Abstract
AIM: To study the expression of neurokinin-1 receptor (NK-1R) and neurokinin-2 receptor (NK-2R) in distal ileum of acute necrotizing pancreatitis (ANP) and to evaluate the relationship between expression of these two receptors and intestinal mucosal damage.
METHODS: A total of 130 adult Sprague-Dawley rats were randomly divided into two groups: the rats in ANP group (n = 80) were induced by the retrograde intraductal infusion of 30 g·L-1 sodium taurocholate. And the rats in normal control group (n = 50) received laparotomy only. Sacrifices were made 6 h, 12 h, 24 h and 48 h later in ANP and normal control group after induction respectively. Intestinal mucosal permeability was studied by intrajejunal injection of 1.5mCi radioactive isotope 99mTc-diethlene triamine pentacetic acid (DTPA) and the radioactivity of 99mTc-DTPA content in urine was measured 6 h, 12 h, 24 h and 48 h after induction. Then the pancreas and intestine were prepared for pathology. Reverse transcription polymerase chain reaction (RT-PCR) was used to determine the mRNA expression of NK-1R and NK-2R, and Western blot was used to investigate the protein level of NK-1R and NK-2R.
RESULTS: In ANP rats, serious histologic damages in intestinal mucosa were observed, and the radioactivity of 99mTc-DTPA in urine increased significantly in the ANP group. RT-PCR revealed that NK-1R and NK-2R mRNA level was overexpressed in the distal ileum of ANP as compared with the normal control group. Western blot discovered stronger NK-1R (14-fold increase) and NK-2R (9-fold increase) immunoreactivity in the intestinal mucosa of ANP rats. Moreover, the overexpression of NK-1R was associated with mucosal pathological score (r = 0.77, P < 0.01) and intestinal permeability (r = 0.68, P < 0.01) in ANP rats.
CONCLUSION: NK-1R and NK-2R contribute to disrupted neuropeptides loop balance, deteriorate intestinal damage, and are involved in pathophysiological changes in ANP.
INTRODUCTION
Acute necrotizing pancreatitis (ANP) has a complicated and ill-defined pathophysiology. It is associated with a high complication rate and unpredictable outcom, with a mortality rate of 10%-45%[1]. The hypothesis that ANP promotes bacterial translocation, leading to infection in the inflamed pancreas and peripancreatic tissue, has been studied in rats fed with fluorescent beads, sensitive inert markers of translocation[2]. The results suggested a translocated bacteria route for pancreatic infection. Normal intestinal mucosal barrier can keep the bacteria from translocation, however, this barrier is damaged in ANP[3,4]. The mechanism, which leads to the dysfunction of mucosal barrier, remains unclear[5-9].
Recent studies have revealed the important role of Substance P (SP) and its receptors in ANP[10-13]. However, the expression of SP’s two receptors-neurokinin-1 receptor (NK-1R) and neurokinin-2 receptor (NK-2R) in intestinal mucosa of ANP, remains unclear. And their roles in mucosal damage has not been revealed.
Therefore, in the present study the mRNA of NK-1R and NK-2R in intestinal mucosa of ANP was analyzed using reverse transcription polymerase chain reaction (RT-PCR), the protein level of these two receptors was analyzed by Western blot. And the relationship between mRNA level and intestinal mucosal damage/intestinal permeability was also investigated.
MATERIALS AND METHODS
Animals
Adult Sprague-Dawley rats weighing 250-300 g were obtained from the Laboratory Animal Center of Southeast University, and fed with standard rat chow. Animals were fasted overnight and anesthetized with 20 g·L-1 sodium pentobarbital (intraperitoneal injection). ANP models (n = 80) were induced by the retrograde intraductal infusion of 30 g·L-1 sodium taurocholate (0.1 ml·min-1·kg-1). And the rats in normal control group (n = 50) received laparotomy, the duodenum was taken out of the abdominal cavity and the pancreas was turned over for three times.
Sacrifices were made 6 h, 12 h, 24 h and 48 h later in ANP and normal control group after induction respectively. The distal ileum, pancreas and blood in portal vein were obtained for further studies. Freshly removed tissue samples were immediately fixed in paraformaldehyde solution for 12-24 hours and paraffin-embedded for routine histopathologic analysis. Concomitantly, tissue samples destined for RNA and protein extraction were immediately snap-frozen in liquid nitrogen and maintained at -80 °C until use. Blood was obtained for serum amylase determinations.
