Abstract
We investigated the clinical and biological significance of germinal centers (GC) present in the minor salivary glands of patients with Sjögren’s syndrome (SS). Minor salivary gland tissue biopsies from 93 patients with SS were used to identify GC-like structures, which were confirmed by CD21-positive follicular dendritic cell networks. Patients were compared based upon sociodemographics, glandular and extraglandular manifestations, and laboratory findings including autoantibody profiles, complement, and immunoglobulin levels; EULAR SS disease activity index (ESSDAI) and SS disease damage index (SSDDI) were also measured. GC-like structures were observed in 28 of 93 SS patients (30.1%). Mean focus scores and CRP levels were significantly higher in GC-positive patients than in GC-negative patients; GC-positive patients also exhibit a higher prevalence of rheumatoid factor and anti-SS-A/Ro antibodies compared to GC-negative patients. No differences in glandular or extra-glandular manifestations were evident between groups. In conclusion, SS patients with GC-like structures in the minor salivary glands exhibited laboratory profiles significantly different from those of their GC-negative counterparts. Long-term follow-up of these patients will be necessary to determine whether these laboratory abnormalities are predictive of clinical outcomes.
Keywords: Germinal Center, Sjögren’s Syndrome, Biopsy, Salivary Glands
Graphical Abstract
INTRODUCTION
Sjögren’s syndrome (SS) is chronic autoimmune inflammatory disease characterized by sicca symptoms and various extraglandular manifestations (1,2). Disease symptoms are driven in part by lymphocytic infiltration into the exocrine glands consists primarily of T cells and B cells, resulting in dysregulation of the Th1/Th2 balance and B cell hyperactivity (3,4). Over time, these chronic immune cell disturbances manifest in a variety of ways, including hypergammaglobulinemia, circulating immune complexes, organ-specific autoantibodies such as anti-SS-A/Ro or anti-SS-B/La, non-specific autoantibodies such as rheumatoid factor (RF), formation of ectopic germinal center (GC)-like structures, and the enhanced risk of B cell lymphoma (5,6,7,8,9,10).
Studies have shown lymphoid infiltrates in SS organizing into structures resembling the germinal centers of secondary lymphoid tissues, at frequencies ranging from 18% to 59% of all SS patients (6,9,11,12,13,14). Similar lymphoid infiltrates have also been described in the affected tissues of other autoimmune diseases, including the synovium in rheumatoid arthritis (RA) (15), the thyroids in Hashimoto’s thyroiditis (16), the thymus in myasthenia gravis (17), the central nervous system in multiple sclerosis (18), and the gastric mucosa during chronic Helicobacter pylori infections (19).
As GCs play a pivotal role in driving both T and B cell activation, their presence within the glandular infiltrates of SS patients is thought to play a significant role disease progression (20). In several previous studies (12,13,21,22,23,24), SS patients exhibiting GC-like structures in the minor salivary glands have showed a higher prevalence of anti-SS-A/Ro or anti-SS-B/La antibodies (Ab) or rheumatoid factor (RF), higher lymphocyte focus score in minor salivary gland biopsy, enhanced levels of local and systemic proinflammatory mediators, and higher risk of lymphoma development compared with GC-negative SS patients. While the presence of ectopic GC-like structures in chronic inflammatory diseases is not a new finding, the role of GCs in SS is still being defined. Here, we analyzed the prevalence of GCs in minor salivary glands of patients with SS, and compared their laboratory and clinical profiles with that of GC-negative patients.
MATERIALS AND METHODS
Population and study design
We performed a retrospective analysis of medical records from 93 SS patients seen in our outpatient clinic from January 2006 to March 2012. We included patients who underwent minor salivary gland biopsies in the process of diagnosing SS and finally confirmed the diagnosis using the revised criteria proposed by the American-European Consensus Group (AECG). As part of routine evaluation for SS, all patients underwent ophthalmologic test, 99-mTc salivary glands scintigraphy, and laboratory tests. Schirmer’s tests were performed by an ophthalmologist, with a positive diagnosis defined as < 5 mm in 5 minutes. Next, a tear film break-up time (BUT) test was performed, with a positive result defined as < 10 seconds. Salivary glands scintigraphy with 99-mTc was considered positive when the tracer showed delayed uptake, reduced concentration, or delayed excretion.
