Abstract
Background:
Repigmentation of vitiligo is closely related to hair follicles. Hence, replenishing melanocytes in vitiliginous patches utilizing undifferentiated stem cells of the hair follicles using follicular unit transplantation (FUT) is a possible treatment option.
Objectives of the Study:
To study the efficacy of FUT in cases of segmental/stabilized vitiligo as a treatment option for leukotrichia.
Materials and Methods:
Fifty patients with 63 lesions of stable vitiligo over nonglabrous areas were treated with follicular unit grafts. Reduction in the size of vitiligo patches as well as improvement in the associated leukotrichia were evaluated using subjective and objective assessments.
Results:
Of the 63 patches, good to excellent response was seen in 39 (61.9%), fair in 16 (25.4%), and poor in eight (12.7%) lesions. No repigmentation was seen in two (4.8%) lesions. The mean improvement seen was 61.17%. Excellent color match was observed in 44 lesions (69.8%). Repigmentation of the depigmented hairs occurred in 11 out of 46 patients with associated leukotrichia.
Conclusion:
FUT is a safe and effective method for treating localized and segmental vitiligo, especially on hairy parts of the skin. Though labor intensive, it was found to be associated with a quick patient recovery time, very low morbidity, and good color match.
KEYWORDS: Hair follicle, leukotrichia, surgery, transplantation, vitiligo
INTRODUCTION
Vitiligo is one of the oldest diseases plaguing mankind. It is a common depigmenting disorder characterized clinically by milky-white patches and histologically by an absence of functional melanocytes in the affected area. Despite modern advances in medical science and in the social attitude of people, it continues to be psychologically devastating for the patient.
Vitiligo causes a partial or total destruction of melanocytes, initially only of the epidermis and later even of the hair follicles known as leukotrichia. Repigmentation can be achieved by either activating the existing melanocyte reservoir or providing a melanocyte reservoir as a source for pigmentation. This forms the underlying principle for various treatment modalities available today. Follicular unit transplantation (FUT) is one such relatively uncharted surgical technique that relies on providing a reservoir of undifferentiated stem cells to the depigmented lesional skin.
The aim was to study the efficacy of FUT in cases of segmental/stabilized vitiligo affecting the nonglabrous skin and as a means to improve the cosmetic result in combination with other modalities in glabrous skin.
MATERIALS AND METHODS
This was a prospective study involving 50 patients with stable vitiligo in nonglabrous parts of the body. The study was carried out at the dermatology department of a tertiary care hospital of southern India from November 2011 to November 2013. Ethical clearance was obtained prior to starting the study. The patients were selected randomly according to the inclusion and exclusion criteria.
Inclusion criteria
Patients willing for the procedure (written informed consent obtained).
Male and female patients with segmental or localized stable vitiligo as per the Indian Association of Dermatologists Venereologists and Leprologists (IADVL) Task Force for standard guidelines of care for dermatological procedures (A patient reporting no new lesions, no progression of existing lesions, and absence of Koebner phenomenon during the past 1 year).[1]
Patients not responding to the medical line of treatment in the past 1 year.
Exclusion criteria
Patients with active vitiligo.
Patients with a history of Koebner phenomenon.
Patients with keloidal tendency.
Patients with a history of bleeding disorders.
Procedure
Written informed consent was obtained from all the patients for their participation in the study. Details about the patient and a detailed history about the disease such as the site of onset, duration, progression, stability of the disease, and history of medication was taken. Any previous history of systemic diseases, endocrinological disturbances, bleeding tendency or herpes labialis was noted. The selected patients were thoroughly examined for the number of lesions, size, site, and type of vitiligo. Old scars and Bacillus Calmette-Guérin (BCG) scars were examined to exclude keloidal tendency.
All the patients were investigated for complete hemogram, bleeding time, and clotting time. Lignocaine sensitivity was tested before the surgery. Photographs were taken before the procedure and then periodically to compare the pigmentation and color match.
