Abstract
The Schedule of Fatigue and Anergy/General Physician (SOFA/GP) was developed to screen for prolonged fatigue in the primary care setting. We aimed to evaluate the reliability and validity of the Korean version of the SOFA/GP (SOFA/GP-K), which is adapted from the original English version. We performed translation and back translation, and after conducting a pilot study, we tested the final version of the questionnaire for its reliability and validity in a Korean primary care setting. Two hundred participants that visited a health examination center in a university hospital completed the survey between September and November 2012. A second survey was performed within 2 weeks of the primary survey to test for reliability. We evaluated concurrent validity between the SOFA/GP-K score, the Fatigue Severity Scale (FSS), and Brief Fatigue Index (BFI) scores. The Spearman correlation coefficient between SOFA/GP-K and FSS was 0.71 and 0.61 between SOFA/GP-K and BFI. Internal consistency of SOFA/GP-K was observed (Cronbach's alpha = 0.82) and construct validity was confirmed by factor analysis. The Kappa scores for test-retest reliability for each survey item were between 0.28 and 0.64. The SOFA/GP-K is a valid and reliable questionnaire for screening fatigue in a primary care setting.
Keywords: Fatigue, Anergia, Korean, Primary Health Care, Validation, Scale
Graphical Abstract
INTRODUCTION
Although fatigue is one of the most common symptoms experienced by many people, it is yet to be conceptualized or accurately diagnosed despite many attempts (1). In Korea, around 29.5% of patients visiting primary care units report significant fatigue (2). The high prevalence of prolonged fatigue states (PFS) is of renewed interest in psychiatry and general medicine as they challenge conventional etiological concepts and the current classification of common forms of anxiety, depression, and somatic distress syndromes (3).
PFS is assumed when fatigue lasts more than one month with or without comorbid conditions elucidating fatigue, whereas chronic fatigue syndrome can be diagnosed when fatigue lasts more than 6 months without physical or mental illness as the main reason for fatigue. PFS have different characteristics than other common psychological and somatic forms of distress. The essential components of PFS are mental and physical fatigue, neurocognitive symptoms, and musculoskeletal pain (4). States of prolonged fatigue negatively affect quality of life and adversely influences a person's functioning consequently resulting in financial losses and social isolation (5). Therefore, early detection and screening of PFS is crucial.
In recent years, an increasing number of scales have been developed attempting to measure the nature, severity, and impact of fatigue in a range of clinical populations such as the Brief Fatigue Index (BFI), Fatigue Severity Scale (FSS), Chalder Fatigue Scale, and many others (1,5). Each scale has varied in the purpose of measure and in response to the multi-dimensional nature of fatigue. Many of these questionnaires were translated into Korean and validated BFI (6) and FSS (7), however, there are limitations to applying these questionnaires to primary care settings due to the fact that a great part of these questionnaires deals with fatigue in specific diseases. For instance, the FSS is a measurement of fatigue and was developed for patients with multiple sclerosis and systemic lupus erythematosus to facilitate research and treatment (6,8). The BFI has been validated with the general Korean population (9), and is more commonly used in cancer patients to assess for cancer related fatigue. In addition, BFI and FSS measure levels of acute fatigue within a short period of time (the past 24 hours and the past week, respectively), which supports the limitation for their use in detecting PFS.
Hadzi-Pavlovic et al. (4) developed and validated the Schedule of Fatigue and Anergia (SOFA) to identify cases of prolonged and disabling fatigue in community and general practice settings. The Schedule of Fatigue and Anergia/General Physician in Korean (SOFA/GP-K) screen for PFS differ from conventional screening tools because it is simple and not limited to specific diseases. The goal of this study was to produce a simple instrument that is sensitive, reliable, and valid for use in future primary clinics to accurately screen for PFS.
MATERIALS AND METHODS
Participants and data collection
Between September and November 2012, two hundred participants visiting a health examination center at a university hospital in Korea for a routine health screening were enrolled. They were asked to complete a self-administered questionnaire following brief instructions pertaining to the survey on the day of the hospital visit. The necessary sample size was obtained from a similar fatigue questionnaire validation study (10). The same survey was completed again after two weeks when the subjects visited the hospital for the results of their health screening tests. To assess for stress, we used the validated Korean Brief Encounter Psychosocial Instrument (BEPSI-K) (11). To be eligible, the subjects 1) had to be between 18 and 65 years of age, 2) had to understand and complete the questionnaires, 3) were not be taking psychiatric medications including sleeping pills and anti-anxiety agents, and 4) not under current treatment for malignancy or other acute diseases (abrupt onset with a short duration, mainly, common cold and hepatitis).