Clinical and laboratory manifestations
Sociodemographic, clinical, and laboratory data were collected at the time of minor salivary gland biopsy and again during follow-up period. Patients were examined by an experienced rheumatologist to assess common disease symptoms, including sicca symptoms and symptom onset age, enlargement of parotid glands, and experience of extraglandular manifestations such as photosensitivity, purpura, Raynaud’s phenomenon, sclerodactyly, arthritis, psychosis and lymphadenopathy. Interstitial lung disease or pulmonary fibrosis was documented based on chest radiograph or high-resolution computed tomography (HRCT). Renal involvement was defined as proteinuria (> 500 mg/day), active urine sediment, impaired glomerular filtration rate (GFR) (< 60 mL/minute) or renal tubular acidosis. Serositis was defined by radiologic pleural effusion or pericardial effusion. Gastroesophageal reflux was diagnosed by gastroscopy in patients with symptoms of heartburn or regurgitation. Carpal tunnel syndrome was diagnosed based upon complaints of abnormal sensation and confirmed using a nerve conduction study. Autoimmune thyroiditis was defined as hypothyroidism in combination with increased autoantibody levels such as anti-thyroid peroxidase or anti-thyroglobulin antibodies. Lymphoma was confirmed by lymph node biopsy. To measure disease activity and degree of damage, we used the EULAR SS disease activity index (ESSDAI) and SS disease damage index (SSDDI), respectively. ESSDAI and SSDDI were completed retrospectively by reviewing the medical records carefully.
Routine laboratory profiles were performed at the time of the labial salivary gland biopsy to measure white blood cell (WBC) count, lymphocyte, hemoglobin, platelets, erythrocyte sedimentation rate (ESR), C-reactive protein (CRP), immunoglobulin G (IgG), IgA, IgM, and complement level (C3, C4, CH50). CRP was measured with a turbidimetric immunoassay (Wako, Osaka, Japan), IgG, IgA, IgM, C3, and C4 were measured using nephelometric assays (Siemens, Marburg, Germany) and CH50 was measured with an liposome immunoassay (Wako, Osaka, Japan). The presence of autoantibodies against SS-A/Ro, SS-B/La (ORGENTEC Diagnostika, Mainz, Germany), and dsDNA (Trinity Biotec, Wicklow, Ireland) was determined by ELISA; rheumatoid factor was assessed by nephelometry (Beckman Coulter, Galway, Ireland).
Tissue samples and immunohistochemistry
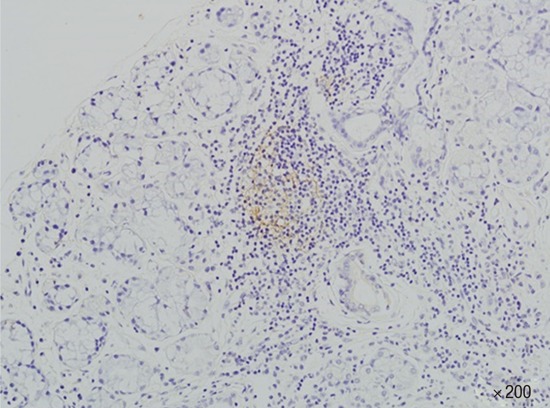
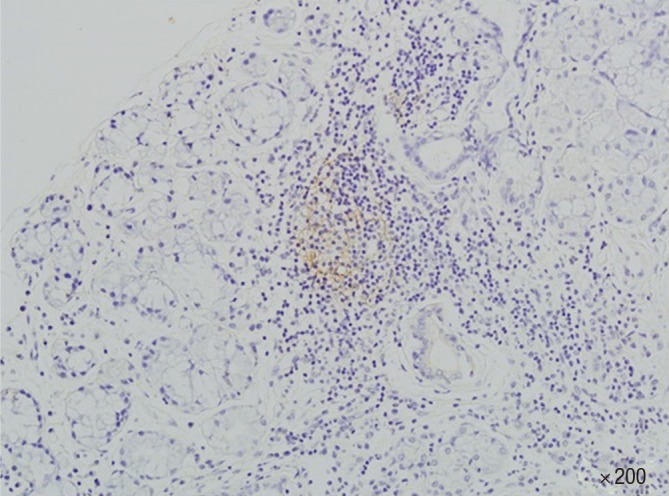
A labial salivary gland biopsy was performed for all SS patients. The focus score (FS) was determined using the classification method of Chisholm and Mason, defined as the number of inflammatory cell foci containing at least 50 mononuclear cells per 4 mm2 within otherwise normal salivary gland epithelium. Hematoxylin and eosin (H&E) stained paraffin-embedded labial salivary gland tissue sections were screened morphologically for the presence of GC-like structures containing at least 50 mononuclear cells consisting of a densely packed dark zone and a light zone. Ectopic GCs were confirmed by immunohistochemical (IHC) staining indicating the presence of a CD21-positive network-like morphology (Fig. 1). All of the slides were reviewed with a pathologist who was blinded to the patient data and any discrepancies were resolved by discussion. The presence of GC was confirmed by another pathologist.
