Abstract
Little is known about perceptions surrounding self-management for attention deficit hyperactivity disorder (ADHD), although such interventions appear commonly used and are considered essential components of the chronic care model. Our research is part of a mixed methods study that followed students at high and low risk for ADHD over 11 years. During the final study years, area-representative samples of 148 adolescents (54.8% participation; 97 ADHD high-risk group; 51 low-risk peers) and 161 parents (59.4% participation; 108 parents of high-risk adolescent; 53 parents of low-risk peer) completed a cross-sectional survey on community-identified self-management interventions for ADHD (activity outlets, sleep regulation, dietary restriction, homework help, family rules, and prayer). Respondents also answered open-ended questions addressing undesirable self-management effects, which were analyzed using grounded theory methods. High-risk adolescents expressed significantly lower willingness towards all self-management interventions than did adult respondents, except for increased activity outlets. They also reported lower receptivity towards sleep regulation and dietary restriction than did their low-risk peer group. No gender or race differences in self-management willingness were found, except for higher receptivity to prayer in African American respondents. Cost, perceived ineffectiveness, disruptions to routines, causation of interpersonal conflicts, and reduced future self-reliance were seen as potential undesirable effects. Findings suggest that activity-based ADHD interventions appear particularly acceptable across all demographic and risk groups, unlike sleep regulation and dietary approaches. Further research on self-care effectiveness is needed to incorporate adolescents’ viewpoints about ADHD self-management, as interventions may be acceptable to adults, but resisted by adolescents.
Keywords: Attention Deficit Hyperactivity Disorder, intervention willingness, perceptions, side effect perceptions, mixed methods research, barriers to evidence-based treatment
Introduction
Attention-deficit/hyperactivity disorder (ADHD) is a highly prevalent, impairing neurodevelopmental disorder that frequently persists into adolescence and beyond (Lara et al., 2009). Evidence-based pharmacological and psychosocial therapies have been identified (Brown et al., 2005; Evans, Owens, & Bunford, 2014) and practice guidelines have been developed for pediatric (Wolraich et al., 2011) (Wolraich, et al., 2011) and specialty mental health settings (Pliszka, 2007). Yet, many families still fail to seek medical treatment for affected children (Sawyer et al., 2004), and ongoing adherence among those who start treatment tends to be low (Charach & Fernandez, 2013; Van Cleave & Leslie, 2008), with youth remaining untreated or receiving self-care, including complementary alternative treatments and other self-management strategies (Berwid & Halperin, 2012; Chan, 2002).
Gaining a clear understanding of the current extent of self-care for ADHD is important, because self-management assumes a recognized role in Chronic Care Models (Bodenheimer, Wagner, & Grumbach, 2002a, 2002b), including those proposed for pediatric mental health conditions such as ADHD to enhance access to care and outcomes (Van Cleave & Leslie, 2008). The chronic care model calls for family and self-management support among other essential “pillars” of care, along with decision supports, delivery system design, clinical information systems, and community resources (Van Cleave & Leslie, 2008). The World Health Organization (WHO) defined self-care as “activities individuals, families, and communities undertake with the intention of enhancing health, preventing disease, limiting illness and restoring health. These activities are derived from knowledge and skills from the pool of both professional and lay experience. They are undertaken by lay people on their own behalf, either separately or in participative collaboration with professionals” (WHO, 1984).
To date, however, there is limited research to guide systems to implement chronic care models and optimally support self-management for ADHD, a disorder frequently treated in primary care settings. A recent review of qualitative research on self-care experiences for mental disorders found that adults experientially used complementary therapies, sport and physical exercise, creative expression, diet modification, a structured routine for daily life, as well as religious and spiritual beliefs (Lucock et al., 2011). Only a few studies have examined self-management practices, preferences and perceptions among adolescents and young adults with ADHD, and conclusions are also limited by the studies’ small samples sizes. In a study of self-management procedures to enhance the classroom preparation skills for secondary students with ADHD, all participants showed improvement even after the program was systematically faded (Gureasko-Moore, Dupaul, & White, 2006). After an ADHD coaching intervention, undergraduate students reported improved self-regulation resulting in positive academic experiences (Parker, Hoffman, Sawilowsky, & Rolands, 2013). In a study of perceptions of non-medication treatments, Australian youth with ADHD identified “extra tutoring and learning assistance” as most beneficial (Leggett & Hotham, 2011). Sleep interventions for youth with ADHD have been reported to improve sleep, but not ADHD symptoms in two small clinical trials (Sciberras, Fulton, Efron, Oberklaid, & Hiscock, 2011; Weiss, Wasdell, Bomben, Rea, & Freeman, 2006).
Unlike other chronic conditions (e.g., diabetes mellitus), self-management practices for ADHD have not been formally assessed for professional endorsement or dissemination. Some ADHD self-management practices may be associated with physiological parameters shown to play a role in regulating activity and attention levels, such as physical exercise (Berwid & Halperin, 2012), sleep duration (Konofal, Lecendreux, & Cortese, 2010), or nutritional intake (Nigg, Lewis, Edinger, & Falk, 2012). Still others such as disciplinary strategies or prayer, may represent culturally situated interventions and thus applicable in some populations and not others (Bussing, M, Williamson, Gary, & Wilson Garvan, 2006). In the absence of empirically supported or guideline-recommended self-management practices, this study investigates six strategies (activity outlets, sleep regulation, dietary restriction, homework help, family rules, and prayer) that were identified through community-based research as being practiced in the community and as potentially helpful for youth with ADHD. Specifically, two quantitative research questions were addressed, with hypotheses formulated informed by previous research (Bussing et al., 2014; Bussing, Koro-Ljungberg, et al., 2012; Bussing, et al., 2006) as well as one qualitative inquiry (without a hypothesis):
-
Do adolescents and parents differ in their willingness to use ADHD self-management interventions, and does ADHD risk-status matter?
We hypothesized that, for all of the six ADHD interventions, adolescents would express lower willingness than would parents irrespective of risk-status and that adolescents’ willingness does not differ by risk status.
-
Do intervention perceptions, ADHD-risk status and demographic characteristics predict willingness to use ADHD self-management interventions?
We hypothesized that ADHD self-management willingness would positively correlate with higher perceptions of acceptability and effectiveness and negatively correlate with expectations of side effects and embarrassment. We further hypothesized that adolescents from the ADHD high-risk cohort would express lower intervention willingness than would parents in either risk cohort, but that high-risk adolescents would not differ from their low-risk peers. We finally hypothesized that African American respondents would express higher willingness to use prayer interventions than would their European American counterparts.
