Abstract
In recent decades, the use of nanomaterials has received much attention in industrial and medical fields. However, some reports have mentioned adverse effects of these materials on the biological systems and cellular components. There are several major mechanisms for cytotoxicity of nanoparticles (NPs) such as physicochemical properties, contamination with toxic element, fibrous structure, high surface charge and radical species generation. In this review, a brief key mechanisms involved in toxic effect of NPs are given, followed by the in vitro toxicity assays of NPs and prooxidant effects of several NPs such as carbon nanotubes, titanium dioxide NPs, quantum dots, gold NPs and silver NPs.
Keywords: Oxidative stress, Reactivity oxygen species, Cytotoxicity, Nanoparticles, Mechanism, Prooxidant effects
Introduction
Nanotechnology advancement in medical sciences led to the design and synthesis of nanostructures for biomedical applications. Due to unique properties of NPs such as small size (1-100 nm in diameter) and the greater surface area to volume ratio as well as different electronic, magnetic, optical and mechanical properties and also particle shape, these particles hold great interests in the various fields.1-6
It may seem that NPs do not have toxic effects. However, the greater surface area to volume ratio of these particles causes their higher chemical reactivity and results in increased production of reactive oxygen species (ROS). Indeed, the NPs surface area is a key factor in their intrinsic toxicity because of the interaction of their surfaces with biological system.7-10
ROS formation is one of the mechanisms of NPs toxicity which could cause oxidative stress, inflammation and consequent damages to the proteins, cell membrane and DNA. Therefore, assessment of nanoparticles toxicity is necessary in biomedical applications including drug delivery systems, gene delivery and therapeutic applications.11-14
Prooxidants are chemicals that induce oxidative stress through either creating reactive oxygen species or inhibiting antioxidants. NPs react with cells and induce their prooxidant effects via intracellular ROS generation involving mitochondrial respiration and activation of NADPH-dependent enzyme systems.15-17
NPs can activate the cellular redox system specifically in the lungs where the immune cells including alveolar macrophages (AM) and neutrophils act as direct ROS inducers. Professional phagocytic cells of the immune system including neutrophils and AMs induce remarkable ROS upon internalization of NPs via the NADPH oxidase enzyme system.16,18
In this review, we have focused on introducing in vitro toxicity assays for cytotoxicity assessment of nanoparticles. We have also reviewed toxic effect of several nanoparticles such as carbon nanotubes, titanium dioxide NPs, quantum dots, gold NPs and silver NPs.
Cytotoxicity assays of nanoparticles
Cytotoxicity assays are classified as in vivo and in vitro tests. In vivo toxicity assays (cell-based assay) are time-consuming and expensive and involve ethical issues but in vitro toxicity tests (cell cultured-based assay) are faster, convenient, less expensive and devoid of any ethical issues. Due to these advantages, in vitro assays are the first choice for toxicity assessment of most nanomaterials.19
In vitro methods include approaches for assessment of integrity of the cell membrane and the metabolic activity of viable cells. Evaluation of cell membrane integrity is one of the most common approaches to measure cell viability. It is based on the leakage of substances such as lactate dehydrogenase (LDH) that normally reside inside cells to the external environment and the measurement of LDH activity in the extracellular media. Alternatively, membrane integrity can be determined by penetration of dyes such as trypan blue and neutral red into the damaged cells and staining intracellular components. These dyes cannot enter living cells. Metabolic activity of viable cells could be determined through colorimetric assays, such as the MTT and MTS assays.20-23
Bioluminescent methods including methods using luciferase, which catalyzes the formation of light from adenosine triphosphate (ATP) are also commonly used as cell viability assays in which the number of surviving cells is determined by measuring the uptake and accumulation of neutral red dye and trypan blue after exposure to the toxicant.24-26 Among in vitro methods, LDH, MTT and MTS assay are most widely used for assessment of nanoparticles cytotoxicity (Table 1).27
Table 1. Some in vitro assays with type of NPs and cell types.
| Assay | Type of NPs | Type of cells (system) | References |
| MTT assay | QDs | Human embryonic kidney cells | 90 |
| TiO2 | Human erythrocyte/ lymphocyte cells | 59 | |
| Natural red | TiO2 NPs | Zebrafish embryos | 91 |
| LDH test | TiO2 NPs | Human kidney cells | 92 |
| CNTs | human pneumocytes cells | ||
| MTS assay | Ag NPs | mouse embryonic fibroblasts | 93 |
| Gold NPs | Mammalian cells | 94 | |
| Trypan blue | Gold NPs | mouse fibroblast | 78 |
| TiO2 NPs | human lung epithelial cells | 95 |
LDH test
In general, LDH test is a colorimetric assay that quantitatively measures LDH, a marker of cell membrane integrity, released from damaged cells into the culture media. This assay is a fast, simple and reliable method for determining cellular toxicity.28
MTT assay
MTT assay is another candidate assay for measurement of cytotoxicity of NPs. 3-(4,5-Dimethylthiazol-2-yl)-2,5-Diphenyltetrazolium Bromide, (MTT), is a yellow substance which reduces to purple insoluble formazan crystals by mitochondrial succinate dehydrogenases in viable cells. This method is directly related to the number of viable cells.29
MTS assay
In the MTS (3-(4,5-dimethylthiazol-2-yl)-5-(3-carboxymethoxyphenyl)-2-(4-sulfophenyl)-2H-tetrazolium) assay, viable cells will convert tetrazolium salt into a colored soluble formazan product by mitochondrial dehydrogenase enzymes. Indeed, in MTS assay, similar to MTT assay, a colorimetric product is formed. The formazan produced is directly proportional to the number of living cells in the culture.30
Toxicity mechanisms of nanoparticles
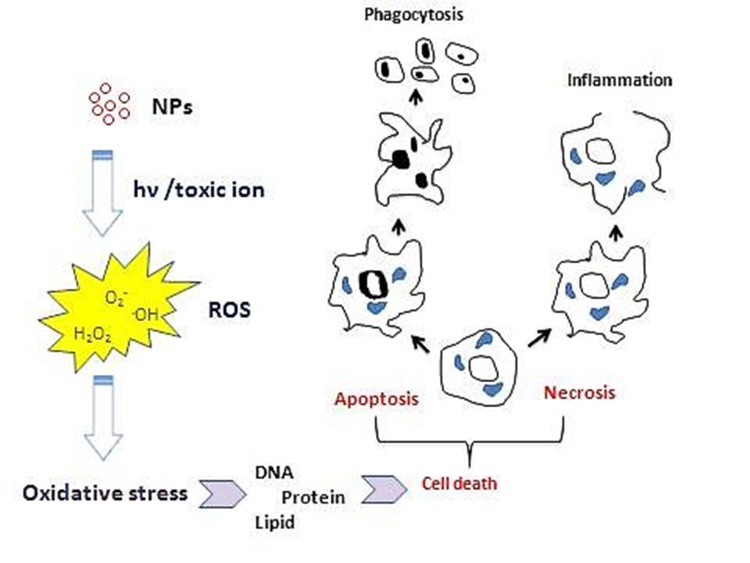
Physicochemical reactivity of NPs lead to the formation of free radicals or ROS including superoxide radical anions and hydroxyl radicals direct or indirect through activation of oxidative enzymatic pathways result in oxidative stress (Figure 1).31-36 In general, there are several sources for oxidative stress:
Figure 1.