Fig. 1. Immunohistochemical staining of minor salivary gland tissue from a patient with Sjögren’s syndrome. Germinal center was identified by morphology in H&E and confirmed by the positivity of CD21.
Statistical analyses
Data we analyzed using the SPSS software version 18 (SPSS, Chicago, IL, USA). Comparisons between groups were performed using the Mann-Whitney U test for continuous variables, and chi-squared test for categorical data. P values < 0.05 were considered to indicate statistical significance.
Ethics statement
This study was approved by the institutional review board of Chonnam National University Hospital (IRB No. CNUH-2015-049). Informed consent was waived by the IRB.
RESULTS
A total of 93 patients was included in this study, consisted of 2 males and 91 females. The mean age at the time of minor salivary gland biopsy was 44.91 ± 11.61 years; the mean age of sicca symptom onset was 42.40 ± 10.95 years. GCs were detected in 28 of 93 patients (30.1%), with one male present in each group. The mean follow-up period for all patients was 40.88 ± 34.71 months (range: 3.1–157.4 months). Three patients were lost to follow-up because they did not visit the clinic, and one patient died due to pneumonia. The sociodemographic and clinical manifestations of each group at the time of minor salivary gland biopsy are summarized in Table 1.
Table 1. Baseline sociodemographic characteristics and clinical manifestations at the time of the minor salivary gland biopsy.
| Characteristics | Germinal center (+) (N = 28) |
Germinal center (-) (N = 65) |
P value |
|---|---|---|---|
| Age (yr) | 43.39 ± 12.79 | 45.08 ± 11.69 | 0.451 |
| Female (%) | 27/28 (96.4) | 64/65 (98.5) | 0.514 |
| Sicca symptom onset age (yr) | 40.86 ± 11.82 | 42.12 ± 11.04 | 0.471 |
| Glandular manifestation | |||
| Ocular symptom (%) | 28/28 (100) | 64/65 (98.5) | 1.000 |
| Oral symptom (%) | 28/28 (100) | 61/65 (93.8) | 0.312 |
| Schirmer's test positive rates (%) | 23/28 (82.1) | 59/65 (90.8) | 0.297 |
| BUT positive rates (%) | 28/28 (100) | 64/65 (98.5) | 1.000 |
| Enlargement of parotid glands (%) | 3/28 (10.7) | 5/65 (7.7) | 0.693 |
| Salivary scan positive rates (%) | 26/26 (100) | 55/62 (88.7) | 0.099 |
| Extraglandular manifestation | |||
| Photosensitivity (%) | 3/28 (10.7) | 5/65 (7.7) | 0.693 |
| Arthritis (%) | 14/28 (50.0) | 43/65 (66.2) | 0.142 |
| Raynaud's phenomenon (%) | 6/28 (21.4) | 15/65 (23.1) | 0.862 |
| Renal involvement (%) | 2/28 (7.1) | 1/65 (1.5) | 0.215 |
| Distal RTA (%) | 0/28 (0) | 3/65 (4.6) | 0.551 |
| Psychosis (%) | 0/28 (0) | 3/65 (4.6) | 0.551 |
| Purpura (%) | 1/28 (3.6) | 3/65 (4.6) | 1.000 |
| Serositis (%) | 2/28 (7.1) | 2/65 (3.1) | 0.581 |
| Lymphadenopathy (%) | 6/28 (21.4) | 8/65 (12.3) | 0.343 |
| Lymphoma (%) | 1/28 (3.6) | 0/65 (0) | 0.301 |
| ILD/pulmonary fibrosis (%) | 0/28 (0) | 5/65 (7.7) | 0.318 |
| Sclerodactyly (%) | 1/28 (3.6) | 0/65 (0) | 0.301 |
| GER (%) | 3/28 (10.7) | 7/65 (10.8) | 1.000 |
| Autoimmune thyroiditis (%) | 5/28 (17.9) | 3/65 (4.6) | 0.051 |
| Carpal tunnel syndrome (%) | 1/28 (3.6) | 0/65 (0) | 0.301 |
| Focus score | 2.71 ± 0.66 | 1.65 ± 0.97 | <0.001 |
| ESSDAI | 3.04 ± 2.24 | 2.65 ± 1.58 | 0.560 |
| SSDDI | 1.14 ± 1.41 | 1.18 ± 0.83 | 0.256 |
Data are presented as means ± SD.
