Abstract
Red blood cell alloimmunization remains a major complication for transfusion-dependent patients, but immune factors governing risk for alloimmunization are unknown. We hypothesized that CD4+ regulatory T cells (Tregs), which we have shown control the rate and the frequency of red blood cell alloimmunization in mouse models, may dictate responder/nonresponder status. Using a transfusion regimen in which more than 50% of mice develop alloantibodies to human glycophorin A antigen, we found reduced in vitro and in vivo Treg-suppressive activity in responders compared with nonresponders that was the result of impaired Treg suppressor function. Moreover, responders were prone to developing additional alloantibodies to strong immunogens, whereas nonresponders were resistant to alloimmunization. Altogether, our data raise the possibility that Treg activity may be used as a marker for identifying responder/nonresponder status in transfusion recipients.
Introduction
Exposure to red blood cell (RBC) alloantigens through transfusion, pregnancy, or transplantation may result in production of antibodies in the recipient. Alloimmunization may cause several complications, including delay in obtaining matched blood as well as potentially life-threatening delayed hemolytic transfusion reactions, and autoimmunization.1–4 RBC alloimmunization rates are reportedly as low as 0.5% in transfusion recipients but are highest in chronically transfused patients with hemoglobinopathies.5,6 Even nonchronically transfused patients who become alloimmunized are 20 times more likely to form additional antibodies after one or more repeat transfusion events.7
Several factors are predicted to influence the recipient's immune system to react to alloantigens, including the dose and the immunogenicity of the antigen as well as genetic or acquired patient-related factors.8–11 However, possible differences in the immune makeup of transfused patients who make alloantibodies (responders) and those who do not (nonresponders) are not known. By identifying such markers, it may be possible to predict in advance responders and nonresponders, thereby avoiding the use of costly antigen-matched units for nonresponders, and only selecting phenotyped-matched units1,12–15 for responders to reduce alloimmunization-associated morbidity and mortality. CD4+ regulatory T cells (Tregs) characterized by coexpression of Foxp3 and CD25 are key regulators of a wide spectrum of immune responses,16 suppressing activation and proliferation of effector T cells and other immune cells in vivo and/or in vitro.17 We recently found that manipulation of Treg numbers affects the rate and frequency of RBC alloimmunization in mouse models of RBC transfusions.18 Given that Tregs participate in the control of transfusion-associated RBC alloantibody responses,18 we hypothesized that Treg status may differ between responders and nonresponders. In this study, we used a mouse RBC alloimmunization model to test this hypothesis.
Methods
Mouse studies
Male or female 12-week-old C57/BL6 mice were transfused intravenously with 50 μL Ficoll-treated packed RBCs from transgenic human glycophorin A (huGPA)19 or Duffy Fyb mice,20 equivalent to 1 to 2 packed RBC units with 50 μg unmethylated CpG-containing oligonucleotides (CpG-ODN)18,21 for the first week and then on a weekly basis for 2 to 3 additional weeks with RBCs alone. Alloantibody levels in blood samples obtained by retro-orbital sinus bleeding were measured by incubating diluted plasma with GPA transgenic RBCs and analysis by flow cytometry.18 RBC survival studies were performed as previously described.22 Foxp3 expression in splenocytes was measured by intracellular staining with anti-Foxp3 following the manufacturer's instructions (eBioscience, San Diego, CA) and analysis by flow cytometry.
For adoptive transfer experiments, 106 purified sorted splenic CD4+CD25+ cells (> 95% purity; data not shown) were injected in the tail vein, followed by the aforementioned transfusion regimen a day later.18 All animal procedures were performed as approved by the Institutional Animal Care and Use Committee of the New York Blood Center.
Proliferation assay
CD4+CD25− and CD4+CD25+ T cells (5 × 104 cells/well) were cultured in duplicates or triplicates alone or together at various ratios in the presence of anti-CD3 (clone, 1 μg/mL; BD Biosciences, San Jose, CA) together with 5 × 104/well of irradiated splenocytes from responder mice as antigen-presenting cells for 72 hours. The cultures were pulsed with 1 μCi [3H]thymidine for the last 16 hours.