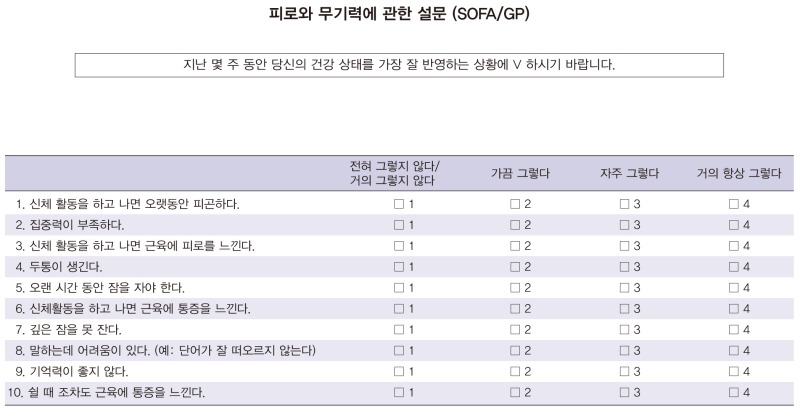
Schedule of fatigue anergia/general physician
The SOFA questionnaire exists in two forms: SOFA/CFS for identification of patients with chronic fatigue syndrome in specialized clinics, and the SOFA/GP, a modified version for the identification of fatigue syndromes in community and primary care settings. For our study, we created a Korean version of the latter questionnaire to be used in primary care settings in the community and hospitals. The SOFA/GP consists of 10 questionnaire items with anchor points ranging from 1 to 4 (1: none or little ~ 4: most of the time). A score of 1 is given for each question if the answer is 'a good part of the time' or 'most of the time'. A score of 0 is given if the answer is only true 'some of the time' or less. A total point cutoff of ≥3 points maximizes specificity (sensitivity 81%, specificity 100%) (4).
After acquiring permission from Dr. Hadzi-Pavlovic, cross-cultural adaptation of original questionnaire was performed based on recent guidelines (12). The SOFA/GP-K was developed using the forward-backward translation process. In the translation process, the items were first translated into Korean by two translators whose native language was Korean and then back-translated into English by two other translators whose native language was English, and who had not seen the original English version. Bilingual fluency was required of both translators to complete the translation. The back-translated English versions were compared with the original questionnaire. A committee of three people reviewed the translations and back translations to compare sources and developed the final version. The original developer of the survey confirmed the final version. Comprehensibility and appropriateness of language in the Korean cultural context were emphasized for the translation and cross-cultural adaptation procedure. For example, it was noted that a proportion of Korean patients associated the phrase "poor concentration" with lack of or a loss of concentration. Hence, the second item of the questionnaire "My concentration is poor" was translated to "Decreased concentration" in order to avoid ambiguity. A pilot study of 10 subjects was performed and based on feedback; the final version of the questionnaire was developed (Appendix 1).
Brief fatigue inventory
The BFI, developed by Mendoza et al. (13), consists of 9 items using a numerical scale of 0 to 10 on a single page. The first 3 items ask patients to describe their fatigue now, at its usual level, and at its worst level during the previous 24 hours, using extreme points from "no fatigue" to "fatigue as bad as you can imagine." The next 6 items ask patients to describe how much fatigue has interfered with different aspects of their life during the previous 24 hours. The global score for the BFI is calculated as the mean value of these 9 items. The validity and reliability of the original scale were well established in English, as well as in Korean (6).
Fatigue severity scale
The FSS is one of the best known and most used fatigue scales. It was developed by Krupp et al. for patients with multiple sclerosis and systemic lupus erythematosus to facilitate research and treatments (8). The scale contains nine items that measure the severity of fatigue symptoms of subjects during the past week. Items are scored from 1 to 7 on a numeric visual analog scale (VAS). The total score is calculated by deriving an arithmetic mean. It has been validated on several medical disorders such as multiple sclerosis, systemic lupus erythematosus, spinal cord injury, stroke, cancer, and many others (8,14).
