Abstract
Brown tumor affects multiple bones in the body with variable clinical symptoms, which may be misdiagnosed as multiple bone metastases or primary bone tumor. In the present case report, we report the usefulness of 99mTc-MDP bone scan and 99mTc-MIBI whole body scan in differentiating brown tumor of hyperparathyroidism from giant cell tumor.
Keywords: Bone scan, brown tumor, giant cell tumor, 99mTc MIBI scan, primary hyperparathyroidism
Introduction
Brown tumors are not true tumors and arise in the settings of excess osteoclast activity caused by excretion of parathyroid hormone in association with hyperparathyroidism. Brown tumor affects multiple bones in the body with variable clinical symptoms, which may be misdiagnosed as multiple bone metastases or primary bone tumor. Microscopically, giant cell tumor (GCT) and brown tumor of hyperparathyroidism (BTH) have a similar finding containing giant cells and spindle-shaped cells in fibrous matrix but treatment-wise, both these conditions are totally different.
Case Report
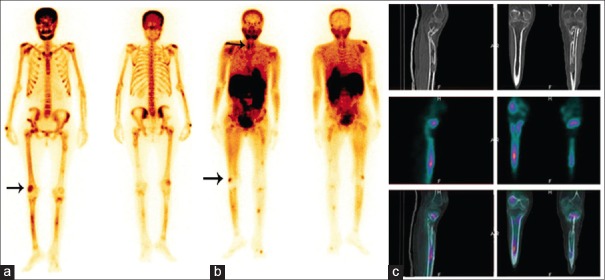
A 42-year-old female patient presented with history of bone pain in the upper region of the left tibia. Magnetic resonance imaging (MRI) showed an expansile lesion in the metadiaphyseal region of the upper one-third region of the left tibia. A biopsy from tibial lesion showed large osteoclastic giant cells in a background of spindle-shaped cells and mononuclear cells. A diagnosis of giant cell tumor (GCT) was made and the patient was treated with curettage and bone grafting followed by local radiotherapy. Subsequently, bone scan was done for metastatic workup of the GCT. (a) 99mTc-methoxyisobutylisonitrile (MIBI) bone scan Figure 1a showed multiple foci of increased uptake in the skull bones, mandible, and axial and appendicular skeleton with focally increased uptake in the upper and lower ends of both femurs, both tibia, both shoulder joints and forearm bones. The bone scan findings were more consistent with metabolic bone disease than with metastatic bone disease. Biochemical tests were obtained and the values (serum calcium-15.09 mg/dL, serum phosphorus-2.38 mg/dL, ALP-943.24U/L and iPTH-1987 pg/mL) were in favor of metabolic bone disease. The patient was subjected to 99mTc-MIBI dual-phase (DP) parathyroid scan and whole body scan (WBS). (b) 99mTc-MIBI WBS Figure 1b showed increased uptake in the mandible, upper and lower ends of the right femur, both tibial bones and around the shoulder joints, similar to the bone scan and single photon emission computed tomography/computed tomography (SPECT/CT) of lower limb Figure 1c showed MIBI avid lytic-cystic lesions in the lower end of the right femur and mid shaft of both tibial bones.
Figure 1.