BUT, Tear film break-up time; ESSDAI, EULAR Sjögren’s syndrome disease activity index; GER, gastro-esophageal reflux; ILD, Interstitial lung disease; SSDDI, Sjögren’s syndrome disease damage index.
The age at the time of minor salivary gland biopsy and the age at sicca symptom onset did not differ significantly between GC-positive and GC-negative SS patients. Glandular manifestations including dry eye, dry mouth, positive rates of Schirmer’s test, positive rates of tear film break-up time, parotid gland enlargement, and salivary scan positivity were also similar between groups. In terms of extraglandular manifestations, autoimmune thyroiditis was more common in GC-positive SS patients than in GC-negative SS patients (17.9% vs. 4.6%, respectively; P = 0.051). Other extraglandular manifestations including photosensitivity, arthritis, Raynaud’s phenomenon, renal involvement, distal RTA, psychosis, purpura, serositis, lymphadenopathy, lymphoma, interstitial lung disease, pulmonary fibrosis, sclerodactyly, gastro-esophageal reflux, and carpal tunnel syndrome did not differ between the two groups. No patients exhibited either primary biliary cirrhosis or autoimmune hepatitis. The focus scores of GC-positive SS patients were significantly higher than GC-negative SS patients (2.71 ± 0.66 vs. 1.65 ± 0.97, respectively; P < 0.001). For clinical manifestations, ESSDAI and SSDDI did not differ between the two groups.
Laboratory and immunological manifestations are described in Table 2. CRP was significantly higher in GC-positive SS patients than GC-negative SS patients (0.62 ± 0.97 mg/dL vs. 0.35 ± 0.52 mg/dL, respectively; P = 0.046); other laboratory findings, including WBC count, lymphocyte, hemoglobin, platelets, ESR, IgG, IgA, IgM, C3, C4, and CH50 were not significantly different between groups. Among autoantibodies, RF levels were significantly higher among GC-positive patients compared as compared to their GC-negative counterparts (70.55 ± 94.61 vs. 35.84 ± 66.62 mg/dL, respectively; P = 0.002), with a significantly higher degree of RF positivity in GC-positive patients (66.7% vs. 41.3%, P = 0.027). Anti-SS-A/Ro titer was also higher in GC-positive SS patients (171.8 ± 71.46 vs. 141.6 ± 85.47 mg/dL, respectively; P = 0.02). Other autoantibodies, including anti-SS-B/La titer, as well as the positive rates of anti-SS-A/Ro, anti-SS-B/La, and anti-dsDNA did not differ significantly between the two groups.
Table 2. Laboratory and immunologic manifestations.
| Parameters | Germinal center (+) (N = 28) |
Germinal center (-) (N = 65) |
P value |
|---|---|---|---|
| WBC (/µL) | 5,400 ± 1,872 | 5,341 ± 1,986 | 0.769 |
| Lymphocyte (/µL) | 1671 ± 576.6 | 1746 ± 689.4 | 0.788 |
| Hgb (g/dL) | 11.96 ± 1.669 | 12.46 ± 1.420 | 0.254 |
| Platelet (103/µL) | 208.6 ± 64.00 | 241.4 ± 70.98 | 0.111 |
| ESR (mm/hr) | 43.07 ± 26.91 | 40.51 ± 29.66 | 0.513 |
| CRP (mg/dL) | 0.62 ± 0.97 | 0.35 ± 0.52 | 0.046 |
| Ig G (mg/dL) | 2,053 ± 604.2 | 2,080 ± 737.1 | 0.691 |
| Ig A (mg/dL) | 335.1 ± 113.3 | 304.7 ± 128.9 | 0.072 |
| Ig M (mg/dL) | 139.2 ± 57.52 | 167.5 ± 161.6 | 0.904 |
| C3 (mg/dL) | 97.02 ± 23.68 | 100.6 ± 23.79 | 0.577 |
| C4 (mg/dL) | 19.88 ± 8.065 | 20.30 ± 9.235 | 0.997 |
| CH50 (U/mL) | 52.01 ± 15.76 | 51.74 ± 12.57 | 0.975 |
| RF (IU/mL) | 70.55 ± 94.61 | 35.84 ± 66.62 | 0.002 |
| Anti-SS-A/Ro (U/mL) | 171.8 ± 71.46 | 141.6 ± 85.47 | 0.020 |
| Anti-SS-B/La (U/mL) | 42.90 ± 62.63 | 46.26 ± 71.42 | 0.740 |
| RF (%) | 18/27 (66.7) | 26/63 (41.3) | 0.027 |
| Anti-SS-A/Ro (%) | 26/28 (92.9) | 55/65 (84.6) | 0.336 |
| Anti-SS-B/La (%) | 12/28 (42.9) | 25/65 (38.5) | 0.691 |
| Anti-dsDNA (%) | 7/26 (26.9) | 15/60 (24.6) | 0.819 |
Data are presented as means ± SD.
