Abstract
The Digenea (Platyhelminthes: Trematoda) are a diverse and complex group of internal metazoan parasites. These parasites can serve as hosts to obligate intracellular bacteria belonging to the genus Neorickettsia (Family: Anaplasmataceae). Neorickettsiae persist within all stages of the fluke life cycle and thus are maintained through vertical transmission. However, the low prevalence of Neorickettsia in nature limits study of their transmission biology at different steps of digenean life cycles. To resolve this dilemma, we have developed for the first time a laboratory model allowing to maintain Neorickettsia sp. through the whole life cycle of a digenean, Plagiorchis elegans. The laboratory life cycle of P. elegans consists of a snail first intermediate host, Lymnaea stagnalis, an aquatic arthropod second intermediate host, Culex pipiens (mosquito larva), and a vertebrate definitive host, Mesocricetus auratus (Syrian hamster). This paper focuses on the development of the laboratory life cycle, as well as outlines its potential uses in studying the transmission biology of Neorickettsia and its evolutionary relationship within its digenean host.
Keywords: Digenean, Life cycle, Neorickettsia, Plagiorchis elegans
1. Introduction
The Digenea (Platyhelminthes: Trematoda) are the largest group of parasitic flatworms with roughly 18,000 nominal species (Cribb et al, 2001). They have complex life cycles, using mollusks (primarily gastropods) as first intermediate hosts, several phyla of animals (such as mollusks, arthropods or vertebrates) as second intermediate hosts and all major vertebrate groups as definitive hosts. Due to their highly complex life cycles, cultivation of digeneans in the laboratory also requires cultivation of gastropods and other appropriate host species, and thus is more labor-intensive than that of more typical model organisms. Nevertheless, laboratory cultivation of digeneans allows for major contributions in immunological studies and vaccine development against digenean infection, diagnostics and taxonomic studies, and biochemical or physiological studies (Smyth and Halton, 1984; Ndiaye et al., 2012; Greani et al. 2014; Mwangi et al., 2014).
Since the 1950s, it has been known that some digeneans harbor intracellular bacteria. These endosymbiotic alpha-proteobacteria belong to the genus Neorickettsia (Order Rickettsiales, family Anaplasmataceae) and are transmitted vertically from one digenean life cycle stage to the next throughout the life cycle (Vaughan et al., 2012). In some cases, Neorickettsia bacteria can also be transmitted horizontally from the digenean to the vertebrate definitive host. When this happens, the bacteria may infect vertebrate leucocytes and cause disease. In the USA, Philip et al. (1953, 1955) discovered that a lethal disease of dogs, known locally as ‘salmon dog poisoning’ because of its association with salmon spawning along the Pacific Northwest, was actually caused by the bacterial endosymbionts of an intestinal digenean species, Nanophyetus salmincola. This digenean species uses salmonid fish as its second intermediate host and piscivorous mammals (e.g., raccoons, bears, dogs, etc.) as definitive hosts. Philip (1955) erected a new genus and species, Neorickettsia helminthoeca, to accommodate the digenean-borne bacteria responsible for salmon dog poisoning. At least 3 other species of Neorickettsia have since been described that can cause vertebrate disease (i.e., N. risticii, N. elokominica, N. sennetsu). Recently, an increasing number of other, genetically distinct species level lineages of Neorickettisia of uncertain pathogenicity have been discovered (Tkach et al., 2012; Greiman et al., 2014). The most geographically widespread species of Neorickettsia is N. risticii, which can infect horses (=Potomac horse fever) causing septicemia, severe diarrhea, foundering, even death. Neorickettsia risticii is also the most widespread in terms of the taxonomic diversity of digeneans in which it has been found, including members of several digenean families such as lecithodendriids Acanthatrium sp., Lecithodendrium sp., dicrocoeliid Conspicuum icteridorum, echinostomatid Echinoparyphium rubrum, heronimid Heronimus mollis, and macroderoidid Alloglossidium corti (Pusterla et al., 2003; Gibson et al., 2005; Gibson and Rikihisa, 2008, Tkach et al., 2012).
