Abstract
Background
In Cameroon the rate of infant-juvenile mortality remains high and most death occur in the community. Mortality statistics is usually based on hospital data which are generally insufficient and less reliable. In a context where legislation on death registration is not applied, and where conventional autopsy is not often done, verbal autopsy (VA) provides information on mortality. This study tried to experiment this method and also analyses the therapeutic pathway of a group of children who died before arrival at the emergency department of a pediatric hospital.
Methods
A cross sectional descriptive study was carried out on children who died before arrival, at the Mother and Child Centre of the Chantal Biya Foundation in Yaounde, between October 2013 and April 2014. The addresses of parents or relatives of the deceased children were registered at the start of the study. Each respondent was interviewed 5 to 6 weeks later at the residence of the deceased child, with the aid of a VA questionnaire. Information obtained was on the socio-demographic characteristics of the families, past history of deceased, clinical presentation and the different health care services sought before the death.
Results
In all, 40 children who died were included in the study. The majority of the deceased children were less than 5 years (82.5%) with 50.0% being less than 1 year of age. Almost half of them (47.5%) had been ill for more than 24 hours, 40% for more than 3 days. Up to 50.0% had not been taken to a health facility. Most of them had visited 2 or 3 other health facilities before dying on the way to our hospital. Auto medication was frequent (42.5%); parents initially recourse to drugs which were either bought or obtained from home. Some parents (25.0%) brought their children only after they had been to a private dispensary, or a traditional healer (15.0%). Only 7.5% benefited from consultation in a public health facility and 2.5% resorted to prayers and incantations. Whatever the kind of care sought, the choice was mostly guided by its proximity (32.5%), advice from a relative (27.5%) or its affordability.
Conclusions
It is of crucial importance that the government reinforces the measures to avoid the existence of clandestine health centres and check the competence of health care professionals. Improving referral/counter referral system will permit the limitation of fatal medical errors.
Keywords: Children, death before arrival at hospital, verbal autopsy (VA), therapeutic itinerary
Introduction
Statistics from hospitals and other health structures underestimate the impact of diseases in developing countries (1). Different authors have shown that very few patients recourse to a health facility as first intention (2). The search for informal health services is therefore very common (3). These are offered by traditional healers, nurses and doctors working in private practice, with their services being dictated by cost, distance, the type of treatment and the illness (4). Due to the economic situation of Cameroon, many clandestine health centres are rapidly proliferating in rural as well as urban areas. These offer inappropriate health services, and instead of reducing the geographical barriers to health, they contribute in part to the aggravation of the health status of patients, due to their inadequate technical platform. Also, communication between health professionals in different levels of the health pyramid is poor (5). The dysfunction of the referral/counter referral system doesn’t also facilitate the continuity of health care in our context. As a result of this, families recourse to others services before deciding to bring their children to the hospital. Children, who have been subjected to these, are 6 times more likely to be readmitted in the hospital (6). Returning to a different health structure other than the former increased the risk of death in the month following the previous hospital admission (7). In these conditions medical errors will be equally common. These have been reported in paediatrics services in developed regions (8), the same situation can be disastrous in our resource limited context (8). According to different authors, the probability of death of children after hospitalisation (1–18%) is greater than that during hospitalisation (9). Many die in the community (10) or before arrival in the hospital. Delay, either in recognising signs of gravity of the disease or in seeking health care will explain such a scenario (11). It is for this reason that, some children arrive at the emergency services already death during course of their transportation to the hospital. Given the emotional state of the family members after the death, it is not usually possible to precise the circumstances of death. Verbal autopsy (VA) helps us to describe the health seeking pathway and the reasons that guided the choice of health services visited by parents before death occurred.
Methods
It was a cross sectional descriptive study which started in the paediatric emergency unit of the Mother and Child Centre of the Chantal Biya Foundation (MCC/CBF) of Yaounde and continued at the home of the children. Children who arrived already deceased between June 2013 and April 2014 were included.