Statistical analysis
The significance of differences between groups of mice was calculated using the Student t test. Relationship between levels of alloanti-huGPA and alloanti-Fyb was determined by the Pearson r correlation.
Results and discussion
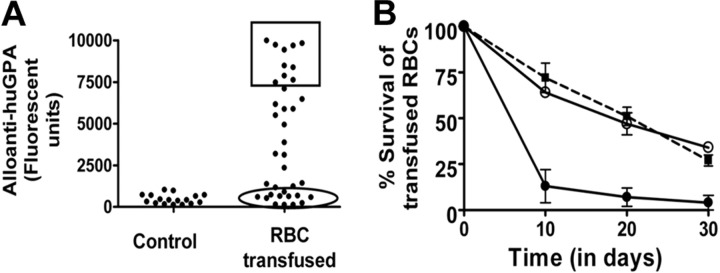
Using a weekly transfusion regimen with allogeneic huGPA RBCs in which the administration of CpG-ODN adjuvant is confined to the first week, more than 50% of B6 mice developed alloantibodies after 4 weeks (Figure 1A, 6 separate experiments), indicating minor genetic or environmental variations even within inbred mouse strains. Transfused recipients were grouped as either nonresponders (no alloantibodies with normal transfused allogeneic RBCs survival) or responders (with highest alloanti-huGPA levels plus shortened transfused RBC survival; Figure 1) to explore potential Treg-associated differences between the 2 cohorts. Analysis of Foxp3 expression indicated no differences in the frequency of Tregs between responders and nonresponders (Figure 2A,B).
Figure 1.
Mouse model of RBC alloimmunization. (A) Mice (n = 38, 6 separate experiments) were given intravenous transfusion of buffy-coated/granulocyte-depleted huGPA RBCs (equivalent to 1-2 packed units) with CpG-ODN adjuvant, followed by weekly transfusions of red cells alone for another 3 weeks. The presence of IgG-specific alloanti-huGPA in plasma from mice was then measured using diluted plasma (1 in 4) and huGPA transgenic RBCs followed by analysis using flow cytometry and is expressed in fluorescent units on the y-axis. Some mice (n = 17) did not receive any transfusions (“control”). The square box represents the cohort with the highest levels of alloantibodies, whereas the oval box includes the group with background control levels of alloanti-huGPA. (B) Red cell survival studies were performed using approximately 50 μL of PKH-26-labeled huGPA red cells transfused into mice with the highest levels of alloanti-huGPA (square box in panel A and line with ● in panel B, n = 5) and into mice with background levels of alloanti-huGPA (oval in panel A and line with ○ in panel B, n = 5). Control B6 mice were transfused with labeled wild-type red cells to show normal red cell survival (…, n = 3). Percentage survival of transfused cells is shown on the y-axis, and time in days is shown on the x-axis. Error bars represent SEM. Recipients with highest levels of alloanti-huGPA in addition to shortened transfused allogeneic RBC survival were designated “responders,” and those with background alloantibody levels plus normal RBC survival were called “nonresponders.”
Figure 2.