ROS generation induced by NPs and their cytotoxicity mechanism.
Oxidant-generating properties of particles themselves as well as their ability to stimulate generation of ROS as a part of cellular response to nanoparticles
Transition metal-based nanoparticles or transition metal contaminants used as catalysts during the production of non-metal nanoparticles.
Relatively stable free radical intermediates present on reactive surfaces of particles.
Redox active groups resulting from functionalization of nanoparticles
The following briefly introduces cytotoxicity of some of nanoparticles such as carbon nanotubes, titanium dioxide NPs, quantum dots, gold NPs and silver NPs.
Cytotoxicity of carbon nanotubes
Carbon nanotubes (CNTs), fiber shaped nanostructures, are allotropes of carbon which are categorized as single wall carbon nanotubes (SWCNT) and multi wall carbon nanotubes (MWCNT). In addition to industrial uses, carbon nanotubes, due to their unique electrical, physical and thermal qualities hold great interest in biomedical applications.37-39
Numerous reports have shown that CNT could induce the ROS generation in multitudes of cell lines and activation of ROS-associated intracellular signaling pathways in a dose-dependent manner such as mitogen activated protein kinase (MAPK), activator protein-1 (AP-1) and nuclear factor kappa-light-chain-enhancer of activated B cells (NF-κB) in mesothelial cells.40-43
It has been reported that MWCNT are able to stimulate the release of the cytokines, IL-1β, TNF-α, IL-6 and IL-8 from mesothelial cells and macrophages. Murphy et al. demonstrated that direct exposure to MWCNT causes to length-dependent cytokine release from macrophages but not mesothelial cells. However, treatment of the mesothelial cells with conditioned medium from CNT-treated macrophages led to increased secretion of cytokines. In another study, MWCNT were revealed to trigger the macrophages to produce TGF-β1 and platelet-derived growth factor (PDGF) that promoted the transformation of lung fibroblasts to myofibroblasts, a major factor in development of fibrosis.44
Cytotoxicity of TiO2 nanoparticles
Widespread applications of titanium dioxide nanoparticles (TiO2 NPs) in consumer products including cosmetic, paints, pharmaceutical preparations, food additives and so on is a result of their ability to confer opacity and whiteness.45,46 In recent years, the photocatalytic killing effect of TiO2 NPs on cancerous cells has received great attention.47-49
The potential mechanism of cytotoxicity induced by these non-soluble metal oxide NPs are still controversial. In some literature, these NPs are even considered as a natural nanomaterial.50 Conversely, some reports have pointed out the potential toxicity of TiO2 nanoparticles, including their ability to induce oxidative stress, genotoxicity and immunotoxicity.51,52 However, the mechanisms of these toxic effects are still blurred but cytotoxicity evaluation of these metal oxide NPs is important for in vivo and in vitro studies. Despite other NPs such as ZnO, quantum dots and so, TiO2 NPs do not release toxic ions hence toxicity of these particles could be attributed to the size-dependent interaction between nanoparticles and intracellular biomolecules adsorbed onto nanoparticles.53-55 These interactions result in generation of ROS, mitochondrial depolarization, plasma membrane leakage, intracellular calcium influx and cytokine release.56-59
In a study, Xiong et al. investigated size influence of TiO2 NPs on their phototoxicity. Results showed that there was a converse relationship between phototoxicity and the size of these particles; as, the mortality of the cells treated with 10 nm TiO2 NPs after photoactivation by UV light was significantly higher than that of the cells treated with larger particles (20 and 100 nm particles). Furthermore, cytotoxicity of non-photoacivated 10, 20 and 100 nm NPs was not inconsiderable for cells treated with them. In addition, the treated cells with 10 nm photoactivated particles demonstrated a higher generation of mitochondrial superoxide in comparison to 20 and 100 nm particles.