In 2012, we detected neorickettisal DNA in field isolates of Plagiorchis elegans, a plagiorchiid digenean that is commonly found in local pond snails (Lymnaeidae) in North Dakota. Originally reported to be N. risticii (Greiman et al., 2013) and doubtless very closely related, the neorickettsial strain within P. elegans has since been characterized as genetically divergent from N. risticii based on Bayesian phylogenetic analysis of a 1400 bp fragment of the 16s rRNA gene (Greiman et al., 2014). Plagiorchis elegans is a generalist parasite, capable of utilizing multiple groups of aquatic arthropods as second intermediate hosts (e.g., Chironomus sp., Gammarus pulex, Asellus aquaticus, Culex spp.) (Gorman, 1980) and a wide range of wild vertebrates as definitive hosts. Importantly, it can also use as definitive hosts several species of animals such as LACA mice, rats, hamsters, gerbils, chicks, ducklings and pigeons (Gorman, 1980). This makes P. elegans a prime candidate for establishing a laboratory life cycle.
Currently, the majority of research on Neorickettsia has focused on the molecular biology, immunology, diagnostics and treatment of neorickettsiae and neorickettsial diseases, while fundamental aspects of the transmission biology of Neorickettsia within the digenean host have been little studied (Vaughan et al., 2012). Establishing laboratory life cycles of digeneans infected with Neorickettsia provides a controlled environment in which to study the transmission biology of Neorickettsia, something that is difficult to do in the field. We describe here for the first time the in vivo culture and maintenance of Neorickettsia throughout all stages of a digenean life cycle in the laboratory.
2. Materials and Methods
2.1 Ethics statement
The use of vertebrate animals was approved by the University of North Dakota Institutional Animal Care and Use Committee (protocol 1011-1c).
2.2 Snail Collection
Aquatic snails, Lymnaea stagnalis, were collected during the summer of 2011 from a pond in Nelson County, North Dakota (Lat: 48° 1′43.80″N and Long: 97°59′24.88″W). Snails were rinsed with water and placed into glass jars filled with aged tap water conditioned with commercial aquarium conditioner to remove chlorine/chloramines. To promote cercarial shedding, snails were kept for several hours under fluorescent lamps followed by several hours without light. Afterwards, the water in jars was examined at low magnification (5 to 20x) with transillumination for the presence of xiphidiocercariae. Snails shedding xiphidiocercariae were given a small section of fresh leaf lettuce and maintained singly in labeled jars until the xiphidiocercariae were assayed for the presence of Neorickettsia. Snails not shedding cercariae were placed together in large trays with 3–4 inches of treated water and maintained for breeding stock.
2.3 DNA extraction
Initial screening for snails shedding Neorickettsia positive P. elegans cercariae was done using homogenates from pooled cercariae. Approximately 20–30 cercariae from each shedding snail were pipetted into a 1.75 ml microcentrifuge tube and centrifuged at 13,000 rpm for five minutes. Supernatant was removed and 75 µl of ultrapure water added. Cercariae were homogenized by direct sonication using a UP100H compact ultrasonic processor (Hielscher USA, Inc., Ringwood, NJ) at an amplitude of 80–90% for fifteen seconds, and immediately placed on ice. A subsample (5 µl) of each homogenates was used directly as template for real-time PCR amplification procedures. The remainder of each homogenate was extracted for DNA using the guanidine thiocyanate method as described by Tkach and Pawlowski (1999).
2.4 Molecular detection and identification
Homogenates were first tested for the presence of Neorickettsia using a real-time PCR protocol designed by Greiman et al. (2014). Five microliters of each homogenate were used. The real-time PCR amplified a 152-bp portion of the 3′ end of the heat shock protein coding gene, GroEL. The primer pair used was: groel-1500F (5′- ATAGATCCAGCKAAGGTAGTGCGTGT-3′) and groel-1620R (5′- TTCCACCCATGCCACCACCAGGCATCATTG-3′). The real-time PCR reactions were run on a Bio-Rad CFX96 Touch Real-Time PCR detection system (Bio-Rad Laboratories, Hercules, CA) using iTaq universal SYBR Green supermix (Bio-Rad Laboratories, Hercules, CA) according to the manufacturer's instructions. A two-step program was used with a denaturation temperature of 95°C for 3 seconds, a annealing and extension temp of 64°C for 25 seconds and 36 cycles. A melting curve was run starting from 72°C and moving at 0.2°C increments every 5 seconds until reaching 95°C.