Follicular unit grafting was done in the vitiliginous lesion and the hair was transplanted 3-5 mm apart. After giving tumescent anesthesia (lignocaine with 1:100,000 adrenaline diluted in the ratio of 1:10 with normal saline), the donor follicles were extracted using 1-mm biopsy punch [follicular unit extraction (FUE) technique]. The donor area was the occipital or postauricular region of the scalp chosen as per the patient's requirement, i.e., the number of hair required, the characteristics of the hair at the recipient site, etc. The hair follicles so extracted were stored in Petri dish with cold normal saline till the transplantation was complete. The hair follicles were transplanted intact as follicular units. After infiltrative anesthesia at the recipient site, transplantation was done using Kolkata slits/18-G needle/SAVA ®transplanter (Vasa Surgiart Pvt. Ltd., Ahmedabad, Gujrat, India) to create slits in the recipient area and the hair follicle was gently inserted using a jeweler's forceps into the created slits. Topical corticosteroid and tacrolimus or topical PUVAsol therapy was started after 10 days to facilitate repigmentation.
Assessment
The patients were followed up regularly for a period of 6 months, at an interval of every 2 weeks or till repigmentation was first observed and then at monthly intervals. The results were assessed at the end of 6 months for the extent of repigmentation, color match, and complications. Since the areas for which the follicular unit transplant was done were very small, standard scores like the vitiligo area severity index (that uses % body area as an index for the size of lesion) could not be used. Hence, we devised two methods, one qualitative, depending on the patient's assessment, and the other quantitative, using a point counting method to assess the extent of repigmentation. The degree of repigmentation was evaluated qualitatively on the basis of visual analogue system score for the extent of pigmentation and color match. This grading was as follows:
0-25% — poor response (Grade I).
25-50% — fair response (Grade II).
50-75% — good response (Grade III).
75-100% — excellent response (Grade IV).
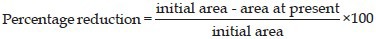
Quantitative assessment was done by calculating the percentage area of reduction in the area of vitiligo. The area was calculated with a simple point counting method using a transparent sheet to mark the outlines of the lesion and calculate the area using a standard graph paper [See Figure]. This was done at every follow-up. The percentage reduction in size was calculated as follows:
Hair in the vitiliginous patch was also observed for any change in pigmentation.
Statistical tools
The information collected regarding all the selected cases were recorded in a master chart. Data analysis was done with the help of computer using IBM SPSS Statistics v22 statistical software.
RESULTS
The study included 50 patients of stable vitiligo of the nonglabrous skin with 63 patches at various sites of the body treated with FUT.
Among the 50 patients, 30 (60%) were males and 20 (40%) were females. The age of these patients ranged 6-65 years with a mean of 23.7 years. Maximum patients were between 11 years and 30 years of age with the median age being 21 years.
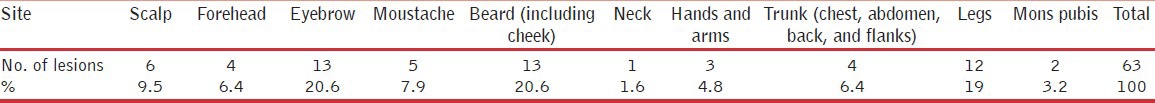
Out of the lesions treated, the most common was the localized type [Chart 1]. The size varied from 10.7 cm2 of the largest lesion to 0.4 cm2 for the smallest lesion treated. Only nonglabrous skin was treated with this method. The most common site treated was the face, including the eyebrows, beard, and moustache, and the forehead [Table 1]. The duration of vitiligo ranged from 1-25 years with a mean duration of 5.18 years. Vtiligo was present for 5-10 years in 40%, 2-5 years in 30%, less than 2 years in 18%, while 12% had a duration of more than 10 years.
Chart 1.
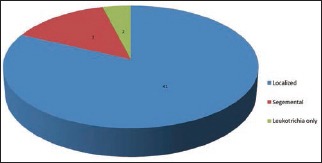
Type of vitiligo
Table 1.
Site distribution
Postoperative evaluation
After the procedure, there was formation of scabs and crusts around the hair follicles that peeled off in most of the patients within 1 week. The transplanted hair follicles were taken up in almost all the patients, with only five out of 50 patients showing poor uptake. The reason for poor uptake in these patients was found to be improper care of the wound site.
After the uptake of the hair follicles, onset of pigmentation ranged 2-12 weeks. Maximum number of lesions showed pigmentation between 3 weeks and 4 weeks. The median time for the onset of pigmentation was 4 weeks [Chart 2].
Chart 2.