Procedure and methodology
Data collection was done in two stages; first we identified children who died before arrival at the hospital, as well as at least one relative who accompanied them. Then, an arrangement was made for a visit at home which was done about 5 to 6 weeks later. The time interval was short enough to guarantee a good recall what happened during the episode of illness. We interviewed the family with help of two types of WHO standard VA questionnaire. Depending on the age of the deceased, we either submitted a questionnaire for infants up to 4 weeks of age or that for children 4 weeks to 14 years (12).
One parent or close relative responded to the questions; the respondent must have lived with the deceased child during the last month and during the period of illness. Mothers were prioritised due to the fact that they were better placed to recall of the events leading up to the death. Sometimes mothers refused to talk about the death of their children and in such circumstances, information was got from another close family member. The latter most have lived with the child in the last month and most have followed up the child’s treatment during the last episode of illness. Information obtained included, age of the deceased, the frequency of visit to a health facility during the last month of life, the different health services visited during the last illness, the reasons motivating choices for these sites and drugs administered. As for the respondent the data collected included their age, level of education, and the presumed cause of death.
Analyses of data on VA
The interpretation of the data was by the physician review method (11,13). It was done in two stages, firstly by two trained paediatricians, who individually attributed a direct and associated cause of death to each case. They independently assigned to each dead a medical cause following the World Health Organization international diseases classification (CIM10) (12). Afterward, their conclusion were compared and considered when they were concordant, if not, a 3rd pediatrician was requested for discussion with the previous two with the aim of harmonizing their points of view.
Statistical analysis
Data was analysed with the aid of the software program Epi Info7 and Excel 2007. Categorical data was presented as percentages. Whereas quantitative data were expressed in the form of median and interquartile range. The Khi2 was used to compare proportions and the difference was significant for P<0.05.
Ethical considerations
Ethical clearance was obtained from the Ethical Committee of the Faculty of Medicine and Biomedical Sciences of the University of Yaounde I. The goals of the study were explained to the parents and their informed consent obtained verbally or written prior to data collection. We scrupulously followed the appointment schedules given by the parents in order to respect their grief and mourning period.
Results
Socio demographic characteristics of the study population
Data was obtained from 40 out of 47 children who died before arrival at the emergency room. Their median age was 8 months (interquartile range, 3 to 11 months) with extremes ranging from 1 to 28 months (Figure 1). Mostly biological parents (87.5%) were interviewed, 52.0% being their mothers. The rest (12.5%) were either aunties, uncles or grandparents. Respondents were young, the youngest being, 19 years old and about half of them being less than 30.5 years (interquartile range, 26 to 36.5 years).They were mostly in free unions (65%) or single about one third of them (32.0%) had at least secondary school education. For more than two thirds of respondent, the deceased was the first child they had lost; 22.5% and 2.5% were experiencing the loss of a child for the second or third time respectively.
Figure 1.
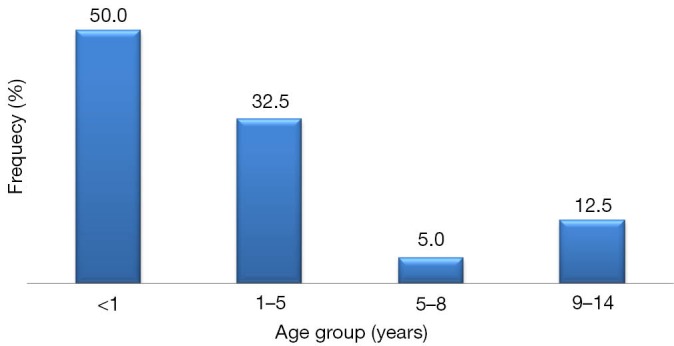
Distribution of patients with regards to age.
Therapeutic path before death
From the information obtained 40% of the children were sick for greater than three days, and 45% were died within 24 and 72 hours, 17.5% in less than 24 hours. As far as visits to health facilities were concerned, 29 that is close to three quarters (72.5%) had not been in contact with a health facility during the last month of their life. However, 17.5%, 5% and 5% had been, once, twice and thrice respectively at a health care service the last month of their life. Ten subjects had a history of previous hospitalisations, amongst whom, 3 (30.0%) died in less than 24 hours; 3 (30.0%) between the 2nd and 6th day and 4 (40.0%) above 6 days. Meningitis and malaria constituted the principal causes of death, 50.0% and 33.3% respectively. The majority of subjects (87.0%) had benefited from 2 to 3 modern medical or informal health services. Only 5% and 7.5% were at their first and fourth consultations respectively.