Indeed, the higher cytotoxicity induced by smaller particles is related to their higher surface area and hence contain a larger number of surface-exposed TiO2 molecules. Phototoxicity of these NPs could be decreased via surface coating with chitosan or PEMA because of the prevention of biomolecule adsorption and hydroxyl radicals (.OH) production in the photoactivation process.54
In another study, size-dependent toxicity of both TiO2 and PLGA was investigated. Findings revealed that biomedically used PLGA nanoparticles did not show strong cytotoxic effect in comparison to TiO2 nanoparticles. However, the smaller PLGA nanoparticles have the potential to trigger the release of TNF-α. 200 nm PLGA nanoparticles could not trigger any negative response from cells. Higher cytotoxic effect was observed in cells treated with TiO2 nanoparticles, especially at concentrations higher than 100μg/ml. The size-dependent cytotoxicity of both PLGA and TiO2 nanoparticles could be attributed to the smaller size and larger specific surface area and thus exposure of more molecules on the surface that led to the adsorption of more biomolecules such as proteins in the environment.60
Cytotoxicity of quantum dots
Quantum dots (QDs), colloidal semiconductor nanoparticles, are a promising type of NPs which possess exceptional optical properties including high fluorescent quantum yield, broad absorption, narrow emission and high photostability. These properties make QDs an attractive candidate for in vivo imaging instead of fluorescent dyes.61
Similar to other NPs, cytotoxicity of QDs depends on parameters including size, shape, concentration, charge, redox activity, surface coatings and mechanical stability of these particles. Toxicity of uncoated core CdSe or CdTe-QDs have been investigated in some literature. Two major mechanisms are involved in the toxicity effects of these inorganic nanoparticles are as follows:62-65
-
Cd+2 ions existing in QDs structure:
These toxic metal ions cause toxic effects through several routes such as interference with DNA repair and substitution for physiologic Zn. Cd+2 ions increase oxidative stress but they cannot directly generate free radicals.
-
Free radical formation:
QDs of CdSe and CdTe are highly reactive, thus, photoactivation of these QDs via visible or UV light leads to their oxidation. Indeed, a photon of light could excite the QD and consequently generates an excited electron that transfers to molecular oxygen, forming singlet oxygen. Reaction of singlet oxygen with water/other biological molecules results in production of free radicals.
Kauffer et al. recently demonstrated that variation in core compositions and surface chemistries of QDs, CdSe QDs vs. CdS QDs, lead to their different cytotoxicity. The former produced •OH radicals immediately after light activation, while the latter required extensive irradiation to generate an equivalent amount of radicals. Therefore, the toxicity observed for CdSe QDs could be directly related to •OH radicals produced. Indeed, cytotoxicity of colloidal NPs can be controlled and relieved by choosing appropriate materials for QD core and suitable irradiation condition.66
Cytotoxicity of gold nanoparticles
Gold nanoparticles (GNPs), are one of the promising inorganic (NPs) that have attracted scientific and technological interests due to their ease of synthesis, chemical stability and excellent optical properties.67-69 These unique properties of GNPs, make them appealing tools for cancer diagnosis and treatment.70-72
Most of in vitro studies have indicated that these NPs are nontoxic for cells. Evaluation of GNPs cytotoxicity is essential because of broad spectrum application of GNPs in biomedical sciences. In the most of literature investigations have demonstrated that these inorganic nanoparticles are nontoxic. Cytotoxicity of GNPs depends on their size, shape and surrounding ligands.73,74 Anisotropic GNPs have more potential oxidation than the isotropic ones due to their highly exposed surface areas and defects. Also, in some literature investigations exhibited that spherical GNPs are suitable for biomedical application.75-77
Recently, the cytotoxicity effects of 5 and/or 15 nm GNPs 5 and 15 nm in vitro on Balb/3T3 mouse fibroblasts have been investigated. In order to understand the observed differences in cytotoxicity of two sizes of GNPs, Gioria et al. examined the uptake and the intracellular distribution of the NPs. The results indicated cytotoxicity effects only for the cells treated with 5 nm GNPs but no toxicity was revealed on Balb/3T3 for 15 nm GNPs. This observation is due to high number of 5 nm GNPs taken-up by cells in comparison to the larger particles (15 nm particles).78
Cytotoxicity of silver nanoparticles
Antimicrobial properties of silver nanoparticles (AgNPs) cause to the use of these NPs in a broad spectrum of consumer products including cosmetics, electronics, household appliances, textiles, and food products.79,80 In the recent decade, AgNPs have been used in medical fields such as drug delivery, designing biosensors, and imaging contrast agents etc.81-83 Thus, toxicity assay is an important factor to be considered in their application for biomedical purposes. Cytotoxicity of these NPs is related to comfortable oxidation AgNPs to Ag+ ions which are very toxic for biological systems and cellular components.84-87
Compton and coworkers in a study showed that AgNPs in aqueous system are more toxic compared to the bulk Ag is more toxic due to the presence of dissolved oxygen, its reduction on NPs and then the release of H2O2 from AgNPs. Also, results demonstrated that ROS generation from nanoparticulated Ag are greater than that of macro (bulk) silver.88
Recently, in a report the size- and coating-dependent toxicity of thoroughly characterized AgNPs was investigated following exposure to human lung cells. The results revealed that only the cytotoxicity of the 10 nm particles was independent of surface coating. In contrast, all AgNPs tested caused an increase in overall DNA damage after 24 h which suggests independent mechanisms for the cytotoxicity and DNA damage. However, there was no increased production of intracellular ROS; therefore, the toxicity observed was related to the rate of intracellular Ag release. Interaction with thiol and amino groups of biomolecules and appearance of the toxicity effect on cellular components were a result of sliver release. Thus, AgNPs with higher Ag release are more toxic.89
Conclusion
Despite the wide spread applications of nano-sized materials in various sciences areas, there are numerous reports about side effects of these materials on biological systems and cellular compartments. In addition to physicochemical properties, the production of toxic ions, fibrous structure, high surface charge and generation of radical species result in cytotoxicity by NPs including carbon nanotubes, titanium dioxide NPs, quantum dots, gold NPs and silver NPs. Both in vivo and in vitro assays are used for toxicity assessment of NPs. In vitro assays have received more attentions compared to in vivo assays due to being faster, convenient, less expensive, and devoid lacking any ethical issues.
Ethical Issues
Not applicable.
Conflict of Interest
The authors declare that they have no conflict of interest.
