INTRODUCTION
Intervention therapy has become one of the main therapies of hepatic cancer[41,43,46,50]. The introduction of hepatic arterial perfusion and embolization has provided opportunities for a secondary operation on patients with intermediate and advanced cancer[42,51-53], thus prolonging patients’ life and improving their life quality[1]. However, intractable ascites and hemorrhage of upper digestive tract caused by portal hypertension still greatly threatened the patients’ life [2,7-9,11,14,17,19-25,39]. So far there has been little report on the incidence rate of hepatic arterio venous fistula (HA-V)[4] and the relationship between its typing and hepatic cancer as well as portal hypertention[3,6,12,18,26-28,31,32,34,54,59]. In the present study, a series of observation and analysis were made for 110 cases of hepatic arteriovenous fistula concurrent with intermediate and advanced hepatic cancer.
MATERIALS AND METHODS
Clinical data
One hundred and ten cases were selected from the 583 cases of hepatic cancer, which were clinically verified by radiological images and admitted to our department from 1989 to 1999. The cases were diagnosed as hepatic arteriovenous fistula by Seldinger technique with DSA, among which, 102 were males and 8 females aged between 27 years and 70 years (average 48 ± 5 years). One hundred and three cases were primary and 7 were secondary hepatic cancer. The latter include 3 cases of primary carcinoma of colon, 2 carcinoma of ampulla, 1 carcinoma of pancreas and 1 cardiac cancer. Among the 110 cases, there were 58 (52.72%) cases of concurrent ascites and 31 (28.18%) hemorrhage of upper digestive tract.
Examination
Examination of hepatic arteriovenous fistula All the cases underwent percutaneous femoral puncture by Seldinger technique. Guided by X-ray, the head of the conduct cannula was placed in the celiac artery and upper mesenteric artery. Through the cannula, 38% cardiografin or Ultravist of 20 mL-25 mL at a time and at a rate of 4 mL/S-5 mL/S was perfused with high pressure while the arteries were photographed continuously at 2 frames per second until the pylicstem was developed or the photography lasted up to 20 s. The DSA results indicate that portal vein, hepatic vein or inferior caval vein in hepatic arterial phase or hepatic parenchymic phase developed ahead of the expected time could be diagnosed as concurrent hepatic arteriovenous fistula. The 110 cases of hepatic arteriovenous fistula received DSA examination for a total of 273 times, for some cases once at least and some 9 times at most.
Barium meal examination of upper digestive tract Thirty cases received routine pneumobarium double contrast examination.
Gastrofiberscopy Thirty-three cases took routine gastrofiberscopy.
Statistical analysis χ² test and U test were performed according to NoSA software package.
RESULTS
Among the 583 patients with hepatic cancer, 110 were found to have hepatic arteriovenous fistula, which indicated an average incidence rate of 18.86%. From 1989 to 1999, the annual incidence rate of hepatic arteriovenous fistula ranged from 2.38% to 47.72%, as shown in Figure 1.
Figure 1.
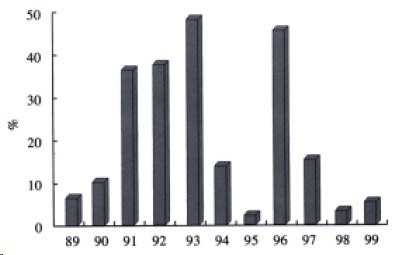
Annual incidence rate of hepatic arteriovenous fistula from 1989 to 1999.
Of the 110 cases of hepatic arteriovenous fistula, 57 had their focuses in the right lobe (51.81%), 13 in the left lobe (11.81%) and 40 involved both (36.36%). Seventy-four were massive (67.27%), 21 nodular (19.09%) and 15 diffuse (13.63%). Eleven were aberrant in their hepatic arterial origins (10.00%), of which 7 were of the right vagoheptatic artery, 1 of the common vagohepatic artery, 1 of the right vagoaccessary hepatic artery (all the above-mentioned 9 aberrant cases originated in the superior mesenteric artery), and the others, 1 left vagohepatic artery originated in the left arterial gastric and 1 common vagohepatic artery in the right diaphragmatic artery. DSA detected sufficient blood supply in 89 cases (89.90%), moderate blood supply 14 (12.72%) and poor supply 7 (6.36%).