Pathological examination for intestinal mucosa and pancreas
Paraffin-embedded tissue sections (2-3 mm thick) were subjected to hematoxylin & eosin staining. Intestinal mucosal damage was evaluated blindly under microscope by two pathologists[14,15].
Determinatins of intinstinal mucosal permeability
Intestinal mucosal permeability was investigated by intrajejunal injection of 1.5 mCi radioactive isotope 99mTc (Chinese Institute of Nuclear Power)-diethlene triamine pentacetic acid (DTPA, Chinese Institute of Nuclear Power) and the radioactivity of 99mTc-DTPA content in urinary were measured 6 h, 12 h, 24 h and 48 h after induction. Urinary volume was measured and radioactive impulse was determined using radio-immunity γ counter. Intestinal mucosal permeability was calculated using the following formula: Intestinal mucosal permeability (%) = 99mTc-DTPA excretory rate (%) = [(urine-background) × volume]/(sdandard-background) × 100%[16,17].
RNA extraction and RT-PCR
Total RNA was extracted using the single-step guanidinium isothiocyanate method, as previously reported[18,19]. Following DNAse treatment, total RNA was reversely transcribed into cDNA using random hexamers according to the manufacturer’s instructions (Roche Diagnostics, Rotkreuz, Switzerland). The primers were designed using Primer Express software (Germany) and synthesized by Amplimmun (Amplimmun AG, Madulain, Switzerland). The sequence is shown in Table 1.
Table 1.
The sequence of primers used for RT-PCR
| Primers | Sequence | Primer size (bp) | PCR products size (bp) |
| NK-1R | |||
| Forward primer | 5'-CAT CAA CCC AGA TCT CTA CC-3' | 20 | 380 |
| Reverse primer | 5'-GCT GGA GCT TTC TGT CAT GGA-3' | 21 | |
| NK-2R | |||
| Forward primer | 5'-CAT CAC TGT GGA CGA GGG GG-3' | 20 | 491 |
| Reverse primer | 5'-TGT CTT CCT CAG TTG GTG TC-3' | 20 | |
| GAPDH | |||
| Forward primer | 5'-TGA AGG TCG GTG TCA ACG GAT TTG GC-3' | 26 | 999 |
| Reverse primer | 5'-CAT GTA GGC CAT GAG GTC CAC CAC-3' | 24 | |
PCR amplification was carried out using either NK-1R or NK-2R or GAPDH in a final volume of 25 μl with a Perkin-Elmer GeneAmp System 9700 and 0.625 U of Taq DNA polymerase (Roche Diagnostics GmbH, Mannheim, Germany). Cycling conditions were as follows: 35 cycles of denaturation at 94 °C for 1 min, annealing at 62 °C for 1 min and elongation at 72 °C for 2.5 min. The first PCR cycle was preceded by denaturation at 94 °C for 3 min, and last PCR cycle was followed by incubation at 72 °C for 10 min.
For each PCR reaction, an identical tube containing the same amount of regent, and same amount of water was substituted for cDNA in these tubes. These tubes served as negative control of PCR.
RNA concentrations and PCR were titrated to establish standard curves to document linearity and to permit semiquantitative analysis of signal strength[20-22]. Amplified PCR products were separated by electrophoresis through a 1% agarose gel at 45 V for 120 min. The cDNA bands were visualized by ultraviolet illumination after the gels were stained with 0.5 g·L-1 ethidium bromide dissolved in Tris-borate-EDTA buffer (89 mM Tris, 89 mM boric acid, 2.5 mM EDTA, pH8.2). The gels were photographed, and the films were scanned and analyzed with a computerized densitometer (Image-Pro Plus, Version 3.0.01).
Western blot
Western blot for NK-1R and NK-2R was performed as previously reported with certain modifications[18,19]. Briefly, 200 mg of tissue samples were powered in liquid nitrogen and then homogenized in lysis buffer (50 mM Tris-HCl, pH7.5, 150 mM NaCl, 2 mM EDTA, 1% SDS) supplemented with a protease inhibitor cocktail (Roche Diagnostics, Rotkreuz, Switzerland). The lysate was collected and centrifuged at 4 °C for 10 min with 14000 rpm to remove the insoluble material. The protein concentration was measured by spectrophotometry using the BCA protein assay (Pierce, Rockford, IL, USA). For each sample, 40 mg of protein was separated on 12% SDS-polyacrylamide gels and electroblotted onto nitrocellulose membranes.
