash/clean/dry/tighten the vagina | ||||
| None | 153 | 13 (8.5) | 1 | - |
| Water/fingers only or water/soap | 211 | 44 (20.9) | 2.84 (1.47–5.48) | 0.002 |
| Cloth | 48 | 9 (18.8) | 2.49 (0.99–6.24) | 0.053 |
| Lemon juice/detergents | 12 | 3 (25.0) | 3.59 (0.86–14.92) | 0.079 |
| Cleaning the vagina after sexual intercourse | ||||
| No | 227 | 28 (12.3) | 1 | - |
| Yes | 197 | 41 (20.8) | 1.87 (1.11–3.16) | 0.019 |
| Cervicovaginal signs and symptoms | ||||
| Ectopy¶ | ||||
| No | 226 | 34 (15.0) | 1 | - |
| Yes | 197 | 34 (17.3) | 1.18 (0.70–1.98) | 0.536 |
| Degree of ectopy¶ | ||||
| Absent | 226 | 34 (15.0) | 1 | - |
| Small | 53 | 8 (15.1) | 1.00 (0.44–2.32) | 0.993 |
| Moderate | 139 | 24 (17.3) | 1.18 (0.67–2.09) | 0.573 |
| Large | 5 | 2 (40.0) | 3.77 (0.61–23.4) | 0.155 |
| Colposcopic findings§,¶ | ||||
| No | 380 | 59 (15.5) | 1 | - |
| Yes | 43 | 10 (23.3) | 1.65 (0.77–3.53) | 0.197 |
| Cervical mucus | ||||
| No | 270 | 39 (14.4) | 1 | - |
| Mild to moderate | 140 | 28 (20.0) | 1.48 (0.87–2.53) | 0.151 |
| Abundant | 14 | 2 (14.3) | 0.99 (0.21–4.58) | 0.987 |
| Reported abnormal discharge | ||||
| No | 399 | 64 (16.0%) | 1 | - |
| Yes | 25 | 5 (20%) | 1.31 (0.47–3.61) | 0.604 |
| Vaginal discharge on speculum | ||||
| No | 332 | 52 (15.7) | 1 | - |
| Yes | 92 | 17 (18.5) | 0.82 (0.45–1.50) | 0.518 |
| Vaginal epithelial abnormalities | ||||
| No | 419 | 67 (16.0) | 1 | - |
| Yes | 5 | 2 (40.0) | 3.50 (0.57–21.36) | 0.174 |
| Cervical epithelial abnormalities | ||||
| No | 379 | 64 (16.9) | 1 | - |
| Yes | 45 | 5 (11.1) | 0.62 (0.23–1.62) | 0.325 |
| Red blood cells in urine | ||||
| No | 358 | 58 (16.2) | 1 | - |
| Yes | 66 | 11 (16.7) | 1.03 (0.51–2.10) | 0.925 |
| White blood cells in urine | ||||
| No | 328 | 56 (17.1) | 1 | - |
| Yes | 96 | 13 (13.5) | 0.76 (0.40–1.46) | 0.411 |
| Microbiological factors | ||||
| BV visit 1 (Amsel criteria) | ||||
| No BV | 346 | 61 (17.6) | 1 | - |
| BV | 78 | 8 (10.3) | 0.53 (0.24–1.17) | 0.116 |
| BV (Nugent) ¶ | ||||
| No BV (Nugent 0–3) | 217 | 37 (17.1) | 1 | - |
| Intermediate (Nugent 4–6) | 29 | 6 (20.7) | 1.30 (0.60–2.83) | 0.507 |
| BV (Nugent 7–10) | 137 | 13 (9.5) | 0.29 (0.12–0.70) | 0.006 |
| Reproductive tract infection (RTI) | ||||
| No RTI | 352 | 60 (17.0) | 1 | - |
| 1 or more RTI | 60 | 8 (13.3) | 0.75 (0.34–1.66) | 0.475 |
| >1 RTI | 12 | 1 (8.3) | 0.44 (0.06–3.50) | 0.439 |
| Syphilis | ||||
| No | 415 | 69 (16.6) | 1 | - |
| Yes | 9 | 0 (0.0) | N/A | 0.001 |
| Chlamydia trachomatis | ||||
| No | 382 | 62 | 1 | - |
| Yes | 42 | 7 | 1.03 (0.44–2.43) | 0.942 |
| Neisseria gonorrhoeae | ||||
| No | 415 | 69 (16.6) | 1 | - |
| Yes | 9 | 0 (0.0) | N/A | 0.001 |
| Trichomonas vaginalis | ||||
| No | 390 | 66 (16.9) | 1 | - |
| Yes | 26 | 3 (11.5) | 0.64 (0.19–2.20) | 0.478 |
| Candida albicans (qPCR) | ||||
| No | 375 | 50 (13.3) | 1 | - |
| Yes | 46 | 17 (37.0) | 3.81 (1.95–7.44) | <0.001 |
| Escherichia coli (qPCR) | ||||
| No | 354 | 89 (25.1) | 1 | - |
| Yes | 67 | 29 (43.3) | 2.27 (1.33–3.90) | 0.003 |
| HSV-2 serology | ||||
| No | 276 | 42 (15.2%) | 1 | - |
| Yes | 147 | 27 (18.4%) | 1.25 (0.74–2.13) | 0.404 |
| Vaginal pH | ||||
| < 4.4 | 126 | 15 (11.9) | 1 | - |
| 4.4–5.3 | 240 | 42 (17.5) | 1.57 (0.83–2.96) | 0.163 |
| 5.4 and more | 58 | 12 (20.7) | 1.93 (0.84–4.44) | 0.122 |
| PSA present | ||||
| No | 233 | 31 (13.3) | 1 | - |
| Yes | 181 | 38 (21.0) | 1.73 (1.03–2.91) | 0.039 |
| Systemic antibiotics visit 1 | ||||
| No | 341 | 62 (18.1) | 1 | - |
| Yes | 83 | 7 (8.4) | 0.41 (0.18–0.94) | 0.036 |
| Systemic antibiotics screening visit | ||||
| No | 391 | 68 (17.4) | 1 | - |
| Yes | 33 | 1 (3.0) | 0.15 (0.02–1.11) | 0.063 |
*bold: significant at the 5% level
£completed secondary school, or post-secondary school
££Primary school (completed or not), secondary school but not completed
#Socio-economic-status was constructed from total income, type of housing, type of toilet
@with partners within three months prior to enrolment
&missing data for 5
%sex morning or evening before visit &
€low risk: 1 or no partners in last year and did not have any partner (in the last 3 months) with multiple partners and age first sex at least 15 years; medium risk: 2 partners last year or had at least one sexual partner (in the last 3 months) who had multiple partners; high risk: sex worker or at least 3 partners last year or at had at least one sexual partner with HIV in the last 3 months or age first sex less than 15 years; N/A, no odds ratio due to no cases in one category
¶data missing for 1 (ectopy, colposcopic findings, HSV-2 serology), 3 (C. albicans, E. coli), 8 (T. vaginalis), 41 (BV Nugent, unreadable slides)
§petechiae (6 GBS cases/20), abrasion (2 GBS cases/5), erythema (1 GBS case/10), laceration (1 GBS case/4); BV, bacterial vaginosis; IUD, intrauterine device.
Table 4. Sociodemographic characteristics, reproductive health, sexual behavior, vaginal practices, vaginal signs & symptoms, and microbiological associations with vaginal E. coli carriage (univariable analysis).