References
- 1.Farokhzad OC, Langer R. Nanomedicine: Developing smarter therapeutic and diagnostic modalities. Adv Drug Deliv Rev. 2006;58(14):1456–9. doi: 10.1016/j.addr.2006.09.011. [DOI] [PubMed] [Google Scholar]
- 2.Roco MC. Nanotechnology: Convergence with modern biology and medicine. Curr Opin Biotechnol. 2003;14(3):337–46. doi: 10.1016/S0958-1669(03)00068-5. [DOI] [PubMed] [Google Scholar]
- 3.Caruthers SD, Wickline SA, Lanza GM. Nanotechnological applications in medicine. Curr Opin Biotechnol. 2007;18(1):26–30. doi: 10.1016/j.copbio.2007.01.006. [DOI] [PubMed] [Google Scholar]
- 4.Silva GA. Introduction to nanotechnology and its applications to medicine. Surg Neurol. 2004;61(3):216–20. doi: 10.1016/j.surneu.2003.09.036. [DOI] [PubMed] [Google Scholar]
- 5.Singh M, Singh S, Prasad S, Gambhir IS. Nanotechnology in medicine and antibacterial effect of silver nanoparticles. Dig J Nanomater Bios. 2008;3(3):115–22. [Google Scholar]
- 6.Nie S, Xing Y, Kim GJ, Simons JW. Nanotechnology applications in cancer. Annu Rev Biomed Eng. 2007;9:257–88. doi: 10.1146/annurev.bioeng.9.060906.152025. [DOI] [PubMed] [Google Scholar]
- 7.Choi O, Hu Z. Size dependent and reactive oxygen species related nanosilver toxicity to nitrifying bacteria. Environ Sci Technol. 2008;42(12):4583–8. doi: 10.1021/es703238h. [DOI] [PubMed] [Google Scholar]
- 8.Hussain SM, Hess KL, Gearhart JM, Geiss KT, Schlager JJ. In vitro toxicity of nanoparticles in brl 3a rat liver cells. Toxicol In Vitro. 2005;19(7):975–83. doi: 10.1016/j.tiv.2005.06.034. [DOI] [PubMed] [Google Scholar]
- 9.Zoroddu M, Medici S, Ledda A, Nurchi V, Lachowicz J, Peana M. Toxicity of nanoparticles. Current Medicinal Chem. 2014;21(33):3837–53. doi: 10.2174/0929867321666140601162314. [DOI] [PubMed] [Google Scholar]
- 10. Marie Curie Initial Training Network - Environmental Chemoinformatics (ECO). Toxicity of nanoparticles. Project report – ITN-ECO: 2012.
- 11.Ahamed M, Karns M, Goodson M, Rowe J, Hussain SM, Schlager JJ. et al. DNA damage response to different surface chemistry of silver nanoparticles in mammalian cells. Toxicol Appl Pharmacol. 2008;233(3):404–10. doi: 10.1016/j.taap.2008.09.015. [DOI] [PubMed] [Google Scholar]
- 12.Sharma V, Shukla RK, Saxena N, Parmar D, Das M, Dhawan A. DNA damaging potential of zinc oxide nanoparticles in human epidermal cells. Toxicol Lett. 2009;185(3):211–8. doi: 10.1016/j.toxlet.2009.01.008. [DOI] [PubMed] [Google Scholar]
- 13.Wang F, Yu L, Monopoli MP, Sandin P, Mahon E, Salvati A. et al. The biomolecular corona is retained during nanoparticle uptake and protects the cells from the damage induced by cationic nanoparticles until degraded in the lysosomes. Nanomedicine. 2013;9(8):1159–68. doi: 10.1016/j.nano.2013.04.010. [DOI] [PubMed] [Google Scholar]
- 14.Elsaesser A, Howard CV. Toxicology of nanoparticles. Adv Drug Deliv Rev. 2012;64(2):129–37. doi: 10.1016/j.addr.2011.09.001. [DOI] [PubMed] [Google Scholar]
- 15.Regoli F, Giuliani ME. Oxidative pathways of chemical toxicity and oxidative stress biomarkers in marine organisms. Mar Environ Res. 2014;93:106–17. doi: 10.1016/j.marenvres.2013.07.006. [DOI] [PubMed] [Google Scholar]
- 16.Jomova K, Baros S, Valko M. Redox active metal-induced oxidative stress in biological systems. Transition Met Chem. 2012;37(2):127–34. doi: 10.1007/s11243-012-9583-6. [DOI] [Google Scholar]
- 17.Chen H, Yoshioka H, Kim GS, Jung JE, Okami N, Sakata H. et al. Oxidative stress in ischemic brain damage: mechanisms of cell death and potential molecular targets for neuroprotection. Antioxid Redox Signal. 2011;14(8):1505–17. doi: 10.1089/ars.2010.3576. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Soenen SJ, Rivera-Gil P, Montenegro JM, Parak WJ, De Smedt SC, Braeckmans K. Cellular toxicity of inorganic nanoparticles: Common aspects and guidelines for improved nanotoxicity evaluation. Nano Today. 2011;6(5):446–65. doi: 10.1016/j.nantod.2011.08.001. [DOI] [Google Scholar]
- 19.Mahmoudi M, Hofmann H, Rothen-Rutishauser B, Petri-Fink A. Assessing the in vitro and in vivo toxicity of superparamagnetic iron oxide nanoparticles. Chem Rev. 2012;112(4):2323–38. doi: 10.1021/cr2002596. [DOI] [PubMed] [Google Scholar]
- 20.Fischer J, Prosenc MH, Wolff M, Hort N, Willumeit R, Feyerabend F. Interference of magnesium corrosion with tetrazolium-based cytotoxicity assays. Acta Biomater. 2010;6(5):1813–23. doi: 10.1016/j.actbio.2009.10.020. [DOI] [PubMed] [Google Scholar]