What perceptions of undesirable effects influence self-management for adolescents’ ADHD?
Method
Participants
The participants for this study were part of a longitudinal mixed methods study of ADHD detection and service use in the United States and included cohort members of our ADHD high-risk group and of the low-risk peer group (Bussing, Mason, Bell, Porter, & Garvan, 2010). Study participants originally were recruited in 1998 from stratified random sampling of public school records, oversampling girls by a factor of two to one to ensure sufficient female representation. Parents of 1,615 elementary school students completed telephone screening interviews and teachers made behavior ratings of 1,205 students. Based on results of the initial study wave, children were assigned to the ADHD high-risk group if they were previously diagnosed with ADHD, specifically suspected of having ADHD, or obtained elevated parent and teacher ADHD behavior ratings. The ADHD low-risk peers were participants without prior ADHD diagnosis or concerns whose behavior ratings were in the normal range. The study setting was a school district in North Florida containing an urban center and several smaller communities with rural characteristics. The treatment willingness study reported here was conducted between 2007 and 2009 as one of the longitudinal follow-up waves. The survey was completed by 309 participants, including 161 parents (59% response rate) and 148 adolescents (55% response rate). Numbers of responders, refusers, failures to reply, and total invited were as follows: parents (161/30/80/271), and adolescents (148/36/86/270). Adolescent age ranged from 14 years to 19 years (M = 16.5, SD = 1.30). Of the 148 adolescents, 97 (65.5%) were from the ADHD high risk group and 51 (34.5%) were low-risk peers. Almost all parent respondents were female (96%), 28% were African American, and most (52%) were in the 41-50 year age range, with an mean Hollingshead score of 40.8 (SD = 14.6); 108 (67.1%) parents had an adolescent in the ADHD high–risk group and 53 (32.9%) had an adolescent in the low-risk group. Further details about participant characteristics are provided in Table 1.
Table 1.
Respondent demographic characteristics
| Variables | Adolescents’ childhood ADHD status | Parents’ child’s ADHD status | ||||||
|---|---|---|---|---|---|---|---|---|
| High risk N = 97 |
Low risk N = 51 |
High risk N = 108 |
Low risk N = 53 |
|||||
| n | % | n | % | n | % | n | % | |
| Gender | ||||||||
| Female | 57 | 58.76% | 30 | 58.82% | 99 | 96.12% | 49 | 92.45% |
| Race | ||||||||
| White | 65 | 67.01% | 43 | 84.31% | 71 | 66.36% | 44 | 84.62% |
| African American /Other | 32 | 32.99% | 8 | 15.69% | 36 | 33.64% | 8 | 15.38% |
| Age | ||||||||
| <20 years old | 97 | 100% | 51 | 100% | - | - | - | - |
| 21-30 years old | - | - | - | - | ||||
| 1-40 years old | 33 | 31.13% | 4 | 7.69% | ||||
| 41-50 years old | 51 | 48.11% | 31 | 59.62% | ||||
| 51-60 years old | 20 | 18.87% | 17 | 32.69% | ||||
| >60 years old | 2 | 1.89% | 0 | 0% | ||||
| Socioeconomics | M | SD | M | SD | M | SD | M | SD |
| Hollingshead score | 43.34 | 12.68 | 36.37 | 14.40 | 37.70 | 14.19 | 47.13 | 13.56 |
Procedures
The Institutional Review Board at the University of Florida approved this study. Parental consent and child assent were obtained for all surveys completed by adolescents. Written informed consent was waived for all adult participants; instead, completion of the survey constituted consent. Parent and adolescent participants had the option of completing the survey questionnaire during a study visit conducted at a location of their choice, including home, research office or community library, or could receive the survey in the mail, complete it, and mail it back. Each respondent received a $15 gift card incentive upon survey completion.
Development of ADHD Treatment Perception Survey
The current survey research was embedded in a longitudinal mixed methods study of help-seeking and barriers to ADHD interventions. Interventions from three domains considered relevant for children with ADHD (health sector, academic and self-management) were chosen for survey inclusion through a sequential process including: (a) qualitative research aimed at identifying community academic practices through a sequence of longitudinal experience sampling and focus groups eliciting perspectives of adolescents, parents and teachers on helpful interventions; (b) literature review of health sector ADHD practice guidelines (Pliszka, 2007; Wolraich, et al., 2011) educational interventions and accommodations for ADHD (DuPaul, 2007), review of the available literature on self-management (Baverstock & Finlay, 2012; Berwid & Halperin, 2012; Konofal, et al., 2010; Millichap & Yee, 2012; Nigg, et al., 2012) and complementary and alternative medicine (CAM) (Sinha & Efron, 2005) for ADHD; and (c) survey pilot testing to confirm final item selection, adjust wording and improve item clarity. Through this process we selected 18 interventions (five from health sectors, seven from academic and six from self-management) that expanded upon solely research-based approaches to include interventions grounded in current community practice and elicited as helpful through our qualitative research strategies. Findings on the health sector and academic interventions are reported elsewhere (Bussing, et al., 2014; Bussing, Koro-Ljungberg, et al., 2012). The current report focuses on the six self-management interventions and examines respondents’ intervention willingness. To anchor survey responses, we developed a vignette describing a child with sufficient DSM-IV symptoms to qualify for an ADHD diagnosis, and respondents answered questions regarding the person in the vignette, which had male and female versions (fictitious names chosen were “Jennifer” and “Joseph”).
Survey items
The six self-management interventions were described to participants as follows (using the example of a female vignette): 1) activity outlets: Jennifer participates in activities that serve as energy outlets, such as sports, martial arts, ROTC (Reserve Officer Training Course), YMCA (Young Men’s Christian Association), or part-time jobs; 2) sleep regulation: Jennifer and her parents work on improving her sleep through improving sleep habits, like limiting daytime naps, enforcing regular bedtime, or restricting things that interfere with sleep (TV in room, caffeinated beverages after lunch time); 3) dietary restrictions: Jennifer or her parents restrict certain foods or sugar to improve her ADHD behavior; 4) homework help: The parent hires a homework coach/tutor in an effort to minimize conflicts between parent and teenager over school assignments; 5) family rules: To help improve Jennifer’s behavior, the family sets up clear rules, spells out consequences, and applies them consistently; and 6) prayer: Jennifer and her parents rely on prayer or spiritual practices to help with ADHD related problems. After reading the vignette, respondents rated each of the six treatments on separate 5-point scales (worded according to domain with 1 = not at all, 3 = moderately, 5 = very) for the following five domains: acceptability (e.g., 1 = not acceptable at all, 3 = moderately acceptable, 5 = very acceptable), perceived effectiveness/helpfulness, potential to be embarrassing (intended to represent a proxy for treatment stigma), likelihood of causing undesirable effects, and their self-rated level of knowledge about the treatment. Respondents indicated whether they had experienced the strategy personally (yes/no). Respondents rated their willingness to use a given intervention (1= not willing at all, 3= moderately willing, 5= very willing), and this rating served as dependent variables for our quantitative analyses.