| n | E. coli + n (%) | Crude OR (95% CI) | p-value* | |
|---|---|---|---|---|
| 421 | 118 (28.0) | |||
| Sociodemographic characteristics | ||||
| City (Country) | ||||
| Mombasa (Kenya) | 164 | 39 (23.6) | 0.87 (0.54–1.41) | 0.569 |
| Kigali (Rwanda) | 60 | 27 (45.0) | 2.28 (1.25–4.15) | 0.007 |
| Johannesburg (SA) | 197 | 52 (26.5) | 1 | - |
| Age (years) | ||||
| <18 | 58 | 12 (20.7) | 0.73 (0.36–1.47) | 0.376 |
| 18–24 | 147 | 49 (33.3) | 1.40 (0.88–2.20) | 0.154 |
| >24 | 216 | 57 (26.4) | 1 | - |
| Educational level | ||||
| Higher educational level£ | 187 | 56 (29.9) | 1 | - |
| Lower educational level££ | 234 | 62 (26.5) | 0.84 (0.55–1.29) | 0.434 |
| Marital status | ||||
| Never married | 240 | 71 (29.6) | 1 | - |
| Married | 147 | 37 (25.2) | 0.80 (0.50–1.27) | 0.348 |
| Separated/divorced/widowed | 34 | 10 (29.4) | 0.99 (0.45–2.18) | 0.984 |
| Socio-economic status# | ||||
| Low | 106 | 27 (25.5) | 1 | - |
| Medium | 163 | 46 (28.2) | 1.15 (0.66–2.00) | 0.620 |
| High | 152 | 45 (29.6) | 1.23 (0.70–2.15) | 0.467 |
| Reproductive health | ||||
| Pregnant | ||||
| No | 363 | 104 (28.7) | 1 | - |
| Yes | 58 | 14 (24.1) | 0.79 (0.42–1.51) | 0.478 |
| Parity | ||||
| 0 | 149 | 35 (23.5) | 1 | - |
| 1–2 | 209 | 62 (29.7) | 1.37 (0.85–2.22) | 0.196 |
| >2 | 63 | 21 (33.3) | 1.63 (0.85–3.11) | 0.139 |
| Gravity | ||||
| 0 | 118 | 25 (21.2) | 1 | - |
| 1–2 | 208 | 63 (30.3) | 1.62 (0.95–2.75) | 0.077 |
| >2 | 95 | 30 (31.6) | 1.72 (0.93–3.19) | 0.087 |
| Regular cycle | ||||
| Yes | 254 | 65 (25.6) | 1 | - |
| No/unknown | 167 | 54 (33.3) | 1.42 (0.92–2.18) | 0.111 |
| Menstrual cycle | ||||
| No cycle | 194 | 58 (29.9) | 1 | - |
| With cycle | 227 | 60 (26.4) | 0.84 (0.55–1.29) | 0.430 |
| Contraceptive | ||||
| None | 72 | 20 (27.8) | 1 | - |
| Condom only | 106 | 28 (26.4) | 0.93 (0.48–1.83) | 0.841 |
| Others (hormones/IUD/sterilisation/pregnant) | 243 | 70 (28.8) | 1.05 (0.59–1.89) | 0.865 |
| Currently breastfeeding | ||||
| No | 387 | 106 (27.4) | 1 | - |
| Yes | 34 | 12 (35.3) | 1.45 (0.69–3.03) | 0.327 |
| Sexual behaviour | ||||
| Age at first sexual encounter (years) | ||||
| <16 | 79 | 29 (36.7) | 1 | - |
| 16–18 | 197 | 52 (26.4) | 0.62 (0.35–1.08) | 0.090 |
| 19–21 | 103 | 26 (25.2) | 0.58 (0.31–1.10) | 0.096 |
| >21 | 42 | 11 (26.2) | 0.61 (0.27–1.40) | 0.224 |
| Sexually active (last 3 months) | ||||
| No | 55 | 16 (29.1) | 1 | - |
| Yes | 366 | 102 (27.9) | 0.94 (0.50–1.76) | 0.851 |
| Condom use (at last sexual encounter) | ||||
| No | 283 | 68 (24.0) | 1.80 (1.16–2.79) | 0.009 |
| Yes | 138 | 50 (36.2) | 1 | - |
| Lifetime n° of sex partners | ||||
| 1 | 110 | 28 (25.5) | 1 | - |
| 2–3 | 185 | 42 (22.7) | 0.86 (0.50–1.49) | 0.591 |
| > 3 | 126 | 48 (38.1) | 1.80 (1.03–3.15) | 0.039 |
| N° of sex partners in the last 3 months | ||||
| 0 | 25 | 6 (24.0) | 1 | - |
| > = 1 | 396 | 112 (28.3) | 1.25 (0.49–3.21) | 0.644 |
| Recent vaginal sex% | ||||
| No | 340 | 91 (26.8) | 1 | - |
| Yes | 81 | 27 (33.3) | 1.37 (0.81–2.30) | 0.238 |
| Sexual risk taking€ | ||||
| Low | 167 | 44 (26.3) | 1 | - |
| Medium | 152 | 37 (22.4) | 0.90 (0.54–1.49) | 0.681 |
| High | 102 | 37 (36.3) | 1.59 (0.94–2.71) | 0.086 |
| Estimated frequency of sexual encounters in last 3 months@, & | ||||
| 0 | 55 | 16 (29.1) | 1 | - |
| < 10 times | 135 | 31 (23.0) | 0.73 (0.36–1.47) | 0.376 |
| 11–30 times | 128 | 43 (33.6) | 1.23 (0.62–2.45) | 0.550 |
| > 30 times | 98 | 27 (27.6) | 0.93 (0.45–1.93) | 0.839 |
| HIV status partner@ | ||||
| HIV positive | 38 | 11 (28.9) | 1 | - |
| HIV negative | 247 | 63 (25.5) | 0.84 (0.39–1.79) | 0.653 |
| Unknown | 79 | 28 (35.4) | 1.35 (0.58–3.12) | 0.486 |
| Estimated frequency of unprotected sex in last 3 months | ||||
| No sexual contacts | 55 | 16 (29.1) | 1 | - |
| Never unprotected | 102 | 34 (33.3) | 1.22 (0.60–2.49) | 0.586 |
| < 10 times | 87 | 19 (21.8) | 0.68 (0.31–1.48) | 0.330 |
| > = 10 times | 177 | 49 (27.7) | 0.93 (0.48–1.82) | 0.839 |
| New partner (within 3 months) | ||||
| No | 375 | 96 (25.6) | 1 | - |
| Yes | 46 | 22 (47.8) | 2,66 (1.43–4.97) | 0.002 |
| Circumcision status partner@ | ||||
| Circumcised | 238 | 62 (26.1) | 1 | - |
| Not circumcised/don’t know | 128 | 40 (31.3) | 1.29 (0.80–2.07) | 0.291 |
| Female sex worker | ||||
| No | 391 | 97 (24.8) | 1 | - |
| Yes | 30 | 21 (70.0) | 7.07 (3.13–15.96) | <0.001 |
| Vaginal practices | ||||
| Washing inside the vagina when bathing | ||||
| No | 175 | 44 (25.1) | 1 | - |
| Yes | 246 | 74 (30.1) | 1.28 (0.83–1.98) | 0.267 |
| Drying the vagina before sex | ||||
| No | 411 | 114 (27.3) | 1 | - |
| Yes | 10 | 4 (40.0) | 1.74 (0.48–6.27) | 0.399 |
| Washed inside the vagina recently (morning or evening before study visit) | ||||
| No | 229 | 64 (27.9) | 1 | - |
| Yes | 192 | 54 (28.1) | 1.01 (0.66–1.55) | 0.968 |
| Products to wash/clean/dry/tighten the vagina | ||||
| None | 153 | 40 (26.1) | 1 | - |
| Water/fingers only or water/soap | 210 | 59 (28.1) | 1.10 (0.69–1.77) | 0.680 |
| Cloth | 46 | 16 (34.8) | 1.51 (0.74–3.05) | 0.255 |
| Lemon juice/detergents | 12 | 3 (25.0) | 0.94 (0.24–3.65) | 0.931 |
| Cleaning the vagina after sexual intercourse | ||||
| No | 226 | 61 (27.0) | 1 | - |
| Yes | 195 | 57 (29.2) | 1.12 (0.73–1.71) | 0.610 |
| Cervicovaginal signs and symptoms | ||||
| Ectopy¶ | ||||
| No | 224 | 49 (21.9) | 1 | - |
| Yes | 196 | 69 (35.2) | 1.94 (1.26–2.99) | 0.003 |
| Degree of ectopy¶ | ||||
| Absent | 224 | 49 (21.9) | 1 | - |
| Small | 52 | 22 (42.3) | 2.62 (1.39–4.94) | 0.003 |
| Moderate | 139 | 46 (33.1) | 1.77 (1.10–2.84) | 0.019 |
| Large | 5 | 1 (20.0) | 0.89 (0.10–8.17) | 0.920 |
| Colposcopic findings§, ¶ | ||||
| No | 377 | 102 (27.1) | 1 | - |
| Yes | 43 | 16 (37.2) | 1.60 (0.83–3.09) | 0.163 |
| Cervical mucus | ||||
| No | 269 | 67 (24.9) | 1 | - |
| Mild to moderate | 138 | 47 (34.1) | 1.56 (1.00–2.44) | 0.052 |
| Abundant | 14 | 4 (28.6) | 1.21 (0.37–3.97) | 0.758 |
| Reported abnormal discharge | ||||
| No | 396 | 112 (28.3) | 1 | - |
| Yes | 25 | 6 (24.0) | 0.80 (0.31–2.06) | 0.644 |
| Vaginal discharge on speculum | ||||
| No | 331 | 85 (25.7) | 1 | - |
| Yes | 90 | 33 (36.7) | 1.68 (1.02–2.75) | 0.041 |
| Vaginal epithelial abnormalities | ||||
| No | 416 | 116 (27.9) | 1 | - |
| Yes | 5 | 2 (40.0) | 1.72 (0.28–10.45) | 0.554 |
| Cervical epithelial abnormalities | ||||
| No | 377 | 105 (27.9) | 1 | - |
| Yes | 44 | 13 (29.5) | 1.09 (0.55–2.16) | 0.813 |
| Red blood cells in urine | ||||
| No | 355 | 101 (28.5) | 1 | - |
| Yes | 66 | 17 (25.8) | 0.87 (0.48–1.59) | 0.655 |
| White blood cells in urine | ||||
| No | 325 | 81 (24.9) | 1 | - |
| Yes | 96 | 37 (38.5) | 1.89 (1.17–3.06) | 0.010 |
| Microbiological factors | ||||
| BV visit 1 (Amsel criteria) | ||||
| No BV | 344 | 99 (28.8) | 1 | - |
| BV | 77 | 19 (24.7) | 0.81 (0.46–1.43) | 0.469 |
| BV visit 1 (Nugent) ¶ | ||||
| No BV (Nugent 0–3) | 217 | 60 (27.6) | 1 | - |
| Intermediate (Nugent 4–6) | 29 | 15 (51.7) | 2.80 (1.28–6.16) | 0.010 |
| BV (Nugent 7–10) | 137 | 33 (24.1) | 0.83 (0.51–1.36) | 0.459 |
| GBS | ||||
| No | 354 | 89 (25.1) | 1 | - |
| Yes | 67 | 29 (43.3) | 2.27 (1.33–3.90) | 0.003 |
| Reproductive tract infection (RTI) | ||||
| No RTI | 349 | 96 (27.5) | 1 | - |
| 1 or more RTI | 60 | 19 (31.7) | 1.22 (0.68–2.21) | 0.508 |
| >1 RTI | 12 | 3 (25.0) | 0.88 (0.23–3.31) | 0.848 |
| Syphilis | ||||
| No | 412 | 117 (28.4) | 1 | - |
| Yes | 9 | 1 (11.1) | 0.32 (0.04–2.55) | 0.279 |
| Chlamydia trachomatis | ||||
| No | 379 | 107 (28.2) | 1 | - |
| Yes | 42 | 11 (26.2) | 0.90 (0.44–1.86) | 0.780 |
| Neisseria gonorrhoeae | ||||
| No | 412 | 114 (27.7) | 1 | - |
| Yes | 9 | 4 (44.4) | 2.09 (0.55–7.93) | 0.278 |
| Trichomonas vaginalis¶ | ||||
| No | 387 | 105 (27.1) | 1 | - |
| Yes | 26 | 11 (42.3) | 1.97 (0.88–4.43) | 0.101 |
| Candida albicans (qPCR) | ||||
| No | 375 | 102 (27.2) | 1 | - |
| Yes | 46 | 16 (34.8) | 1.43 (0.75–2.73) | 0.282 |
| HSV-2 serology¶ | ||||
| No | 274 | 80 (29.2) | 1 | - |
| Yes | 146 | 38 (26.0) | 0.85 (0.54–1.34) | 0.492 |
| Vaginal pH | ||||
| < 4.4 | 125 | 34 (27.2) | 1 | - |
| 4.4–5.3 | 237 | 65 (27.4) | 1.01 (0.62–1.65) | 0.963 |
| 5.4 and more | 58 | 19 (32.8) | 1.30 (0.66–2.56) | 0.441 |
| PSA present | ||||
| No | 231 | 69 (29.9) | 1 | - |
| Yes | 180 | 48 (26.7) | 0.85 (0.55–1.32) | 0.475 |
| Systemic antibiotics visit 1 | ||||
| No | 338 | 98 (29.0) | 1 | - |
| Yes | 83 | 20 (24.0) | 0.78 (0.45–2.36) | 0.374 |
| Systemic antibiotics screening visit | ||||
| No | 388 | 111 (28.6) | 1 | - |
| Yes | 33 | 7 (21.2) | 0.67 (0.28–1.59) | 0.366 |
*Bold: significant at the 5% level
£completed secondary school, or post-secondary school
££Primary school (completed or not), secondary school but not completed
#Socio-economic-status was constructed from total income, type of housing, type of toilet
@with partners within three months prior to enrolment
&missing data for 5
%sex morning or evening before visit
€low risk: 1 or no partners in last year and did not have any partner (in the last 3 months) with multiple partners and age first sex at least 15 years; medium risk: 2 partners last year or had at least one sexual partner (in the last 3 months) who had multiple partners; high risk: sex worker or at least 3 partners last year or at had at least one sexual partner with HIV in the last 3 months or age first sex less than 15 years; N/A, no odds ratio due to no cases in one category
¶data missing for 1 (ectopy, colposcopic findings, HSV-2 serology), 8 (T. vaginalis), 38 (BV Nugent, unreadable slides)
§petechiae (6 E. coli cases/20), abrasion (2 E. coli cases/5), erythema (3 E. coli cases/10), laceration (2 E. coli cases/4), ulcer (2 E. coli cases/6), ecchymosis (2 E. coli cases/6); BV, bacterial vaginosis.