WBC, white blood cell; CRP, C-reactive protein; ESR, erythrocyte sedimentation rate; Hgb, hemoglobin; Ig, immunoglobulin; RF, rheumatoid factor.
DISCUSSION
In this study, 30.1% of SS patients were positive for GC formation. Presence of these GCs was significantly associated with increases in mean focus score, CRP levels, RF prevalence, and anti-SSA/Ro antibody titers relative to that of GC-negative patients. However, despite these differences clinical manifestations were not significantly different between the two groups.
Differences in GC status were not associated with age, gender ratio, sicca symptoms, or salivary dysfunction. Many studies have reported decreases in salivary production among GC-positive SS patients (12,13,25,26); while this study did not measure saliva secretion, severe glandular dysfunction was evident in both groups. As glandular secretions tend to be lower across all SS patients, these data therefore imply mechanisms other than ectopic GCs in salivary gland as a cause of sicca symptoms and glandular dysfunction.
In this study, mean focus scores of minor salivary gland biopsies were significantly higher in GC-positive SS patients relative to their GC-negative counterparts, consistent with previous results (13,23,24,25,26). Chronic inflammation is associated with progressive lymphocyte recruitment, resulting in ectopic GC formation as these diffuse infiltrates transition to more highly organized structures (27). These GCs would lead to progressive increases in lymphocyte infiltration by facilitating interactions between surrounding inflammatory cells, adhesion molecules, cytokines, and chemokines, resulting in higher focus scores in the salivary glands of SS patients.
In terms of laboratory findings, GC-positive patients exhibited increased prevalence of RF, higher titers of anti-SS-A/Ro Ab, and higher CRP levels compared to GC-negative patients. These results are broadly consistent with previous reports, which tend to describe SS patients with ectopic GC-like structures as having higher prevalence of RF, anti-SS-A/Ro, and anti-SS-B/La (12,13,21,26). Moreover, our results revealed increased CRP, a classic inflammation, in the GC-positive group. Other groups have reported increases in a range of inflammatory mediators, including activation-induced cytidine deaminase (AID) and cytokines in GC-positive patients (21,24,26,28,29), however there have been no reports of increased CRP production in SS. Like other inflammatory mediators, the serum CRP would be elevated in the presence of GCs, which are closely associated with inflammation. As CRP is sensitive to various inflammatory and other factors, the significance of this result remains to be seen. Further research will be necessary to determine both the cause of this increase, as well as the clinical implications of such as response. While the relation between GCs, autoantibodies, and inflammatory mediators in this situation is not fully understood, GCs should play an important role in driving T and B cell activation and disturbances of B cell maturation, which results in increased production of autoantibodies, inflammatory chemokines and cytokines. Taken together, GCs clearly contribute to the inflammation and immune activation seen in SS, though other functions may also be possible.
For extraglandular manifestations, Hashimoto’s thyroiditis was more common in GC-positive SS patients than in GC-negative SS patients, though this difference was not statistically significant; other extraglandular features, including lymphoma, were also statistically similar between groups. No differences in either ESSDAI or SSDDI scores were evident between groups. These observations are similar to that of other studies, with the exception of lymphoma, which has found to be significantly associated with ectopic GCs in SS patients (21,29). As a whole, SS patients are 16 to 44-fold more likely to develop lymphoma, with upwards of 5%-10% of all patients expected to develop some form of lymphoma, particularly non-Hodgkin’s lymphoma (30,31,32). The most common predictors of lymphoma in SS patients include persistent or recurrent salivary gland swelling, palpable purpura, skin vasculitis, and low C4, though a direct association between ectopic GCs and lymphoma has also been shown (21,30). Our data failed to observe any such association between GCs and lymphoma, with only one of our GC-positive SS patients diagnosed with lymphoma. The most likely cause of this difference is the relatively short duration of this study, suggesting a need for both close monitoring and long-term follow-up of these patients.