Samples shown to be Neorickettsia-positive by real-time PCR, were verified using a substantially modified nested PCR protocol initially described by Barlough et al. (1997). Five microliters of each complete DNA extract were used for the first PCR reaction and 1 µl of the first PCR product was used for the nested PCR. The nested PCR amplified a 527-bp portion of the 5′ end of the 16s rRNA gene. The primer pairs (designed by SEG) used in the first round were: n16s-25F (5′-TCAGAACGAACGCTAGCGGT-3′) and n16s-610R (5′-GACGTTCCTCTTGATATCTACG-3′). Primers used in the nested round were: n16s-70F (5′-GAATCAGGGCTGCTTGCA-3′) and ER2-R (5′- GTTTTAAATGCAGTTCTTGG-3′). The nested PCR reactions were run on a Mastercycler EP Gradient thermocycler (Eppendorf, Hauppauge, NY) using OneTaq Quick Load 2X Master Mix with GC Buffer (New England Biolabs, Ipswich, MA) according to the manufacturer's instructions. Annealing temperature of 54°C and 40 cycles were used in both first and nested PCRs. DNA of N. risticii used as a positive control was graciously provided by Dr. John Madigan (University of California Davis).
Cercariae were identified using partial sequences of the nuclear large ribosomal subunit gene (28S). Digenean DNA, from the completed DNA extracts of cercarial homogenates, was amplified by PCR using forward primer digl2 (5-AAGCATATCACTAAGCGG-3′) and reverse primer 1500R (5-GCTATCCTGAGGGAAACTTCG-3′).
PCR amplicons of both Neorickettsia and digeneans were purified using ExoSAP-IT PCR clean-up enzymatic kit (Affimetrix, Santa Clara, CA) according to the manufacturers' instructions. The PCR products were cycle-sequenced using ABI BigDye™ (Thermo Fisher Scientific Inc, Grand Island, NY) chemistry, alcohol precipitated and run on an ABI Prism 3100™ (Thermo Fisher Scientific Inc, Grand Island, NY) automated capillary sequencer. For sequencing of Neorickettsia, nested PCR primers were used. For sequencing of cercariae an internal reverse primer ECD2 (5-CTTGGTCCGTGTTTCAAGACGGG-3) was used. Contiguous sequences of Neorickettsia and of cercariae were assembled and edited using Sequencher™ ver. 4.2 (GeneCodes Corp., Ann Arbor, MI) and submitted to GenBank under accession numbers.
2.5 Snail intermediate host cultures
Twenty to thirty uninfected locally collected Lymnaea stagnalis were used to establish a laboratory colony of snail first intermediate hosts. Adult snails were placed in large plastic containers with 6–8 centimeters of aged tap water conditioned with commercial aquarium conditioner to remove chlorine/chloramines. Egg sacs were periodically removed and placed into smaller containers where they hatched. Once hatched, young snails were allowed to develop to approximately 1.5–2 centimeters in length before being used for infection with P. elegans eggs. For general rearing, snails were maintained on leaf lettuce, feces were removed daily, and every several days ca. 1/3 of the water was removed and replaced with fresh water.
2.6 Mosquito intermediate host cultures
Culex pipiens mosquito stocks originated from wild populations captured in Larimer County, Colorado. Larvae were reared in flat polyurethane trays containing ca. 500ml of aged tap water supplied daily with a small amount of commercial fish food (TetraPond®) ground to a fine powder using a coffee grinder. Upon pupation, the pupae were transferred to aluminum screen cages to emerge as adults. One to two weeks after eclosion, female mosquitoes were allowed to blood feed on an anesthetized rodent. Two to three days later, cages were supplied with a container of aged tap water for gravid females to oviposit. Egg rafts were transferred to larval rearing pans to begin the cycle anew.