In our final multivariable GBS model (Table 5), BV by Nugent score remained significantly negatively associated with GBS carriage (AOR, 0.43; 95% CI, 0.21–0.88; p = 0.022), and a positive association was observed for vaginal Candida albicans carriage (AOR, 3.25; 95% CI, 1.50–7.06; p = 0.003), vaginal E. coli carriage (AOR, 2.01; 95% CI, 1.10–3.80; p = 0.023), recent vaginal intercourse (AOR, 2.63; 95% CI, 1.35–5.15; p = 0.005), and currently washing the vagina (AOR, 2.26; 95% CI, 1.16–4.37; p = 0.016).
Table 5. Multivariable associations with vaginal GBS carriage.
| n | GBS+ (%) | adjusted OR (95% CI) | p-value$ | |
|---|---|---|---|---|
| 424 | 69 (16.3) | |||
| Recent vaginal sex% | ||||
| No | 343 | 49 (14.3) | 1 | - |
| Yes | 81 | 20 (24.7) | 2.63 (1.35–5.15) | 0.005 |
| Washing inside the vagina# | ||||
| No | 176 | 15 (8.5) | 1 | - |
| Yes | 248 | 54 (21.8) | 2.26 (1.16–4.37) | 0.016 |
| BV (Nugent)¶ | ||||
| No BV (Nugent 0–3) | 217 | 37 (17.1) | 1 | - |
| Intermediate (Nugent 4–6) | 29 | 6 (20.7) | 0.93 (0.33–2.64) | 0.898 |
| BV (Nugent 7–10) | 137 | 13 (9.5) | 0.43 (0.21–0.88) | 0.022 |
| Candida albicans (qPCR)¶ | ||||
| No | 375 | 50 (13.3) | 1 | - |
| Yes | 46 | 17 (37.0) | 3.25 (1.50–7.06) | 0.003 |
| Escherichia coli ¶ | ||||
| No | 303 | 38 (12.5) | 1 | - |
| Yes | 118 | 29 (24.6) | 2.01 (1.10–3.80) | 0.023 |
$bold, significant at the 5% level
#when having shower or bath
%morning or evening before study visit
¶data missing for 3 (C. albicans, E. coli), 41 (BV, unreadable slides).
In our multivariable E. coli model, an intermediate Nugent score remained significantly negatively associated with vaginal E. coli carriage (AOR, 2.61; 95% CI, 1.15–5.94; p = 0.023), and a positive association was observed with working as a FSW (AOR, 7.83; 95% CI, 2.88–21.30; p<0.001), vaginal GBS carriage (AOR, 2.05; 95% CI, 1.09–3.83; p = 0.025), and cervical ectopy (AOR, 1.64; 95% CI, 1.01–2.68; p = 0.046) (Table 6).
Table 6. Multivariable associations with vaginal E. coli carriage.
| n | E. coli + (%) | adjusted OR (95% CI) | p-value$ | |
|---|---|---|---|---|
| 421 | 118 (25.2) | |||
| Condom use (at last sexual encounter) | ||||
| No | 283 | 68 (24.0) | 1.53 (0.92–2.56) | 0.104 |
| Yes | 138 | 50 (36.2) | 1.0 | - |
| Female sex worker | ||||
| No | 391 | 97 (24.8) | 1 | - |
| Yes | 30 | 21 (70.0) | 7.83 (2.88–21.30) | <0.001 |
| Ectopy ¶ | ||||
| No | 224 | 49 (21.9) | 1 | - |
| Yes | 196 | 69 (35.2) | 1.64 (1.01–2.68) | 0.046 |
| Vaginal discharge on speculum | ||||
| No | 331 | 85 (25.7) | 1 | - |
| Yes | 90 | 33 (36.7) | 1.63 (0.92–2.88) | 0.095 |
| BV (Nugent)¶ | ||||
| No BV (Nugent 0–3) | 217 | 60 (27.6) | 1 | - |
| Intermediate (Nugent 4–6) | 29 | 15 (51.7) | 2.61 (1.15–5.94) | 0.023 |
| BV (Nugent 7–10) | 137 | 33 (24.1) | 0.66 (0.38–1.15) | 0.140 |
| GBS | ||||
| No | 354 | 89 (25.1) | 1 | - |
| Yes | 67 | 29 (43.3) | 2.05 (1.09–3.83) | 0.025 |
$bold, significant at the 5% level
¶data missing for 1 (ectopy), 38 (BV, unreadable slides).
Discussion
Group B streptococci (GBS) and E. coli account for the majority of EOS cases worldwide.
Vaginal carriage of GBS and E. coli is considered a prerequisite for GBS or E. coli transmission to the neonate in GBS EOS and E. coli EOS, respectively. However, epidemiological data of vaginal GBS and E. coli carriage, which are essential for the development and implementation of prevention strategies, are very limited in sub-Saharan Africa (SSA) [16, 17].
In this study, we aimed to present vaginal GBS and E. coli carriage rates, GBS serotype distribution and define risk factors for carriage in populations from three SSA countries.
Vaginal GBS and E. coli carriage rates
We found a vaginal GBS carriage rate of 20.2% and 23.2% in the Kenyan and South African reference groups (adult, non-pregant, HIV-negative women at average risk of HIV), respectively. Compared to these reference groups, adolescents in our study were found to have lower GBS carriage rates: 3.6% of the Kenyan and 0% of the SA adolescents carried GBS vaginally. Other studies report conflicting associations between age and vaginal GBS carriage [39–47]. All of these studies (except for [44]) report on pregnant women. Interestingly, when we compare different age groups (< 18 years, 18–24 years, > 24 years) in our Kenyan and SA population, we see no age-group dependent GBS colonization in the pregnant women. However, we do see a statistically significant age-group dependent GBS association in the non-pregnant women, with the lowest and the highest GBS carrier rates in the youngest and the oldest age groups, respectively (Pearson Chi-Square test, data not shown).
The pregnant women in our study population had vaginal GBS carriage rates of 14.3% and 10.0% in Kenya and SA, respectively. This is lower then most other studies reporting (recto)vaginal GBS carriage rates in SSA (see Table 7). Although the CDC recommends rectovaginal sampling for detection of GBS in pregnant women, we only swabbed vaginally, to be able to study the interaction of GBS with the vaginal immune system and vaginal microbiome (to be published). This vaginal sampling may (partly) explain the lower GBS carriage rates found by us, as rectovaginal sampling has been shown to yield higher GBS recovery rates compared to vaginal sampling alone [48, 49]. Furthermore, in contrast to other studies (listed in Table 7) using culturing techniques, we used qPCR without prior enrichment step to detect GBS. Although the CDC allows PCR for the detection of GBS (albeit recommending an enrichment step), this difference with other studies probably does not account (or to a lesser extent) for the lower rates found by us, as PCR (even without an enrichment step) has been shown to be more sensitive than culture [14, 50–53]. A further difference with other studies regards the fact that the pregnant women in our study were up to 14 weeks of gestation, while the other studies listed in Table 7 sampled pregnant women at 35–37 weeks of gestation, which also may account for differences, as some authors have reported on varying GBS rates during pregnancy [45].