According to the locations of the fistula or the abnormal split-flow, the 110 cases can be divided into two main types: 95 peripheral (86.36%) and 15 central (13.63%). Hepatic arteriovenous fistula usually occurs in the cases with sufficient blood supply and massive hepatic cancer (Table 1) There were 103 simple cases (93.63%) and 7 complicated cases (6.36%) (Table 2).
Table 1.
The relationship between locations of hepatic arteriovenous fistula and the typing as well as neoplastic blood supply
| Location | na |
Typingb |
Neoplastic blood supply |
||||
| Massive | Nodular | Diffuse | Sufficient | Moderate | Poor | ||
| Peripheral | 95 | 67 | 18 | 10 | 79 | 9 | 7 |
| Central | 15 | 7 | 3 | 5 | 10 | 5 | 0 |
| N = 110 | 74 | 21 | 15 | 89 | 14 | 7 | |
aPeripheral cases significantly outnumbered central ones (P < 0.05, χ² = 6.05).
Massive cases significantly outnumbered diffuse ones (P < 0.05, χ² = 6.09). There is no difference between massive ones and nodular ones, or nodular ones and diffuse ones (P > 0.05). Peripheral ones outnumbered central ones in blood supply (P < 0.05, χ² = 7.34). Sufficient blood supply cases significantly outnumbered cases of moderate blood supply (P < 0.05, χ² = 5.83). There is no difference between those with sufficient and poor supply, or with moderate and poor supply (P > 0.05).
Table 2.
Typing of hepatic arteriovenous fistula
| Typing | n | HA-PV | Others | P |
| Simple | 103 | 97 | 6 | < 0.01 |
| Complicated | 7 | 0 | 7 | χ² = 55.78 |
One hundred and three cases (93.63%) are simple ones which indicate hepatic arterioportal vein fistula in 97 cases (88.18%) (Figure 2), hepatic arteriovenous fistula in 4 cases (Figure 3), hepatoinferior vena cava fistula in 2 cases (Figure 4). Seven cases are complicated ones which indicate both HA-IV fistula and HA-PV fistula in 3 cases, both HA-IV fistula and HA-V fistula in 1 case, first HA-V and then HA-IV fistula in 1 case, HA-IV fistula first and then HA-PV fistula in 1 case, three HA-PV fistulas in 1 case (Figure 5, Figure 6, Figure 7). The simple ones are more than complicate ones significantly (Table 2).
Figure 2.
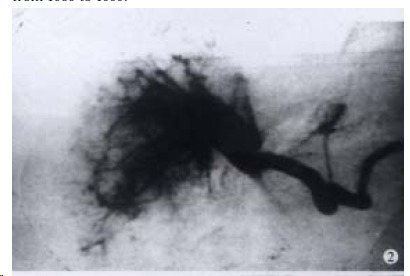
The hepatic arterioportal vein fistula (central cases).
Figure 3.

The hepatic arteriovenous fistula (peripheral cases).
Figure 4.

The hepatoinferior vena cava fistula (peripheral cases).
Figure 5.
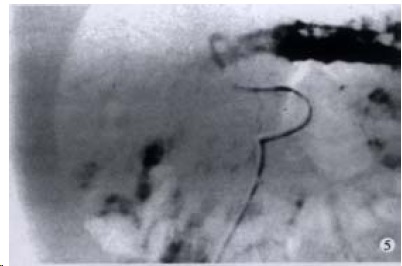
The left vagoaccessary hepatic arterioportal vein fistula (central cases)
Figure 6.

The right hepatic arterioportal vein fistula (peripheral cases): the superior mesenteric vein retrogradely developed.
Figure 7.
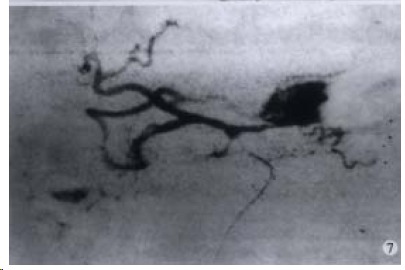
The left hepatoportal vein fistula (central cases).