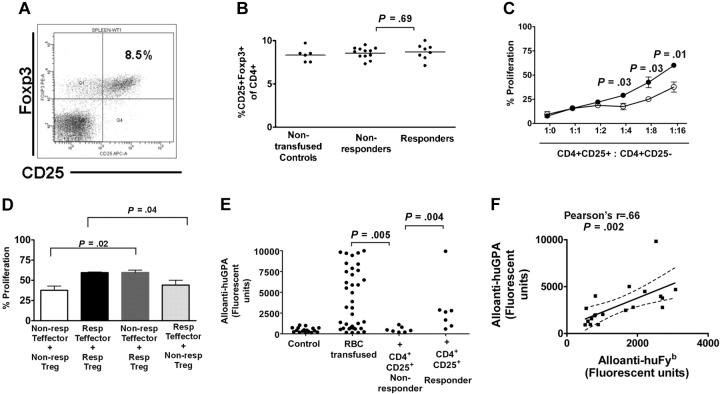
In vitro and in vivo Treg-suppressive activity of responders versus nonresponders. (A) Representative dot plot of CD25 and Foxp3 reactivity of gated CD4+ T-cell population in mouse splenocytes. Isotype control for anti-Foxp3 antibody was used to set the gates for calculating the percentage of the Foxp3+CD25+ cells within the CD4+ subset. (B) The percentages of Foxp3+CD25+ cells in splenocytes of nontransfused (“Nontransfused controls”) as well as nonresponder and responder mice as calculated by the gating strategy shown in panel A. (C) Sorted splenic suppressor Treg (CD4+CD25+) and T effector (CD4+CD25−) cells were stimulated with accessory cells from responders and anti-CD3 antibodies alone or cocultured at various suppressor/T effector ratios (CD4+CD25+/CD4+CD25− of 1:1, 1:2, 1:4, 1:8, and 1:16). Proliferation was measured by incorporation of [3H]thymidine. The mean percentage proliferative responses of stimulated CD4+CD25− cells by autologous CD4+CD25+ cells from responders (●) and nonresponders (○) was calculated as (cpm incorporated in the coculture)/cpm of effector T cells alone) × 100%. Proliferative responses of T effectors were thus normalized to 100%. Addition of CD4+CD25+ cells at 1:1 ratios to CD4+CD25− T effector cells inhibited proliferative responses, and decreasing the number of CD4+CD25+ cells resulted in more proliferation (less suppression). For comparison, percentage proliferation of CD4+CD25+ when stimulated alone (1:0) is also shown. Error bars represent SEM. The P values show the statistically significant differences in suppression of proliferation between responders and nonresponders at the indicated suppressor/effector ratios. In Figure S1 (available on the Blood website; see the Supplemental Materials link at the top of the online article), the comparative proliferation of mice treated with CpG-ODN alone for 1 week is shown. (D) CD4+CD25− nonresponder T effector cells were cocultured with CD4+CD25+ Tregs from responders ( ) and CD4+CD25− responder T effector cells were cocultured with CD4+CD25+ Tregs from nonresponders (
) and CD4+CD25− responder T effector cells were cocultured with CD4+CD25+ Tregs from nonresponders ( ), and mean percentage proliferation was calculated for the 1:16 suppressor/effector T-cell ratio. For comparison, the mean percentage autologous proliferative responses of nonresponders (□) and responders (■) from panel C are shown. The indicated P values reflect the difference between the proliferation of nonresponder CD4+CD25− using CD4+CD25+ from responders and nonresponders as well as differences between the proliferation of responder CD4+CD25− using CD4+CD25+ from responders and nonresponders. Tregs from nonresponders were equally effective in suppressing T effector cells from responders and nonresponders (P = .5; not indicated in the figure). Similarly, responder Tregs suppressed T effector cells from responders and nonresponders to the same degree (P = .9; not indicated in the figure). (E) Groups of mice were adoptively transferred with CD4+CD25+ from splenocytes of nonresponder (“+ CD4+CD25+ Non-responder”) and responder (“+ CD4+CD25+ Responder”) syngeneic mice. After 24 hours, the mice were given intravenous transfusions of buffy-coated/granulocyte-depleted huGPA red cells (equivalent to 1-2 packed units) with CpG-ODN adjuvant followed by weekly transfusions of red cells alone for another 3 weeks. After that, levels of alloantibodies (IgG) in the plasma were measured using diluted plasma (1 in 4) followed by analysis using flow cytometry and are expressed in fluorescent units on the y-axis. Levels of alloanti-huGPA in untransfused (“control”) and nonadoptively transferred transfused mice (“RBC transfused”) from Figure 1A is also shown. The P values indicate the difference in alloantibody levels in nonadoptively transferred transfused mice (“RBC transfused”) and mice adoptively transferred with nonresponder Tregs (P = .005) as well as the difference in alloantibody levels in mice