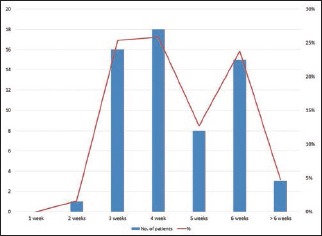
Onset of pigmentation
Using the visual analogue score for assessment in 63 patches, good to excellent response was seen in 39 (61.9%), fair in 16 (25.4%), and poor in eight (12.7%) lesions [Figures 1a and b–4a and b]. No repigmentation was seen in two (4.8%) lesions [Table 2]. One was due to the poor uptake of hair follicles caused by improper postoperative care, the other was a case of piebaldism where follicular unit transplant was tried as a treatment for leukotrichia.
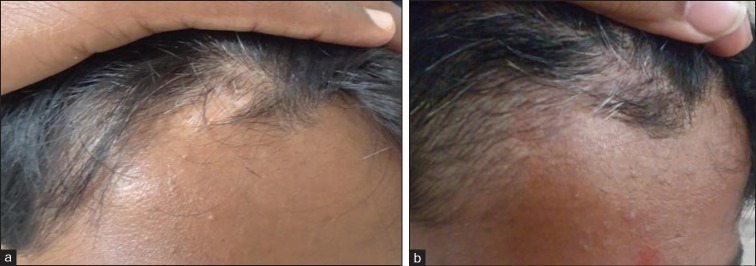
Figure 1.
(a) Vitiligo lesion over scalp - before the procedure (b) Six months after the procedure; improvement in vitiligo and leukotrichia with excellent color match
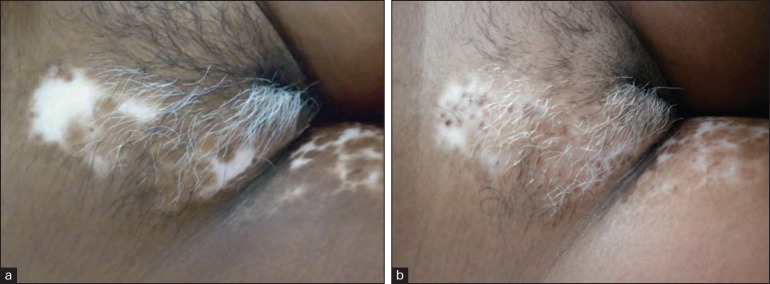
Figure 4.
(a) Vitiligo lesions over the mons pubis before the procedure (b) Vitiligo lesions over the mons pubis 6 months after the procedure
Table 2.
Grade of improvement
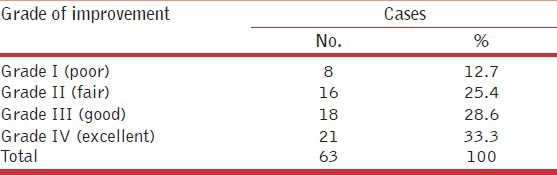
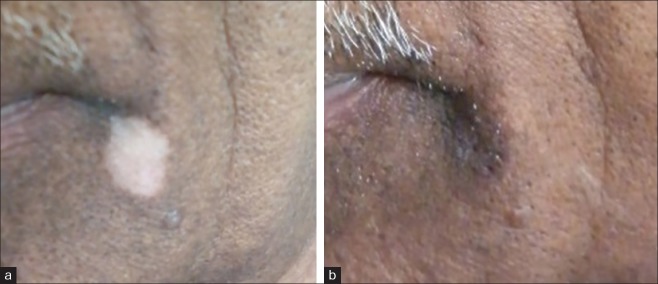
Figure 2.
(a) Vitiligo lesion over the moustache before the procedure (b) Vitiligo lesion over the moustache area- 2 months after the procedure; excellent response to treatment with excellent color match
Figure 3.
(a) Vitiligo with leukotrichia over the scalp (b) Vitiligo with leukotrichia over the scalp after 2 months
The color of the repigmented area was compared with the adjacent normally pigmented area and was scored as excellent, good, and poor. Out of the 63 lesions that were treated, two (4.8%) failed to show repigmentation and have been considered as poor color match here. Of the 61 lesions that showed pigmentation, excellent color match was seen in 44 (72.1%) and good color match in 16 (26.2%). None of the patients who responded to treatment had a poor match [Chart 3]. Two lesions initially developed hyperpigmentation that gradually faded by 4-5 months to match the surrounding skin.