Statistical analysis
The reliability and validity of the SOFA/GP-K were evaluated. The test-retest reliability was assessed with the kappa score and percent agreement for dichotomous variables. Internal consistency reliability was assessed using Cronbach's alpha coefficient. This coefficient ranges from 0 to 1, with higher values indicating good reliability. Construct validity was evaluated based on the factor analysis and the fit of the factor model was evaluated based on the results of the scree test, interpretability, and examination of the residuals. Concurrent validity was evaluated by calculating the Spearman correlation coefficients between SOFA/GP-K and FSS and BFI. All statistical procedures were performed using the STATA statistical software program (version 12.0).
Ethics statement
The study was approved by the institutional review board of Seoul National University Bundang Hospital in Korea (IRB number: B-1207/162-304). Each participant gave written consent after being fully informed of the study.
RESULTS
Participant characteristics
The participants were between 22 and 65 years old with a mean age of 46.5. Fifty percent of participants had a past medical history; 45 with hypertension, diabetes, dyslipidemia, or cardiovascular disease; 20 with chronic respiratory diseases including asthma; 8 with thyroid disease; 6 with chronic liver disease; and 14 with other diseases. Around thirty percent of participants exercised more than 3 times per week. Occupation was divided into three categories, unskilled/semi-skilled (108 participants), skilled (15 participants), and professional (61 participants). Among the 184 participants that were included in our study, 176 subjects completed the BEPSI-K and were classified into three categories depending on their scores; 76 with low intensity, 88 with middle intensity, and 12 subjects with high intensity stress (Table 1).
Table 1. Clinical characteristics of 184 subjects enrolled in the study.
| Parameters | No. | % |
|---|---|---|
| Gender | ||
| Male | 101 | 54.9 |
| Female | 83 | 45.1 |
| Mean Age, yr (range) | 46.5 (22-65) | |
| Education | ||
| ≤ Middle school | 5 | 2.7 |
| ≥ High school | 179 | 97.3 |
| Occupation | ||
| Unskilled/semi-skilled* | 108 | 58.7 |
| Skilled | 15 | 8.2 |
| Professional | 61 | 33.1 |
| Exercise | ||
| Yes | 61 | 33.2 |
| No | 123 | 66.8 |
| BEPSI-K | ||
| Low | 76 | 43.2 |
| Middle | 88 | 50.0 |
| High | 12 | 6.8 |
| Past medical history† | ||
| Yes | 92 | 50 |
| No | 92 | 50 |
*Including unemployed, housewife, service worker, and retired; †Including hypertension, diabetes, dyslipidemia, stroke, chronic liver disease, thyroid disease, chronic respiratory disease, cardiovascular disease, degenerative/rheumatoid arthritis, asthma, allergy, endometriosis, gastritis, prostatitis, alopecia, arrhythmia, history of prostate cancer (surgically removed). BEPSI-K, Korean Brief Encounter Psychosocial Instrument.
Rate of missing data
There were 5 missing responses for SOFA/GP-K, with a missing rate of 0.25% of the total data points. There were 11 incomplete questionnaires for the other fatigue instruments including surveys on general information. Therefore, a total number of 184 participants were included for analysis.
Internal consistent reliability and Test-retest reliability
The overall Cronbach's alpha coefficient for the SOFA/GP-K was 0.82 (between 0.78 and 0.81 if any one of the ten items was deleted) (Table 2). The percent agreement between each survey items were between 55.07% and 81.16% with kappa scores of 0.28-0.64 (Table 3).
Table 2. Internal consistency with Cronbach's Alpha and Alpha coefficient if item deleted.
| Scales | Coefficient (n = 184) |
|---|---|
| Alpha | 0.82 |
| Alpha if item deleted | |
| 1. Tired for a long time after activity | 0.79 |
| 2. Poor concentration | 0.80 |
| 3. Muscle tiredness after activity | 0.78 |
| 4. Headaches | 0.80 |
| 5. Sleep for a long time | 0.81 |
| 6. Muscle aches after activity | 0.79 |
| 7. Sleep poorly | 0.81 |
| 8. Problems with speech | 0.80 |
| 9. Poor memory | 0.80 |
| 10. Muscle pain at rest | 0.80 |
Table 3. Test-retest reliability coefficients (Kappa) for the SOFA/GP-K.
| Items | Percent agreement (%) | Kappa score |
|---|---|---|
| 1. Tired for a long time after activity | 62.3 | 0.37 |
| 2. Poor concentration | 69.6 | 0.49 |
| 3. Muscle tiredness after activity | 62.3 | 0.33 |
| 4. Headaches | 79.0 | 0.64 |
| 5. Sleep for a long time | 56.5 | 0.34 |
| 6. Muscle aches after activity | 55.1 | 0.28 |
| 7. Sleep poorly | 68.1 | 0.53 |
| 8. Problems with speech | 70.3 | 0.50 |
| 9. Poor memory | 71.0 | 0.48 |
| 10. Muscle pain at rest | 81.2 | 0.51 |
SOFA/GP-K, Korean Schedule of Fatigue and Anergia/General Physician.