Tc99m methylene diphosphonate bone scan (a) showing multiple foci of increased uptake in the skull bones, mandible, axial and appendicular skeleton with focally increased uptake in the upper and lower ends of both femurs, both tibia, both shoulder joints and forearm bones. 99mTc-MIBI WBS (b) showing increased uptake in the mandible, upper and lower ends of the right femur, both tibial bones, and around the shoulder joints, similar to that of the bone scan and SPECT/CT (c) of the lower limb that showed MIBI avid lytic-cystic lesions in the lower end of the right femur and midshaft of both tibial bones
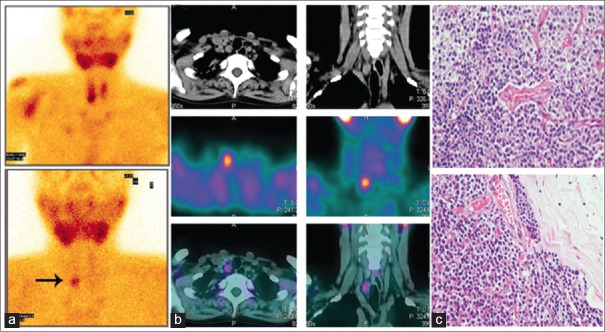
DP 99mTc-MIBI parathyroid scan of the neck Figure 2a showed focally increased tracer uptake in relation to the inferior pole of the right lobe of thyroid gland, which on SPECT/CT Figure 2b of the neck was localized to an isodense lesion of 1.3 × 1.2 cm size inferior to lower pole of the right lobe of thyroid gland suggestive of right inferior parathyroid adenoma, which later on was confirmed on histopathology [Figure 2c]. The patient underwent surgery and histopathology that showed chief cells, clear cells and tumor cell with thick capsule (hematoxylin and eosin stain, 400x magnification) confirming diagnosis of parathyroid adenoma. 99mTc-MIBI WBS [Figure 3a and b] acquired 2 months after surgical removal of parathyroid adenoma (Figure 3a and b) showed complete resolution of MIBI avid lesions as compared to presurgical scan and DP parathyroid scan Figure 3c showed no abnormal MIBI avid lesion in the neck. The clinical symptom and laboratory results of the patient also improved.
Figure 2.
DP 99mTc-MIBI parathyroid scan of the neck (a) showing focally increased tracer uptake in relation to the inferior pole of the right lobe of thyroid gland, which on SPECT/CT of the neck (b) localized to an isodense lesion inferior to lower pole of the right lobe of thyroid gland, suggestive of right inferior parathyroid adenoma that was confirmed on histopathology (c)
Figure 3.
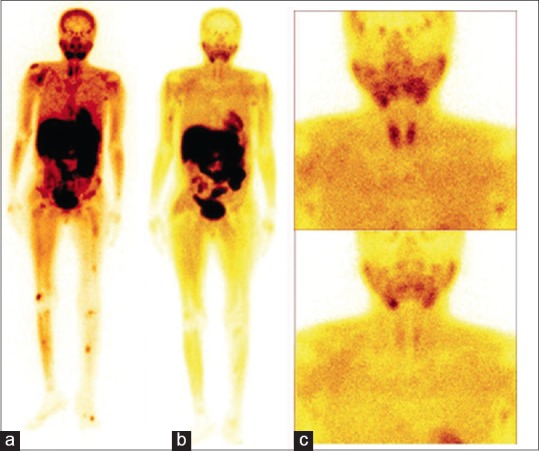
99mTc-MIBI WBS scan acquired 2 months after surgical removal of parathyroid adenoma (a and b) shows complete resolution of MIBI avid lesions as compared to presurgical scan and DP parathyroid scan (c) showing no abnormal MIBI avid lesion in the neck
Brown tumor contains giant cells, spindle-shaped cells and a background of fibrous matrix. Microscopically, BTH, giant-cell granuloma,[1] and GCT[2] have similar findings because all these conditions contain giant-cell lesions. Differential diagnoses of all these conditions may not be possible without knowledge of the clinical features, radiological findings, and laboratory results. Brown tumor commonly affects the jaws, skull, pelvis, clavicle, ribs, femurs and spine.[2,3,4,5] The CT scan findings are not specific for brown tumor[2] and show multilobular cystic change.[6,7] Multiple bony lesions of brown tumor may be misdiagnosed on CT scan as metastatic carcinoma, bone cysts, and especially GCT.[8] 99mTc-MDP bone scan is an effective method for distinguishing BTH from multiple bone metastases.[9]
Conclusion
In conclusion, diagnosis of BTH must be considered in patients with multiple bone lesions, elevated calcium and alkaline phosphatase (ALP), and mimicking multiple bone metastases especially from GCT, as these conditions have similar histopathological and radiological findings.[10,11,12] The 99mTc-MDP bone scan and 99mTc-MIBI WBS are useful in differentiating and managing these conditions.