The first choice was that of illicit sales of drugs (42.5%). Some (15%) had visited a traditional healer (Figure 2). The children who hadn’t visited a health structure in the last month, had as first intention visited mostly a hospital during the last episode of their disease; half (51.7%) and 1/4 (24.1%) being in private and public structure respectively (Khi2 =40.398; P=0.007). Some (17.2%) were treated at home meanwhile, 7.8% were at a dispensary before dying their transport to the MCC/CBF.
Figure 2.
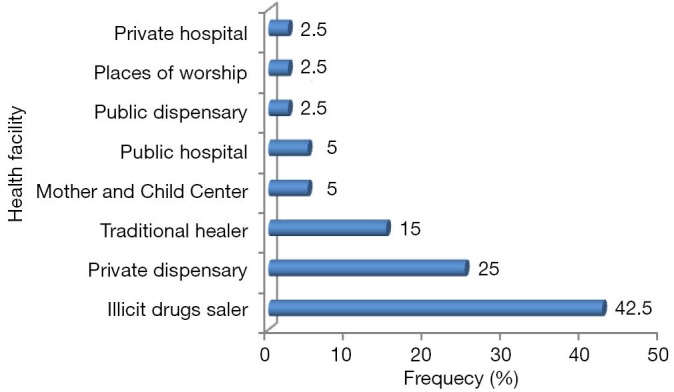
Health facility were first health care was given.
Seven of the children (17.5%) had visited a health facility in the month preceding their death. Among them, 67.1% consulted at a hospital during the last episode of their disease. Meanwhile, 28.6% of them didn’t seek any medical care or resorted to prayers and incantations before the death. Only one (14.3%) had been in a public dispensary. Their choice was guided most especially by proximity of the health facilities (32.5%) and advice of a close relative (27.5%). Familiarity with the health facility and its affordability also influenced the choice of the health facilities, in 20% of cases.
Concerning those who had visited a second health facility, second recourse, private health facilities were mostly visited (73.3%) against 23.7% for public structures, and 2.6% for traditional healer. The choice was influenced by advice from a relative (44.7%), affordability (36.8%) and habit (18.4%).
Finally three patients visited three health facilities during the last episode of the illness. These were a private or public dispensary or public hospital, each representing 33.3% of cases respectively and following the same advices.
Causes of death according to respondents and treatment administered
More than a third of respondents (37.5%) believed that their child had died of anaemia, respiratory problems (12.5%), poor management (10.0%), diarrhoea (7.5%) and HIV/AIDS (5.0%). On rare occasions intoxication, malnutrition, intestinal occlusion, prematurity, and trauma were mentioned as the cause of death, representing 2.5% each. Some respondents (12.5%) didn’t have any idea about the cause of their children’s death. However following their description or from information recorded in the hospital books, 34 (87.0%) subjects had benefited at least from some treatment before death. The duration of treatment was less than 4 days before death in 75.5%. It was administered as monotherapy, and equally in the form of combination of several drugs associated with traditional concoctions (Table 1).
Table 1. Health structure utilization during the last month of life and during the fatal episode of illness.