Construct validity
The screen test for the SOFA/GP-K suggested a three-factor solution. The eigenvalue was 3.89 for the first factor; tiredness after physical activity, followed by 1.19 and 1.02 for the next two factors; cognitive dysfunction and residual fatigue (Table 4).
Table 4. Extraction of factors via factor analysis.
| Item No. | Tiredness after physical activity | Cognitive dysfunction | Residual fatigue |
|---|---|---|---|
| 1. Tired for a long time after activity | 0.76 | 0.12 | 0.22 |
| 2. Poor concentration | 0.40 | 0.65 | -0.02 |
| 3. Muscle tiredness after activity | 0.82 | 0.15 | 0.22 |
| 4. Headaches | 0.24 | 0.20 | 0.59 |
| 5. Sleep for a long time | 0.71 | 0.18 | -0.16 |
| 6. Muscle aches after activity | 0.57 | 0.11 | 0.48 |
| 7. Sleep poorly | 0.08 | 0.14 | 0.77 |
| 8. Problems with speech | 0.05 | 0.74 | 0.37 |
| 9. Memory is poor | 0.13 | 0.84 | 0.07 |
| 10. Muscle pain even at rest | 0.40 | 0.25 | 0.52 |
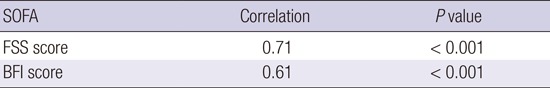
Concurrent validity
The concurrent validity of the SOFA/GP-K was demonstrated by calculating the correlations between the SOFA/GP-K and other fatigue instrument scores, the BFI and FSS (Table 5). The SOFA/GP-K was significantly correlated with the well validated FSS and BFI. The correlation between SOFA/GP-K and FSS was (rho: 0.71, P<0.001) and BFI was (rho: 0.61, P<0.001).
Table 5. Test of validity of SOFA/GP-K.
| SOFA | Correlation | P value |
|---|---|---|
| FSS score | 0.71 | < 0.001 |
| BFI score | 0.61 | < 0.001 |
The Spearman correlation coefficients between scores for SOFA/GP-K items and FSS and BFI. SOFA/GP-K, Korean Schedule of Fatigue and Anergia/General Physician; FSS, fatigue severity scale; BFI, brief fatigue inventory.
DISCUSSION
It is hard to evaluate subjective symptoms such as fatigue when a commonly agreed upon definition is lacking. The usefulness of patient self-reports on subjective symptoms is widely acknowledged, thus a variety of self-report instruments have been developed and are currently in use. Although many of these scales are promising, as of yet there is no fatigue scale designed specifically to screen PFS. A valid and reliable instrument is needed to screen prolonged fatigue and to communicate in the same terms between patients and physicians. To do so, an appropriate validation of the psychometric instrument is essential, even more so when the study is cross-cultural in nature. Hence, a rigorous process of an initial pilot study, translation, back-translation, cross-cultural adaptation and validation was performed according to proposed guidelines by Guillemin et al. (12). The present study is the first to evaluate the validity and reliability of the SOFA/GP in patients visiting primary care units in Korea. Test-retest reliability, internal consistency, and concurrent validity of the questionnaire resulted in excellent validity and fair to moderate reliability. The relatively low missing rate supports that the questionnaire is easy to administer.
The factor analysis gave a three-factor solution, somewhat similar to the results of the original article using latent class analysis. The first factor, related to tiredness after physical activity consisted of 4 items. The second factor consisted of 3 items related to cognitive aspects. The third factor consisted of 3 items, related to neither physical activity nor cognitive function; therefore, we classified them as residual fatigue. The Kappa scores of the test-retest reliabilities for each item are somewhat low, but still respectable (16). The internal consistency was high with a Cronbach's alpha coefficient of 0.82, which shows that the scale is a coherent, additive instrument, in which the individual items have meaning.