The main limitation of this study is its retrospective design. To fully establish an association between GCs, disease pathology, and clinical features, a prospective would be necessary, incorporating a wide range of laboratory, histological, and clinical measurements. Furthermore, as our data was collected using a standard medical chart review, recall bias may have influenced the assessment of some clinical features.
In conclusion, SS patients with ectopic GC-like structures exhibit similar glandular dysfunction, but differ from GC-negative patients across several laboratory parameters. The formation of ectopic GC within the salivary glands of SS patients may be an important step in the process of lymphocytic sialadenitis. Although our study failed to identify any significant associations between the presence of GC and clinical features, GC-positive SS patients do exhibit distinct serological features; long-term follow-up of these patients will be necessary to determine whether these laboratory abnormalities translate into important clinical outcomes.
Footnotes
Funding: This study was supported by a grant (CRI13904-24.3) Chonnam National University Hospital Biomedical Research Institute.
DISCLOSURE: The authors declare no conflicts of interest to disclose.
AUTHOR CONTRIBUTION: Study conception and design: Lee KE, Park DJ, Yoon KC, Lee SS. Acquisition of data: Lee KE, Kang JH, Yim YR, Kim JE, Lee JW, Wen L, Park DJ, Kim TJ, Park WY. Analysis and interpretation of data: Lee KE, Yoon KC, Lee JS, Lee SS. Writing: Lee KE, Lee SS. Revision: all authors. Final approval and responsibility for the integrity: all authors.
References
- 1.Kassan SS, Moutsopoulos HM. Clinical manifestations and early diagnosis of Sjögren syndrome. Arch Intern Med. 2004;164:1275–1284. doi: 10.1001/archinte.164.12.1275. [DOI] [PubMed] [Google Scholar]
- 2.Hansen A, Lipsky PE, Dörner T. Immunopathogenesis of primary Sjögren’s syndrome: implications for disease management and therapy. Curr Opin Rheumatol. 2005;17:558–565. doi: 10.1097/01.bor.0000172801.56744.c3. [DOI] [PubMed] [Google Scholar]
- 3.Hagiwara E, Pando J, Ishigatsubo Y, Klinman DM. Altered frequency of type 1 cytokine secreting cells in the peripheral blood of patients with primary Sjögren’s syndrome. J Rheumatol. 1998;25:89–93. [PubMed] [Google Scholar]
- 4.Mitsias DI, Tzioufas AG, Veiopoulou C, Zintzaras E, Tassios IK, Kogopoulou O, Moutsopoulos HM, Thyphronitis G. The Th1/Th2 cytokine balance changes with the progress of the immunopathological lesion of Sjogren’s syndrome. Clin Exp Immunol. 2002;128:562–568. doi: 10.1046/j.1365-2249.2002.01869.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Bohnhorst JO, Bjørgan MB, Thoen JE, Jonsson R, Natvig JB, Thompson KM. Abnormal B cell differentiation in primary Sjögren’s syndrome results in a depressed percentage of circulating memory B cells and elevated levels of soluble CD27 that correlate with Serum IgG concentration. Clin Immunol. 2002;103:79–88. doi: 10.1006/clim.2002.5199. [DOI] [PubMed] [Google Scholar]
- 6.Amft N, Curnow SJ, Scheel-Toellner D, Devadas A, Oates J, Crocker J, Hamburger J, Ainsworth J, Mathews J, Salmon M, et al. Ectopic expression of the B cell-attracting chemokine BCA-1 (CXCL13) on endothelial cells and within lymphoid follicles contributes to the establishment of germinal center-like structures in Sjögren’s syndrome. Arthritis Rheum. 2001;44:2633–2641. doi: 10.1002/1529-0131(200111)44:11<2633::aid-art443>3.0.co;2-9. [DOI] [PubMed] [Google Scholar]
- 7.Hansen A, Gosemann M, Pruss A, Reiter K, Ruzickova S, Lipsky PE, Dörner T. Abnormalities in peripheral B cell memory of patients with primary Sjögren’s syndrome. Arthritis Rheum. 2004;50:1897–1908. doi: 10.1002/art.20276. [DOI] [PubMed] [Google Scholar]