The blots were incubated in blocking solution (50 g·L-1 non-fat milk in 20 mM Tris-HCl, 150 mM NaCl, 1 g·L-1 Tween-20 [TBS-T]), followed by incubation with 1:1000 dilution of goat anti-rat NK-1R antibody (Santa Cruz Biotechnology, Santa Cruz, CA, USA) or 1:1000 dilution of goat anti-rat NK-2R antibody (Santa Cruz Biotechnology, Santa Cruz, CA, USA) at 4 °C overnight. The membranes were then washed with TBS-T and incubated with donkey anti-goat IgG (1:3000 dilution) for 60 min at room temperature. Antibody detection was performed with an enhanced chemiluminescence reaction (ECL Western blotting detection, Amersham Life Science, Amersham, UK).
Statistical analysis
Results were expressed as mean ± SD. Statistical analysis was made using the Prism software (Prism, GraphPad Software Inc., San Diego, CA, USA). The comparative statistical evaluations among groups were done using the Mann-Whitney U test or Chi-square test. Spearmann correlation analysis was used for correlation analysis of the parameters. Significance was defined as P < 0.05.
RESULTS
Serum amylase and pathological examination
Serum amylase increased significantly in ANP group as compared with normal controls (P < 0.01). The diagnoses of ANP were confirmed by gross appearance and microscopy. In ANP group, mucosal edema, epithelia degeneration, necrosis or even abscission were observed after 6 h. Hemangiectasia, hemorrhage and inflammatory cell infiltration were revealed in mucosa or submucosa (Table 2).
Table 2.
The pathological score of intestinal mucosa
| Groups | 0 h | 6 h | 12 h | 24 h | 48 h |
| Control | 0.92 ± 0.47 | 0.90 ± 0.35 | 0.93 ± 0.38 | 0.93 ± 0.29 | 1.07 ± 0.36 |
| ANP | 2.11 ± 0.47a | 2.65 ± 0.49b | 3.91 ± 0.82b | 4.89 ± 1.21b |
P < 0.05 vs each time point of control group, respectively;
P < 0.01 vs each time point of control group, respectively
Intestinal mucosal permeability change in ANP rats
The intestinal mucosal permeability was determined using isotope. The results revealed that permeability increased significantly after 6 h (Table 3).
Table 3.
Changes of intestinal mucosal permeability
| Groups | 0 h | 6 h | 12 h | 24 h | 48 h |
| Control | 0.0411 ± 0.0156 | 0.0455 ± 0.0174 | 0.0532 ± 0.0188 | 0.0693 ± 0.0153 | 0.0698 ± 0.0223 |
| ANP | 0.2367 ± 0.1132a | 0.3457 ± 0.0473a | 0.6651 ± 0.1411a | 0.7021 ± 0.1523a |
P < 0.01 vs each time point of control group, respectively
mRNA expression of NK-1R and NK-2R in distal ileum
The rats were sacrified 6 h, 12 h, 24 h or 48 h after model inducing, distal ileum was obtained for determination of NK-1R and NK-2R mRNA. Figure 1 shows the amplification plot at the time point of 6 h. The gene above had been amplified effectively, and amplification of GAPDH was comparable in each sample, which suggested comparable mRNA in each sample (Figure 1B, Figure 1D), whereas amplification of NK-1R in normal controls was so weak that some of the samples could only been observed in the gel. In contrast, the amplification of NK-1R in ANP group was relatively stronger (Figure 1A). The expression of NK-2R was similar to NK-1R (Figure 1C). After 12 h, 24 h or 48 h, the expression of above genes maintained the same pattern as before.
Figure 1.
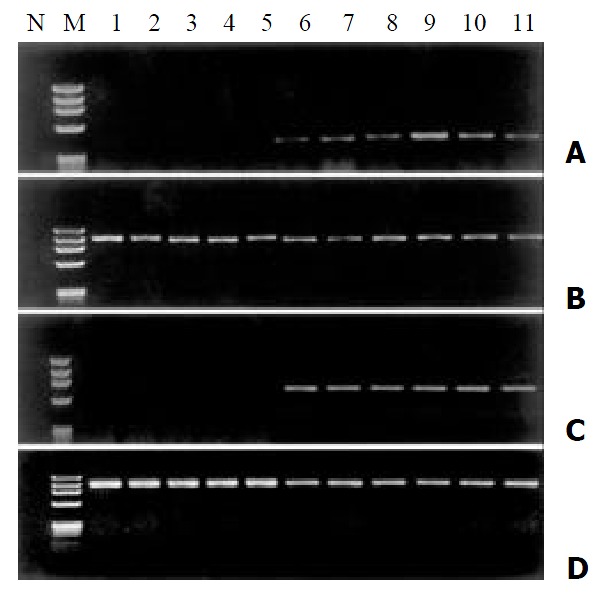
Amplification results of NK-1R, NK-2R and GAPDH from RT-PCR in control and ANP intestinal tissue. A: amplifi-cation results of NK-1R; C: amplification results of NK-2R; B, D: amplification results of GAPDH. N: PCR negative control; M: PCR Marker (upper to lower: 1000, 800, 600, 400, 200 and 100 bp); 1-5: group of normal control; 6-11: group of ANP
Correlation of expression of NK-1R and NK-2R with intestinal mucosal damage
We then evaluated whether there was a relationship between the expression levels of these two genes and intestinal mucosal pathological score and permeability. A significant relationship between NK-1R mRNA and mucosal pathological score (r = 0.77, P < 0.01) was found (Figure 2A). Furthermore, statistical analysis revealed a significant relationship between NK-1R mRNA and mucosal permeability (r = 0.68, P < 0.01, Figure 2B). Although NK-2R mRNA was overexpressed in ANP, there was no significant relationship between this gene expression and intestinal mucosal pathological score (r = 0.32, P = 0.31) and permeability (r = 0.28, P = 0.21).