Table 7. Studies reporting (recto)vaginal GBS carriage rates in SSA.
| Country | Year | n | Population | % GBS | Sample | Detection | Reference |
|---|---|---|---|---|---|---|---|
| Nigeria | 1980 | 588 | P, L | 19 | V | SB+C | [55] |
| Nigeria | 1983 | 225 | P | 20 | V | SB+C | [56] |
| Zimbabwe | 1990 | 89 | P | 31 | V | SB+C | [57] |
| Togo | 1991 | 106 | P | 4 | V, R | SB+C | [58] |
| Gambia | 1994 | 136 | P | 22 | V, R | SB+C | [34] |
| Malawi | 2005 | 97 | P | 16.5 | V, R | SA | [59] |
| Mozambique | 2008 | 113 | P | 1.8 | V, R | SB+C | [60] |
| Tanzania | 2009 | 300 | P | 23.0 | V, R | SB+C | [54] |
| Zimbabwe | 2010 | 780 | P | 47, 24, 21# | V, R | SB+C | [61] |
| Malawi | 2011 | 1840 | P, HIV+ and HIV- | 21.2 | V, R | SB+C | [35] |
| South Africa | 2014 | 661, 621, 595, 521$ | P | 33.0, 32.7, 28.7, 28.4$ | V, R | SA | [37] |
| DR Congo | 2015 | 509 | P | 20.2 | V | SA | [62] |
L, women in labor; NP, non-pregnant women; P, pregnant women; V, vaginal swab; R, rectal swab; SB+C, selective broth and culturing; SA, selective agar
#week 20, 26, and delivery, respectively
$week 20–25, week 26–30, week 31–35, and week 37+, respectively.
In the group of HIV positive women, we did not observe any GBS carriers, which is probably explained by the fact that most of the HIV positive women (26/30) received prophylactic cotrimoxazole, which is largely effective against GBS [54].
Our reference groups from Kenya and SA had vaginal E. coli carriage rates of 25.0% and 27.1%, respectively. Compared to other studies from SSA reporting vaginal carriage of E. coli, these prevalences are higher than the ones reported by Karou and coworkers (2012) and Ekwempu and coworkers (1981), lower than the ones reported by Schellenberg and coworkers (2011) and Cutland and coworkers (2012), and comparable with the prevalence reported by Sagna and coworkers (2010) (See Table 8)[63–67]. Vaginal E. coli carriage rates in Asia, Europe, North and South America appear lower. Different study populations, sampling and detection techniques might account for these differences.
Table 8. Studies reporting (recto)vaginal E. coli carriage rates.
| Country | Year | n | Population | % E. coli | Sample | Detection | Reference |
|---|---|---|---|---|---|---|---|
| Africa (pooled prevalence 36.0% (2846/7912); range 9.1–46.5%) | |||||||
| Burkina Faso | 2010 | 156 | HIV+ | 28.4 | V | C | [67] |
| Burkina Faso | 2012 | 2000 | S | 16.7 | V | C | [63] |
| Kenya | 2011 | 44 | HIV+, HIV-, HESN | 40.1 | V | cpn60 | [65] |
| Nigeria | 1981 | 187 | L | 9.1 | C | C | [64] |
| SA | 2012 | 1347 | P, HIV+ | 42.3 | V | C | [66] |
| SA | 2012 | 3752 | P, HIV- | 46.5 | V | C | [66] |
| Asia (pooled prevalence 5.3% (163/3072); range 0–25.8%) | |||||||
| Iraq | 2011 | 90 | S, NP | 16.2 | V | C | [68] |
| Iraq | 2011 | 20 | S, P | 25.8 | V | C | [68] |
| Iran | 2014 | 85 | S, P | 18.0 | V | C | [69] |
| Japan | 2002 | 2575 | NP, P | 3.4 | V | C | [70] |
| Pakistan | 2012 | 100 | HC | 28 | V | C | [71] |
| Pakistan | 2012 | 100 | H | 6 | V | C | [71] |
| Turkey | 2007 | 34 | IUD | 14.7 | V | C | [72] |
| Turkey | 2007 | 34 | HC | 2.9 | V | C | [72] |
| Turkey | 2007 | 34 | H | 0.0 | V | C | [72] |
| Europe (pooled prevalence 13.4% (670/4980); range 3.1–51.2%) | |||||||
| Croatia | 2011 | 114 | IUD | 25.5 | V | C | [73] |
| Croatia | 2011 | 122 | H | 8.2 | V | C | [73] |
| Denmark | 2014 | 668 | P | 11.7 | V | C | [74] |
| Germany | 2007 | 166 | H | 16.3, 51.2, 25.9* | V | C | [75] |
| Greece | 2008 | 1632 | S | 3.1 | V | C | [76] |
| Lithuania | 2012 | 970 | P | 19.9 | V, R | C | [77] |
| Spain | 2002 | 623 | P | 27.0 | V | C | [78] |
| Spain | 2011 | 321 | P | 15 | E, V | C | [79] |
| Spain | 2011 | 327 | NP | 12 | E, V | C | [79] |
| Sweden | 2008 | 37 | H | 5.4 | V | C | [80] |
| North America (pooled prevalence 12.7% (430/3373); range 0–29.5%) | |||||||
| Canada | 1983 | 495 | H | 12.3 | V | C | [81] |
| US | 1997 | 2646 | P | 13.0 | V | C | [6] |
| US | 2001 | 44 | H | 18.2, 9.1, 29.5, 6.8, 6.8 # | V | C | [82] |
| US | 2005 | 20 | H | 0 | V | 16S | [83] |
| US | 2012 | 70 | P | 10 | V | C | [84] |
| US | 2012 | 35 | NP | 23 | V | C | [84] |
| US | 2013 | 47 | P | 2.1, 2.2, 5.6, 8.3£ | V | C | [85] |
| US | 2013 | 16 | NP | 6.3, 0, 12.5, 20 | V | C | [85] |
| South America (pooled prevalence 19.7% (135/684); range 14.3–23.0%) | |||||||
| Argentina | 2013 | 259 | P | 14.3 | V | C | [86] |
| Chile | 2009 | 425 | S | 23.0 | V | C | [87] |
The electronic bibliographic database PubMed was searched for articles using the search terms ‘(Escherichia) AND (coli) AND (vaginal)’ with no date or language restriction. Studies were included if the number of vaginal E. coli carriers and the total number of individuals tested were reported; studies were excluded if women were not of childbearing age. 16S, deep sequencing of the 16S rRNA gene; cpn60, deep sequencing of the cpn60 gene; C, conventional culturing and identification; E, endocervial swab; FSW, female sex workers; H, healthy women; HC, women using hormonal contraception; HESN, HIV exposed seronegative women; IUD, women using an intrauterine device as contraception; L, women in labor; NP, non-pregnant women; P, pregnant women; Q, qPCR; R, rectal swab; S, women with vaginal symptoms or clinical diagnosis of infection; V, vaginal swab
*pre, mid, post cycle, respectively
# visit 1at 1 month before visit 2 and 19–24 days after cycle, 1–2 days before intercourse, 8-12h after intercourse, 3–4 days after intercourse, 5–6 days after intercourse
£ <14weeks, between 14–28 weeks, >28weeks, postpartum.
Compared to the reference group in Kenya, pregnant women had a lower prevalence of vaginal E. coli carriage; compared to the reference group in SA, adolescent women had a lower prevalence of E. coli carriage. The FSW study group in Kigali had a very high prevalence of E. coli carriage, i.e. 70%, and will be discussed below (risk factors).
To our knowledge, this is the first study to determine simultaneously the vaginal GBS and E. coli carriage rates in SSA populations using qPCR, known to be more sensitive than culture-based techniques. Moreover, vaginal carriage rates of GBS in Kenya and Rwanda and E. coli in Rwanda have not yet been described.
Risk factors for vaginal E. coli and GBS carriage
The presence of vaginal C. albicans, recent vaginal intercourse, working as a FSW, an intermediate vaginal microbiome, BV, washing the vagina and cervical ectopy were independent risk factors for vaginal GBS or E. coli colonization.
Women carrying C. albicans were 3.6 times more likely also to carry GBS. Three US based studies have shown this same significantly positive association between GBS and Candida or yeast [40, 88, 89].
Intravaginal practices, like e.g. cleaning inside the vagina beyond the introitus or insertion of substances into the vagina to dry or tighten the vagina, are common in Africa and are associated with adverse outcomes including increased risk for BV and for sexually transmitted infections [90]. Our model showed that washing inside the vagina was an independent risk factor for vaginal GBS carriage: women were twice as likely to be colonized with GBS compared to women not washing inside the vagina. A study by van de Wijgert and coworkers [91] showed that women using substances other than plain water to finger-clean or wipe inside the vagina had a GBS prevalence of 26.3% (n = 99), whereas women not engaging in these practices had a GBS prevalence of 14.7% (n = 70). However, their findings did not reach significance, most probably because of the smaller sample size (169 women compared to 424 women in our study).
Women who had recent vaginal sex (the morning or evening before the study visit) were more than twice as likely to carry GBS vaginally than women who did not. Accordingly, a positive PSA test was also significantly correlated with GBS carriage. GBS is generally not considered an STI, and the influence of sexual behavior on vaginal GBS carriage or acquisition is a matter of debate [92–94]. Based on published literature and our own data, we hypothesize that sexual activity might lead to a brief temporal GBS colonization of the vagina. This hypothesis is strengthened by a recent longitudinal deep-sequencing study of the vaginal microbiome, where 25 women were sampled on a daily basis over a 10 week period, revealing an average of 0.39 GBS episodes per week and an average GBS episode of 2.8 days (Fig 1 and additional file 4 in [95]), contrasting with earlier studies—where sampling occurred every 3 weeks—that report average GBS episodes of 13.7 weeks [96]. The brief colonization might explain why we and other authors find parameters such as ‘age of first sexual intercourse’ not to be associated with GBS carriage (they do not cover the recent aspect), while parameters such as ‘high frequency of intercourse during last month’ (as a consequence, a higher chance of also having had recent intercourse) do correlate. Taken together, GBS should be considered as a potentially pathogenic micro-organism that can be sexually transmitted and whose vaginal presence can be enhanced by sexual activity.