Open-ended question
To enhance our understanding of potential concerns about self-management strategies, the ratings of embarrassment were followed by the open-ended question “What other undesirable effects are you concerned about?” and participants could write in their own responses, which were typed into an excel sheet as stated in their survey and utilized for the qualitative data analysis.
Sociodemographics
Information about respondent gender, race, age and socioeconomic status (SES) was obtained through survey questionnaires. SES scores were calculated using the Hollingshead 4-factor Index (Hollingshead, 1975).
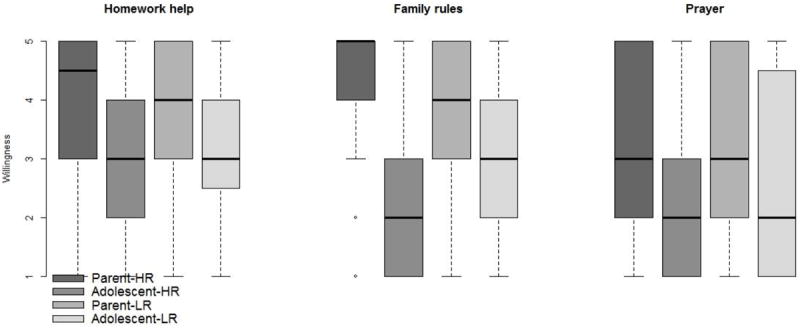
Variable construction and statistical analysis
To address Aim 1 we conducted a Kruskal-Wallis for each of the six dependent variables (i.e., ADHD self-management willingness) by our main independent predictor variable (i.e., four-level respondent type, indicating parent/adolescent and high/low ADHD risk status) followed by a multiple comparison procedure in the form of Bonferroni corrected Wilcoxon rank sum tests. We constructed box plots to display and compare the willingness data by respondent type. Box plots conventionally display the median (solid line), boxes depicting the lower (Q1) and upper (Q3) quartile, whiskers (minimum and maximum values within inner fences, defined as Q1, Q3 ±, 1.5* interquartile range), and identify outliers (open circle) that fall outside the inner fences. For Aim 2 we conducted logistic regression analyses for each of the six dependent variables, dichotomized as willing (score of 3, 4 or 5) or unwilling (score of 1 or 2). The independent variables included the potentially mutable perceptual variables (feeling knowledgeable, treatment acceptability, effectiveness, potential embarrassment, and undesirable effects), respondent type (four groups, indicating parent/adolescent and high/low ADHD risk, with high-risk adolescents serving as reference group), gender and race. All logistic regression models also adjusted for respondents’ past experience with intervention and SES. Our level of significance was set at .05; all hypothesis testing was two-sided. Analyses were performed using SAS (version 9.3; Cary, N.C.).
Qualitative data analysis
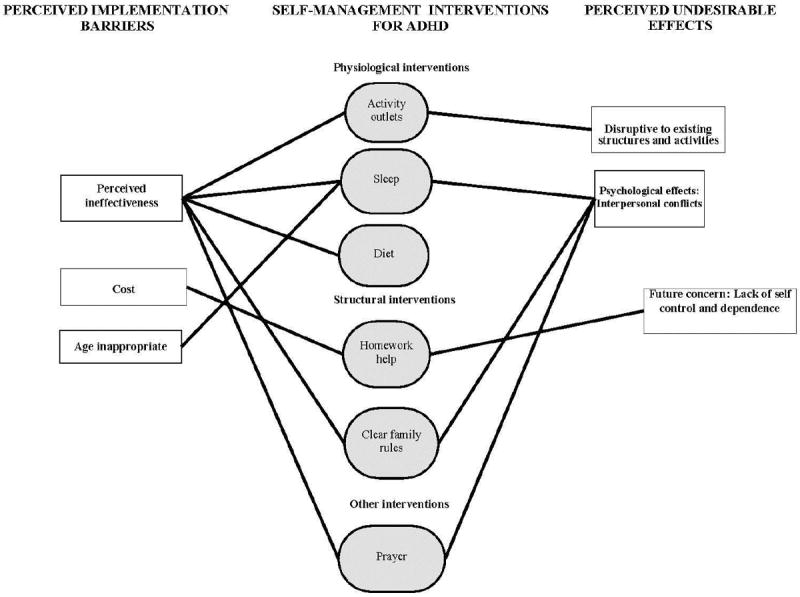
Constructivist theoretical perspective guided qualitative data analysis in this study. Constructivism enabled us to focus on individual meaning making processes, participants experiences and perceptions (see e.g., Crotty, 1998; Fosnot, 2005; Guba, 1990). The constructivist grounded Theory method was used to analyze open-ended survey responses. Grounded theory analysis was chosen because it enabled data reduction, across comparisons, and theorizing. Glaser (1978) defined grounded theory as “a detailed grounding by systematically analyzing data sentence by sentence by constant comparison as it is coded until a theory results” (Glaser, 1978) (p. 16). Furthermore, in grounded theory analysis various coding levels, constant comparison, and memo-ing are used to ensure that the resulting theory and the conclusions drawn from the data are grounded in the data (Charmaz, 2006). Consistent with this method, first, verbatim open-ended survey responses were typed into a database, read and open-coded. The code-book and codes were continuously revised, modified, and clarified by our multi-disciplinary coding team, resulting in 93 codes and categories. Examples of open codes were embarrassment, feeling different, disruptive to academics, or inconsistency. Next, we formed core categories and selective codes. All selective codes were constantly compared with each other with the intention of reducing and selecting them further to develop theoretical codes (Holton, 2007). The most prevalent theoretical codes were used to generate an integrated theoretical model of intervention concerns. The model illustrates perceived differences among different interventions and how the participants understood potential obstacles related to the use of the each self-management strategy. More specifically, model represents parent and adolescent perspectives together, distinguishing perceptions that function as implementation barriers (“why not start this intervention”) from concerns over unintended effects of ADHD self-management interventions (“undesirable effects after using intervention”) (see Figure 1).