adoptively transferred with Tregs from nonresponders (“+ CD4+CD25+ Non-responder”) versus responders (“+ CD4+CD25+ Responder”; P = .004). In Figure S2, alloanti-huGPA levels after adoptive transfer of control, nonsuppressive CD4+CD25− sorted cells from responders and nonresponders are shown. (F) Mice were given intravenous transfusion of buffy-coated/granulocyte-depleted red cells from human Duffy Fyb (huFyb) transgenic mice (equivalent to 1-2 packed units) with CpG-ODN adjuvant followed by weekly transfusions of red cells alone for another 2 weeks. The mice were then given a single transfusion of huGPA RBCs (no CpG). The presence of IgG-specific alloanti-GPA and allo-Fyb in plasma from mice was then measured using diluted plasma (1 in 4) and huGPA or huFyb transgenic red cells, followed by analysis using flow cytometry, and is expressed in fluorescent units on the y-axis and x-axis, respectively. The correlative relationship between the 2 sets of values is indicated by Pearson r and P values. The upper and lower 95% confidence interval bands of the regression line (—) are shown by the dotted lines.
), and mean percentage proliferation was calculated for the 1:16 suppressor/effector T-cell ratio. For comparison, the mean percentage autologous proliferative responses of nonresponders (□) and responders (■) from panel C are shown. The indicated P values reflect the difference between the proliferation of nonresponder CD4+CD25− using CD4+CD25+ from responders and nonresponders as well as differences between the proliferation of responder CD4+CD25− using CD4+CD25+ from responders and nonresponders. Tregs from nonresponders were equally effective in suppressing T effector cells from responders and nonresponders (P = .5; not indicated in the figure). Similarly, responder Tregs suppressed T effector cells from responders and nonresponders to the same degree (P = .9; not indicated in the figure). (E) Groups of mice were adoptively transferred with CD4+CD25+ from splenocytes of nonresponder (“+ CD4+CD25+ Non-responder”) and responder (“+ CD4+CD25+ Responder”) syngeneic mice. After 24 hours, the mice were given intravenous transfusions of buffy-coated/granulocyte-depleted huGPA red cells (equivalent to 1-2 packed units) with CpG-ODN adjuvant followed by weekly transfusions of red cells alone for another 3 weeks. After that, levels of alloantibodies (IgG) in the plasma were measured using diluted plasma (1 in 4) followed by analysis using flow cytometry and are expressed in fluorescent units on the y-axis. Levels of alloanti-huGPA in untransfused (“control”) and nonadoptively transferred transfused mice (“RBC transfused”) from Figure 1A is also shown. The P values indicate the difference in alloantibody levels in nonadoptively transferred transfused mice (“RBC transfused”) and mice adoptively transferred with nonresponder Tregs (P = .005) as well as the difference in alloantibody levels in mice adoptively transferred with Tregs from nonresponders (“+ CD4+CD25+ Non-responder”) versus responders (“+ CD4+CD25+ Responder”; P = .004). In Figure S2, alloanti-huGPA levels after adoptive transfer of control, nonsuppressive CD4+CD25− sorted cells from responders and nonresponders are shown. (F) Mice were given intravenous transfusion of buffy-coated/granulocyte-depleted red cells from human Duffy Fyb (huFyb) transgenic mice (equivalent to 1-2 packed units) with CpG-ODN adjuvant followed by weekly transfusions of red cells alone for another 2 weeks. The mice were then given a single transfusion of huGPA RBCs (no CpG). The presence of IgG-specific alloanti-GPA and allo-Fyb in plasma from mice was then measured using diluted plasma (1 in 4) and huGPA or huFyb transgenic red cells, followed by analysis using flow cytometry, and is expressed in fluorescent units on the y-axis and x-axis, respectively. The correlative relationship between the 2 sets of values is indicated by Pearson r and P values. The upper and lower 95% confidence interval bands of the regression line (—) are shown by the dotted lines.