Cervical ectopy was an independent risk factor for vaginal E. coli carriage, 21.9% of women without cervical ectopy were E. coli carriers as opposed to 35.2% of women with cervical ectopy. Cervical ectopy has been associated with CT [97], HPV [98] and an increased susceptibility to HIV infection [99]. Although we could not determine the cause-effect relation of this association, it seems biologically plausible that a niche is created by the glandular columnar epithelium of women with cervical ectopy that somehow—directly or indirectly—favors the colonization by E. coli. Some studies have e.g. related cervical ectopy with a reduced cell-mediated or changed humoral immunity [21, 100].
Working as a FSW was an independent risk factor for vaginal E. coli carriage. We could not explain this by any of the sexual behavioural or other parameters presented in Table 4. In our study, none of the participants, including the female sex workers, reported having had anal intercourse during the last 3 months. These percentages probably are underestimates, since stigma associated with anal intercourse often leads to reduced reporting [101]. Furthermore, Ghanem and coworkers [102] showed that regarding anal intercourse, significantly more women reported to engage in these practices when asked by means of computer assisted self interviews compared to face-to-face interviews, which was used in our study. It is not unlikely that FSW engage more in anal intercourse, compared to the general population, and that in our FSW population, vaginal contamination with E. coli is higher by transfer of (peri)anal bacteria during anal/vaginal intercourse. Other studies from East-Africa report anal intercourse prevalences in FSW of up to 40.8% [103]. Interestingly, anal intercourse during pregnancy has been reported as a significant risk factor for neonatal E. coli colonization [77].
Besides above-mentioned risk factors for GBS or E. coli carriage, we show for the first time that colonization with GBS and E. coli, the leading causes of EOS, are positively associated.
Abovementioned risk factors can be translated and implemented into strategies that aim to reduce the maternal carriage of GBS and E. coli. First, behavioral change by advocating abstinence from sexual intercourse and vaginal washing during late pregnancy, e.g. via counseling in family planning facilities, could help to reduce the risk of maternal GBS and E. coli colonization in resource-poor settings. Second, the extension of GBS screening with screening for C. albicans and E. coli–risk factors for vaginal GBS carriage–should be further investigated. Furthermore, the screening for E. coli itself also merits further investigation because of its role as a major EOS causative agent for which currently no prevention measures are taken, nor in low-income, nor in high-income countries [104]. In this context, the presence of cervical ectopy–a risk factor for vaginal E. coli carriage–should be further investigated.
GBS serotype distribution
As IAP is not effective against LOS and culture-based screening and administration of costly intravenous antibiotics might not be feasible in most low-income countries, an alternative and long-term solution lies in the development of effective GBS vaccines, that however would not cover for other micro-organisms causing EOS. As most GBS vaccines under development aim at eliciting protective antibodies against capsular polysaccharides, the principal difficulty in developing globally effective GBS vaccines is the existence of several serotypes with different geographical distributions. In our study, the most prevalent GBS serotypes were Ia (27.3%), V (27.3%) and III (22.7%) in Kenya; Ia (34.5%), V (31.0%), and IV (13.8%) in SA; and Ia (83.3%) and II (16.7%) in Rwanda. Only few other studies have documented vaginal GBS serotype distribution in Africa and these are largely in line with our findings (Table 4 and Fig 1).
Interestingly, compared to the low prevalences in Europe and the US, we found relatively high prevalences of serotypes IV, VI, VII–shown for the first time in sub-Saharan Africa—and VIII in the Kenyan and South African population (VI, 13.6%; VII, 4.5%; VIII 4.5% in Kenya, and IV, 13.8%; VI, 6.9%; VIII, 3.4% in SA) (Table 4). In contrast, we did not detect any serotype Ib, which has, according to a recent meta-analysis, a prevalence of 8.1% in the US and 12.4% in Europe [38].
Differences in serotype distribution between our study and other studies (Table 4) might be explained by differences in study populations, most studies listed in Table 4 typed strains isolated from pregnant women whereas most of our GBS strains were isolated from non-pregnant women. Methodological differences might also contribute. Many GBS capsular polysaccharide typing methods have been described, with the most commonly used method being a serological test, used by all studies listed in Table 4, except our study. We used a molecular capsular typing method, developed and applied by European (reference) laboratories [105, 106]. Brigtsen and coworkers (2015) compared capsular typing of 426 GBS strains by a conventional latex agglutination test with PCR, and found that a substantial proportion of the strains were non-typeable by serotyping, but typeable by genotyping, and that an agreement between serotyping and genotyping was shown in 71.1% (of the isolates that were typeable by both methods) [107]. Moreover, we used a molecular technique directly on DNA extracts from vaginal swabs (and not on DNA extracts from isolates), which could lead to the detection of certain serotypes that would not have been isolated by culture.
Currently, there are two candidate vaccines in phase II clinical trials, i.e. a trivalent vaccine targeting serotypes Ia, Ib, and III, and a conjugate vaccine targeting serotype III (www.clinicaltrials.gov). In theory, the first vaccine could cover for 50.0%, 83.3% and 44.8% of vaginal GBS cases in our Mombasa, Kigali and Johannesburg population, respectively, but only a minority of women would be protected by the conjugate vaccine (22.7%, 0% and 10.3%, respectively).
GBS, E. coli and the vaginal microbiome
Our results show that vaginal GBS and E. coli carriage were significantly associated with disturbances of the vaginal microbiome: compared to women with a normal vaginal microbiome, women with an intermediate vaginal microbiome were 2.61 times more likely to carry E. coli, whereas women with BV were 2.33 less likely to carry GBS. The latter finding is in accordance a study of Hillier and coworkers [108], reporting a significant negative association between GBS carriage and BV by Nugent scoring, studying 7,918 pregnant women. Two other studies did not confirm these findings [94, 109]. In depth analysis of abovementioned interdependencies of GBS, E. coli, C. albicans, BV and the vaginal microbiome will be published elsewhere.
Our study was limited by the fact that we used vaginal sampling instead of rectovaginal sampling for the detection of GBS (as recommended by the CDC), which has been shown to have higher recovery rates for GBS. Furthermore, we did not use a selective broth enrichment prior to PCR, as recommended by the CDC. In our study, pregnant women were up to 14 weeks of gestation, and were not sampled at 35–37 weeks’ gestation as recommended by the CDC, which could have biased our results. Our study was further limited by the rather small sample size of our Rwanda study population.
In conclusion, vaginal GBS carriage rate and serotype distribution were similar to high-income countries, except for the higher prevalence of serotypes VI, VII and VIII. E. coli carriage rate was higher compared to high-income countries. We identified risk factors for GBS or E. coli carriage, ie. recent sexual intercourse, vaginal washing, C. albicans colonization and presence of cervical ectopy, that can be implemented in strategies to reduce maternal colonization. Immunoprophylaxis with current phase II candidate GBS vaccines would not protect the majority of women against vaginal GBS carriage in our study population. The most important causative agents of EOS, GBS and E. coli, both associated with disturbances of the vaginal microbiome, are positively associated.
Acknowledgments
The authors wish to thank Pierette Melin (Belgian Streptococcus agalactiae reference center) for providing us S. agalactiae control strains.
Data Availability
All relevant data are available in the paper.
Funding Statement
The project was funded by the European & Developing Countries Clinical Trials Partnership (IP_2007_33070_001, http://www.edctp.org/). The funders had no role in study design, data collection and analysis, decision to publish, or preparation of the manuscript.