Figure 1.
Results
Our theoretical model illustrates that our participants perceived implementation barriers to all self-management interventions (see Figure 1). In particular, all interventions except homework help were seen as potentially ineffective. Many parents and adolescents liked the idea of having homework help and they believed that a homework coach could improve educational outcomes. However, parents reported that costs associated with hiring the coach might prohibit them from using this intervention. Activity outlets, dietary restrictions, and clear family rules elicited concerns associated with perceived ineffectiveness without references to additional implementation barriers. Parents and adolescents worried that these interventions would not help yet would be hard to reinforce and follow through on. Sleep regulation was associated with two sets of implementation barriers. Interestingly, interventions related to sleep regulation were not only seen as ineffective but also as age inappropriate. Parents anticipated that forcing specific bed times on their teenagers would create too many conflicts, and thought it might work against adolescents’ biorhythms. Adolescents, in turn, noted that earlier bed times could cause insomnia and would make them feel treated like a child. Even though many parents and teens acknowledged the impact of prayer and religious/spiritual practices in their lives, study participants felt that prayer on its own would not be a sufficiently successful intervention. One parent exemplified this notion by stating that while prayer helps people, adolescents with ADHD need more than prayers.
Most interventions were also expected to have undesirable consequences. Parents thought that activity outlets could be disruptive to family schedules and dedicated study time. Adolescents, in turn, described how additional structured activities might single them out, make them overly tired, and interfere with school work. Three of the proposed self-management interventions were perceived to create interpersonal struggles between teenagers and their parents, as well as conflicts with peers. For example, sleep regulation and the use of prayer were seen as interventions leading to relationship conflicts. Similarly, many teenagers described how strongly reinforced family rules might distance adolescents from their families and incite rebellious behavior, yet might still not help teenagers to control their ADHD symptoms better. Some adolescents and parents expected that getting more homework help might impede adolescents’ development towards independence, self-control, and ability to differentiate right from wrong. Thus, the most frequently perceived unintended effect of homework help was reduced future self-reliance.
Because the qualitative data analysis indicated an integrated side effect model for parents and adolescents, we provide an unstratified quantitative summary of respondent perceptions regarding the six self-management strategies, as shown in Table 2. On average, respondents considered themselves at least moderately knowledgeable on most interventions, except dietary restrictions and homework help, and found all interventions at least moderately acceptable, with prayer achieving the lowest scores. Average anticipations of undesirable effects, including embarrassment resulting from interventions, were low across all six strategies. Respondents expected all but the prayer intervention to be at least moderately effective.
Table 2.
Odds ratios (OR) and 95% confidence intervals (95% CI) from multiple logistic regression predicting self-management willingness
| Activity outlets | Sleep regulation | Dietary restriction | Homework help | Family rules | Prayer | |||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
|
| ||||||||||||
| OR | (95% CI) | OR | (95% CI) | OR | (95% CI) | OR | (95% CI) | OR | (95% CI) | OR | (95% CI) | |
| Perceptions | ||||||||||||
| Knowledgeable | 1.63 | (1.01-2.64) | 1.56 | (1.08-2.24) | 1.42 | (0.99-2.02) | 1.73 | (1.22-2.45) | 1.22 | (0.87-1.72) | 1.84 | (1.28-2.64) |
| Acceptable | 1.79 | (1.06-3.01) | 1.55 | (1.06-2.28) | 2.15 | (1.51-3.06) | 2.26 | (1.55-3.31) | 1.60 | (1.05-2.44) | 1.65 | (1.09-2.50) |
| Embarrassing | 1.15 | (0.63-2.11) | 0.91 | (0.63-1.32) | 0.86 | (0.59-1.26) | 0.81 | (0.56-1.18) | 0.99 | (0.76-1.46) | 1.10 | (0.76-1.60) |
| Side effects | 0.76 | (0.43-1.34) | 0.60 | (0.38-0.92) | 0.90 | (0.61-1.32) | 0.59 | (0.40-0.87) | 0.63 | (0.44-0.89) | 0.51 | (0.34-0.75) |
| Effectiveness | 1.05 | (0.95-1.15) | 1.13 | (1.06-1.20) | 1.13 | (1.07-1.21) | 1.04 | (0.98-1.10) | 1.08 | (1.02-1.15) | 1.13 | (1.06-1.21) |
| Sociodemographics | ||||||||||||
| Parent -HR a | 2.66 | (0.70-10.42) | 3.75 | (1.45-9.72) | 6.79 | (2.53-18.23) | 4.40 | (1.67-11.62) | 10.76 | (3.42-33.79) | 1.80 | (0.68-4.79) |
| Parent - LR a | 2.48 | (0.50-12.42) | 7.77 | (1.50-40.36) | 15.93 | (4.12-61.66) | 2.98 | (0.99-9.01) | 5.10 | (1.54-16.88) | 3.57 | (1.13-11.28) |
| Adolescent -LR a | 3.04 | (0.52-17.87) | 3.19 | (1.22-8.33) | 3.06 | (1.18-7.97) | 1.37 | (0.51-3.67) | 1.15 | (0.48-2.79) | 0.84 | (0.28-2.48) |
| AA vs. Caucasian | 0.35 | (0.11-1.15) | 0.97 | (0.38-2.45) | 0.45 | (0.18-1.13) | 1.65 | (0.67-4.08) | 0.69 | (0.29-1.66) | 2.85 | (1.07-7.60) |
| Male vs. Female | 1.38 | (0.37-5.19) | 0.48 | (0.20-1.17) | 1.14 | (0.47-2.80) | 1.11 | (0.47-2.62) | 1.02 | (0.46-2.31) | 1.67 | (0.69-4.06) |
Notes. LR = Low ADHD Risk; HR = High ADHD Risk; AA = African American;
comparison group is Adolescent - HR; willingness dichotomized as as willing (score of 3, 4 or 5, indicating moderately to very willing) or unwilling (score of 1 or 2, indicating not at all to not willing); all analyses adjusted for respondent socioeconomic status and intervention experience; statistically significant OR indicated in bold
All of the six Kruskal-Wallis analyses were significant, p< .0001 except one (activity outlets), p=.0206. As hypothesized, we found that in the results of the pairwise Bonferroni corrected Wilcoxon rank sum comparisons, adolescents expressed significantly lower willingness than did parents for most ADHD self-management interventions. Exceptions were activity outlets where no differences were found between parent and adolescent except for the comparison of parents of at risk teens and the teens who were at risk (p = .0003). Furthermore, there were no differences found between parents whose teens were not at risk and teen groups for prayer. Lastly, as hypothesized, risk status was not associated with adolescent willingness of all interventions except sleep regulation (p= .0075). Box plots for the self-management willingness variables, stratified by respondent type and ADHD risk status, are displayed in Figures 2 and 3.