2.7 Establishment of laboratory lifecycle of P. elegans infected with Neorickettsia sp
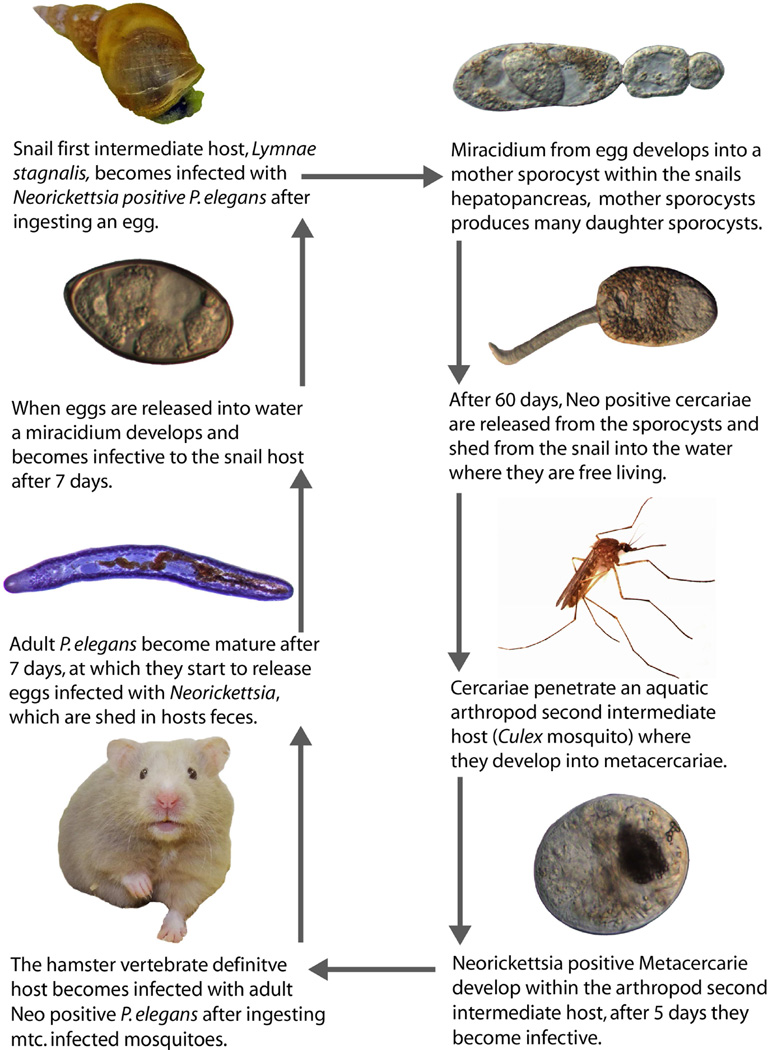
The life cycle of P. elegans harboring Neorickettsia sp. was initially established as follows (Fig 1). Approximately 20–40 Culex larvae (3rd and 4th instar) were exposed for 2 to 3 hours to approximately 500 Neorickettsia sp. positive P. elegans cercariae shed from a naturally infected L. stagnalis snail. Cercariae penetrated and encysted in the Culex larvae forming metacercariae. To ensure that metacercariae had formed within the mosquito host, one to three Culex larvae were squished by a cover slip and examined for metacercariae under a compound microscope.
Figure 1.
Laboratory life cycle of Plagiorchis elegans harboring Neorickettsia sp.
In some cases Plagiorchis elegans metacercariae may become infective to the definitive host after 48 hours (Gorman 1980). To ensure high infectivity of the metacercariae we waited 5 days before feeding metacercariae-infected mosquito larvae to the definitive host, a Syrian hamster, Mesocricetus auratus. Hamsters were anesthetized lightly with isoflurane and force fed with 15–20 Culex larvae. Hamsters were maintained in individual cages on standard rodent diet (Purina LabDiet®) and the bedding was replaced twice a week.
To monitor infection success, wet mounts of hamster feces were periodically examined under a compound microscope for operculate digenean eggs. Eggs were first found within the feces 7 days post-infection (PI) and were still present after 29 days PI. After 11–29 days PI, hamsters were anesthetized with isoflurane and euthanized by cervical dislocation. The small intestines were removed, placed flat in a Petri dish with saline, teased apart with forceps, and examined for adult P. elegans under a stereo-microscope.
Adult worms were removed with a glass pipette and placed in Petri dishes containing sterile saline. From each dish, ten adult worms were selected and placed individually in separate Petri dishes containing heat-sterilized aquarium water. Individual worms were then teased apart with fine needles to remove mature eggs from the distal portion of the digenean uterus. To determine if each of these “egg donor” digeneans actually harbored Neorickettsia, the remainder of each worm was then homogenized and screened for Neorickettsia sp. using real-time PCR as described above. The eggs were evenly distributed around the dish using a clean glass pipette, and left to incubate for 7 days at room temperature. To minimize microbial growth during the weeklong incubation, approximately a third of the water was carefully removed every day with a clean pipette and replenished with fresh water. It has been shown previously that an incubation period of 7 days is sufficient to allow P. elegans miracidia to develop and become infective to lymnaeid snails (Gorman, 1980). To confirm this, periodically a single egg was placed in water under a cover slip, and visualized under a compound microscope to monitor miracidium development. After 7 days, groups of 10 uninfected snails were placed into each of the Petri dishes containing embryonated eggs and allowed to graze along the bottom for ca. 1 hour. Afterwards, snails were removed, placed in separate labeled containers with aerated water at 20–22°C and maintained as described above. Fifty to 60 days after infection, surviving snails began to release cercariae. Newly shed cercariae were collected and screened for Neorickettsia using real-time PCR as described above. Snails shedding Neorickettsia positive cercariae were placed into containers containing fresh mosquito larvae in order to produce Neorickettsia positive metacercariae and repeat the life cycle.