In vitro suppression of T-cell receptor–stimulated proliferation of other T cells is a commonly used assay for assessing Treg suppressive function.23,24 We examined the immunosuppressive effects of responder and nonresponder Tregs on proliferation of autologous effector CD4+CD25− cells (n = 3, involving 2-4 mice per group). Sorted Tregs from both groups were equally hyporesponsive to polyclonal stimulation with anti-CD3 and antigen-presenting cells (3H incorporation for responders 833 ± 27 cpm and nonresponders 748 ± 65 cpm; P > .3), indicating that Tregs from both cohorts of mice do exhibit the characteristic anergic Treg phenotype. In contrast, sorted CD4+CD25− cells from both responders and nonresponders proliferated (3H incorporation for responders, 14 381 ± 4105 cpm; nonresponders, 10 660 ± 2200 cpm; P > .4). On coculture of autologous CD4+CD25+ and CD4+CD25− cells at different ratios, Tregs from nonresponders and responders suppressed proliferation of effector T cells at 1:1 and 1:2 ratios in a dose-dependent manner (Figure 2C). However, Tregs from nonresponders were better suppressors as indicated by lower proliferation rates at low Treg to CD4+CD25− ratios (at 1:4 ratio, 18% vs 29%; at 1:8 ratio, 25% vs 43%; and at 1:16 ratio, 38% vs 60%, all P < .05, Figure 2C).
The reduced regulatory function in responders could be the result of a decrease in their Treg function or to refractoriness of their CD4+CD25− cells to suppression. Cross-mixing experiments were performed in which responder and nonresponder Tregs were cocultured with the autologous and the converse CD4+CD25− cells from either nonresponders or responders. At 1:16 CD4+CD25+/CD4+CD25− ratios, responder Tregs could not effectively inhibit proliferation of nonresponder or responder CD4+CD25− cells (Figure 2D), indicating an inherent impaired suppressor function in responder Tregs. In contrast, Tregs from nonresponders suppressed the proliferation of CD4+CD25− cells from both responders and nonresponders to a similar degree (Figure 2D), indicating normal responsiveness of responder effector cells to suppression. We next examined whether the demonstrated differential in vitro Treg activity affected alloimmunization rates in vivo. Naive B6 mice were adoptively transferred with sorted splenic Tregs from responders and nonresponders before initiation of the transfusion regimen with huGPA RBCs. We found that, although adoptive transfer of responders and nonresponder Tregs suppressed the levels of alloantibodies in transfusion recipients, suppression was more effective in mice treated with Tregs from nonresponders (Figure 2E, P = .004), consistent with the in vitro data.
We also tested whether responders with less suppressive Treg activity are more susceptible to developing additional alloantibodies if challenged, and conversely, whether nonresponders with better Treg suppressors are resistant to development of additional alloantibodies. We used RBCs from transgenic mice expressing human Duffy Fyb antigen.20 We found that mice mounted a weaker alloanti-Fyb response compared with alloanti-huGPA responses using our standard transfusion regimen (data not shown), indicating that huFyb is less immunogenic than huGPA. When mice were transfused with huGPA RBCs followed by huFyb RBCs, 17 of 29 mice produced alloanti-huGPA, but none of the mice developed detectable alloanti-Fyb. In the reverse transfusion experiment using huFyb RBCs first and then huGPA RBCs, the levels of alloanti-huGPA production correlated with those of alloanti-Fyb (Figure 2F, Pearson r = 0.66 and P = .002). These data suggest that, despite a reduced Treg activity in responder mice, the immunogenicity of the second alloantigen is an important factor in eliciting an immune response.25 Nevertheless, nonresponders with the demonstrated potent Treg suppressor function are resistant to making subsequent alloantibodies, whereas responders are more susceptible, raising the possibility that Treg activity may be used as a marker for evaluating responder/nonresponder status in transfusion recipients.