- 21.Rabolli V, Thomassen LC, Princen C, Napierska D, Gonzalez L, Kirsch-Volders M. et al. Influence of size, surface area and microporosity on the in vitro cytotoxic activity of amorphous silica nanoparticles in different cell types. Nanotoxicology. 2010;4(3):307–18. doi: 10.3109/17435390.2010.482749. [DOI] [PubMed] [Google Scholar]
- 22.Kumbıçak Ü, Çavaş T, Çinkılıç N, Kumbıçak Z, Vatan Ö, Yılmaz D. Evaluation of in vitro cytotoxicity and genotoxicity of copper-zinc alloy nanoparticles in human lung epithelial cells. Food Chem Toxicol. 2014;73:105–12. doi: 10.1016/j.fct.2014.07.040. [DOI] [PubMed] [Google Scholar]
- 23.Fotakis G, Timbrell JA. In vitro cytotoxicity assays: Comparison of ldh, neutral red, mtt and protein assay in hepatoma cell lines following exposure to cadmium chloride. Toxicol Lett. 2006;160(2):171–7. doi: 10.1016/j.toxlet.2005.07.001. [DOI] [PubMed] [Google Scholar]
- 24.Crouch SPM, Kozlowski R, Slater KJ, Fletcher J. The use of atp bioluminescence as a measure of cell proliferation and cytotoxicity. J Immunol Methods. 1993;160(1):81–8. doi: 10.1016/0022-1759(93)90011-U. [DOI] [PubMed] [Google Scholar]
- 25.Schiewe MH, Hawk EG, Actor DI, Krahn MM. Use of a bacterial bioluminescence assay to assess toxicity of contaminated marine sediments. Can J Fish Aquat Sci. 1985;42(7):1244–8. doi: 10.1139/f85-154. [DOI] [Google Scholar]
- 26.Benton MJ, Malott ML, Knight SS, Cooper CM, Benson WH. Influence of sediment composition on apparent toxicity in a solid-phase test using bioluminescent bacteria. Environ Toxicol Chem. 1995;14(3):411–4. doi: 10.1002/etc.5620140309. [DOI] [Google Scholar]
- 27.Asare N, Instanes C, Sandberg WJ, Refsnes M, Schwarze P, Kruszewski M. et al. Cytotoxic and genotoxic effects of silver nanoparticles in testicular cells. Toxicology. 2012;291(1-3):65–72. doi: 10.1016/j.tox.2011.10.022. [DOI] [PubMed] [Google Scholar]
- 28.Korzeniewski C, Callewaert DM. An enzyme-release assay for natural cytotoxicity. J Immunol Methods. 1983;64(3):313–20. doi: 10.1016/0022-1759(83)90438-6. [DOI] [PubMed] [Google Scholar]
- 29. van Meerloo J, Kaspers GJ, Cloos J. Cell sensitivity assays: The MTT assay. In: Cree IA, editor. Cancer cell culture. Hatfield: Springer; 2011. P. 237-45. [DOI] [PubMed]
- 30.Malich G, Markovic B, Winder C. The sensitivity and specificity of the mts tetrazolium assay for detecting the in vitro cytotoxicity of 20 chemicals using human cell lines. Toxicology. 1997;124(3):179–92. doi: 10.1016/S0300-483X(97)00151-0. [DOI] [PubMed] [Google Scholar]
- 31.Cho WS, Duffin R, Thielbeer F, Bradley M, Megson IL, MacNee W. et al. Zeta potential and solubility to toxic ions as mechanisms of lung inflammation caused by metal/metal oxide nanoparticles. Toxicol Sci. 2012;126(2):469–77. doi: 10.1016/10.1093/toxsci/kfs006. [DOI] [PubMed] [Google Scholar]
- 32.Donaldson K, Poland CA, Schins RP. Possible genotoxic mechanisms of nanoparticles: Criteria for improved test strategies. Nanotoxicology. 2010;4(4):414–20. doi: 10.3109/17435390.2010.482751. [DOI] [PubMed] [Google Scholar]
- 33.Stern ST, Adiseshaiah PP, Crist RM. Autophagy and lysosomal dysfunction as emerging mechanisms of nanomaterial toxicity. Part Fibre Toxicol. 2012;9(1):20. doi: 10.1186/1743-8977-9-20. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Li Y, Zhang W, Niu J, Chen Y. Surface-coating-dependent dissolution, aggregation, and reactive oxygen species (ros) generation of silver nanoparticles under different irradiation conditions. Environ Sci Technol. 2013;47(18):10293–301. doi: 10.1021/es400945v. [DOI] [PubMed] [Google Scholar]
- 35.Nishanth RP, Jyotsna RG, Schlager JJ, Hussain SM, Reddanna P. Inflammatory responses of raw 264.7 macrophages upon exposure to nanoparticles: Role of ros-nfκb signaling pathway. Nanotoxicology. 2011;5(4):502–16. doi: 10.3109/17435390.2010.541604. [DOI] [PubMed] [Google Scholar]
- 36.Luna-Velasco A, Field JA, Cobo-Curiel A, Sierra-Alvarez R. Inorganic nanoparticles enhance the production of reactive oxygen species (ros) during the autoxidation of L-3,4-dihydroxyphenylalanine (L-dopa) Chemosphere. 2011;85(1):19–25. doi: 10.1016/j.chemosphere.2011.06.053. [DOI] [PubMed] [Google Scholar]
- 37. Shao W, Arghya P, Yiyong M, Rodes L, Prakash S. Carbon nanotubes for use in medicine: Potentials and limitations. In: Suzuki S, editor. Syntheses and Applications of Carbon Nanotubes and Their Composites. Croatia: InTech; 2013. P. 285-311.
- 38.De Volder MF, Tawfick SH, Baughman RH, Hart AJ. Carbon nanotubes: Present and future commercial applications. Science. 2013;339(6119):535–9. doi: 10.1126/science.1222453. [DOI] [PubMed] [Google Scholar]
- 39. O’connell MJ. Carbon nanotubes: Properties and applications. Boca Raton: CRC Press; 2012.