Chart 3.
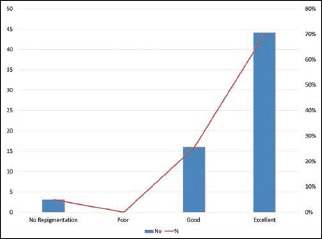
Color match
Two lesions were excluded while calculating the reduction in the area of vitilignous lesions as they were only leukotrichia and the percentage reduction of area could not be calculated. Out of the 61 lesions considered, the majority, i.e., 21 (34.4%) had >80% repigmentation, 16 (26.2%) of which had 100% repigmentation. Five lesions (8.2%) responded with < 20% repigmentation and one (1.6%) did not show any pigmentation at all [Chart 4]. Out of the 63 lesions, 46 lesions had leukotrichia. Out of these 46 lesions, 11 (23.9%) showed improvement in leukotrichia.
Chart 4.
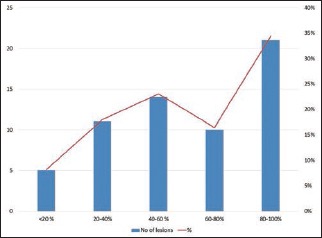
Percentage reduction in size
Difference between the initial and the final sizes of the lesion was also statistically analyzed using Wilcoxon signed-rank test and was found to be highly significant (P < 0.005). As the data were found to be nonparametric, Spearman's rank correlation coefficient was calculated to find the correlation between age, duration of vitiligo, and duration of stability of vitiligo. No correlation was found between the age, duration of vitiligo, or duration of stability and response to treatment. Correlation with sex was also analyzed (using Mann-Whitney U test) and was not found to be statistically significant.
No major complications were seen in this procedure. The donor site showed no complications in any of the 50 patients included in the study. Four (6.35%) patients showed complications at the recipient site. One of the patients had intraoperative bleeding at the recipient site that was controlled using figure-of-8 suture ligation. One of the patients presented with inclusion cyst at the recipient site due to deep impaction of the hair follicle. Two patients showed reactivation of vitiligo after 3 months and 4 months of the procedure, respectively. Correlation between the procedure and reactivation could not be conclusively established.
In nine cases out of the 63 lesions, FUT was combined with other modalities. The purpose of combining two modalities was to assess if FUE on nonglabrous skin could be combined with other vitiligo surgeries on glabrous skin in order to enhance the cosmetic result. In two cases, FUT was done as a touch-up procedure after mini punch grafting (MPG) while in two cases, it was done in the hairy area, along with MPG in nonhairy area(s). In one case each, follicular unit transplant was combined with suction blister grafting (SBG), ultrathin epidermal sheet grafting (UTESG), and epidermal cell suspension (ECS) for the nonhairy area(s). In all the cases, the outcome was found to be very good with excellent color match except in one case of combination with ECS. The poor response was due to poor uptake of the graft.
DISCUSSION
The clinical observation that early repigmentation usually appears at the orifice of hair follicles indicates that a melanocyte reservoir may reside in the hair follicles. Follicular unit grafting is based on the transfer of this reservoir of melanocytes to serve as a source of pigmentation for the depigmented vitiligo lesions.
The presence of stem cells in the hair follicle has been established time and again. As early as in 1959, Starrico found that there were some DOPA-negative, amelanotic melanocytes in the outer root sheaths (ORSs) of normal hair follicles that showed light cytoplasm and dark blue nuclei by DOPA-toluidine blue stain.[2] These melanocytes did not synthesize melanin under normal circumstances but became active to produce melanin when stimulated by ultraviolet light or by removal of the epidermis and the upper part of hair follicles by dermabrasion. The author concluded that these amelanotic melanocytes could move up long the regenerated epidermis and mature morphologically and functionally.[2,3,4] In 1980, Ortonne et al. used DOPA stain and scanning electron microscopy (SEM) to examine the repigmented skin after treatment with PUVA and found that pigment islands had follicular cores and that there was a melanocyte reservoir in the human hair follicles that maybe the reservoir for the melanocytes found in the repigmenting skin.[5] Cui et al. studied the different stages of repigmentation in vitiligo and conclusively demonstrated the existence of this melanocyte reservoir in the ORS of the hair follicles.[6]
Vitiligo is a process in which only active melanocytes in the ORS are destroyed while the inactive melanocytes are preserved, thereby serving as the only source for repigmentation. Recovery from vitiligo is initiated by these inactive melanocytes followed by upward migration to the nearby epidermis to form perifollicular pigmentation and downward migration to the hair matrices to produce melanin. Follicular unit transplant is aimed at reintroducing the stem cells into the vitiliginous area, which then replenish the dwindling melanocyte stores.