Acknowledgments
The authors thank Dr Petra Hoffmann (University Hospital Regensburg, Regensburg, Germany) for helpful discussions.
Footnotes
The online version of this article contains a data supplement.
The publication costs of this article were defrayed in part by page charge payment. Therefore, and solely to indicate this fact, this article is hereby marked “advertisement” in accordance with 18 USC section 1734.
Authorship
Contribution: W.B., S.H., and J.Y. designed and performed research and analyzed data; and K.Y. designed research, analyzed data, and wrote the paper.
Conflict-of-interest disclosure: The authors declare no competing financial interests.
Correspondence: Karina Yazdanbakhsh, Laboratory of Complement Biology, New York Blood Center, 310 E 67th St, New York, NY 10021; e-mail: kyazdanbakhsh@nybloodcenter.org.
References
- 1.Singer ST, Wu V, Mignacca R, Kuypers FA, Morel P, Vichinsky EP. Alloimmunization and erythrocyte autoimmunization in transfusion-dependent thalassemia patients of predominantly Asian descent. Blood. 2000;96:3369–3373. [PubMed] [Google Scholar]
- 2.Zumberg MS, Procter JL, Lottenberg R, Kitchens CS, Klein HG. Autoantibody formation in the alloimmunized red blood cell recipient: clinical and laboratory implications. Arch Intern Med. 2001;161:285–290. doi: 10.1001/archinte.161.2.285. [DOI] [PubMed] [Google Scholar]
- 3.Ameen R, Al Shemmari S, Al Humood S, Chowdhury RI, Al Eyaadi O, Al Bashir A. RBC alloimmunization and autoimmunization among transfusion-dependent Arab thalassemia patients. Transfusion. 2003;43:1604–1610. doi: 10.1046/j.1537-2995.2003.00549.x. [DOI] [PubMed] [Google Scholar]
- 4.Aygun B, Padmanabhan S, Paley C, Chandrasekaran V. Clinical significance of RBC alloantibodies and autoantibodies in sickle cell patients who received transfusions. Transfusion. 2002;42:37–43. doi: 10.1046/j.1537-2995.2002.00007.x. [DOI] [PubMed] [Google Scholar]
- 5.Seyfried H, Walewska I. Analysis of immune response to red blood cell antigens in multitransfused patients with different diseases. Mater Med Pol. 1990;22:21–25. [PubMed] [Google Scholar]
- 6.Hewitt PE, Macintyre EA, Devenish A, Bowcock SJ, Contreras M. A prospective study of the incidence of delayed haemolytic transfusion reactions following peri-operative blood transfusion. Br J Haematol. 1988;69:541–544. doi: 10.1111/j.1365-2141.1988.tb02412.x. [DOI] [PubMed] [Google Scholar]
- 7.Schonewille H, Van de Watering LM, Brand A. Additional red blood cell alloantibodies after blood transfusions in a nonhematologic alloimmunized patient cohort: is it time to take precautionary measures? Transfusion. 2006;46:630–635. doi: 10.1111/j.1537-2995.2006.00764.x. [DOI] [PubMed] [Google Scholar]
- 8.Issitt PD, Anstee DJ. 4th Ed. Durham, NC: Montgomery Scientific; 1998. Applied Blood Group Serology. [Google Scholar]
- 9.Bauer MP, Wiersum-Osselton J, Schipperus M, Vandenbroucke JP, Briet E. Clinical predictors of alloimmunization after red blood cell transfusion. Transfusion. 2007;47:2066–2071. doi: 10.1111/j.1537-2995.2007.01433.x. [DOI] [PubMed] [Google Scholar]
- 10.Zimring JC, Hendrickson JE. The role of inflammation in alloimmunization to antigens on transfused red blood cells. Curr Opin Hematol. 2008;15:631–635. doi: 10.1097/MOH.0b013e328313695e. [DOI] [PubMed] [Google Scholar]