- 40.Shvedova AA, Pietroiusti A, Fadeel B, Kagan VE. Mechanisms of carbon nanotube-induced toxicity: Focus on oxidative stress. Toxicol Appl Pharmacol. 2012;261(2):121–33. doi: 10.1016/j.taap.2012.03.023. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Johnston HJ, Hutchison GR, Christensen FM, Peters S, Hankin S, Aschberger K. et al. A critical review of the biological mechanisms underlying the in vivo and in vitro toxicity of carbon nanotubes: The contribution of physico-chemical characteristics. Nanotoxicology. 2010;4(2):207–46. doi: 10.3109/17435390903569639. [DOI] [PubMed] [Google Scholar]
- 42.Campagnolo L, Massimiani M, Palmieri G, Bernardini R, Sacchetti C, Bergamaschi A. et al. Biodistribution and toxicity of pegylated single wall carbon nanotubes in pregnant mice. Part Fibre Toxicol. 2013;10(1):21. doi: 10.1186/1743-8977-10-21. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Clift MJ, Endes C, Vanhecke D, Wick P, Gehr P, Schins RP. et al. A comparative study of different in vitro lung cell culture systems to assess the most beneficial tool for screening the potential adverse effects of carbon nanotubes. Toxicol Sci. 2014;137(1):55–64. doi: 10.1093/toxsci/kft216. [DOI] [PubMed] [Google Scholar]
- 44.Murphy FA, Poland CA, Duffin R, Al-Jamal KT, Ali-Boucetta H, Nunes A. et al. Length-dependent retention of carbon nanotubes in the pleural space of mice initiates sustained inflammation and progressive fibrosis on the parietal pleura. Am J Pathol. 2011;178(6):2587–600. doi: 10.1016/j.ajpath.2011.02.040. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Yin ZF, Wu L, Yang HG, Su YH. Recent progress in biomedical applications of titanium dioxide. Phys Chem Chem Phys. 2013;15(14):4844–58. doi: 10.1039/C3CP43938K. [DOI] [PubMed] [Google Scholar]
- 46.Weir A, Westerhoff P, Fabricius L, Hristovski K, von Goetz N. Titanium dioxide nanoparticles in food and personal care products. Environ Sci Technol. 2012;46(4):2242–50. doi: 10.1021/es204168d. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Sha B, Gao W, Han Y, Wang S, Wu J, Xu F. et al. Potential application of titanium dioxide nanoparticles in the prevention of osteosarcoma and chondrosarcoma recurrence. J Nanosci Nanotechnol. 2013;13(2):1208–11. doi: 10.1166/jnn.2013.6081. [DOI] [PubMed] [Google Scholar]
- 48.Wu Q, Guo D, Du Y, Liu D, Wang D, Bi H. UVB irradiation enhances TiO2 nanoparticle-induced disruption of calcium homeostasis in human lens epithelial cells. Photochem Photobiol. 2014;90(6):1324–31. doi: 10.1111/php.12322. [DOI] [PubMed] [Google Scholar]
- 49.Pierzchala K, Lekka M, Magrez A, Kulik AJ, Forró L, Sienkiewicz A. Photocatalytic and phototoxic properties of TiO2-based nanofilaments: ESR and AFM assays. Nanotoxicology. 2012;6(8):813–24. doi: 10.3109/17435390.2011.625129. [DOI] [PubMed] [Google Scholar]
- 50.PetkoviC J, Zegura B, StevanoviC M, Drnovšek N, UskokoviC D, Novak S. et al. DNA damage and alterations in expression of DNA damage responsive genes induced by TiO2 nanoparticles in human hepatoma hepg2 cells. Nanotoxicology. 2011;5(3):341–53. doi: 10.3109/17435390.2010.507316. [DOI] [PubMed] [Google Scholar]
- 51.Gerloff K, Fenoglio I, Carella E, Kolling J, Albrecht C, Boots AW. et al. Distinctive toxicity of TiO2 rutile/anatase mixed phase nanoparticles on Caco-2 cells. Chem Res Toxicol. 2012;25(3):646–55. doi: 10.1021/tx200334k. [DOI] [PubMed] [Google Scholar]
- 52.Montiel-Dávalos Al, Ventura-Gallegos JL, Alfaro-Moreno E, Soria-Castro E, García-Latorre E, Cabañas-Moreno JG. et al. TiO2 nanoparticles induce dysfunction and activation of human endothelial cells. Chem Res Toxicol. 2012;25(4):920–30. doi: 10.1021/tx200551u. [DOI] [PubMed] [Google Scholar]
- 53.Jin C, Tang Y, Yang FG, Li XL, Xu S, Fan XY. et al. Cellular toxicity of TiO2 nanoparticles in anatase and rutile crystal phase. Biol Trace Elem Res. 2011;141(1-3):3–15. doi: 10.1007/s12011-010-8707-0. [DOI] [PubMed] [Google Scholar]
- 54.Xiong S, George S, Ji Z, Lin S, Yu H, Damoiseaux R. et al. Size of TiO2 nanoparticles influences their phototoxicity: An in vitro investigation. Arch Toxicol. 2013;87(1):99–109. doi: 10.1007/s00204-012-0912-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Ivask A, Bondarenko O, Jepihhina N, Kahru A. Profiling of the reactive oxygen species-related ecotoxicity of CuO, ZnO, TiO2, silver and fullerene nanoparticles using a set of recombinant luminescent escherichia coli strains: Differentiating the impact of particles and solubilised metals. Anal Bioanal Chem. 2010;398(2):701–16. doi: 10.1007/s00216-010-3962-7. [DOI] [PubMed] [Google Scholar]
- 56.Chen EY, Garnica M, Wang YC, Mintz AJ, Chen CS, Chin WC. A mixture of anatase and rutile TiO2 nanoparticles induces histamine secretion in mast cells. Part Fibre Toxicol. 2012;9:2. doi: 10.1186/1743-8977-9-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Scherbart AM, Langer J, Bushmelev A, van Berlo D, Haberzettl P, van Schooten FJ. et al. Contrasting macrophage activation by fine and ultrafine titanium dioxide particles is associated with different uptake mechanisms. Part Fibre Toxicol. 2011;8:31. doi: 10.1186/1743-8977-8-31. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Fu J, Rong G, Deng Y. Mammalian cell cytotoxicity and genotoxicity of metallic nanoparticles. Adv Sci Lett. 2012;5(1):294–8. doi: 10.1166/asl.2012.1946. [DOI] [Google Scholar]
- 59.Ghosh M, Chakraborty A, Mukherjee A. Cytotoxic, genotoxic and the hemolytic effect of titanium dioxide (TiO2) nanoparticles on human erythrocyte and lymphocyte cells in vitro. J Appl Toxicol. 2013;33(10):1097–110. doi: 10.1002/jat.2863. [DOI] [PubMed] [Google Scholar]
- 60.Xiong S, George S, Yu H, Damoiseaux R, France B, Ng KW. et al. Size influences the cytotoxicity of poly (lactic-co-glycolic acid) (PLGA) and titanium dioxide (TiO2) nanoparticles. Arch Toxicol. 2013;87(6):1075–86. doi: 10.1007/s00204-012-0938-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61. Osiński M, Parak WJ, Jovin TM, Yamamoto K. Colloidal Quantum Dots for Biomedical Applications V, SPIE International Symposium on Biomedical Optics BiOS 2010, Vol. 7575, Paper 75750Z San Francisco, California, 23‐25 January 2010.