Figure 2.
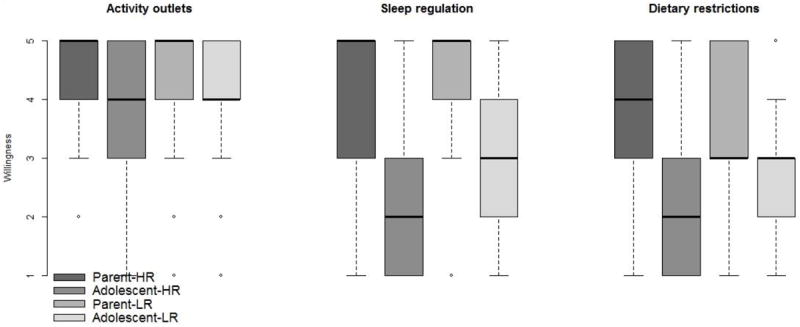
Figure 3.
As shown in more detail in Table 3, associations between self-management-use willingness and perceptions of the interventions occurred in the hypothesized direction, except that embarrassment was not linked to any of the willingness outcomes. Acceptability of interventions was associated with willingness for all six self-management strategies with odds ratios (ORs) ranging from 1.55 to 2.26. The remaining three predictors were associated with four of the six outcomes, with ORs for knowledge ranging from 1.22 to 1.84, and for effectiveness from 1.08 to 1.13. Expectations of side effects were negatively correlated with intervention willingness (ORs ranging from 0.51 to 0.63). The qualitative analysis results provide further content of the types of side effect concerns surrounding these self-management interventions.
Table 3.
Odds ratios (OR) and 95% confidence intervals (95% CI) from multiple logistic regression predicting self-management willingness
| Activity outlets | Sleep regulation | Dietary restriction | Homework help | Family rules | Prayer | |||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
|
| ||||||||||||
| OR | (95% CI) | OR | (95% CI) | OR | (95% CI) | OR | (95% CI) | OR | (95% CI) | OR | (95% CI) | |
| Perceptions | ||||||||||||
| Knowledgeable | 1.63 | (1.01-2.64) | 1.56 | (1.08-2.24) | 1.42 | (0.99-2.02) | 1.73 | (1.22-2.45) | 1.22 | (0.87-1.72) | 1.84 | (1.28-2.64) |
| Acceptable | 1.79 | (1.06-3.01) | 1.55 | (1.06-2.28) | 2.15 | (1.51-3.06) | 2.26 | (1.55-3.31) | 1.60 | (1.05-2.44) | 1.65 | (1.09-2.50) |
| Embarrassing | 1.15 | (0.63-2.11) | 0.91 | (0.63-1.32) | 0.86 | (0.59-1.26) | 0.81 | (0.56-1.18) | 0.99 | (0.76-1.46) | 1.10 | (0.76-1.60) |
| Side effects | 0.76 | (0.43-1.34) | 0.60 | (0.38-0.92) | 0.90 | (0.61-1.32) | 0.59 | (0.40-0.87) | 0.63 | (0.44-0.89) | 0.51 | (0.34-0.75) |
| Effectiveness | 1.05 | (0.95-1.15) | 1.13 | (1.06-1.20) | 1.13 | (1.07-1.21) | 1.04 | (0.98-1.10) | 1.08 | (1.02-1.15) | 1.13 | (1.06-1.21) |
| Sociodemographics | ||||||||||||
| Parent –HR a | 2.66 | (0.70-10.42) | 3.75 | (1.45-9.72) | 6.79 | (2.53-18.23) | 4.40 | (1.67-11.62) | 10.76 | (3.42-33.79) | 1.80 | (0.68-4.79) |
| Parent - LR a | 2.48 | (0.50-12.42) | 7.77 | (1.50-40.36) | 15.93 | (4.12-61.66) | 2.98 | (0.99-9.01) | 5.10 | (1.54-16.88) | 3.57 | (1.13-11.28) |
| Adolescent -LR a | 3.04 | (0.52-17.87) | 3.19 | (1.22-8.33) | 3.06 | (1.18-7.97) | 1.37 | (0.51-3.67) | 1.15 | (0.48-2.79) | 0.84 | (0.28-2.48) |
| AA vs. Caucasian | 0.35 | (0.11-1.15) | 0.97 | (0.38-2.45) | 0.45 | (0.18-1.13) | 1.65 | (0.67-4.08) | 0.69 | (0.29-1.66) | 2.85 | (1.07-7.60) |
| Male vs. Female | 1.38 | (0.37-5.19) | 0.48 | (0.20-1.17) | 1.14 | (0.47-2.80) | 1.11 | (0.47-2.62) | 1.02 | (0.46-2.31) | 1.67 | (0.69-4.06) |
Notes. LR = Low ADHD Risk; HR = High ADHD Risk; AA = African American;
comparison group is Adolescent - HR; willingness dichotomized as as willing (score of 3, 4 or 5, indicating moderately to very willing) or unwilling (score of 1 or 2, indicating not at all to not willing); all analyses adjusted for respondent socioeconomic status and intervention experience; statistically significant OR indicated in bold
Furthermore, as hypothesized, adolescents from the high risk cohort expressed less intervention willingness than did parents in the high risk cohort (except for activity outlets and prayer) and parents in the low risk cohort (except activity interventions and homework help). No significant willingness differences were observed between high-risk and low-risk adolescents except for sleep and diet interventions, with low-risk peers expressing higher willingness (OR 3.19, 95% CI [1.22-8.33] and OR 3.06, 95% CI [1.18-7.97], respectively). Lastly, as hypothesized, being African American was associated with higher odds of prayer willingness (OR 2.85, 95% CI [1.07-7.60]). Gender was not associated with willingness differences for any interventions. SES characteristics and past self-management experience were not independently associated with willingness to use self-management interventions in the multiple logistic regression analysis with one exception, namely, past experience with activity outlets lowered the odds of intervention willingness (OR 0.19, 95% CI [0.05-0.65]).
Discussion
As expected, parents and adolescent differed significantly in their willingness to engage in various self-management practices for ADHD, with adolescents less receptive than parents, except for adding activity outlets to their daily routines. Furthermore, sleep and dietary self-management practices stood out as particularly unpopular among adolescents with high ADHD risk. These findings have relevance to clinicians treating adolescents with ADHD as well as implications for researchers seeking to develop empirically supported self-management programs.