Follicular unit transplant was first introduced to repigment vitiligo patches in 1998. In the one study by Na et al.,[7] perifollicular repigmentation around the grafted hair was observed in 71% of patients within 2-8 weeks. In cases of localized/segmental vitiligo, perifollicular pigmentation was seen in 82% of patients and the study concluded single hair grafting to be an effective method for treating localized/segmental vitiligo, especially on hairy parts of the skin including the eyelids and eyebrows and for small areas of vitiligo. In 2011, Malakar et al. conducted a study on three patients with five vitiliginous patches. They have reported success in all the five lesions with excellent color matching.[8] Single follicular unit transplant conducted by Kumaresan in 2011[9] showed excellent repigmentation after 4-8 weeks with no recurrences in a case of vitiligo.
There are many advantages of this procedure. A single hair contains more melanocytes than normally pigmented nonglabrous skin and thus, provides a larger melanocyte and stem cell reservoir. Though the appearance of pigment is delayed as compared to the other modalities, the color match is much more acceptable than that with other methods. The cause of a more acceptable color match in hair transplantation than in other methods could be related to the stem cell migration from the graft and then location-specific transient that amplifies cells proliferation. As the occiput is the donor site, we can completely avoid the complications of other grafting procedures (e.g., punch grafting, split-thickness skin grafting, and blister technique); all these have visible scar and/or hypo- or hyperpigmentation at the donor site. The method produces minimal postoperative hyperpigmentation in the grafted sites unlike procedures like autologous suction blister grafts. This method can be easily applied to a small area of vitiligo. It can be performed in the eyelash area or at an angle of the mouth where performing other surgical methods, such as epidermal grafting or minigrafting, are difficult.[7,10] The procedure has the potential to become the method of choice to repigment the vitiligo patch having leukotrichia.
Though the surgical modalities are important in the treatment strategies of vitiligo, all of them have their limitations. Each patient of vitiligo should be individualized for the technique he/she will undergo. The use of this method to repigment vitiligo over the nonhairy areas is still a matter of controversy. The procedure can become cumbersome if it has to be used for a larger area. Also, vitiliginous skin heals slowly with this method because the grafted melanocytes require a long time to spread.[7,10]
Three studies previously carried out on follicular unit grafting have used the strip method for the extraction of follicles, i.e., the FUT method. A strip of the scalp was removed from the occipital/postauricular region and the hair follicles were dissected. In the present study, we used 1-mm biopsy punch to obtain follicles from the donor area, thereby minimizing scarring, postoperative pain, and downtime. This technique is popularly known as the FUE technique. All the three previous studies have dissected the hair follicles to obtain single hair follicles that were then transplanted onto the recipient site. On the contrary, the present study transplants the whole follicular unit onto the recipient sites.
Follicular unit is the term given to the hair follicles emerging from the scalp in groups; histologically, these units are comprised of one-four terminal and one-two vellus hairs that form a distinct group bounded by a circumferential band of adventitial collagen, the perifolliculum.[11] The follicular unit is held together by the arrector pili muscle and forms a pyramid-shaped bundle with the tight zone of attachment of the arrector pili forming the apex and splaying the hair bulbs loosely adherent to the adventitious tissue below. Once the hold of the arrector pili is weakened, the inferior segment can be extracted easily. Another advantage of this method is that the hair follicles are intact in their surrounding milieu, which may enhance their uptake and growth.