- 62.Chen N, He Y, Su Y, Li X, Huang Q, Wang H. et al. The cytotoxicity of cadmium-based quantum dots. Biomaterials. 2012;33(5):1238–44. doi: 10.1016/j.biomaterials.2011.10.070. [DOI] [PubMed] [Google Scholar]
- 63.Hoshino A, Hanada S, Yamamoto K. Toxicity of nanocrystal quantum dots: The relevance of surface modifications. Arch Toxicol. 2011;85(7):707–20. doi: 10.1007/s00204-011-0695-0. [DOI] [PubMed] [Google Scholar]
- 64.Zheng X, Tian J, Weng L, Wu L, Jin Q, Zhao J. et al. Cytotoxicity of cadmium-containing quantum dots based on a study using a microfluidic chip. Nanotechnology. 2012;23(5):055102. doi: 10.1088/0957-4484/23/5/055102. [DOI] [PubMed] [Google Scholar]
- 65.Singh BR, Singh BN, Khan W, Singh HB, Naqvi AH. ROS-mediated apoptotic cell death in prostate cancer LNCaP cells induced by biosurfactant stabilized CdS quantum dots. Biomaterials. 2012;33(23):5753–67. doi: 10.1016/j.biomaterials.2012.04.045. [DOI] [PubMed] [Google Scholar]
- 66.Kauffer FA, Merlin C, Balan L, Schneider R. Incidence of the core composition on the stability, the ROS production and the toxicity of CdSe quantum dots. J Hazard Mater. 2014;268:246–55. doi: 10.1016/j.jhazmat.2014.01.029. [DOI] [PubMed] [Google Scholar]
- 67.Dykman L, Khlebtsov N. Gold nanoparticles in biomedical applications: Recent advances and perspectives. Chem Soc Rev. 2012;41(6):2256–82. doi: 10.1039/C1CS15166E. [DOI] [PubMed] [Google Scholar]
- 68.Tiwari PM, Vig K, Dennis VA, Singh SR. Functionalized gold nanoparticles and their biomedical applications. Nanomaterials. 2011;1(1):31–63. doi: 10.3390/nano1010031. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 69.Yeh YC, Creran B, Rotello VM. Gold nanoparticles: Preparation, properties, and applications in bionanotechnology. Nanoscale. 2012;4(6):1871–80. doi: 10.1039/C1NR11188D. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 70.Lim ZZJ, Li JEJ, Ng CT, Yung LYL, Bay BH. Gold nanoparticles in cancer therapy. Acta Pharmacol Sin. 2011;32(8):983–90. doi: 10.1038/aps.2011.82. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 71.Jain S, Hirst DG, O'sullivan JM. Gold nanoparticles as novel agents for cancer therapy. Br J Radiol. 2012;85(1010):101–13. doi: 10.1259/bjr/59448833. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 72.Heo DN, Yang DH, Moon HJ, Lee JB, Bae MS, Lee SC. et al. Gold nanoparticles surface-functionalized with paclitaxel drug and biotin receptor as theranostic agents for cancer therapy. Biomaterials. 2012;33(3):856–66. doi: 10.1016/j.biomaterials.2011.09.064. [DOI] [PubMed] [Google Scholar]
- 73.Khlebtsov N, Dykman L. Biodistribution and toxicity of engineered gold nanoparticles: A review of in vitro and in vivo studies. Chem Soc Rev. 2011;40(3):1647–71. doi: 10.1039/C0CS00018C. [DOI] [PubMed] [Google Scholar]
- 74. Taylor U, Barchanski A, Garrels W, Klein S, Kues W, Barcikowski S, et al. Toxicity of gold nanoparticles on somatic and reproductive cells. In: Zahavy E, Ordentlich A, Yitzhaki S, Shafferman A, editors. Nano-biotechnology for biomedical and diagnostic research. New York: Springer; 2012. P. 125-33. [DOI] [PubMed]
- 75.Loumaigne M, Richard A, Laverdant J, Nutarelli D, Débarre A. Ligand-induced anisotropy of the two-photon luminescence of spherical gold particles in solution unraveled at the single particle level. Nano lett. 2010;10(8):2817–24. doi: 10.1021/nl100737y. [DOI] [PubMed] [Google Scholar]
- 76.Arnida Arnida, Janát-Amsbury MM, Ray A, Peterson CM, Ghandehari H. Geometry and surface characteristics of gold nanoparticles influence their biodistribution and uptake by macrophages. Eur J Pharm Biopharm. 2011;77(3):417–23. doi: 10.1016/j.ejpb.2010.11.010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 77.Pissuwan D, Niidome T, Cortie MB. The forthcoming applications of gold nanoparticles in drug and gene delivery systems. J Control Release. 2011;149(1):65–71. doi: 10.1016/j.jconrel.2009.12.006. [DOI] [PubMed] [Google Scholar]
- 78.Coradeghini R, Gioria S, García CP, Nativo P, Franchini F, Gilliland D. et al. Size-dependent toxicity and cell interaction mechanisms of gold nanoparticles on mouse fibroblasts. Toxicol lett. 2013;217(3):205–16. doi: 10.1016/j.toxlet.2012.11.022. [DOI] [PubMed] [Google Scholar]