Clinicians generally do not “prescribe” ADHD self-management, but may offer psychoeducation informed by emerging evidence or expert consensus, for example, on sleep hygiene (Weiss, et al., 2006) or dietary practices (Millichap & Yee, 2012). Our study results suggest that implementing such strategies could easily increase conflicts between parents/caregivers and their adolescents with ADHD. Clinicians therefore should elicit differing willingness and concerns surrounding sleep or diet strategies and assist families in resolving them beforehand. In view of the high prevalence of sleep complaints in patients with ADHD (Owens, 2008), development of effective, acceptable sleep interventions appears particularly needed. Our study findings have several implications for intervention developers. First, in the current study, the wording for sleep intervention examples focused on restrictions (e.g., sleep-impairing foods/beverages) and diminished adolescent decision-making power (e.g., about bedtime or naps). The “restrictive” wording was derived from community-based focus groups, but had the survey emphasized choices and teen decision input for sleep interventions, adolescents with ADHD might have expressed more willingness to use them. Emphasis on restriction might also explain the willingness difference between high- and low-risk adolescents for sleep and dietary interventions; low-risk adolescents were more receptive because the “restrictions” would not affect them personally, only the group at high risk for ADHD. Secondly, developers of sleep interventions can take into account the qualitative study results showing concerns about developmental appropriateness (adolescent bio-rhythms, fear of iatrogenic insomnia, feeling treated like a young child) to optimize intervention compatibility for both parents and adolescents.
Activity-based ADHD interventions were acceptable across all demographic and ADHD risk groups. The range of activity examples was broad, including physical exercise, but also structured social participation in ROTC, YMCA, or part-time jobs. Of these activity intervention examples, physical exercise is particularly promising because emerging research suggests therapeutic benefits for youth with ADHD (Berwid & Halperin, 2012; Rommel, Halperin, Mill, Asherson, & Kuntsi, 2013). Future research still needs to establish whether exercise interventions can produce clinically relevant improvements in ADHD symptoms, functional impairment and relevant social outcomes. Until that point is reached, the addition of activity outlets for adolescents with ADHD appears to be a well-accepted self-management practice as long as potential disruption of family and school schedules can be minimized.
As hypothesized, African American respondents expressed higher willingness to use prayer as ADHD intervention for adolescents than did European Americans. Previous research had shown that African American parents were more likely than European American parents to turn to religion as a way to help their child with behavioral and emotional problems (Bussing, et al., 2006). This is consistent with high levels of involvement in organized religion in Southern African American families, but may also reflect their less medically influenced explanatory model of the causation of ADHD. Several previous studies have documented racial/ethnic differences in beliefs about the etiology of ADHD (Bussing, Zima, et al., 2012; Yeh, Hough, McCabe, Lau, & Garland, 2004). However, overall perceptions of the effectiveness of prayer for ADHD were low, exemplified by the notion that prayer helps but is not enough.
As posited, self-management willingness was positively correlated with perceptions of acceptability and effectiveness. Thus, uptake of promising interventions could potentially be increased by targeted social interventions, such as news coverage or specific social media campaigns (Hamm et al., 2014). However, presently ADHD self-management interventions require further development and efficacy testing before proposing more wide-spread dissemination efforts. In contrast to other chronic conditions, best exemplified by diabetes mellitus (Funnell et al., 2010), self-management for ADHD has not risen to an empirical level with national standards and certified educators. Of note, even though study participants overall endorsed low anticipation of undesirable effects, expectations of side effects significantly was negatively correlated with willingness to engage in self-management. However, embarrassment (intended as proxy for stigma perceptions) did not impede intervention willingness for any of the six self-management strategies. We question whether this finding may be the result of word choice for the survey (embarrassment instead of stigma), or whether self-management practices (which are private by nature) are less subject to stigma perceptions than interventions in the school or health sector (which involve official records), where stigma was identified as significant concern (Bussing, et al., 2014; Bussing, Koro-Ljungberg, et al., 2012; Bussing, Zima, Mason, Porter, & Garvan, 2011). Our qualitative analysis provided valuable insights into concerns that may need to be addressed during development of acceptable self-management curricula for chronic care models, namely cost, disruptiveness to daily routines, creation of interpersonal conflict, and interference with the development of self-reliance.
The study findings must be considered in the context of some limitations, most notably sampling, geographic, and participation rates. Our sample is representative of a school district in a Southeastern US, and due to school district demographic characteristics, includes only Caucasian and African American adolescents and precludes conclusions about other racial/ethnic groups. Findings are further limited by participation rates, even though they exceed those of many other available surveys of parents and adolescents. Because our survey did not allow further probing, the qualitative data analysis was limited by occasional brevity of responses and by our inability to clarify or elaborate on responses with participants. Even though most of the open-ended survey responses were well crafted, and many participants wrote sentences or whole paragraphs, the interpretation of some responses could have benefitted from better contextualization and additional background information. Lastly, the self-management strategies included in this paper were selected based on their use in the community, as elicited during qualitative research efforts of this mixed methods study, and do not represent empirically validated interventions, nor do they include self-management strategies that might be employed in other community settings.
To conclude, our study contributes important new findings to the emerging literature on intervention perceptions surrounding mental health self-management strategies. Our multi-perspective design shows significant discrepancies between adolescents’ and adults’ willingness to use common ADHD self-management strategies, with low adolescent willingness for all interventions except increasing activity outlets. Findings highlight the need to develop engaging and effective self-management practices for adolescents with ADHD and their families. Adolescents’ viewpoints must be elicited as interventions may be acceptable to adults, but resisted by adolescents. Activity-based ADHD interventions appear particularly acceptable across all demographic and risk groups.
Acknowledgments
The authors thank the parents, adolescents, teachers and health professionals whose participation made the study possible. This study was supported by grant RO1MH57399 from the National Institute of Mental Health.
Contributor Information
Regina Bussing, Department of Psychiatry, University of Florida, Gainesville, FL.
Dana Mason, Department of Psychiatry, University of Florida, Gainesville, FL.
Cynthia Wilson Garvan, Department of Health Care Environments and Systems, University of Florida, Gainesville, FL.
Tina Gurnani, Child & Adolescent Psychiatry, Department of Psychiatry, Mount Sinai St. Luke’s, New York, NY.