- 11.Higgins JM, Sloan SR. Stochastic modeling of human RBC alloimmunization: evidence for a distinct population of immunologic responders. Blood. 2008;112:2546–2553. doi: 10.1182/blood-2008-03-146415. [DOI] [PubMed] [Google Scholar]
- 12.Lau FY, Wong R, Chan NP, et al. Provision of phenotype-matched blood units: no need for pre-transfusion antibody screening. Haematologica. 2001;86:742–748. [PubMed] [Google Scholar]
- 13.Ness PM. To match or not to match: the question for chronically transfused patients with sickle cell anemia. Transfusion. 1994;34:558–560. doi: 10.1046/j.1537-2995.1994.34794330007.x. [DOI] [PubMed] [Google Scholar]
- 14.Vichinsky EP, Luban NL, Wright E, et al. Prospective RBC phenotype matching in a stroke-prevention trial in sickle cell anemia: a multicenter transfusion trial. Transfusion. 2001;41:1086–1092. doi: 10.1046/j.1537-2995.2001.41091086.x. [DOI] [PubMed] [Google Scholar]
- 15.Castro O, Sandler SG, Houston-Yu P, Rana S. Predicting the effect of transfusing only phenotype-matched RBCs to patients with sickle cell disease: theoretical and practical implications. Transfusion. 2002;42:684–690. doi: 10.1046/j.1537-2995.2002.00126.x. [DOI] [PubMed] [Google Scholar]
- 16.Sakaguchi S. Naturally arising CD4+ regulatory t cells for immunologic self-tolerance and negative control of immune responses. Ann Rev Immunol. 2004;22:531–562. doi: 10.1146/annurev.immunol.21.120601.141122. [DOI] [PubMed] [Google Scholar]
- 17.von Boehmer H. Mechanisms of suppression by suppressor T cells. Nat Immunol. 2005;6:338–344. doi: 10.1038/ni1180. [DOI] [PubMed] [Google Scholar]
- 18.Yu J, Heck S, Yazdanbakhsh K. Prevention of red cell alloimmunization by CD25 regulatory T cells in mouse models. Am J Hematol. 2007;82:691–696. doi: 10.1002/ajh.20959. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Auffray I, Marfatia S, De Jong K, et al. Glycophorin A dimerization and band 3 interaction during erythroid membrane biogenesis: in vivo studies in human glycophorin A transgenic mice. Blood. 2001;97:2872–2878. doi: 10.1182/blood.v97.9.2872. [DOI] [PubMed] [Google Scholar]
- 20.Chaudhuri A, Yuen G, Fang F, Storry J. Development of Duffy transgenic mouse: in vivo expression of human Duffy gene with −33T→C promoter mutation in non-erythroid tissues. Br J Haematol. 2004;127:356–359. doi: 10.1111/j.1365-2141.2004.05208.x. [DOI] [PubMed] [Google Scholar]
- 21.Krieg AM. CpG motifs in bacterial DNA and their immune effects. Ann Rev Immunol. 2002;20:709–760. doi: 10.1146/annurev.immunol.20.100301.064842. [DOI] [PubMed] [Google Scholar]
- 22.Mqadmi A, Zheng X, Yazdanbakhsh K. CD4+CD25+ regulatory T cells control induction of autoimmune hemolytic anemia. Blood. 2005;105:3746–3748. doi: 10.1182/blood-2004-12-4692. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Sakaguchi S, Powrie F. Emerging challenges in regulatory T cell function and biology. Science. 2007;317:627–629. doi: 10.1126/science.1142331. [DOI] [PubMed] [Google Scholar]
- 24.Thornton AM, Shevach EM. CD4+CD25+ immunoregulatory T cells suppress polyclonal T cell activation in vitro by inhibiting interleukin 2 production. J Exp Med. 1998;188:287–296. doi: 10.1084/jem.188.2.287. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Schonewille H, Brand A. Does an alloimmune response to strong immunogenic red blood cell antigens enhance a response to weaker antigens? Transfusion. 2008;48:958–963. doi: 10.1111/j.1537-2995.2008.01659.x. [DOI] [PubMed] [Google Scholar]