| Item | Number of deceased | Percentage (%) |
|---|---|---|
| Number of contacts with a health facility during the last month of life | ||
| 0 | 29 | 72.5 |
| 1 | 7 | 17.5 |
| 2 | 2 | 5.0 |
| 3 | 2 | 5.0 |
| Any previous hospitalisation | ||
| Yes | 10 | 25.0 |
| No | 30 | 75.0 |
| Number of health facilities visited during the last episode of fatal ill-health | ||
| 1 | 2 | 5.0 |
| 2 | 14 | 35.0 |
| 3 | 21 | 52.5 |
| 4 | 3 | 7.5 |
| Reason for choice of first health visit during the last episode of fatal ill-health (n=40) | ||
| Advice from someone close | 11 | 27.5 |
| Proximity | 13 | 32.5 |
| Habit | 8 | 20.0 |
| Affordability | 8 | 20.0 |
| Reason for the second choice for health visit during illness (n=24) | ||
| Advice from relatives | 13 | 54.2 |
| Habit | 3 | 12.5 |
| Affordability | 8 | 33.3 |
| Reason for 3rd choice during recourse to health care during fatal illness (n=3) | ||
| Advice from a relative | 1 | 33.3 |
| Habit | 1 | 33.3 |
| Affordability | 1 | 33.3 |
Discussion
Death of children before arrival to the Emergency room is common in our hospitals, but the exact statistics are not well known. The characterisation of these subjects cannot be better done without the aid of the VA in our setting where this method is embryonic. VA is useful to help determine cause of death close to that diagnosed by the clinician (14). We used it to determine the therapeutic path taken by the deceased before arrival at our hospital. The delay observed between the occurrence of death and the interview permitted the establishment of a faith relationship with the affected families, so as to reduce the frequency of refusal to participate in the study and thus obtain reliable information.
Our results revealed that death rates were highest in children less than 2 years; this is similar to what was found in Zimbabwe (15). Also, just as in other studies (16), more than half of study participants had not been seen in any health structure despite the fact that many (40%) had been sick for at least 3–8 days or more. Different authors also showed that most deaths occurred in the community (10) partly due to the delay in recognizing signs of gravity, or delay in seeking health care (11,17). Very few families could recognize specific symptoms of illness. This is true in our milieu, where the integrated management of the child illness (IMCI) is not yet well developed and the pressure from traditional healers is high. There may also be a time lapse between the recognition of danger signs and seeking formal health care (18). However, this wasn’t the case in Newcastle where mothers easily recognised the severity of symptoms in their children and knew equally how to seek medical attention (19).
Studies also reveal that, access to health care is determined by the socio-economic status of the families of the children (20,21). Financial barriers were identified as a cause of absence of health care (22,23). Mothers interviewed were mostly in free unions in their relationships. It has been shown that the absence of a health insurance policy and the fact that children were from single mothers, made them less inclined to visit a health structure in the course of a year (20). Subscription to insurance could modify mothers’ attitudes so that, those with lower educational backgrounds, or the single mother sought health care more frequently than the most educated one or those who lived in couple (20). Meanwhile educational level or the ability to count can influence the knowledge of an illness and not health care seeking by mothers (24). This reason however is not applicable in the case of sick neonates in developing countries (25). In this study, mothers were mostly in free unions (65%) or single and about one third (32.0%) reached the level of secondary school. The perception of illness and degree of anxiety of mothers as concerns the state of health of their children will influence their decision to seek health care (26). In case their children were faced with health problems, the parents relied more on the advice of relatives in order to adopt a particular attitude. In our study, the advice of relatives justified the recourse to certain healthcare after the trials of certain common auto medication which were not helpful. In Senegal, some authors thought that the sale of illicit drugs was an asset as it helped in the adaptation of lifestyle of the population (27). Road side drugs favoured certain social relations, despite the fact that it was impossible to differentiate the good from the bad (28). In Cameroon, 20% of patients obtain drugs without any prescription and 30% of prescribed drugs are not bought (29). This means that even drugs prescribed formally will not be respected and because of lack of information provided to them, drugs preferred by parents will not always be appropriate to the health status of their children.
Health care provided by illegal health centres is of poor quality; because the personnel are not usually qualified and are often not supervised. Studies have shown that errors in paediatric prescriptions are frequent even in authorized/health facilities (8) this will be the same and even worse in our context. The practice of all components of the integrated management of childhood illness is therefore a necessity. It permits the reinforcement of capacities of personnel, and the community health workers close to families so as to permit early management of ill-health in children (30). Such interventions have permitted mothers to ameliorate their capacity to recognise danger signs in neonates and thus seek appropriate health care (31,32). In our context however, parents have less confidence in public health facilities and prefer private structures (32). This has been illustrated in this study in which parents prefer to seek health care in private health facility. We noted that certain subjects had sought health care from several structures before dying. Some authors have shown that, nearly 3% of children have had at least 4 hospitalisations per year (33). The probability of death occurring in children after a hospitalisation is higher than that which occurs during hospitalisation (9). Death is frequent in children who are re-hospitalised, especially when there is lack of communication between the doctors at different levels, during referral or during discharge (5). Health facilities offer opportunities, where parents are advised on the attitude to adopt depending on the evolution of their children’s disease. Many authors think that communication will permit avoiding errors during drug prescription (34).