Mirka Koro-Ljungberg, Mary Lou Fulton College, Arizona State University, Phoenix, AZ.
Kenji Noguchi, Department of Psychology, University of Southern Mississippi Gulf Coast, Long Beach, MS.
Dolores Albarracin, Deparment of Psychology, Liberal Arts and Sciences, and Department of Business Administration, College of Business, University of Illinois, Champaign, IL.
References
- Baverstock A, Finlay F. Faith healing in paediatrics: what do we know about its relevance to clinical practice? Child: care, health and development. 2012;38(3):316–320. doi: 10.1111/j.1365-2214.2011.01284.x. Review. [DOI] [PubMed] [Google Scholar]
- Berwid OG, Halperin JM. Emerging support for a role of exercise in attention-deficit/hyperactivity disorder intervention planning. Current psychiatry reports. 2012;14(5):543–551. doi: 10.1007/s11920-012-0297-4. Research Support, N.I.H., Extramural Review. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bodenheimer T, Wagner EH, Grumbach K. Improving primary care for patients with chronic illness. JAMA. 2002a;288(14):1775–1779. doi: 10.1001/jama.288.14.1775. Research Support, Non-U.S. Gov’t. [DOI] [PubMed] [Google Scholar]
- Bodenheimer T, Wagner EH, Grumbach K. Improving primary care for patients with chronic illness: the chronic care model, Part 2. JAMA. 2002b;288(15):1909–1914. doi: 10.1001/jama.288.15.1909. [DOI] [PubMed] [Google Scholar]
- Brown RT, Amler RW, Freeman WS, Perrin JM, Stein MT, Feldman HM, Wolraich ML, et al. Treatment of attention-deficit/hyperactivity disorder: overview of the evidence. Pediatrics. 2005;115(6):e749–757. doi: 10.1542/peds.2004-2560. Review. [DOI] [PubMed] [Google Scholar]
- Bussing R, Koro-Ljungberg M, Gagnon JC, Mason DM, Ellison A, Noguchi K, Albarracin D, et al. Feasibility of School-Based ADHD Interventions: A Mixed-Methods Study of Perceptions of Adolescents and Adults. Journal of attention disorders. 2014 doi: 10.1177/1087054713515747. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bussing R, Koro-Ljungberg M, Noguchi K, Mason D, Mayerson G, Garvan CW. Willingness to use ADHD treatments: a mixed methods study of perceptions by adolescents, parents, health professionals and teachers. Social science & medicine. 2012;74(1):92–100. doi: 10.1016/j.socscimed.2011.10.009. Research Support, N.I.H., Extramural. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bussing R, E K-L M, Williamson P, Gary FA, Wilson Garvan C. What “Dr. Mom” ordered: a community-based exploratory study of parental self-care responses to children’s ADHD symptoms. Social science & medicine. 2006;63(4):871–882. doi: 10.1016/j.socscimed.2006.03.014. Research Support, N.I.H., Extramural. [DOI] [PubMed] [Google Scholar]
- Bussing R, Mason DM, Bell L, Porter P, Garvan C. Adolescent outcomes of childhood attention- deficit/hyperactivity disorder in a diverse community sample. Journal of the American Academy of Child and Adolescent Psychiatry. 2010;49(6):595–605. doi: 10.1016/j.jaac.2010.03.006. Research Support, N.I.H., Extramural. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bussing R, Zima BT, Mason DM, Meyer JM, White K, Garvan CW. ADHD knowledge, perceptions, and information sources: perspectives from a community sample of adolescents and their parents. The Journal of adolescent health : official publication of the Society for Adolescent Medicine. 2012;51(6):593–600. doi: 10.1016/j.jadohealth.2012.03.004. Research Support, N.I.H., Extramural. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bussing R, Zima BT, Mason DM, Porter PC, Garvan CW. Receiving treatment for attention-deficit hyperactivity disorder: do the perspectives of adolescents matter? The Journal of adolescent health : official publication of the Society for Adolescent Medicine. 2011;49(1):7–14. doi: 10.1016/j.jadohealth.2010.08.014. Research Support, N.I.H., Extramural. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chan E. The role of complementary and alternative medicine in attention-deficit hyperactivity disorder. Journal of developmental and behavioral pediatrics : JDBP. 2002;23(1 Suppl):S37–45. doi: 10.1097/00004703-200202001-00007. Review. [DOI] [PubMed] [Google Scholar]
- Charach A, Fernandez R. Enhancing ADHD medication adherence: challenges and opportunities. Current psychiatry reports. 2013;15371(7) doi: 10.1007/s11920-013-0371-6. Research Support, Non-U.S. Gov’t Review. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Charmaz K. Constructing grounded theory: A practical guide through qualitative analysis. Thousand Oaks, CA: Pine Forge Press; 2006. [Google Scholar]
- Crotty M. The foundations of social research. London: Sage; 1998. [Google Scholar]
- DuPaul GJ. School-based interventions for students with attention deficit hyperactivity disorder: current status and future directions. School Psychology Review. 2007;36(2):183–194. [Google Scholar]
- Evans SW, Owens JS, Bunford N. Evidence-based psychosocial treatments for children and adolescents with attention-deficit/hyperactivity disorder. Journal of clinical child and adolescent psychology : the official journal for the Society of Clinical Child and Adolescent Psychology, American Psychological Association, Division 53. 2014;43(4):527–551. doi: 10.1080/15374416.2013.850700. Research Support, Non-U.S. Gov’t Review. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fosnot C, editor. Constructivism: Theory, perspectives, and practice. 2. New York: Teachers College Press; 2005. [Google Scholar]
- Funnell MM, Brown TL, Childs BP, Haas LB, Hosey GM, Jensen B, Weiss MA, et al. National standards for diabetes self-management education. Diabetes care. 2010;33(Suppl 1):S89–96. doi: 10.2337/dc10-S089. Research Support, N.I.H., Extramural Review. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Glaser BG. Advances in methodology of grounded theory. Mill Valley, CA: Sociological Press; 1978. [Google Scholar]
- Guba E, editor. The paradigm dialog. Newbury Park, CA: Sage; 1990. [Google Scholar]