References
- 1.Lawn JE, Cousens S, Zupan J, Lancet Neonatal Survival Steering T. 4 million neonatal deaths: when? Where? Why? Lancet. 2005;365(9462):891–900. 10.1016/S0140-6736(05)71048-5 . [DOI] [PubMed] [Google Scholar]
- 2.Hornik CP, Fort P, Clark RH, Watt K, Benjamin DK Jr, Smith PB, et al. Early and late onset sepsis in very-low-birth-weight infants from a large group of neonatal intensive care units. Early Hum Dev. 2012;88 Suppl 2:S69–74. 10.1016/S0378-3782(12)70019-1 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Schuchat A. Epidemiology of group B streptococcal disease in the United States: shifting paradigms. Clin Microbiol Rev. 1998;11(3):497–513. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Cutland CL, Madhi SA, Zell ER, Kuwanda L, Laque M, Groome M, et al. Chlorhexidine maternal-vaginal and neonate body wipes in sepsis and vertical transmission of pathogenic bacteria in South Africa: a randomised, controlled trial. Lancet. 2009;374(9705):1909–16. 10.1016/S0140-6736(09)61339-8 . [DOI] [PubMed] [Google Scholar]
- 5.Simonsen KA, Anderson-Berry AL, Delair SF, Davies HD. Early-onset neonatal sepsis. Clin Microbiol Rev. 2014;27(1):21–47. 10.1128/CMR.00031-13 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Krohn MA, Thwin SS, Rabe LK, Brown Z, Hillier SL. Vaginal colonization by Escherichia coli as a risk factor for very low birth weight delivery and other perinatal complications. J Infect Dis. 1997;175(3):606–10. . [DOI] [PubMed] [Google Scholar]
- 7.Acosta CD, Kurinczuk JJ, Lucas DN, Tuffnell DJ, Sellers S, Knight M, et al. Severe maternal sepsis in the UK, 2011–2012: a national case-control study. PLoS Med. 2014;11(7):e1001672 10.1371/journal.pmed.1001672 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Beck S, Wojdyla D, Say L, Betran AP, Merialdi M, Requejo JH, et al. The worldwide incidence of preterm birth: a systematic review of maternal mortality and morbidity. Bull World Health Organ. 2010;88(1):31–8. 10.2471/BLT.08.062554 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Khan KS, Wojdyla D, Say L, Gulmezoglu AM, Van Look PF. WHO analysis of causes of maternal death: a systematic review. Lancet. 2006;367(9516):1066–74. 10.1016/S0140-6736(06)68397-9 . [DOI] [PubMed] [Google Scholar]
- 10.Melin P, Efstratiou A. Group B streptococcal epidemiology and vaccine needs in developed countries. Vaccine. 2013;31 Suppl 4:D31–42. 10.1016/j.vaccine.2013.05.012 . [DOI] [PubMed] [Google Scholar]
- 11.Schrag SJ, Zywicki S, Farley MM, Reingold AL, Harrison LH, Lefkowitz LB, et al. Group B streptococcal disease in the era of intrapartum antibiotic prophylaxis. N Engl J Med. 2000;342(1):15–20. 10.1056/NEJM200001063420103 . [DOI] [PubMed] [Google Scholar]
- 12.Regan JA, Klebanoff MA, Nugent RP, Eschenbach DA, Blackwelder WC, Lou Y, et al. Colonization with group B streptococci in pregnancy and adverse outcome. VIP Study Group. Am J Obstet Gynecol. 1996;174(4):1354–60. . [DOI] [PubMed] [Google Scholar]
- 13.Ohlsson A, Shah VS. Intrapartum antibiotics for known maternal Group B streptococcal colonization. Cochrane Database Syst Rev. 2014;6:CD007467 10.1002/14651858.CD007467.pub4 . [DOI] [PubMed] [Google Scholar]
- 14.Verani JR, McGee L, Schrag SJ, Division of Bacterial Diseases NCfI, Respiratory Diseases CfDC, Prevention. Prevention of perinatal group B streptococcal disease—revised guidelines from CDC, 2010. MMWR Recomm Rep. 2010;59(RR-10):1–36. . [PubMed] [Google Scholar]
- 15.Johri AK, Paoletti LC, Glaser P, Dua M, Sharma PK, Grandi G, et al. Group B Streptococcus: global incidence and vaccine development. Nat Rev Microbiol. 2006;4(12):932–42. 10.1038/nrmicro1552 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Capan M, Mombo-Ngoma G, Akerey-Diop D, Basra A, Wurbel H, Lendamba W, et al. Epidemiology and management of group B streptococcal colonization during pregnancy in Africa. Wien Klin Wochenschr. 2012;124 Suppl 3:14–6. 10.1007/s00508-012-0239-5 . [DOI] [PubMed] [Google Scholar]
- 17.Stoll BJ, Schuchat A. Maternal carriage of group B streptococci in developing countries. Pediatr Infect Dis J. 1998;17(6):499–503. . [DOI] [PubMed] [Google Scholar]
- 18.Gautam R, Borgdorff H, Jespers V, Francis SC, Verhelst R, Mwaura M, et al. Correlates of the molecular vaginal microbiota composition of African women. BMC Infect Dis. 2015;15:86 10.1186/s12879-015-0831-1 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Jespers V, Crucitti T, Menten J, Verhelst R, Mwaura M, Mandaliya K, et al. Prevalence and correlates of bacterial vaginosis in different sub-populations of women in sub-Saharan Africa: a cross-sectional study. PLoS One. 2014;9(10):e109670 10.1371/journal.pone.0109670 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Jespers V, van de Wijgert J, Cools P, Verhelst R, Verstraelen H, Delany-Moretlwe S, et al. The significance of Lactobacillus crispatus and L. vaginalis for vaginal health and the negative effect of recent sex: a cross-sectional descriptive study across groups of African women. BMC Infect Dis. 2015;15:115 10.1186/s12879-015-0825-z [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Kyongo JK, Crucitti T, Menten J, Hardy L, Cools P, Michiels J, et al. Cross-Sectional Analysis of Selected Genital Tract Immunological Markers and Molecular Vaginal Microbiota in Sub-Saharan African Women, with Relevance to HIV Risk and Prevention. Clin Vaccine Immunol. 2015;22(5):526–38. 10.1128/CVI.00762-14 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Nugent RP, Krohn MA, Hillier SL. Reliability of diagnosing bacterial vaginosis is improved by a standardized method of gram stain interpretation. J Clin Microbiol. 1991;29(2):297–301. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Bergh K, Stoelhaug A, Loeseth K, Bevanger L. Detection of group B streptococci (GBS) in vaginal swabs using real-time PCR with TaqMan probe hybridization. Indian J Med Res. 2004;119 Suppl:221–3. . [PubMed] [Google Scholar]
- 24.Chern EC, Siefring S, Paar J, Doolittle M, Haugland RA. Comparison of quantitative PCR assays for Escherichia coli targeting ribosomal RNA and single copy genes. Lett Appl Microbiol. 2011;52(3):298–306. 10.1111/j.1472-765X.2010.03001.x . [DOI] [PubMed] [Google Scholar]
- 25.Guiver M, Levi K, Oppenheim BA. Rapid identification of candida species by TaqMan PCR. J Clin Pathol. 2001;54(5):362–6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Rabe LK, Hillier SL. Optimization of media for detection of hydrogen peroxide production by Lactobacillus species. J Clin Microbiol. 2003;41(7):3260–4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Verhelst R, Verstraelen H, Claeys G, Verschraegen G, Delanghe J, Van Simaey L, et al. Cloning of 16S rRNA genes amplified from normal and disturbed vaginal microflora suggests a strong association between Atopobium vaginae, Gardnerella vaginalis and bacterial vaginosis. BMC Microbiol. 2004;4:16 10.1186/1471-2180-4-16 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Yao K, Poulsen K, Maione D, Rinaudo CD, Baldassarri L, Telford JL, et al. Capsular gene typing of Streptococcus agalactiae compared to serotyping by latex agglutination. J Clin Microbiol. 2013;51(2):503–7. 10.1128/JCM.02417-12 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Poyart C, Tazi A, Reglier-Poupet H, Billoet A, Tavares N, Raymond J, et al. Multiplex PCR assay for rapid and accurate capsular typing of group B streptococci. J Clin Microbiol. 2007;45(6):1985–8. 10.1128/JCM.00159-07 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Imperi M, Pataracchia M, Alfarone G, Baldassarri L, Orefici G, Creti R. A multiplex PCR assay for the direct identification of the capsular type (Ia to IX) of Streptococcus agalactiae. J Microbiol Methods. 2010;80(2):212–4. 10.1016/j.mimet.2009.11.010 . [DOI] [PubMed] [Google Scholar]
- 31.Macaluso M, Lawson L, Akers R, Valappil T, Hammond K, Blackwell R, et al. Prostate-specific antigen in vaginal fluid as a biologic marker of condom failure. Contraception. 1999;59(3):195–201. . [DOI] [PubMed] [Google Scholar]
- 32.Babyak MA. What you see may not be what you get: a brief, nontechnical introduction to overfitting in regression-type models. Psychosom Med. 2004;66(3):411–21. . [DOI] [PubMed] [Google Scholar]
- 33.Wakkee M, Hollestein LM, Nijsten T. Multivariable analysis. J Invest Dermatol. 2014;134(5):e20; quiz e. 10.1038/jid.2014.132 . [DOI] [PubMed] [Google Scholar]
- 34.Suara RO, Adegbola RA, Baker CJ, Secka O, Mulholland EK, Greenwood BM. Carriage of group B Streptococci in pregnant Gambian mothers and their infants. J Infect Dis. 1994;170(5):1316–9. . [DOI] [PubMed] [Google Scholar]
- 35.Gray KJ, Kafulafula G, Matemba M, Kamdolozi M, Membe G, French N. Group B Streptococcus and HIV infection in pregnant women, Malawi, 2008–2010. Emerg Infect Dis. 2011;17(10):1932–5. 10.3201/eid1710.102008 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Madzivhandila M, Adrian PV, Cutland CL, Kuwanda L, Schrag SJ, Madhi SA. Serotype distribution and invasive potential of group B streptococcus isolates causing disease in infants and colonizing maternal-newborn dyads. PLoS One. 2011;6(3):e17861 10.1371/journal.pone.0017861 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Kwatra G, Adrian PV, Shiri T, Buchmann EJ, Cutland CL, Madhi SA. Serotype-specific acquisition and loss of group B streptococcus recto-vaginal colonization in late pregnancy. PLoS One. 2014;9(6):e98778 10.1371/journal.pone.0098778 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Ippolito DL, James WA, Tinnemore D, Huang RR, Dehart MJ, Williams J, et al. Group B streptococcus serotype prevalence in reproductive-age women at a tertiary care military medical center relative to global serotype distribution. BMC Infect Dis. 2010;10:336 10.1186/1471-2334-10-336 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Kim EJ, Oh KY, Kim MY, Seo YS, Shin JH, Song YR, et al. Risk factors for group B streptococcus colonization among pregnant women in Korea. Epidemiol Health. 2011;33:e2011010 10.4178/epih/e2011010 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Regan JA, Klebanoff MA, Nugent RP. The epidemiology of group B streptococcal colonization in pregnancy. Vaginal Infections and Prematurity Study Group. Obstet Gynecol. 1991;77(4):604–10. . [PubMed] [Google Scholar]