- 8.Hansen A, Odendahl M, Reiter K, Jacobi AM, Feist E, Scholze J, Burmester GR, Lipsky PE, Dörner T. Diminished peripheral blood memory B cells and accumulation of memory B cells in the salivary glands of patients with Sjögren’s syndrome. Arthritis Rheum. 2002;46:2160–2171. doi: 10.1002/art.10445. [DOI] [PubMed] [Google Scholar]
- 9.Szodoray P, Alex P, Jonsson MV, Knowlton N, Dozmorov I, Nakken B, Delaleu N, Jonsson R, Centola M. Distinct profiles of Sjögren’s syndrome patients with ectopic salivary gland germinal centers revealed by serum cytokines and BAFF. Clin Immunol. 2005;117:168–176. doi: 10.1016/j.clim.2005.06.016. [DOI] [PubMed] [Google Scholar]
- 10.Hansen A, Lipsky PE, Dörner T. B cells in Sjögren’s syndrome: indications for disturbed selection and differentiation in ectopic lymphoid tissue. Arthritis Res Ther. 2007;9:218. doi: 10.1186/ar2210. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Stott DI, Hiepe F, Hummel M, Steinhauser G, Berek C. Antigen-driven clonal proliferation of B cells within the target tissue of an autoimmune disease. The salivary glands of patients with Sjögren’s syndrome. J Clin Invest. 1998;102:938–946. doi: 10.1172/JCI3234. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Jonsson MV, Skarstein K, Jonsson R, Brun JG. Serological implications of germinal center-like structures in primary Sjögren’s syndrome. J Rheumatol. 2007;34:2044–2049. [PubMed] [Google Scholar]
- 13.Jonsson MV, Skarstein K. Follicular dendritic cells confirm lymphoid organization in the minor salivary glands of primary Sjögren’s syndrome. J Oral Pathol Med. 2008;37:515–521. doi: 10.1111/j.1600-0714.2008.00674.x. [DOI] [PubMed] [Google Scholar]
- 14.Risselada AP, Looije MF, Kruize AA, Bijlsma JW, van Roon JA. The role of ectopic germinal centers in the immunopathology of primary Sjögren’s syndrome: a systematic review. Semin Arthritis Rheum. 2013;42:368–376. doi: 10.1016/j.semarthrit.2012.07.003. [DOI] [PubMed] [Google Scholar]
- 15.Takemura S, Braun A, Crowson C, Kurtin PJ, Cofield RH, O’Fallon WM, Goronzy JJ, Weyand CM. Lymphoid neogenesis in rheumatoid synovitis. J Immunol. 2001;167:1072–1080. doi: 10.4049/jimmunol.167.2.1072. [DOI] [PubMed] [Google Scholar]
- 16.Armengol MP, Juan M, Lucas-Martín A, Fernández-Figueras MT, Jaraquemada D, Gallart T, Pujol-Borrell R. Thyroid autoimmune disease: demonstration of thyroid antigen-specific B cells and recombination-activating gene expression in chemokine-containing active intrathyroidal germinal centers. Am J Pathol. 2001;159:861–873. doi: 10.1016/S0002-9440(10)61762-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Sims GP, Shiono H, Willcox N, Stott DI. Somatic hypermutation and selection of B cells in thymic germinal centers responding to acetylcholine receptor in myasthenia gravis. J Immunol. 2001;167:1935–1944. doi: 10.4049/jimmunol.167.4.1935. [DOI] [PubMed] [Google Scholar]
- 18.Serafini B, Rosicarelli B, Magliozzi R, Stigliano E, Aloisi F. Detection of ectopic B-cell follicles with germinal centers in the meninges of patients with secondary progressive multiple sclerosis. Brain Pathol. 2004;14:164–174. doi: 10.1111/j.1750-3639.2004.tb00049.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Mazzucchelli L, Blaser A, Kappeler A, Schärli P, Laissue JA, Baggiolini M, Uguccioni M. BCA-1 is highly expressed in Helicobacter pylori-induced mucosa-associated lymphoid tissue and gastric lymphoma. J Clin Invest. 1999;104:R49–54. doi: 10.1172/JCI7830. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Vinuesa CG, Sanz I, Cook MC. Dysregulation of germinal centres in autoimmune disease. Nat Rev Immunol. 2009;9:845–857. doi: 10.1038/nri2637. [DOI] [PubMed] [Google Scholar]