Footnotes
Source of Support: Nil
Conflict of Interest: None declared.
References
- 1.Kocher MS, Gebhardt MC, Jaramillo D, Perez-Atayde AR. Multiple lytic skeletal lesions and hypercalcemia in a 13-year-old girl. Clin Orthop Relat Res. 2000;374:298. doi: 10.1097/00003086-200005000-00027. [DOI] [PubMed] [Google Scholar]
- 2.Takeshita T, Tanaka H, Harasawa A, Kaminaga T, Imamura T, Furui S. Brown tumor of the sphenoid sinus in patient with secondary hyperparathyroidism: CT and MR imaging findings. Radiat Med. 2004;22:265–8. [PubMed] [Google Scholar]
- 3.Kanaan I, Ahmed M, Rifai A, Alwatban J. Sphenoid sinus brown tumor of secondary hyperparathyroidism: Case report. Neurosurgery. 1998;42:1374–7. doi: 10.1097/00006123-199806000-00113. [DOI] [PubMed] [Google Scholar]
- 4.Keyser JS, Postma GN. Brown tumor of the mandible. Am J Otolaryngol. 1996;17:407–10. doi: 10.1016/s0196-0709(96)90075-7. [DOI] [PubMed] [Google Scholar]
- 5.Fasanelli S, Graziani M, Boldrini R, Bosman C. “Brown tumor” of the maxilla. Pediatr Radiol. 1992;22:142–4. doi: 10.1007/BF02011319. [DOI] [PubMed] [Google Scholar]
- 6.Smith J, Huvos AG, Chapman M, Rabbs C, Spiro RH. Hyperparathyroidism associated with sarcoma of bone. Skeletal Radiol. 1997;26:107–12. doi: 10.1007/s002560050202. [DOI] [PubMed] [Google Scholar]
- 7.Erem C, Hscihasanoglu A, Cinel A, Ersöz HO, Reis A, Sari A, et al. Sphenoid sinus brown tumor, a mass lesion of occipital bone and hypercalcemia: An unusual presentation of primary hyperparathyroidism. J Endocrinol Invest. 2004;27:366–9. doi: 10.1007/BF03351064. [DOI] [PubMed] [Google Scholar]
- 8.Scholl RJ, Kellett HM, Neumann DP, Lurie AG. Cysts and cystic lesions of the mandible: Clinical and radiologic-histopathologic review. Radiographics. 1991;19:1107–24. doi: 10.1148/radiographics.19.5.g99se021107. [DOI] [PubMed] [Google Scholar]
- 9.Jordan KG, Telepak RJ, Spaeth J. Detection of hypervascular brown tumors on three-phase bone scan. J Nucl Med. 1993;34:2188–90. [PubMed] [Google Scholar]
- 10.Joyce JM, Idea RJ, Grossman SJ, Liss RG, Lyons JB. Multiple brown tumors in unsuspected primary hyperparathyroidism mimicking metastatic disease on radiograph and bone scan. Clin Nucl Med. 1994;19:630–5. doi: 10.1097/00003072-199407000-00016. [DOI] [PubMed] [Google Scholar]
- 11.Hsieh MC, Ko JY, Eng HL. Pathologic Fracture of the distal femur in osteitis fibrosa cystica simulating metastatic disease. Arch Orthop Trauma Surg. 2004;124:498–501. doi: 10.1007/s00402-004-0697-y. [DOI] [PubMed] [Google Scholar]
- 12.Pai M, Park CH, Kim BS, Chung YS, Park HB. Multiple brown tumors in parathyroid carcinoma mimicking metastatic bone disease. Clin Nucl Med. 1997;22:691–4. doi: 10.1097/00003072-199710000-00006. [DOI] [PubMed] [Google Scholar]