Portal hypertension is clinically characterized by ascites and hemorrhage of the upper digestive tract. Barium meal examination and gastrofiberscopy of upper digestive tract of the portal hypertension cases indicated that the positive rate of varices of esophagus detected by gastrofiberscopy was significantly higher than that by barium meal examination. The positive rate of ascites by gastro fiberscopy was 100% whereas that by barium meal check up was only 56.66% (P < 0.01, U = 4.08). The positive rate of hemorrhage of upper digestive tract detected by gastrofiberscopy was 96.96% whereas that by barium meal checkup was 53.33% (P < 0.01, U = 3.77). It is worth notice that among the 52 patients with concurrent hepatic arteriovenous fistula who received neither gastrofiberscopy nor barium meal exam, the incidence rates of ascites and hemorrhage of upper digestive tract were 46.15% and 19.23% respectively, from which the possible existence of esophageal varices could not be excluded.
DISCUSSION
In the present study, we analyzed the relationship between the incidence rate and typing of hepatic arteriovenous fistula and the typing and blood supply of hepatic cancer, compared and analyzed ascites and hemorrhage of upper digestive tract by gastrofiberscopy[57,60-62], barium meal checkup and DSA. According to the results of these investigations, we have come to the following conclusions.
Hepatic arteriovenous fistula claims a relatively high incidence rate[3,5,35-40], among hepatic cancer cases, with an average of 18.86% and every 4 or 5 years as a cycle of change. Primary hepatic cancer accounts for 93.63% of concurrent hepatic arteriovenous fistula cases.
Hepatic arteriovenous fistula is usually found in cases of sufficient blood supply and massive type hepatic cancer, which usually indicates the severity of lesion.
The incidence rate of hepatic arterio-pylic fistula (HA-PV) is significantly higher than that of other types of abnormal hepatic arteriovenous split flow, which indicates that hepatic arteriovenous fistula is an important factor that leads to concurrent portal hypertension of moderate and advanced hepatic cancers[39].
Portal hypertension caused by hepatic arteriovenous fistula is clinically and chiefly characterized by ascites (52.72%) and secondarily by hemorrhage of upper digestive tract (28.18%)[8,11,30].
Barium meal checkup and gastrofiberscopy of upper digestive tract of concurrent portal hypertension cases indicate that the positive rate of esophageal varices detected by gastrofiberscopy was much higher than that by barium meal check up[44,48,49]. Ascites and hemorrhage accounted for 46.15% and 19.23% of the 52 patients with hepatic arteriovenous fistula who did not receive barium meal checkup and gastrofiberscopy[19,29]. It is thus suggested by the authors that gastrofiberscopy should be performed in patients with moderate and advanced cancers no matter whether they have concurrent ascites and hemorrhage of upper digestive tract or not. Gastrofiberscopy should be included in the routine examinations[10,13], especially for patients with concurrent ascites and hemorrhage of upper digestive tract so as to detect esophageal varices as early as possible and treat it timely[15,17,18].
Hepatic arteriovenous fistula is usually found in hepatic cancers of the peripheral type[47], which indicates that embolisation of hepatic artery can block the neoplastic blood supply and inhibit neoplastic growth[48]. In the meantime, the embolisation can also block the abnormal split-flow between hepatic arteries and veins, relieve ascites and hemorrhage of upper digestive tract caused by portal hypertension as well as the distant metastasis caused by venous shunt.
The current therapies applied to the treatment of hepatic cancer mainly include hepatic arterial perfusion, embolisation, local injection of absolute alcohol guided by ultrasonography, radio frequency therapy, etc.[45,55,58]. However, it is difficult for ultrasonography and CT to preliminarily detect hepatic arteriovenous fistula which is highly incidental to primary hepatic cancer of massive and sufficient blood supply types. Besides, the abnormal split- flow between hepatic arteries and veins may inhibit the effect of these therapies and even give rise to some complications[12,26,31,56].