- 41.Hastings MJ, Easmon CS, Neill J, Bloxham B, Rivers RP. Group B streptococcal colonisation and the outcome of pregnancy. J Infect. 1986;12(1):23–9. . [DOI] [PubMed] [Google Scholar]
- 42.Valkenburg-van den Berg AW, Sprij AJ, Oostvogel PM, Mutsaers JA, Renes WB, Rosendaal FR, et al. Prevalence of colonisation with group B Streptococci in pregnant women of a multi-ethnic population in The Netherlands. Eur J Obstet Gynecol Reprod Biol. 2006;124(2):178–83. 10.1016/j.ejogrb.2005.06.007 . [DOI] [PubMed] [Google Scholar]
- 43.Moyo SR, Mudzori J, Tswana SA, Maeland JA. Prevalence, capsular type distribution, anthropometric and obstetric factors of group B Streptococcus (Streptococcus agalactiae) colonization in pregnancy. Cent Afr J Med. 2000;46(5):115–20. . [DOI] [PubMed] [Google Scholar]
- 44.Baker CJ, Goroff DK, Alpert S, Crockett VA, Zinner SH, Evrard JR, et al. Vaginal colonization with group B streptococcus: a study in college women. J Infect Dis. 1977;135(3):392–7. . [DOI] [PubMed] [Google Scholar]
- 45.Baker CJ, Barrett FF, Yow MD. The influence of advancing gestation on group B streptococcal colonization in pregnant women. Am J Obstet Gynecol. 1975;122(7):820–3. . [DOI] [PubMed] [Google Scholar]
- 46.Hadavand S, Ghafoorimehr F, Rajabi L, Davati A, Zafarghandi N. Frequency of Group B Streptococcal Colonization in Pregnant Women Aged 35–37 Weeks in Clinical Centers of Shahed University, Tehran, Iran. Iran J Pathol. 2015;10(2):120–6. [PMC free article] [PubMed] [Google Scholar]
- 47.Javanmanesh F, Eshraghi N. Prevalence of positive recto-vaginal culture for Group B streptococcus in pregnant women at 35–37 weeks of gestation. Med J Islam Repub Iran. 2013;27(1):7–11. [PMC free article] [PubMed] [Google Scholar]
- 48.Gupta C, Briski LE. Comparison of two culture media and three sampling techniques for sensitive and rapid screening of vaginal colonization by group B streptococcus in pregnant women. J Clin Microbiol. 2004;42(9):3975–7. 10.1128/JCM.42.9.3975-3977.2004 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.El Aila NA, Tency I, Claeys G, Saerens B, Cools P, Verstraelen H, et al. Comparison of different sampling techniques and of different culture methods for detection of group B streptococcus carriage in pregnant women. BMC Infect Dis. 2010;10:285 10.1186/1471-2334-10-285 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.El Aila NA, Tency I, Claeys G, Verstraelen H, Deschaght P, Decat E, et al. Comparison of culture with two different qPCR assays for detection of rectovaginal carriage of Streptococcus agalactiae (group B streptococci) in pregnant women. Res Microbiol. 2011;162(5):499–505. 10.1016/j.resmic.2011.04.001 . [DOI] [PubMed] [Google Scholar]
- 51.Davies HD, Miller MA, Faro S, Gregson D, Kehl SC, Jordan JA. Multicenter study of a rapid molecular-based assay for the diagnosis of group B Streptococcus colonization in pregnant women. Clin Infect Dis. 2004;39(8):1129–35. 10.1086/424518 . [DOI] [PubMed] [Google Scholar]
- 52.Convert M, Martinetti Lucchini G, Dolina M, Piffaretti JC. Comparison of LightCycler PCR and culture for detection of group B streptococci from vaginal swabs. Clin Microbiol Infect. 2005;11(12):1022–6. 10.1111/j.1469-0691.2005.01275.x . [DOI] [PubMed] [Google Scholar]
- 53.Rallu F, Barriga P, Scrivo C, Martel-Laferriere V, Laferriere C. Sensitivities of antigen detection and PCR assays greatly increased compared to that of the standard culture method for screening for group B streptococcus carriage in pregnant women. J Clin Microbiol. 2006;44(3):725–8. 10.1128/JCM.44.3.725-728.2006 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Joachim A, Matee MI, Massawe FA, Lyamuya EF. Maternal and neonatal colonisation of group B streptococcus at Muhimbili National Hospital in Dar es Salaam, Tanzania: prevalence, risk factors and antimicrobial resistance. BMC Public Health. 2009;9:437 10.1186/1471-2458-9-437 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Onile BA. Group B streptococcal carriage in Nigeria. Trans R Soc Trop Med Hyg. 1980;74(3):367–70. . [DOI] [PubMed] [Google Scholar]
- 56.Dawodu AH, Damole IO, Onile BA. Epidemiology of group B streptococcal carriage among pregnant women and their neonates: an African experience. Trop Geogr Med. 1983;35(2):145–50. . [PubMed] [Google Scholar]
- 57.Nathoo KJ, Mason PR, Chimbira TH. Neonatal septicaemia in Harare Hospital: aetiology and risk factors. The Puerperal Sepsis Study Group. Cent Afr J Med. 1990;36(6):150–6. . [PubMed] [Google Scholar]
- 58.David-Prince M, Ategbo S, De Souza AE, Eklu-Avlassu EK, Grunitzky-Bekele M, Schmidt-Ehry G, et al. [Carriage of Streptococcus B in the mother and infant pair at birth. Apropos of 106 cases]. Bull Soc Pathol Exot. 1991;84(5 Pt 5):522–31. . [PubMed] [Google Scholar]
- 59.Dzowela TK OO; Igbigbi A. Prevalence of group B Streptococcus colonization in antenatal women at the Queen Elizabeth Central Hospital Blantyre—a preliminary study. Malawi Medical Journal. 2005;17(3):97–9. [Google Scholar]
- 60.de Steenwinkel FD, Tak HV, Muller AE, Nouwen JL, Oostvogel PM, Mocumbi SM. Low carriage rate of group B streptococcus in pregnant women in Maputo, Mozambique. Trop Med Int Health. 2008;13(3):427–9. 10.1111/j.1365-3156.2008.02018.x . [DOI] [PubMed] [Google Scholar]
- 61.Mavenyengwa RT, Afset JE, Schei B, Berg S, Caspersen T, Bergseng H, et al. Group B Streptococcus colonization during pregnancy and maternal-fetal transmission in Zimbabwe. Acta Obstet Gynecol Scand. 2010;89(2):250–5. 10.3109/00016340903398029 . [DOI] [PubMed] [Google Scholar]
- 62.Mitima KT, Ntamako S, Birindwa AM, Mukanire N, Kivukuto JM, Tsongo K, et al. Prevalence of colonization by Streptococcus agalactiae among pregnant women in Bukavu, Democratic Republic of the Congo. J Infect Dev Ctries. 2014;8(9):1195–200. 10.3855/jidc.5030 . [DOI] [PubMed] [Google Scholar]
- 63.Karou SD, Djigma F, Sagna T, Nadembega C, Zeba M, Kabre A, et al. Antimicrobial resistance of abnormal vaginal discharges microorganisms in Ouagadougou, Burkina Faso. Asian Pac J Trop Biomed. 2012;2(4):294–7. 10.1016/S2221-1691(12)60025-2 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64.Ekwempu CC, Lawande RV, Egler LJ. Microbial flora of the lower genital tract of women in labour in Zaria, Nigeria. J Clin Pathol. 1981;34(1):82–3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65.Schellenberg JJ, Links MG, Hill JE, Dumonceaux TJ, Kimani J, Jaoko W, et al. Molecular definition of vaginal microbiota in East African commercial sex workers. Appl Environ Microbiol. 2011;77(12):4066–74. 10.1128/AEM.02943-10 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 66.Cutland CL, Schrag SJ, Zell ER, Kuwanda L, Buchmann E, Velaphi SC, et al. Maternal HIV infection and vertical transmission of pathogenic bacteria. Pediatrics. 2012;130(3):e581–90. 10.1542/peds.2011-1548 . [DOI] [PubMed] [Google Scholar]
- 67.Sagna T, Djigma F, Zeba M, Bisseye C, Karou SD, Ouermi D, et al. Human papillomaviruses prevalence and genital co-infections in HIV-seropositive women in Ouagadougou (Burkina Faso). Pak J Biol Sci. 2010;13(19):951–5. . [DOI] [PubMed] [Google Scholar]
- 68.Razzak MS, Al-Charrakh AH, Al-Greitty BH. Relationship between lactobacilli and opportunistic bacterial pathogens associated with vaginitis. N Am J Med Sci. 2011;3(4):185–92. 10.4297/najms.2011.3185 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 69.Mobasheri M, Saeedi Varnamkhast N, Karimi A, Banaeiyan S. Prevalence study of genital tract infections in pregnant women referred to health centers in Iran. Turk J Med Sci. 2014;44(2):232–6. . [DOI] [PubMed] [Google Scholar]
- 70.Obata-Yasuoka M, Ba-Thein W, Tsukamoto T, Yoshikawa H, Hayashi H. Vaginal Escherichia coli share common virulence factor profiles, serotypes and phylogeny with other extraintestinal E. coli. Microbiology. 2002;148(Pt 9):2745–52. . [DOI] [PubMed] [Google Scholar]
- 71.Kazi YF, Saleem S, Kazi N. Investigation of vaginal microbiota in sexually active women using hormonal contraceptives in Pakistan. BMC Urol. 2012;12:22 10.1186/1471-2490-12-22 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 72.Ocak S, Cetin M, Hakverdi S, Dolapcioglu K, Gungoren A, Hakverdi AU. Effects of intrauterine device and oral contraceptive on vaginal flora and epithelium. Saudi Med J. 2007;28(5):727–31. . [PubMed] [Google Scholar]
- 73.Kaliterna V, Kucisec-Tepes N, Pejkovic L, Zavorovic S, Petrovic S, Barisic Z. An intrauterine device as a possible cause of change in the microbial flora of the female genital system. J Obstet Gynaecol Res. 2011;37(8):1035–40. 10.1111/j.1447-0756.2010.01480.x . [DOI] [PubMed] [Google Scholar]
- 74.Stokholm J, Schjorring S, Eskildsen CE, Pedersen L, Bischoff AL, Folsgaard N, et al. Antibiotic use during pregnancy alters the commensal vaginal microbiota. Clin Microbiol Infect. 2014;20(7):629–35. 10.1111/1469-0691.12411 . [DOI] [PubMed] [Google Scholar]