Figure 2.
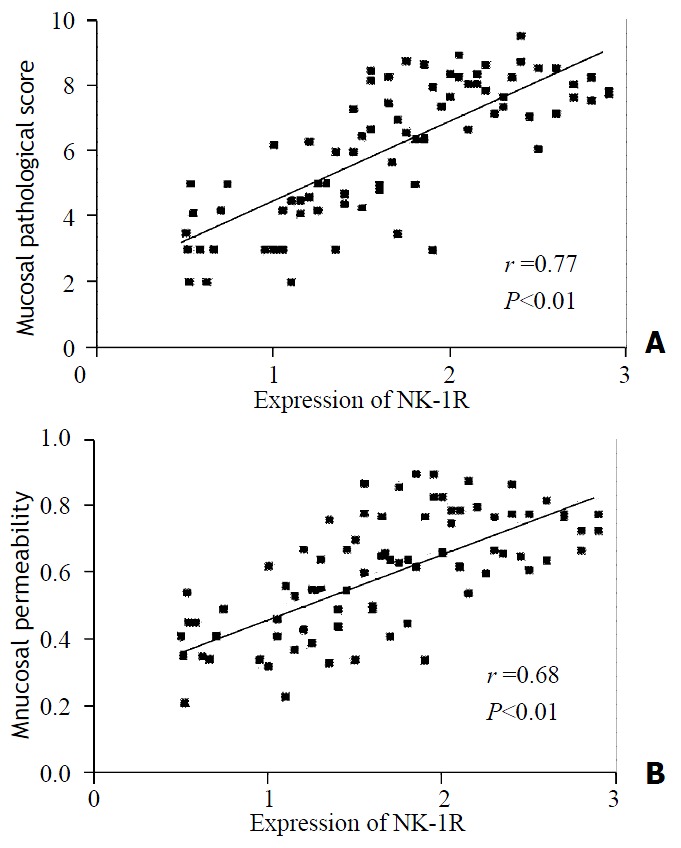
The expression level of NK-AR mRNA was corre-lated with intestinal mucosal pathological score (A) and mucosal permeability (B) in ANP rats
NK-1R and NK-2R protein expression in distal ileum
We then performed the Western blot analysis in controls and ANP group. All the normal controls exhibited approximately 46 kDa band of NK-1R protein of weak intensity. In contrast, the ANP samples showed a more intense signal (Figure 3A). The densitometric analysis demonstrated a 14-fold increase of NK-1R protein level in ANP ileum compared with the normal ileum (P < 0.01).
Figure 3.
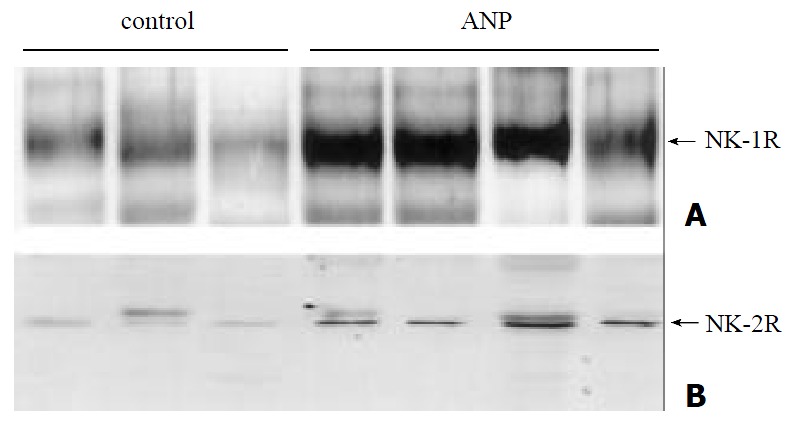
Western blot revealed the protein level of NK-1R (A) and NK-2R (B) in normal control and ANP intestinal tissue
When Western blot analysis for NK-2R was performed, similar pattern was observed, protein signal was weak in normal control, but much stronger in ANP group (Figure 3B). Densitometry revealed a 9-fold increase of NK-2R in ANP ileum (P < 0.01).