Therefore, we conclude that DSA should be included as an important part of the routine examination for the treatment of moderate and advanced hepatic cancer. In order to detect hepatic arteriovenous fistula early and treat the patients with embolisation timely, DSA should be given especially to hepatic cancer patients with concurrent ascites and hemorrhage of upper digestive tract[5,6,16,17,33,34].
Footnotes
Edited by You DY
Verified by Ma JY
References
- 1.Wang ZM, Xu SD, Zhu RF. DSA Observation of hemodynamic change of intermediate and advanced primary hepatic cancers and its clinical significance. Disi Junyi Daxue Xuebao. 1993;14:430–434. [Google Scholar]
- 2.Wang ZY, Shi ZH, Zai RY. [Hepatic arterial infusion chemotherapy and embolization in the treatment of hepatic carcinoma] Zhonghua Zhong Liu Za Zhi. 1994;16:454–457. [PubMed] [Google Scholar]
- 3.Okuda K, Musha H, Yamasaki T, Jinnouchi S, Nagasaki Y, Kubo Y, Shimokawa Y, Nakayama T, Kojiro M, Sakamoto K, et al. Angiographic demonstration of intrahepatic arterio-portal anastomoses in hepatocellular carcinoma. Radiology. 1977;122:53–58. doi: 10.1148/122.1.53. [DOI] [PubMed] [Google Scholar]
- 4.Wang ZM, Wu ZQ. Typing of the DSA symptoms of intermediate and advanced primary hepatic cancers and its clinicalsignificance. Shiyong Fangshexue Zazhi. 1998;14:268–269. [Google Scholar]
- 5.Luo FC, Li XR, Chen WF. Interventional therapy of hepatic arteriovenous fistula concurrent with ruptured and bleeding varices of esophagus. Shiyong Aizheng Zazhi. 1999;14:204–206. [Google Scholar]
- 6.Quan QZ. Causes and treatment of esophagus varicose vein hemorrage. Xin Xiaohuabingxue Zazhi. 1997;5(Suppl 6):18. [Google Scholar]
- 7.Wu DZ, Zhang XD, Zhang LY. Combining therapy for 118 cases of upper digestive tract hemorrage in cirrhosis of liver. Xin Xiaohuabingxue Zazhi. 1997;5(Suppl6):112–113. [Google Scholar]
- 8.Liu Z, Hua ZY, Wang J, Zhao Z. Analysis of 26 cases of portal hypertension upper digestive tract hemorrhage. Xin Xiaohuabingxue Zazhi. 1997;5(Suppl 6):115–116. [Google Scholar]
- 9.Liu SH, Wang TC. Effect of hepatocarcinoma TAE on blood rheology. Xin Xiaohuabingxue Zazhi. 1997;5(Suppl 6):128–129. [Google Scholar]
- 10.Liu DX, Guo H. Endoscopic diagnosis of 293 cases of senile upper digestive tract hemorrhage. Xin Xiaohuabingxue Zazhi. 1997;5(Suppl 6):133. [Google Scholar]
- 11.Wu ZA, Wang RF, He ZJ, Wei XX, Duan P. Analysis of 161 cases of upper digestive tract massive hemorrhage. Xin Xiaohuabingxue Zazhi. 1997;5(Suppl 6):173. [Google Scholar]
- 12.She XF, Lu H. Relationship between Sonogram character of massive type hepatocarcinoma and prognosis. Xin Xiaohuabingxue Zazhi. 1997;5(Suppl 6):177. [Google Scholar]
- 13.Mu ST. Endoscopic diagnosis of 1778 cases of peptic ulcer. Xin Xiaohuabingxue Zazhi. 1997;5(Suppl 6):188. [Google Scholar]
- 14.He QN, Feng ZT, Dong CJ, Sun R, Zhou SC, Sun ZQ, Li CH, Shi SR. Clinical analysis of 3878 cases of in-patients peptic ulcer. Xin Xiaohuabingxue Zazhi. 1997;5(Suppl 6):192–193. [Google Scholar]
- 15.Huang LY, Liu YX, Yi DL. Analysis of dangerious factors in 23 cases failed in injection treatment for gastric ulcer hemorrage. Huaren Xiaohua Zazhi. 1998;6:152. [Google Scholar]
- 16.Zhang J, Wang SZ. Treatment of 6 cases of hemorrage from primary hepat ocarcinoma rupture by embolization. Huaren Xiaohua Zazhi. 1998;6:262. [Google Scholar]