- 75.Chase DJ, Schenkel BP, Fahr AM, Eigner U, Tampon Study G. A prospective, randomized, double-blind study of vaginal microflora and epithelium in women using a tampon with an apertured film cover compared with those in women using a commercial tampon with a cover of nonwoven fleece. J Clin Microbiol. 2007;45(4):1219–24. 10.1128/JCM.02156-06 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 76.Iavazzo C, Vogiatzi C, Falagas ME. A retrospective analysis of isolates from patients with vaginitis in a private Greek obstetric/gynecological hospital (2003–2006). Med Sci Monit. 2008;14(4):CR228–31. . [PubMed] [Google Scholar]
- 77.Tameliene R, Barcaite E, Stoniene D, Buinauskiene J, Markuniene E, Kudreviciene A, et al. Escherichia coli colonization in neonates: prevalence, perinatal transmission, antimicrobial susceptibility, and risk factors. Medicina (Kaunas). 2012;48(2):71–6. . [PubMed] [Google Scholar]
- 78.Bayo M, Berlanga M, Agut M. Vaginal microbiota in healthy pregnant women and prenatal screening of group B streptococci (GBS). Int Microbiol. 2002;5(2):87–90. . [DOI] [PubMed] [Google Scholar]
- 79.Guiral E, Bosch J, Vila J, Soto SM. Prevalence of Escherichia coli among samples collected from the genital tract in pregnant and nonpregnant women: relationship with virulence. FEMS Microbiol Lett. 2011;314(2):170–3. 10.1111/j.1574-6968.2010.02160.x . [DOI] [PubMed] [Google Scholar]
- 80.Nikolaitchouk N, Andersch B, Falsen E, Strombeck L, Mattsby-Baltzer I. The lower genital tract microbiota in relation to cytokine-, SLPI- and endotoxin levels: application of checkerboard DNA-DNA hybridization (CDH). APMIS. 2008;116(4):263–77. 10.1111/j.1600-0463.2008.00808.x . [DOI] [PubMed] [Google Scholar]
- 81.Percival-Smith R, Bartlett KH, Chow AW. Vaginal colonization of Escherichia coli and its relation to contraceptive methods. Contraception. 1983;27(5):497–504. . [DOI] [PubMed] [Google Scholar]
- 82.Eschenbach DA, Patton DL, Hooton TM, Meier AS, Stapleton A, Aura J, et al. Effects of vaginal intercourse with and without a condom on vaginal flora and vaginal epithelium. J Infect Dis. 2001;183(6):913–8. 10.1086/319251 . [DOI] [PubMed] [Google Scholar]
- 83.Hyman RW, Fukushima M, Diamond L, Kumm J, Giudice LC, Davis RW. Microbes on the human vaginal epithelium. Proc Natl Acad Sci U S A. 2005;102(22):7952–7. 10.1073/pnas.0503236102 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 84.Ghartey JP, Carpenter C, Gialanella P, Rising C, McAndrew TC, Mhatre M, et al. Association of bactericidal activity of genital tract secretions with Escherichia coli colonization in pregnancy. Am J Obstet Gynecol. 2012;207(4):297 e1-8. 10.1016/j.ajog.2012.07.025 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 85.Anderson BL, Mendez-Figueroa H, Dahlke JD, Raker C, Hillier SL, Cu-Uvin S. Pregnancy-induced changes in immune protection of the genital tract: defining normal. Am J Obstet Gynecol. 2013;208(4):321 e1-9. 10.1016/j.ajog.2013.01.014 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 86.Villar HE, Aubert V, Baserni MN, Jugo MB. Maternal carriage of extended-spectrum beta-lactamase-producing Escherichia coli isolates in Argentina. J Chemother. 2013;25(6):324–7. 10.1179/1973947813Y.0000000081 . [DOI] [PubMed] [Google Scholar]
- 87.Lobos O, Padilla C. Phenotypic characterization and genomic DNA polymorphisms of Escherichia coli strains isolated as the sole micro-organism from vaginal infections. Microbiology. 2009;155(Pt 3):825–30. 10.1099/mic.0.021733-0 . [DOI] [PubMed] [Google Scholar]
- 88.Cotch MF, Hillier SL, Gibbs RS, Eschenbach DA. Epidemiology and outcomes associated with moderate to heavy Candida colonization during pregnancy. Vaginal Infections and Prematurity Study Group. Am J Obstet Gynecol. 1998;178(2):374–80. . [DOI] [PubMed] [Google Scholar]
- 89.Beigi RH, Meyn LA, Moore DM, Krohn MA, Hillier SL. Vaginal yeast colonization in nonpregnant women: a longitudinal study. Obstet Gynecol. 2004;104(5 Pt 1):926–30. 10.1097/01.AOG.0000140687.51048.73 . [DOI] [PubMed] [Google Scholar]
- 90.Low N, Chersich MF, Schmidlin K, Egger M, Francis SC, van de Wijgert JH, et al. Intravaginal practices, bacterial vaginosis, and HIV infection in women: individual participant data meta-analysis. PLoS Med. 2011;8(2):e1000416 10.1371/journal.pmed.1000416 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 91.van De Wijgert JH, Mason PR, Gwanzura L, Mbizvo MT, Chirenje ZM, Iliff V, et al. Intravaginal practices, vaginal flora disturbances, and acquisition of sexually transmitted diseases in Zimbabwean women. J Infect Dis. 2000;181(2):587–94. 10.1086/315227 . [DOI] [PubMed] [Google Scholar]
- 92.Foxman B, de Azevedo CL, Buxton M, DeBusscher J, Pillai P, De Carvalho NS, et al. Acquisition and transmission of group B Streptococcus during pregnancy. J Infect Dis. 2008;198(9):1375–8. 10.1086/592221 . [DOI] [PubMed] [Google Scholar]
- 93.Foxman B, Gillespie BW, Manning SD, Marrs CF. Risk factors for group B streptococcal colonization: potential for different transmission systems by capsular type. Ann Epidemiol. 2007;17(11):854–62. 10.1016/j.annepidem.2007.05.014 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 94.Honig E, Mouton JW, van der Meijden WI. The epidemiology of vaginal colonisation with group B streptococci in a sexually transmitted disease clinic. Eur J Obstet Gynecol Reprod Biol. 2002;105(2):177–80. . [DOI] [PubMed] [Google Scholar]
- 95.Ravel J, Brotman RM, Gajer P, Ma B, Nandy M, Fadrosh DW, et al. Daily temporal dynamics of vaginal microbiota before, during and after episodes of bacterial vaginosis. Microbiome. 2013;1(1):29 10.1186/2049-2618-1-29 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 96.Foxman B, Gillespie B, Manning SD, Howard LJ, Tallman P, Zhang L, et al. Incidence and duration of group B Streptococcus by serotype among male and female college students living in a single dormitory. Am J Epidemiol. 2006;163(6):544–51. 10.1093/aje/kwj075 . [DOI] [PubMed] [Google Scholar]
- 97.Lee V, Tobin JM, Foley E. Relationship of cervical ectopy to chlamydia infection in young women. J Fam Plann Reprod Health Care. 2006;32(2):104–6. 10.1783/147118906776276440 . [DOI] [PubMed] [Google Scholar]
- 98.Rocha-Zavaleta L, Yescas G, Cruz RM, Cruz-Talonia F. Human papillomavirus infection and cervical ectopy. Int J Gynaecol Obstet. 2004;85(3):259–66. 10.1016/j.ijgo.2003.10.002 . [DOI] [PubMed] [Google Scholar]
- 99.Venkatesh KK, Cu-Uvin S. Assessing the relationship between cervical ectopy and HIV susceptibility: implications for HIV prevention in women. Am J Reprod Immunol. 2013;69 Suppl 1:68–73. 10.1111/aji.12029 . [DOI] [PubMed] [Google Scholar]
- 100.De Luca Brunori I, Facchini V, Filippeschi M, Battini L, Giusti G, Romani L, et al. Cell-mediated immunity in the course of cervical ectropion. Clin Exp Obstet Gynecol. 1994;21(2):105–7. . [PubMed] [Google Scholar]
- 101.Veldhuijzen NJ, Ingabire C, Luchters S, Bosire W, Braunstein S, Chersich M, et al. Anal intercourse among female sex workers in East Africa is associated with other high-risk behaviours for HIV. Sex Health. 2011;8(2):251–4. 10.1071/SH10047 . [DOI] [PubMed] [Google Scholar]
- 102.Ghanem KG, Hutton HE, Zenilman JM, Zimba R, Erbelding EJ. Audio computer assisted self interview and face to face interview modes in assessing response bias among STD clinic patients. Sex Transm Infect. 2005;81(5):421–5. 10.1136/sti.2004.013193 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 103.Schwandt M, Morris C, Ferguson A, Ngugi E, Moses S. Anal and dry sex in commercial sex work, and relation to risk for sexually transmitted infections and HIV in Meru, Kenya. Sex Transm Infect. 2006;82(5):392–6. 10.1136/sti.2006.019794 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 104.Stoll BJ, Hansen NI, Sanchez PJ, Faix RG, Poindexter BB, Van Meurs KP, et al. Early onset neonatal sepsis: the burden of group B Streptococcal and E. coli disease continues. Pediatrics. 2011;127(5):817–26. 10.1542/peds.2010-2217 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 105.Joubrel C, Tazi A, Six A, Dmytruk N, Touak G, Bidet P, et al. Group B streptococcus neonatal invasive infections, France 2007–2012. Clin Microbiol Infect. 2015;21(10):910–6. 10.1016/j.cmi.2015.05.039 . [DOI] [PubMed] [Google Scholar]
- 106.Afshar B, Broughton K, Creti R, Decheva A, Hufnagel M, Kriz P, et al. International external quality assurance for laboratory identification and typing of Streptococcus agalactiae (Group B streptococci). J Clin Microbiol. 2011;49(4):1475–82. 10.1128/JCM.02365-10 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 107.Brigtsen AK, Dedi L, Melby KK, Holberg-Petersen M, Radtke A, Lyng RV, et al. Comparison of PCR and serotyping of Group B Streptococcus in pregnant women: the Oslo GBS-study. J Microbiol Methods. 2015;108:31–5. 10.1016/j.mimet.2014.11.001 . [DOI] [PubMed] [Google Scholar]
- 108.Hillier SL, Krohn MA, Nugent RP, Gibbs RS. Characteristics of three vaginal flora patterns assessed by gram stain among pregnant women. Vaginal Infections and Prematurity Study Group. Am J Obstet Gynecol. 1992;166(3):938–44. . [DOI] [PubMed] [Google Scholar]
- 109.Rocchetti TT, Marconi C, Rall VL, Borges VT, Corrente JE, da Silva MG. Group B streptococci colonization in pregnant women: risk factors and evaluation of the vaginal flora. Arch Gynecol Obstet. 2011;283(4):717–21. 10.1007/s00404-010-1439-8 . [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
All relevant data are available in the paper.