The authors have previously reported a case of a 12-year-old female with a stable vitiligo patch with leukotrichia on the eyebrow where FUT using this method was used. Repigmentation was noted in 6 weeks and complete pigmentation was seen at 12 weeks. Leukotrichia resolved over a period of 6 months. No recurrence was noted at the end of 6 months follow-up with excellent color match.[12]
CONCLUSION
FUE is a safe and inexpensive method of surgical repigmentation. It does not require special equipment or a sophisticated operation theater setting. Small and stable lesions affecting the hairy areas can be easily and effectively treated by this method. As the hair follicles are a reservoir of both active and inactive melanocytes, they have a better cosmetic outcome as compared to other techniques. Leukotrichia was also found to improve with this procedure, though the time taken was longer as compared to the skin lesions. This procedure was also found to be useful in combination with other procedures to enhance the cosmetic results.
Using FUE rather than the strip method (FUT) simplifies the procedure and reduces the chances of complications. Avoiding dissection of the follicular units further simplifies the procedure while also maintaining the internal milieu of the hair follicles and helps to achieve better cosmetic results. As compared to the other surgical modalities available, complications of this procedure are minimal and the color match is excellent. However, this procedure is best done on small lesions involving the hairy areas of the body.
Financial support and sponsorship
Received a grant of  45,500 from IADVL L’Oréal Hair and Skin Research Grant 2013.
45,500 from IADVL L’Oréal Hair and Skin Research Grant 2013.
Conflicts of interest
There are no conflicts of interest.
REFERENCES
- 1.Prasad D, Gupta S. IADVL Dermatosurgery Task Force. Standard guidelines of care of vitiligo surgery. Indian J Dermatol Venerol Leprol. 2008;74(Suppl):S37–45. [PubMed] [Google Scholar]
- 2.Staricco RG. Amelanotic melanocytes in outer sheath of the human hair follicle. J Invest Dermatol. 1959;33:295–7. doi: 10.1038/jid.1959.154. [DOI] [PubMed] [Google Scholar]
- 3.Staricco RG. Mechanism of migration of the melanocytes from the hair follicle into the epidermis following dermabrasion. J Invest Dermatol. 1961;36:99–104. [Google Scholar]
- 4.Staricco RG, Miller-Milinska A. Activation of amelanotic melanocytes in the outer root sheath of the human hair follicle following ultra violet rays exposure. J Invest Dermatol. 1962;39:163–4. doi: 10.1038/jid.1962.97. [DOI] [PubMed] [Google Scholar]
- 5.Ortonne JP, MacDonald DM, Micoud A, Thivolet J. PUVA-induced repigmentation of vitiligo: A histochemical (spli-DOPA) and ultrastructural study. Br J dermatol. 1979;101:1–12. doi: 10.1111/j.1365-2133.1979.tb15285.x. [DOI] [PubMed] [Google Scholar]
- 6.Cui J, Shen LY, Wang GC. Role of hair follicles in repigmentation of vitiligo. J Invest Dermatol. 1991;97:410–6. doi: 10.1111/1523-1747.ep12480997. [DOI] [PubMed] [Google Scholar]
- 7.Na G, Seo SK, Choi SK. Single hair grafting for the treatment of vitiligo. J Am Acad Dermatol. 1998;38:580–4. doi: 10.1016/s0190-9622(98)70121-5. [DOI] [PubMed] [Google Scholar]
- 8.Malakar S, Dhar S. Repigmentation of vitiligo patches by transplantation of hair follicles. Int J Dermatol. 1999;38:237–8. [PubMed] [Google Scholar]
- 9.Kumaresan M. Single-hair follicular unit transplant for stable vitiligo. J Cutan Aesthet Surg. 2011;4:41–3. doi: 10.4103/0974-2077.79191. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Malakar S, Na GY, Lahiri K. Transplantation of hair follicles for vitiligo. In: Gupta S, Olsson MJ, Kanwar AJ, Ortonne JP, editors. Surgical Management of Vitiligo. 1st ed. Oxford: Blackwell; 2007. pp. 123–7. [Google Scholar]
- 11.Bernstein RM, Rassman WR, Szaniawski W, Halperin A. Follicular transplantation. Int J Aesthetic Restorative Surg. 1995;3:119–32. [Google Scholar]
- 12.Sacchidanand S, Thakur P, Purohit V, Sujaya SN. Follicular unit extraction as a therapeutic option for Vitiligo. J Cutan Aesthet Surg. 2013;6:229–31. doi: 10.4103/0974-2077.123413. [DOI] [PMC free article] [PubMed] [Google Scholar]