DISCUSSION
Intestinal bacterial translocation is the main source leading to infection of pancreas, whereas this translocation is dependent, to some degree, on the function of intestinal mucosal barrier. Intestinal mucosal barrier is made up of mechanical, biological, immunologic and chemical barrier, while the mechanical barrier is the fundamental one, which can prevent large molecule and bacteria from passing through[23,24]. More and more evidence showed that gut barrier dysfunction is related to multiorgan system failure in sepsis and immune dysregulation[25-35]. Pancreatitis-induced hypovolaemia due to endothelial barrier leakage and gut arteriovenous shunting causes intestinal ischaemia and reperfusion injury with concomitant gut barrier dysfunction. Gut endothelial barrier dysfunction probably plays a central role. Potential molecular mechanisms could be associated with alterations in intracellular signal transduction, intercellular signal and expression of adhesion molecules on endothelial cells. Bacterial infections are often seen during the progression of ANP, concomitant with the potential development of multiple organ dysfunction[36,37]. The mechanisms underlying gut barrier dysfunction in acute pancreatitis are thus complex and still not fully elucidated.
SP is synthesized by small-diameter C sensory ‘pain’ fibers, and release of this peptide into the dorsal horn of the spinal cord following intense peripheral stimulation was thought to promote central hyperexcitability (central sensitization)[38,39]. In addition, it could result in plasma extravasation, neutrophil infiltration, and vasodilatation. In rats, both SP and NK-1R selective agonist stimulated pancreatic plasma extravasation, and this response was blocked by the NK-1R antagonist. Selective agonist of NK-2R showed no effect[12]. Continuous infusion of SP stimulated plama extravasation in rat pancreas via activation of NK-1R[40-42].
In the present study, expression of NK-1R and NK-2R mRNA was investigated by RT-PCR and the protein levels of NK-1R and NK-2R were determined using Western blot analysis in normal control and ANP intestines. The results revealed that both NK-1R and NK-2R were overexpressed in ANP intestines, and the overexpression of NK-1R was correlated with mucosal damage in ANP rats. Increased level of SP[43] in ANP, together with overexpression of its receptors-NK-1R and NK-2R, results in excessive biological effect, such as aggregation of neutrophilic granulocyte, cascade release of inflammatory transmitter, tissue fluid and plasma extravasation, thus resulting in deterioration of intestinal pathological changes and gut barrier dysfunction, and facilitating gut bacterial translocation.
Better understanding of the molecular biological changes in ANP will provide novel therapies to this disease. Once specific receptors were identified, selective atagonists which blocked these receptors would have therapeutic effects. Antagonists against NK-1R have showed some effects in acute pancreatitis on animal models[12,42]. Knowledge about the regulating events will probably make future pharmacological therapy available for prevention and treatment of the severe complications of ANP, including gut barrier dysfunction.