Conclusions
Apart from deaths which occurred within 24 hours of the onset of ill-health, children who died before arrival at the health facility had received some form of in health care. In order to limit sudden death of children in communities; sensitisation of families on the dangers of inappropriate health facilities, will help them to seek appropriate medical attention for their children, early enough. Parent sensitization for recognition of the danger signs will permit them to seek health care early for their children. It is of crucial importance that the government reinforces measures to avoid clandestine health centres, as well as control the competence of health professionals. This concerns paramedical health staffs which constitute the main human resources component of our health work force. Amelioration of the referral/counter-referral system will limit fatal medical errors.
Acknowledgements
We are grateful to parents of deceased children who have agreed to receive us at home in spite of their pain. We are also grateful to all the staff of Mother and Child Center, Chantal Biya Foundation, especially those of the emergency unit for their great support.
Footnotes
Conflicts of Interest: The authors have no conflicts of interest to declare.
References
- 1.World Health Organization. Statistiques Sanitaires Mondiales 2009.
- 2.Commeyras C, Ndo JR, Merabet O, et al. Household behaviour regarding health and drug consumption in Cameroon. Sante 2006;16:5-12. [PubMed] [Google Scholar]
- 3.Burton DC, Flannery B, Onyango B, et al. Healthcare-seeking behaviour for common infectious disease-related illnesses in rural Kenya: a community-based house-to-house survey. J Health Popul Nutr 2011;29:61-70. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Tizio S, Flori YA. L’initiative de Bamako: santé pour tous ou maladie pour chacun? Tiers-Monde 1997;38:837-58. [Google Scholar]
- 5.Kripalani S, LeFevre F, Phillips CO, et al. Deficits in communication and information transfer between hospital-based and primary care physicians: implications for patient safety and continuity of care. JAMA 2007;297:831-41. [DOI] [PubMed] [Google Scholar]
- 6.Moore C, Wisnivesky J, Williams S, et al. Medical errors related to discontinuity of care from an inpatient to an outpatient setting. J Gen Intern Med 2003;18:646-51. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Staples JA, Thiruchelvam D, Redelmeier DA. Site of hospital readmission and mortality: a population-based retrospective cohort study. CMAJ Open 2014;2:E77-85. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Walsh KE, Landrigan CP, Adams WG, et al. Effect of computer order entry on prevention of serious medication errors in hospitalized children. Pediatrics 2008;121:e421-7. [DOI] [PubMed] [Google Scholar]
- 9.Wiens MO, Pawluk S, Kissoon N, et al. Pediatric post-discharge mortality in resource poor countries: a systematic review. PLoS One 2013;8:e66698. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Koffi AK, Libite P, Moluh S, et al. Social autopsy study identifies determinants of neonatal mortality in Doume, Nguelemendouka and Abong-Mbang health districts, Eastern Region of Cameroon. J Glob Health 2015;5:010413. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Murray CJ, Lozano R, Flaxman AD, et al. Using verbal autopsy to measure causes of death: the comparative performance of existing methods. BMC Med 2014;12:5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.World Health Organization. Normes d’autopsie verbale: établissement et attribution de la cause de décès. 2009.