- 79.Chaloupka K, Malam Y, Seifalian AM. Nanosilver as a new generation of nanoproduct in biomedical applications. Trends Biotechnol. 2010;28(11):580–8. doi: 10.1016/j.tibtech.2010.07.006. [DOI] [PubMed] [Google Scholar]
- 80.García-Barrasa J, López-de-Luzuriaga JM, Monge M. Silver nanoparticles: Synthesis through chemical methods in solution and biomedical applications. Cent Eur J Chem. 2011;9(1):7–19. doi: 10.2478/s11532-010-0124-x. [DOI] [Google Scholar]
- 81.Wang Y, Newell BB, Irudayaraj J. Folic acid protected silver nanocarriers for targeted drug delivery. J Biomed Nanotechnol. 2012;8(5):751–9. doi: 10.1166/jbn.2012.1437. [DOI] [PubMed] [Google Scholar]
- 82.Zhou W, Ma Y, Yang H, Ding Y, Luo X. A label-free biosensor based on silver nanoparticles array for clinical detection of serum p53 in head and neck squamous cell carcinoma. Int J Nanomedicine. 2011;6(1):381–6. doi: 10.2147/IJN.S13249. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 83.Wang J, Song D, Wang L, Zhang H, Zhang H, Sun Y. Design and performances of immunoassay based on spr biosensor with au/ag alloy nanocomposites. Chem. 2011;157(2):Chem 2011;157(2). doi: 10.1016/j.snb.2011.05.020. [DOI] [Google Scholar]
- 84.Mei N, Zhang Y, Chen Y, Guo X, Ding W, Ali SF. et al. Silver nanoparticle-induced mutations and oxidative stress in mouse lymphoma cells. Environ Mol Mutagen. 2012;53(6):409–19. doi: 10.1002/em.21698. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 85.Kim S, Ryu DY. Silver nanoparticle-induced oxidative stress, genotoxicity and apoptosis in cultured cells and animal tissues. J Appl Toxicol. 2013;33(2):78–89. doi: 10.1002/jat.2792. [DOI] [PubMed] [Google Scholar]
- 86.Xin L, Wang J, Wu Y, Guo S, Tong J. Increased oxidative stress and activated heat shock proteins in human cell lines by silver nanoparticles. Hum Exp Toxicol. 2015;34(3):315–23. doi: 10.1177/0960327114538988. [DOI] [PubMed] [Google Scholar]
- 87.Yang X, Gondikas AP, Marinakos SM, Auffan M, Liu J, Hsu-Kim H. et al. Mechanism of silver nanoparticle toxicity is dependent on dissolved silver and surface coating in caenorhabditis elegans. Environ Sci Technol. 2012;46(2):1119–27. doi: 10.1021/es202417t. [DOI] [PubMed] [Google Scholar]
- 88.Batchelor-McAuley C, Tschulik K, Neumann C, Laborda E, Compton RG. Why are silver nanoparticles more toxic than bulk silver? Towards understanding the dissolution and toxicity of silver nanoparticles. Int J Electrochem Sci. 2014;9(3):1132–8. [Google Scholar]
- 89.Gliga AR, Skoglund S, Wallinder IO, Fadeel B, Karlsson HL. Size-dependent cytotoxicity of silver nanoparticles in human lung cells: The role of cellular uptake, agglomeration and ag release. Part Fibre Toxicol. 2014;11(1):11. doi: 10.1186/1743-8977-11-11. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 90.Sanwlani S, Rawat K, Pal M, Bohidar HB, Verma AK. Cellular uptake induced biotoxicity of surface-modified cdse quantum dots. J Nanopart Res. 2014;16:2382. doi: 10.1007/s11051-014-2382-6. [DOI] [Google Scholar]
- 91.Vicario-Parés U, Castañaga L, Lacave JM, Oron M, Reip P, Berhanu D. et al. Comparative toxicity of metal oxide nanoparticles (CuO, ZnO and TiO2) to developing zebrafish embryos. J Nanopart Res. 2014;16:2550. doi: 10.1007/s11051-014-2550-8. [DOI] [Google Scholar]
- 92.Pujalté I, Passagne I, Brouillaud B, Tréguer M, Durand E, Ohayon-Courtès C. et al. Cytotoxicity and oxidative stress induced by different metallic nanoparticles on human kidney cells. Part Fibre Toxicol. 2011;8:10. doi: 10.1186/1743-8977-8-10. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 93.Lee YH, Cheng FY, Chiu HW, Tsai JC, Fang CY, Chen CW. et al. Cytotoxicity, oxidative stress, apoptosis and the autophagic effects of silver nanoparticles in mouse embryonic fibroblasts. Biomaterials. 2014;35(16):4706–15. doi: 10.1016/j.biomaterials.2014.02.021. [DOI] [PubMed] [Google Scholar]
- 94.Chueh PJ, Liang RY, Lee YH, Zeng ZM, Chuang SM. Differential cytotoxic effects of gold nanoparticles in different mammalian cell lines. J Hazard Mater. 2014;264:303–12. doi: 10.1016/j.jhazmat.2013.11.031. [DOI] [PubMed] [Google Scholar]
- 95.Grabowski N, Hillaireau H, Vergnaud J, Santiago LA, Kerdine-Romer S, Pallardy M. et al. Toxicity of surface-modified plga nanoparticles toward lung alveolar epithelial cells. Int J Pharm. 2013;454(2):686–94. doi: 10.1016/j.ijpharm.2013.05.025. [DOI] [PubMed] [Google Scholar]