Footnotes
Supported by the scientific research funding for the returned overseas Chinese scholars, State Personnel Ministry, No. 7690004027
Edited by Ma JY
References
- 1.Büchler MW, Gloor B, Müller CA, Friess H, Seiler CA, Uhl W. Acute necrotizing pancreatitis: treatment strategy according to the status of infection. Ann Surg. 2000;232:619–626. doi: 10.1097/00000658-200011000-00001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Medich DS, Lee TK, Melhem MF, Rowe MI, Schraut WH, Lee KK. Pathogenesis of pancreatic sepsis. Am J Surg. 1993;165:46–50; discussion 51-52. doi: 10.1016/s0002-9610(05)80403-9. [DOI] [PubMed] [Google Scholar]
- 3.Juvonen PO, Alhava EM, Takala JA. Gut permeability in patients with acute pancreatitis. Scand J Gastroenterol. 2000;35:1314–1318. doi: 10.1080/003655200453683. [DOI] [PubMed] [Google Scholar]
- 4.Liu Q, Djuricin G, Nathan C, Gattuso P, Weinstein RA, Prinz RA. The effect of interleukin-6 on bacterial translocation in acute canine pancreatitis. Int J Pancreatol. 2000;27:157–165. doi: 10.1385/IJGC:27:2:157. [DOI] [PubMed] [Google Scholar]
- 5.Li JY, Lu Y, Hu S, Sun D, Yao YM. Preventive effect of glutamine on intestinal barrier dysfunction induced by severe trauma. World J Gastroenterol. 2002;8:168–171. doi: 10.3748/wjg.v8.i1.168. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Simsek I, Mas MR, Yasar M, Ozyurt M, Saglamkaya U, Deveci S, Comert B, Basustaoglu A, Kocabalkan F, Refik M. Inhibition of inducible nitric oxide synthase reduces bacterial translocation in a rat model of acute pancreatitis. Pancreas. 2001;23:296–301. doi: 10.1097/00006676-200110000-00011. [DOI] [PubMed] [Google Scholar]
- 7.Colak T, Ipek T, Paksoy M, Polat E, Uygun N, Kayabaşi B. The effects of cefephim, G-CSF, and sucralfate on bacterial translocation in experimentally induced acute pancreatitis. Surg Today. 2001;31:502–506. doi: 10.1007/s005950170109. [DOI] [PubMed] [Google Scholar]
- 8.Cicalese L, Sahai A, Sileri P, Rastellini C, Subbotin V, Ford H, Lee K. Acute pancreatitis and bacterial translocation. Dig Dis Sci. 2001;46:1127–1132. doi: 10.1023/a:1010786701289. [DOI] [PubMed] [Google Scholar]
- 9.Buttenschoen K, Berger D, Hiki N, Buttenschoen DC, Vasilescu C, Chikh-Torab F, Seidelmann M, Beger HG. Endotoxin and antiendotoxin antibodies in patients with acute pancreatitis. Eur J Surg. 2000;166:459–466. doi: 10.1080/110241500750008772. [DOI] [PubMed] [Google Scholar]
- 10.Bhatia M, Neoptolemos JP, Slavin J. Inflammatory mediators as therapeutic targets in acute pancreatitis. Curr Opin Investig Drugs. 2001;2:496–501. [PubMed] [Google Scholar]
- 11.Steer ML. Relationship between pancreatitis and lung diseases. Respir Physiol. 2001;128:13–16. doi: 10.1016/s0034-5687(01)00259-6. [DOI] [PubMed] [Google Scholar]
- 12.Grady EF, Yoshimi SK, Maa J, Valeroso D, Vartanian RK, Rahim S, Kim EH, Gerard C, Gerard N, Bunnett NW, et al. Substance P mediates inflammatory oedema in acute pancreatitis via activation of the neurokinin-1 receptor in rats and mice. Br J Pharmacol. 2000;130:505–512. doi: 10.1038/sj.bjp.0703343. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Bhatia M, Brady M, Shokuhi S, Christmas S, Neoptolemos JP, Slavin J. Inflammatory mediators in acute pancreatitis. J Pathol. 2000;190:117–125. doi: 10.1002/(SICI)1096-9896(200002)190:2<117::AID-PATH494>3.0.CO;2-K. [DOI] [PubMed] [Google Scholar]
- 14.Denham JW, Hauer-Jensen M, Kron T, Langberg CW. Treatment-time-dependence models of early and delayed radiation injury in rat small intestine. Int J Radiat Oncol Biol Phys. 2000;48:871–887. doi: 10.1016/s0360-3016(00)00708-2. [DOI] [PubMed] [Google Scholar]
- 15.Park PO, Haglund U, Bulkley GB, Fält K. The sequence of development of intestinal tissue injury after strangulation ischemia and reperfusion. Surgery. 1990;107:574–580. [PubMed] [Google Scholar]