SOFA/GP was originally developed to screen for prolonged fatigue states, rather than well-developed chronic fatigue syndrome. It differs from other fatigue evaluating scale in that it is not limited to specific diseases such as cancer, fibromyalgia, neurologic and musculoskeletal disorders, or psychological problems. The high cutoff score of the questionnaire maximizes the specificity for use in the community and primary care facilities. The scales also identify PFS as having quite different characteristics to other common psychological and somatic forms of distress. SOFA/GP differentiates conventional notions of anxiety and depression from PFS, thus recognizing that PFS is not merely somatic symptoms of anxiety and depression. Another distinct advantage of this scale is that the questions are shorter and simpler, allowing subjects to easily complete the entire survey within 2 minutes. SOFA/GP-K uses a Likert scale when evaluating the severity for fatigue rather than the numeric VAS scale as used in FSS. Likert scales have been found to be easier to use and understand for both the researcher and the respondent and that coding as well as interpretation is easier when compared to VAS. It also takes less time to explain to the patients (17). Simplicity is an important advantage, because its main purpose is to assess fatigue. Therefore, it could be argued that a simpler scale, such as the SOFA scale in the form of Likert scale, may be more appropriate when assessing patients with fatigue through its ease of administration.
The current study is subject to several limitations. While presumably healthy, the subjects in our study may differ from the community norms in that they may be more concerned about their health for one reason or another. Although more participants in our study were experiencing stress to a moderate degree (50%) than compared to the low intensity of the general population (57%), the previous study was conducted through telephone interviews of the general population and the results may differ from patients visiting primary care units (11). In addition, if fatigue, through FSS, is defined with a cutoff mean of 3.22 according to previous study (18), our study revealed 40.2% (74/184) of subjects were fatigued. The prevalence of fatigue in Korea's general population is 32.5% (2). However, 45 out of 184 participants (24.5%) of our study were diagnosed with metabolic diseases and cardiovascular diseases, which is similar to the rate in the general population. Therefore, we concluded that subjects visiting a routine health examination center could represent the general Korean population that visits the primary care units. Another possible limitation is that because SOFA/GP is a unidimensional measure of fatigue, it may provide limited reliability and only the most perfunctory information about the patients' experiences with fatigue. However, the SOFA/GP has good psychometric measures as a screening tool to assess fatigue.
In conclusion, our study has shown that the SOFA/GP-K is a reliable, valid self-rating instrument and is suitable for screening for prolonged fatigue. This simple and easily administered measurement of fatigue is essential for studies of its prevalence, severity and for studies of effectiveness of fatigue management in Korea. In a clinical sense, the SOFA/GP-K may minimize barriers of communication between patients and physicians concerning fatigue in Korea. It may additionally provide important and necessary insight into further evaluation and treatment of fatigue. Further studies on the scale's ability to act as an outcome measure with treatment may be necessary.
ACKNOWLEDGMENTS
We thank Dr. Dusan Hadzi-Pavlovic (University of New South Wales, Psychiarty) for his permission to translate the SOFA/GP into Korean. We also thank Hae Lim Kim and Anne Shin for their excellent translation. Finally, we would like to also thank the participants who cooperated willingly.
Appendix SOFA/GP-K
Footnotes
Funding: This study was supported by grant N. 02-2012-055 from the Seoul National University Bundang Hospital Research Fund.
DISCLOSURE: All authors have no potential conflicts of interest to disclose.
AUTHOR CONTRIBUTION: Conception and design: Bae WK, Kim JY, Kim JH. Acquisition of data: Kim S, Jang M. Noh HH. Analysis and interpretation of data: Kim S, Bae WK. First writing of manuscript: Kim S, Jang M. Revision of the manuscript: Kim S, Bae WK. Agree with the manuscript contents and conclusions: Kim S, Bae WK, Kim JY, Kim JH, Jang M, Noh HH.