- 17.Zheng GQ, Yin BT, Liu YM, Jiang HY, Liu FH. Treatment of portal hypertensive digestive tract hemorrhage. Huaren Xiaohua Zazhi. 1998;6:255. [Google Scholar]
- 18.Li ZS, Wang X, Xu GM. Classification, diagnosis and treatment of gastric varicos vein. Huaren Xiaohua Zazhi. 1998;6:342–344. [Google Scholar]
- 19.Song ZQ, Gu CH, Hao F, Zhang J. Current condition and evaluation on comparehensive treatment for refractory asciteswith liver cirrhosis. Huaren Xiaohua Zazhi. 1998;6:347–348. [Google Scholar]
- 20.Chen WH, Chen H, Lin JK, Ren M, Li CJ, Hu PJ. Relationship between hepatocirrhosis gastroesphagel reflux and varicosevein rupture hemorrhage. Huaren Xiaohua Zazhi. 1998;6:358–359. [Google Scholar]
- 21.Wu JS, Li XR. Prospect in study of pathogenesis of portal hypertension. Huaren Xiaohua Zazhi. 1998;6:737–740. [Google Scholar]
- 22.Li XR, He ZS, Wu JS, Ma QJ, Lu JG, Wu YZ. Microstructural changes in splenic arteries and veins of patients with portalhypertension. Huaren Xiaohua Zazhi. 1998;6:760–761. [Google Scholar]
- 23.Wang X, Huang YX, Wen QS, Cu YK, Li DY, Zhang HX, Zhang JZ, Wang YD. Experimental study on gastric mucosal injury by hepatic arterial embolization in rabbits. Huaren Xiaohua Zazhi. 1998;6:997–999. [Google Scholar]
- 24.Yu WX, Li H, Liu AW, Zhang LL. Imagic control of in hepatocarcinoma complicated portal hypertension with or withoutcarcinoma embolus. Shijie Huaren Xiaohua Zazhi. 1999;7:544–545. [Google Scholar]
- 25.Chen LB, Yang L. CO contraction effect of superior mensteric artery and abdominal aorta in rat portal hypertension. Shijie Huaren Xiaohua Zazhi. 1999;7:1001–1002. [Google Scholar]
- 26.Li MC, Zhou YX, Hao CQ, Lei XE, Li GY. Diagnostic value of B-mode ultrasono graph for portal hypertension. Shijie Huaren Xiaohua Zazhi. 1999;7:306–308. [Google Scholar]
- 27.Leng XS. Current status on studies of pathogenesis of portal hypertension. Shijie Huaren Xiaohua Zazhi. 1999;7:369–371. [Google Scholar]
- 28.Li XH, Wang L, Fang YW, Lu YK. Color Doppler ultrasonic exemination surveillances hymodynamic changes of hepatocirrhosis portal hypertension. Shijie Huaren Xiaohua Zazhi. 1999;7:453–454. [Google Scholar]
- 29.Chen SY, Wu TF, Liu HY, Wang JY, Zhang SS, Zhang XD. Hospital-based ten-year data of gastroendoscopy. Shijie Huaren Xiaohua Zazhi. 1999;7:15–17. [Google Scholar]
- 30.Wang ZG, Zou JJ, She S, Li XL, Zhang YP, Huang YQ, Ding FQ, Liu GZ. Effect of chemotherapy on portal venous pressure. Shijie Huaren Xiaohua Zazhi. 2000;8:120–121. [Google Scholar]
- 31.Li KY, Zhang QP. Study on color Doppler exemination of carcinoma embolus of hepatocarcinoma portal vein andhymodynamics. Zhonghua Chaosheng Yingxiangxue Zazhi. 1994;4:145. [Google Scholar]
- 32.Yang HS, Zhao YS, Wang DW. Study on 307 cases of hepatocarcinoma angiography and character. Baiqiuen Yike Daxue Xuebao. 1993;3:262. [Google Scholar]
- 33.Zhou K, Lou LH, He YZ. Interventional therapy for primary hepatocarcinoma complicated with intrahepatic arteriovenousfista (with experience of treatment for 36 cases) Zhongguo Shiyong Waike Zazhi. 1995;3:163. [Google Scholar]
- 34.Kido C, Sasaki T, Kaneko M. Angiography of primary liver cancer. Am J Roentgenol Radium Ther Nucl Med. 1971;113:70–81. doi: 10.2214/ajr.113.1.70. [DOI] [PubMed] [Google Scholar]