- Gureasko-Moore S, Dupaul GJ, White GP. The effects of self-management in general education classrooms on the organizational skills of adolescents with ADHD. Behavior modification. 2006;30(2):159–183. doi: 10.1177/0145445503259387. [DOI] [PubMed] [Google Scholar]
- Hamm MP, Shulhan J, Williams G, Milne A, Scott SD, Hartling L. A systematic review of the use and effectiveness of social media in child health. BMC pediatrics. 2014;14:138. doi: 10.1186/1471-2431-14-138. Research Support, Non-U.S. Gov’t. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hollingshead AB. Four Factor Index of social class. Yale University; New Haven, CT: 1975. [Google Scholar]
- Holton JA. The coding process and its challenges. In: C K, Bryant A, editors. The Sage Handbook of Grounded Theory. London: Sage Publications; 2007. pp. 265–289. [Google Scholar]
- Konofal E, Lecendreux M, Cortese S. Sleep and ADHD. Sleep medicine. 2010;11(7):652–658. doi: 10.1016/j.sleep.2010.02.012. Review. [DOI] [PubMed] [Google Scholar]
- Lara C, Fayyad J, de Graaf R, Kessler RC, Aguilar-Gaxiola S, Angermeyer M, Sampson N, et al. Childhood predictors of adult attention-deficit/hyperactivity disorder: results from the World Health Organization World Mental Health Survey Initiative. Biological psychiatry. 2009;65(1):46–54. doi: 10.1016/j.biopsych.2008.10.005. Research Support, N.I.H., Extramural Research Support, Non-U.S. Gov’t Research Support, U.S. Gov’t, P.H.S. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Leggett C, Hotham E. Treatment experiences of children and adolescents with attention-deficit/hyperactivity disorder. Journal of paediatrics and child health. 2011;47(8):512–517. doi: 10.1111/j.1440-1754.2011.02013.x. [DOI] [PubMed] [Google Scholar]
- Lucock M, Gillard S, Adams K, Simons L, White R, Edwards C. Self-care in mental health services: a narrative review. Health & social care in the community. 2011;19(6):602–616. doi: 10.1111/j.1365-2524.2011.01014.x. Review. [DOI] [PubMed] [Google Scholar]
- Millichap JG, Yee MM. The diet factor in attention-deficit/hyperactivity disorder. Pediatrics. 2012;129(2):330–337. doi: 10.1542/peds.2011-2199. Review. [DOI] [PubMed] [Google Scholar]
- Nigg JT, Lewis K, Edinger T, Falk M. Meta-analysis of attention-deficit/hyperactivity disorder or attention-deficit/hyperactivity disorder symptoms, restriction diet, and synthetic food color additives. Journal of the American Academy of Child and Adolescent Psychiatry. 2012;51(1):86–97 e88. doi: 10.1016/j.jaac.2011.10.015. Meta-Analysis Research Support, Non-U.S. Gov’t. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Owens JA. Sleep disorders and attention-deficit/hyperactivity disorder. Current psychiatry reports. 2008;10(5):439–444. doi: 10.1007/s11920-008-0070-x. Review. [DOI] [PubMed] [Google Scholar]
- Parker DR, Hoffman SF, Sawilowsky S, Rolands L. Self-control in postsecondary settings: students’ perceptions of ADHD college coaching. Journal of attention disorders. 2013;17(3):215–232. doi: 10.1177/1087054711427561. Research Support, Non-U.S. Gov’t. [DOI] [PubMed] [Google Scholar]
- Pliszka S. Practice parameter for the assessment and treatment of children and adolescents with attention-deficit/hyperactivity disorder. Journal of the American Academy of Child and Adolescent Psychiatry. 2007;46(7):894–921. doi: 10.1097/chi.0b013e318054e724. Practice Guideline Review. [DOI] [PubMed] [Google Scholar]
- Rommel AS, Halperin JM, Mill J, Asherson P, Kuntsi J. Protection from genetic diathesis in attention-deficit/hyperactivity disorder: possible complementary roles of exercise. Journal of the American Academy of Child and Adolescent Psychiatry. 2013;52(9):900–910. doi: 10.1016/j.jaac.2013.05.018. Research Support, Non-U.S. Gov’t Review. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sawyer MG, Rey JM, Arney FM, Whitham JN, Clark JJ, Baghurst PA. Use of health and school-based services in Australia by young people with attention-deficit/hyperactivity disorder. Journal of the American Academy of Child and Adolescent Psychiatry. 2004;43(11):1355–1363. doi: 10.1097/01.chi.0000138354.90981.5b. Research Support, Non-U.S. Gov’t. [DOI] [PubMed] [Google Scholar]
- Sciberras E, Fulton M, Efron D, Oberklaid F, Hiscock H. Managing sleep problems in school aged children with ADHD: a pilot randomised controlled trial. Sleep medicine. 2011;12(9):932–935. doi: 10.1016/j.sleep.2011.02.006. Randomized Controlled Trial. [DOI] [PubMed] [Google Scholar]
- Sinha D, Efron D. Complementary and alternative medicine use in children with attention deficit hyperactivity disorder. Journal of paediatrics and child health. 2005;41(1-2):23–26. doi: 10.1111/j.1440-1754.2005.00530.x. [DOI] [PubMed] [Google Scholar]
- Van Cleave J, Leslie LK. Approaching ADHD as a chronic condition: implications for long-term adherence. Pediatric annals. 2008;37(1):19–26. doi: 10.3928/00904481-20080101-07. Case Reports Review. [DOI] [PubMed] [Google Scholar]
- Weiss MD, Wasdell MB, Bomben MM, Rea KJ, Freeman RD. Sleep hygiene and melatonin treatment for children and adolescents with ADHD and initial insomnia. Journal of the American Academy of Child and Adolescent Psychiatry. 2006;45(5):512–519. doi: 10.1097/01chi.0000205706.78818.ef. Comparative Study Randomized Controlled Trial Research Support, Non-U.S. Gov’t. [DOI] [PubMed] [Google Scholar]
- WHO. Health education in self-care: possibilities and limitations. Geneva: The World Health Organization; 1984. [Google Scholar]
- Wolraich M, Brown L, Brown RT, DuPaul G, Earls M, Feldman HM, Visser S, et al. ADHD: clinical practice guideline for the diagnosis, evaluation, and treatment of attention-deficit/hyperactivity disorder in children and adolescents. Pediatrics. 2011;128(5):1007–1022. doi: 10.1542/peds.2011-2654. Practice Guideline Research Support, Non-U.S. Gov’t. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Yeh M, Hough RL, McCabe K, Lau A, Garland A. Parental beliefs about the causes of child problems: exploring racial/ethnic patterns. Journal of the American Academy of Child and Adolescent Psychiatry. 2004;43(5):605–612. doi: 10.1097/00004583-200405000-00014. Research Support, U.S. Gov’t, P.H.S. [DOI] [PubMed] [Google Scholar]