- 13.Du Loû AD, Pison G, Samb B, et al. L’évolution des causes de décès d’enfants en Afrique: une étude de cas au Sénégal avec la méthode d’autopsie verbale. Population 1996;51:845-81. [Google Scholar]
- 14.Aggarwal AK, Kumar P, Pandit S, et al. Accuracy of WHO verbal autopsy tool in determining major causes of neonatal deaths in India. PLoS One 2013;8:e54865. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Wolf BH, Ikeogu MO. Deaths at home and in hospital in Zimbabwe. Arch Dis Child 1992;67:600-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Senga P, Mayanda HF, Etokabeka-Mkanta F. Mortalité hors hôpital des enfants à Brazzaville. Médecine Afr Noire 1993;40:119-21. [Google Scholar]
- 17.Sinclair-Smith C, Dinsdale F, Emery J. Evidence of duration and type of illness in children found unexpectedly dead. Arch Dis Child 1976;51:424-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Dongre AR, Deshmukh PR, Garg BS. Perceptions and health care seeking about newborn danger signs among mothers in rural Wardha. Indian J Pediatr 2008;75:325-9. [DOI] [PubMed] [Google Scholar]
- 19.Pattison CJ, Drinkwater CK, Downham MA. Mothers’ appreciation of their children’s symptoms. J R Coll Gen Pract 1982;32:149-62. [PMC free article] [PubMed] [Google Scholar]
- 20.Heck KE, Parker JD. Family structure, socioeconomic status, and access to health care for children. Health Serv Res 2002;37:173-86. [PubMed] [Google Scholar]
- 21.Saito K, Korzenik JR, Jekel JF, et al. A case-control study of maternal knowledge of malnutrition and health-care-seeking attitudes in rural South India. Yale J Biol Med 1997;70:149-60. [PMC free article] [PubMed] [Google Scholar]
- 22.Srivastava NM, Awasthi S, Agarwal GG. Care-seeking behavior and out-of-pocket expenditure for sick newborns among urban poor in Lucknow, northern India: a prospective follow-up study. BMC Health Serv Res 2009;9:61. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Taffa N, Chepngeno G. Determinants of health care seeking for childhood illnesses in Nairobi slums. Trop Med Int Health 2005;10:240-5. [DOI] [PubMed] [Google Scholar]
- 24.Ciampa PJ, Vaz LM, Blevins M, et al. The association among literacy, numeracy, HIV knowledge and health-seeking behavior: a population-based survey of women in rural Mozambique. PLoS One 2012;7:e39391. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Herbert HK, Lee AC, Chandran A, et al. Care seeking for neonatal illness in low- and middle-income countries: a systematic review. PLoS Med 2012;9:e1001183. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Janicke DM, Finney JW, Riley AW. Children’s health care use: a prospective investigation of factors related to care-seeking. Med Care 2001;39:990-1001. [DOI] [PubMed] [Google Scholar]
- 27.Baxerres C, Le Hesran JY. Le marché parallèle du médicament en milieu rural au Sénégal: Les atouts d’une offre de soins populaire (Note de recherche). Anthropol Sociétés 2006;30:219-30. [Google Scholar]
- 28.Pale A, Ladner J. "Street" medication in Burkina Faso: local names, social relationships, and alleged therapeutic effects. Sante 2006;16:113-7. [PubMed] [Google Scholar]
- 29.Commeyras C, Ndo JR, Merabet O, et al. Health and drug consumption profile in Cameroon. Sante 2006;16:13-9. [PubMed] [Google Scholar]
- 30.Awasthi S, Verma T, Agarwal M. Danger signs of neonatal illnesses: perceptions of caregivers and health workers in northern India. Bull World Health Organ 2006;84:819-26. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Case ME. Abusive head injuries in infants and young children. Leg Med (Tokyo) 2007;9:83-7. [DOI] [PubMed] [Google Scholar]
- 32.Dongre AR, Deshmukh PR, Garg BS. A community based approach to improve health care seeking for newborn danger signs in rural Wardha, India. Indian J Pediatr 2009;76:45-50. [DOI] [PubMed] [Google Scholar]
- 33.Berry JG, Hall DE, Kuo DZ, et al. HOspital utilization and characteristics of patients experiencing recurrent readmissions within children’s hospitals. JAMA 2011;305:682-90. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Benjamin DM. Reducing medication errors and increasing patient safety: case studies in clinical pharmacology. J Clin Pharmacol 2003;43:768-83. [PubMed] [Google Scholar]