- 21.Theander E, Vasaitis L, Baecklund E, Nordmark G, Warfvinge G, Liedholm R, Brokstad K, Jonsson R, Jonsson MV. Lymphoid organisation in labial salivary gland biopsies is a possible predictor for the development of malignant lymphoma in primary Sjögren’s syndrome. Ann Rheum Dis. 2011;70:1363–1368. doi: 10.1136/ard.2010.144782. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Manoussakis MN, Boiu S, Korkolopoulou P, Kapsogeorgou EK, Kavantzas N, Ziakas P, Patsouris E, Moutsopoulos HM. Rates of infiltration by macrophages and dendritic cells and expression of interleukin-18 and interleukin-12 in the chronic inflammatory lesions of Sjögren’s syndrome: correlation with certain features of immune hyperactivity and factors associated with high risk of lymphoma development. Arthritis Rheum. 2007;56:3977–3988. doi: 10.1002/art.23073. [DOI] [PubMed] [Google Scholar]
- 23.Salomonsson S, Jonsson MV, Skarstein K, Brokstad KA, Hjelmström P, Wahren-Herlenius M, Jonsson R. Cellular basis of ectopic germinal center formation and autoantibody production in the target organ of patients with Sjögren’s syndrome. Arthritis Rheum. 2003;48:3187–3201. doi: 10.1002/art.11311. [DOI] [PubMed] [Google Scholar]
- 24.Jonsson MV, Szodoray P, Jellestad S, Jonsson R, Skarstein K. Association between circulating levels of the novel TNF family members APRIL and BAFF and lymphoid organization in primary Sjögren’s syndrome. J Clin Immunol. 2005;25:189–201. doi: 10.1007/s10875-005-4091-5. [DOI] [PubMed] [Google Scholar]
- 25.Szyszko EA, Brokstad KA, Oijordsbakken G, Jonsson MV, Jonsson R, Skarstein K. Salivary glands of primary Sjögren’s syndrome patients express factors vital for plasma cell survival. Arthritis Res Ther. 2011;13:R2. doi: 10.1186/ar3220. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Reksten TR, Jonsson MV, Szyszko EA, Brun JG, Jonsson R, Brokstad KA. Cytokine and autoantibody profiling related to histopathological features in primary Sjogren’s syndrome. Rheumatology (Oxford) 2009;48:1102–1106. doi: 10.1093/rheumatology/kep149. [DOI] [PubMed] [Google Scholar]
- 27.Aloisi F, Pujol-Borrell R. Lymphoid neogenesis in chronic inflammatory diseases. Nat Rev Immunol. 2006;6:205–217. doi: 10.1038/nri1786. [DOI] [PubMed] [Google Scholar]
- 28.Barone F, Bombardieri M, Manzo A, Blades MC, Morgan PR, Challacombe SJ, Valesini G, Pitzalis C. Association of CXCL13 and CCL21 expression with the progressive organization of lymphoid-like structures in Sjögren’s syndrome. Arthritis Rheum. 2005;52:1773–1784. doi: 10.1002/art.21062. [DOI] [PubMed] [Google Scholar]
- 29.Bombardieri M, Barone F, Humby F, Kelly S, McGurk M, Morgan P, Challacombe S, De Vita S, Valesini G, Spencer J, et al. Activation-induced cytidine deaminase expression in follicular dendritic cell networks and interfollicular large B cells supports functionality of ectopic lymphoid neogenesis in autoimmune sialoadenitis and MALT lymphoma in Sjögren’s syndrome. J Immunol. 2007;179:4929–4938. doi: 10.4049/jimmunol.179.7.4929. [DOI] [PubMed] [Google Scholar]
- 30.Voulgarelis M, Dafni UG, Isenberg DA, Moutsopoulos HM. Malignant lymphoma in primary Sjögren’s syndrome: a multicenter, retrospective, clinical study by the European Concerted Action on Sjögren’s Syndrome. Arthritis Rheum. 1999;42:1765–1772. doi: 10.1002/1529-0131(199908)42:8<1765::AID-ANR28>3.0.CO;2-V. [DOI] [PubMed] [Google Scholar]
- 31.Theander E, Henriksson G, Ljungberg O, Mandl T, Manthorpe R, Jacobsson LT. Lymphoma and other malignancies in primary Sjögren’s syndrome: a cohort study on cancer incidence and lymphoma predictors. Ann Rheum Dis. 2006;65:796–803. doi: 10.1136/ard.2005.041186. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Smedby KE, Hjalgrim H, Askling J, Chang ET, Gregersen H, Porwit-MacDonald A, Sundström C, Akerman M, Melbye M, Glimelius B, et al. Autoimmune and chronic inflammatory disorders and risk of non-Hodgkin lymphoma by subtype. J Natl Cancer Inst. 2006;98:51–60. doi: 10.1093/jnci/djj004. [DOI] [PubMed] [Google Scholar]