- 35.Wu ZQ, Fan J, Qiu SJ, Zhou J, Tang ZY. The value of postoperative hepatic regional chemotherapy in prevention of recurrence after radical resection of primary liver cancer. World J Gastroenterol. 2000;6:131–133. doi: 10.3748/wjg.v6.i1.131. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Jiang YF, Yang ZH, Hu JQ. Recurrence or metastasis of HCC: predictors, early detection and experimental antiangiogenic therapy. World J Gastroenterol. 2000;6:61–65. doi: 10.3748/wjg.v6.i1.61. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Zhang ZR, He Q, Liao GT, Bai SH. Study on the anticarcinogenic effect and acute toxicity of liver-targeting mitoxantrone nanoparticles. World J Gastroenterol. 1999;5:511–514. doi: 10.3748/wjg.v5.i6.511. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Thampanitchawong P, Piratvisuth T. Liver biopsy: complications and risk factors. World J Gastroenterol. 1999;5:301–304. doi: 10.3748/wjg.v5.i4.301. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Assy N, Paizi M, Gaitini D, Baruch Y, Spira G. Clinical implication of VEGF serum levels in cirrhotic patients with or without portal hypertension. World J Gastroenterol. 1999;5:296–300. doi: 10.3748/wjg.v5.i4.296. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Zhao WS, Zhi DS, Liu BP, Jiang W, Cong Z, Dong C. Stereotactic conformal radiotherapy of hepatic metastases: clinical analysis of 8 cases. World J Gastroenterol. 1999;5:353–355. doi: 10.3748/wjg.v5.i4.353. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Li L, Wu PH, Mo YX, Lin HG, Zheng L, Li JQ, Lu LX, Ruan CM, Chen L. CT arterial portography and CT hepatic arteriography in detection of micro liver cancer. World J Gastroenterol. 1999;5:225–227. doi: 10.3748/wjg.v5.i3.225. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Lu MD, Chen JW, Xie XY, Liang LJ, Huang JF. Portal vein embolization by fine needle ethanol injection: experimental and clinical studies. World J Gastroenterol. 1999;5:506–510. doi: 10.3748/wjg.v5.i6.506. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Yip D, Findlay M, Boyer M, Tattersall MH. Hepatocellular carcinoma in central Sydney: a 10-year review of patients seen in a medical oncology department. World J Gastroenterol. 1999;5:483–487. doi: 10.3748/wjg.v5.i6.483. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Zhu JY, Leng XS, Dong N, Qi GY, Du RY. Measurement of liver volume and its clinical significance in cirrhotic portal hypertensive patients. World J Gastroenterol. 1999;5:525–526. doi: 10.3748/wjg.v5.i6.525. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.He XS, Huang JF, Liang LJ, Lu MD, Cao XH. Surgical resection for hepatoportal bile duct cancer. World J Gastroenterol. 1999;5:128–131. doi: 10.3748/wjg.v5.i2.128. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.An SZ, Yao XX, Cui DL. Experimental and clinical study on interventional therapy with sclerotic complex agents for hepatic cysts. World J Gastroenterol. 1998;4(Suppl 2):110. [Google Scholar]
- 47.Zhao SL, Pan XF, Lu¹ XP. Primary hepatic carcinoma with extrahepatic metastasis and secondary hepatic carcinoma. World J Gastroenterol. 1998;4(Suppl 2):90–91. [Google Scholar]