- 16.Weiss DJ, Evanson OA, MacLeay J, Brown DR. Transient alteration in intestinal permeability to technetium Tc99m diethylenetriaminopentaacetate during the prodromal stages of alimentary laminitis in ponies. Am J Vet Res. 1998;59:1431–1434. [PubMed] [Google Scholar]
- 17.Li YS, Li JS, Jiang JW, Liu FN, Li N, Qin WS, Zhu H. Glycyl-glutamine-enriched long-term total parenteral nutrition attenuates bacterial translocation following small bowel transplantation in the pig. J Surg Res. 1999;82:106–111. doi: 10.1006/jsre.1998.5525. [DOI] [PubMed] [Google Scholar]
- 18.Kleeff J, Shi X, Bode HP, Hoover K, Shrikhande S, Bryant PJ, Korc M, Büchler MW, Friess H. Altered expression and localization of the tight junction protein ZO-1 in primary and metastatic pancreatic cancer. Pancreas. 2001;23:259–265. doi: 10.1097/00006676-200110000-00006. [DOI] [PubMed] [Google Scholar]
- 19.Koliopanos A, Friess H, Kleeff J, Shi X, Liao Q, Pecker I, Vlodavsky I, Zimmermann A, Büchler MW. Heparanase expression in primary and metastatic pancreatic cancer. Cancer Res. 2001;61:4655–4659. [PubMed] [Google Scholar]
- 20.King KA, Hu C, Rodriguez MM, Romaguera R, Jiang X, Piedimonte G. Exaggerated neurogenic inflammation and substance P receptor upregulation in RSV-infected weanling rats. Am J Respir Cell Mol Biol. 2001;24:101–107. doi: 10.1165/ajrcmb.24.2.4264. [DOI] [PubMed] [Google Scholar]
- 21.Piedimonte G, Rodriguez MM, King KA, McLean S, Jiang X. Respiratory syncytial virus upregulates expression of the substance P receptor in rat lungs. Am J Physiol. 1999;277:L831–L840. doi: 10.1152/ajplung.1999.277.4.L831. [DOI] [PubMed] [Google Scholar]
- 22.Kaltreider HB, Ichikawa S, Byrd PK, Ingram DA, Kishiyama JL, Sreedharan SP, Warnock ML, Beck JM, Goetzl EJ. Upregulation of neuropeptides and neuropeptide receptors in a murine model of immune inflammation in lung parenchyma. Am J Respir Cell Mol Biol. 1997;16:133–144. doi: 10.1165/ajrcmb.16.2.9032120. [DOI] [PubMed] [Google Scholar]
- 23.Andersson R, Wang XD. Gut barrier dysfunction in experimental acute pancreatitis. Ann Acad Med Singapore. 1999;28:141–146. [PubMed] [Google Scholar]
- 24.Wang XD, Börjesson A, Sun ZW, Wallèn R, Deng XM, Zhang HY, Hallberg E, Andersson R. The association of type II pneumocytes and endothelial permeability with the pulmonary custocyte system in experimental acute pancreatitis. Eur J Clin Invest. 1998;28:778–785. doi: 10.1046/j.1365-2362.1998.00340.x. [DOI] [PubMed] [Google Scholar]
- 25.Hirsh M, Dyugovskaya L, Bashenko Y, Krausz MM. Reduced rate of bacterial translocation and improved variables of natural killer cell and T-cell activity in rats surviving controlled hemorrhagic shock and treated with hypertonic saline. Crit Care Med. 2002;30:861–867. doi: 10.1097/00003246-200204000-00025. [DOI] [PubMed] [Google Scholar]
- 26.Shimizu T, Tani T, Endo Y, Hanasawa K, Tsuchiya M, Kodama M. Elevation of plasma peptidoglycan and peripheral blood neutrophil activation during hemorrhagic shock: plasma peptidoglycan reflects bacterial translocation and may affect neutrophil activation. Crit Care Med. 2002;30:77–82. doi: 10.1097/00003246-200201000-00012. [DOI] [PubMed] [Google Scholar]
- 27.Doty JM, Oda J, Ivatury RR, Blocher CR, Christie GE, Yelon JA, Sugerman HJ. The effects of hemodynamic shock and increased intra-abdominal pressure on bacterial translocation. J Trauma. 2002;52:13–17. doi: 10.1097/00005373-200201000-00005. [DOI] [PubMed] [Google Scholar]
- 28.Köylüoglu G, Bakici MZ, Elagöz S, Arpacik M. The effects of pentoxifylline treatment on bacterial translocation after hemorrhagic shock in rats. Clin Exp Med. 2001;1:61–66. doi: 10.1007/pl00012238. [DOI] [PubMed] [Google Scholar]