References
- 1.Dittner AJ, Wessely SC, Brown RG. The assessment of fatigue: a practical guide for clinicians and researchers. J Psychosom Res. 2004;56:157–170. doi: 10.1016/S0022-3999(03)00371-4. [DOI] [PubMed] [Google Scholar]
- 2.Kim CH, Shin HC, Won CW. Prevalence of chronic fatigue and chronic fatigue syndrome in Korea: community-based primary care study. J Korean Med Sci. 2005;20:529–534. doi: 10.3346/jkms.2005.20.4.529. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Hotopf M, Wessely S. Chronic fatigue syndrome--mapping the interior. Psychol Med. 1999;29:255–258. doi: 10.1017/s0033291798008265. [DOI] [PubMed] [Google Scholar]
- 4.Hadzi-Pavlovic D, Hickie IB, Wilson AJ, Davenport TA, Lloyd AR, Wakefield D. Screening for prolonged fatigue syndromes: validation of the SOFA scale. Soc Psychiatry Psychiatr Epidemiol. 2000;35:471–479. doi: 10.1007/s001270050266. [DOI] [PubMed] [Google Scholar]
- 5.Elnicki DM, Shockcor WT, Brick JE, Beynon D. Evaluating the complaint of fatigue in primary care: diagnoses and outcomes. Am J Med. 1992;93:303–306. doi: 10.1016/0002-9343(92)90237-6. [DOI] [PubMed] [Google Scholar]
- 6.Yun YH, Wang XS, Lee JS, Roh JW, Lee CG, Lee WS, Lee KS, Bang SM, Mendoza TR, Cleeland CS. Validation study of the korean version of the brief fatigue inventory. J Pain Symptom Manage. 2005;29:165–172. doi: 10.1016/j.jpainsymman.2004.04.013. [DOI] [PubMed] [Google Scholar]
- 7.Lee JH, Jeong HS, Lim SM, Cho HB, Ma JY, Ko E, Im JJ, Lee SH, Bae S, Lee YJ, et al. Reliability and validity of the fatigue severity scale among university student in South Korea. Korean J Biol Psychiatry. 2013;20:6–11. [Google Scholar]
- 8.Krupp LB, LaRocca NG, Muir-Nash J, Steinberg AD. The fatigue severity scale. Application to patients with multiple sclerosis and systemic lupus erythematosus. Arch Neurol. 1989;46:1121–1123. doi: 10.1001/archneur.1989.00520460115022. [DOI] [PubMed] [Google Scholar]
- 9.Yun YH, Lee MK, Chun HN, Lee YM, Park SM, Mendoza TR, Wang XS, Cleeland CS. Fatigue in the general Korean population: application and normative data of the Brief Fatigue Inventory. J Pain Symptom Manage. 2008;36:259–267. doi: 10.1016/j.jpainsymman.2007.10.016. [DOI] [PubMed] [Google Scholar]
- 10.Cho HJ, Costa E, Menezes PR, Chalder T, Bhugra D, Wessely S. Cross-cultural validation of the Chalder Fatigue Questionnaire in Brazilian primary care. J Psychosom Res. 2007;62:301–304. doi: 10.1016/j.jpsychores.2006.10.018. [DOI] [PubMed] [Google Scholar]
- 11.Kim KN, Park JY, Shin TS, Jun KJ, Choi EY, Kim HJ, Lee SH, Yoo TW, Huh BY. Degree of stress and stress-related factors by the Korean version of the BEPSI. J Korean Acad Fam Med. 1998;19:559–570. [Google Scholar]
- 12.Guillemin F, Bombardier C, Beaton D. Cross-cultural adaptation of health-related quality of life measures: literature review and proposed guidelines. J Clin Epidemiol. 1993;46:1417–1432. doi: 10.1016/0895-4356(93)90142-n. [DOI] [PubMed] [Google Scholar]
- 13.Mendoza TR, Wang XS, Cleeland CS, Morrissey M, Johnson BA, Wendt JK, Huber SL. The rapid assessment of fatigue severity in cancer patients: use of the Brief Fatigue Inventory. Cancer. 1999;85:1186–1196. doi: 10.1002/(sici)1097-0142(19990301)85:5<1186::aid-cncr24>3.0.co;2-n. [DOI] [PubMed] [Google Scholar]
- 14.Anton HA, Miller WC, Townson AF. Measuring fatigue in persons with spinal cord injury. Arch Phys Med Rehabil. 2008;89:538–542. doi: 10.1016/j.apmr.2007.11.009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Herlofson K, Larsen JP. Measuring fatigue in patients with Parkinson's disease - the Fatigue Severity Scale. Eur J Neurol. 2002;9:595–600. doi: 10.1046/j.1468-1331.2002.00444.x. [DOI] [PubMed] [Google Scholar]
- 16.Viera AJ, Garrett JM. Understanding interobserver agreement: the kappa statistic. Fam Med. 2005;37:360–363. [PubMed] [Google Scholar]
- 17.Hasson D, Arnetz BB. Validation and findings comparing VAS vs. Likert scales for psychosocial measurements. Int Electron J Health Educ. 2005;8:178–192. [Google Scholar]
- 18.Chung KI, Song CH. Clinical usefulness of Fatigue Severity Scale for patients with fatigue, and anxiety or depression. Korean J Psychosom Med. 2001;9:164–173. [Google Scholar]