- 48.Jiang ZM, Zhang SY, Li YG, Wang XR, Jia RM, Jiang YK, Hao SM, Liu YS. Diagnosis and treatment of gastrojejunocolic fistula and nutrition support action. World J Gastroenterol. 1998;4(Suppl 2):86. [Google Scholar]
- 49.Xu YJ, Liu XN, Guan HW, Zhu LH, Bai DS. Diagnosis and treatment of spontaneous rupture of liver carcinoma withbleeding. World J Gastroenterol. 1998;4(Suppl 2):81. [Google Scholar]
- 50.Gao ZD, Xu XY, Mao AW, Zhou XF, Jiang H. Combination of arterial infusion chemotherapy and radio therapy in the treatment of 36 cases of middle and late stage esophageal cancer. World J Gastroenterol. 1998;4(Suppl 2):72. [Google Scholar]
- 51.Li GF, Xie SB, Sun H, Yang XH, Liu WJ, Zhai Q, Zhou YX, Li ZH, Zhang GM. An investigation of intra-arterial chemotherapy infusion and embolization combined with abdominal chemotherapy for advanced gastric cancer. World J Gastroenterol. 1998;4(Suppl 2):71–72. [Google Scholar]
- 52.Huang FG, Li Y, Xie XD. Side effects and complcations of hepatic arterial infusion and embolization of liver carcinoma inaged patients and its management. World J Gastroenterol. 1998;4(Suppl 2):67–68. [Google Scholar]
- 53.Xiao XW. The value of selective chemoembolization in the treatment of hepatiometastases in colorectal carcinoma. World J Gastroenterol. 1998;4(Suppl2):38–41. [Google Scholar]
- 54.Li L, Wu PH, Lin HG, Li JQ, Mo YX, Zheng L, Lu LX, Ruan CM, Chen L. Findings of non-pathologic perfusion defects by CT arterial portography and non-pathologic enhancement of CT hepatic arteriography. World J Gastroenterol. 1998;4:513–515. doi: 10.3748/wjg.v4.i6.513. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Li L, Wu PH, Li JQ, Zhang WZ, Lin HG, Zhang YQ. Segmental transcatheter arterial embolization for primary hepatocellular carcinoma. World J Gastroenterol. 1998;4:511–512. doi: 10.3748/wjg.v4.i6.511. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Hepworth CC, Kadirkamanathan SS, Gong F, Swain CP. A randomised controlled comparison of injection, thermal, and mechanical endoscopic methods of haemostasis on mesenteric vessels. Gut. 1998;42:462–469. doi: 10.1136/gut.42.4.462. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Longstreth GF, Feitelberg SP. Successful outpatient management of acute upper gastrointestinal hemorrhage: use of practice guidelines in a large patient series. Gastrointest Endosc. 1998;47:219–222. doi: 10.1016/s0016-5107(98)70316-5. [DOI] [PubMed] [Google Scholar]
- 58.Zhu JF, Xu SX, Zhang XH, Shong LP, Shan LC. Combined treatment of advanced hepatic carcinoma guided by laparoscope. China Natl J New Gastroenterol. 1996;2:247–248. [Google Scholar]
- 59.Zhu XX, Chen JK, Lu GM. Magnetic resonance imaging of portal vein invasion in hepatocellular carcinoma: A corroboration of 25 cases. China Natl J New Gastroenterol. 1996;2:167–170. [Google Scholar]
- 60.Ji XL, Liu YX, Wang YH, Zhao H. Histopathological study of hepatocellular carcinoma after transcatheter hepatic arterialembolization. China Natl J New Gastroenterol. 1996;2:79–81. [Google Scholar]
- 61.Fan YZ, Cai TN, Wang BC. Studies on surgical operations and prognosis of extrahepatic bile duct cancer. China Natl J New Gastroenterol. 1996;2:27–29. [Google Scholar]
- 62.Tang ZY. Clinical research of hepatocellular carcinoma in the 21st century. China Natl J New Gastroenterol. 1995;1:2–3. [Google Scholar]