- 29.Ling YL, Meng AH, Zhao XY, Shan BE, Zhang JL, Zhang XP. Effect of cholecystokinin on cytokines during endotoxic shock in rats. World J Gastroenterol. 2001;7:667–671. doi: 10.3748/wjg.v7.i5.667. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Cui DX, Zeng GY, Wang F, Xu JR, Ren DQ, Guo YH, Tian FR, Yan XJ, Hou Y, Su CZ. Mechanism of exogenous nucleic acids and their precursors improving the repair of intestinal epithelium after gamma-irradiation in mice. World J Gastroenterol. 2000;6:709–717. doi: 10.3748/wjg.v6.i5.709. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Wu XN. Current concept of pathogenesis of severe acute pancreatitis. World J Gastroenterol. 2000;6:32–36. doi: 10.3748/wjg.v6.i1.32. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Indaram AV, Nandi S, Weissman S, Lam S, Bailey B, Blumstein M, Greenberg R, Bank S. Elevated basal intestinal mucosal cytokine levels in asymptomatic first-degree relatives of patients with Crohn's disease. World J Gastroenterol. 2000;6:49–52. doi: 10.3748/wjg.v6.i1.49. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Zhu L, Yang ZC, Li A, Cheng DC. Protective effect of early enteral feeding on postburn impairment of liver function and its mechanism in rats. World J Gastroenterol. 2000;6:79–83. doi: 10.3748/wjg.v6.i1.79. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Meng AH, Ling YL, Zhang XP, Zhao XY, Zhang JL. CCK-8 inhibits expression of TNF-alpha in the spleen of endotoxic shock rats and signal transduction mechanism of p38 MAPK. World J Gastroenterol. 2002;8:139–143. doi: 10.3748/wjg.v8.i1.139. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Zhu L, Yang ZC, Li A, Cheng DC. Reduced gastric acid production in burn shock period and its significance in the prevention and treatment of acute gastric mucosal lesions. World J Gastroenterol. 2000;6:84–88. doi: 10.3748/wjg.v6.i1.84. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Schwarz M, Thomsen J, Meyer H, Büchler MW, Beger HG. Frequency and time course of pancreatic and extrapancreatic bacterial infection in experimental acute pancreatitis in rats. Surgery. 2000;127:427–432. doi: 10.1067/msy.2000.104116. [DOI] [PubMed] [Google Scholar]
- 37.Hongo H, Takano H, Imai A, Yamaguchi T, Boku Y, Fujii T, Naito Y, Yoshida N, Yoshikawa T, Kondo M. Pancreatic phospholipase A2 induces bacterial translocation in rats. Immunopharmacol Immunotoxicol. 1999;21:717–726. doi: 10.3109/08923979909007137. [DOI] [PubMed] [Google Scholar]
- 38.Duggan AW, Hendry IA, Morton CR, Hutchison WD, Zhao ZQ. Cutaneous stimuli releasing immunoreactive substance P in the dorsal horn of the cat. Brain Res. 1988;451:261–273. doi: 10.1016/0006-8993(88)90771-8. [DOI] [PubMed] [Google Scholar]
- 39.Cao YQ, Mantyh PW, Carlson EJ, Gillespie AM, Epstein CJ, Basbaum AI. Primary afferent tachykinins are required to experience moderate to intense pain. Nature. 1998;392:390–394. doi: 10.1038/32897. [DOI] [PubMed] [Google Scholar]
- 40.Maa J, Grady EF, Kim EH, Yoshimi SK, Hutter MM, Bunnett NW, Kirkwood KS. NK-1 receptor desensitization and neutral endopeptidase terminate SP-induced pancreatic plasma extravasation. Am J Physiol Gastrointest Liver Physiol. 2000;279:G726–G732. doi: 10.1152/ajpgi.2000.279.4.G726. [DOI] [PubMed] [Google Scholar]
- 41.Maa J, Grady EF, Yoshimi SK, Drasin TE, Kim EH, Hutter MM, Bunnett NW, Kirkwood KS. Substance P is a determinant of lethality in diet-induced hemorrhagic pancreatitis in mice. Surgery. 2000;128:232–239. doi: 10.1067/msy.2000.107378. [DOI] [PubMed] [Google Scholar]
- 42.Kirkwood KS, Kim EH, He XD, Calaustro EQ, Domush C, Yoshimi SK, Grady EF, Maa J, Bunnett NW, Debas HT. Substance P inhibits pancreatic exocrine secretion via a neural mechanism. Am J Physiol. 1999;277:G314–G320. doi: 10.1152/ajpgi.1999.277.2.G314. [DOI] [PubMed] [Google Scholar]
- 43.Bhatia M, Saluja AK, Hofbauer B, Frossard JL, Lee HS, Castagliuolo I, Wang CC, Gerard N, Pothoulakis C, Steer ML. Role of substance P and the neurokinin 1 receptor in acute pancreatitis and pancreatitis-associated lung injury. Proc Natl Acad Sci USA. 1998;95:4760–4765. doi: 10.1073/pnas.95.8.4760. [DOI] [PMC free article] [PubMed] [Google Scholar]