3. Results
3.1 Life cycle
We have for the first time maintained Neorickettsia in the laboratory throughout the entire life cycle of a digenean. One generation of the laboratory life cycle of P. elegans takes approximately 90 days – i.e., 5 days for metacercariae to become infective, 20 days for adults to develop, 7 days for miracidium to become infective within the egg, and 50–60 days for the snail to start shedding cercariae after ingestion of an infective egg. Neoricekttsia sp. infection was maintained in the digenean, P. elegans, for three complete generations. In our subsequent experiments we established three lines of Neorickettsia originating from three different naturally infected snails.
3.2 Host specificity
We attempted to use both hamsters and outbred mice as definitive hosts for P. elegans. However, only hamsters were found to be suitable hosts producing ovigerous P. elegans (Table 1).
Table 1.
Experimental animals infected with Plagiorchis elegans metacercariae (mtc.) from mosquito larvae. Days post infection (PI) before dissection of experimental animal and number of adult P. elegans in intestine provided.
| Experimental animal |
Days PI before dissection |
Number of adult P. elegans |
|---|---|---|
| Mouse #1 | 11 | 1 (underdeveloped) |
| Mouse #2 | 17 | 0 |
| Mouse #3 | 17 | 0 |
| Mouse #4 | 16 | 0 |
| Mouse #5 | 25 | 0 |
| Mouse #6 | 7 | 0 |
| Mouse #7 | 7 | 7 (underdeveloped) |
| Hamster #1 | 11 | 25 |
| Hamster #2 | 14 | 33 |
| Hamster #3 | 14 | 14 |
| Hamster #4 | 17 | 42 |
| Hamster #5 | 12 | 100 |
| Hamster #6 | 27 | 36 |
| Hamster #7 | 28 | 2 |
| Hamster #8 | 22 | 21 |
| Hamster #9 | 27 | 40 |
| Hamster #10 | 29 | 35 |
4. Discussion
The digenean, Plagiorchis elegans, was used for our laboratory life cycle for two reasons. First, P. elegans is found to be naturally infected with Neorickettsia sp. in North Dakota (Tkach et al., 2012; Greiman et al., 2013). From three ponds in eastern North Dakota, 240 L. stagnalis were found infected with P. elegans and of those, 18 proved to be Neorickettsia-positive (7.5%) (Greiman et al., 2013). Second, P. elegans is a generalist parasite, utilizing multiple groups of aquatic arthropods as second intermediate hosts, as well as, infecting a wide range of vertebrate definitive hosts (Gorman, 1980). In North Dakota, muskrats are the most common natural definitive host of P. elegans. Not surprisingly, hamsters proved to be a highly suitable experimental host for these digeneans because they belong to the same family Cricetidae. Likely, some other vertebrates may be used for this purpose (Gorman, 1980), however, in our experiments mice did not produce adult P. elegans.
There are several potential “choke-points” in the lifecycle that deserve special attention. The first is to avoid exposing mosquito larvae to too many cercariae. Gorman (1980) found that by exposing 6 chironomid larvae to approximately 120 cercariae in the confines of a small Petri dish (5 cm in diameter), the insect larvae became infected with 10 to 30 metacercarial cysts. Larger numbers of cercariae per larvae resulted in death of some chironomid larvae. We exposed 20–30 Culex mosquito larvae to approximately 500 cercariae for 2 to 3 hours. We did not count the average number of metacercariae per insect larvae, however, we did observe larval death when exposed to approximately 1000 or more cercariae. Smaller, younger larvae (i.e., 1st and 2nd instar) were less tolerant of multiple cercarial penetrations and mortality was more frequent than with older 3rd and 4th instar larvae.
The second point of attention is to ensure that heat sterilized water is used for egg development. In non-boiled water, the eggs may be damaged by fungi or ingested by ciliate protozoan. The third important element is to pay close attention to the husbandry of snails after they become infected with digeneans (i.e., after exposure to digenean eggs). It has long been known that larval digeneans, including P. elegans (Zakikhani and Rau, 1999), can deplete energy reserves and increase mortality of their molluskan hosts (Cheng and Snyder, 1962; Pinheiro and Amato, 1994), especially under stress. In our initial experiments the majority of our parasitized snails died from what we now believe to have been excessive water removal and replenishment. To prevent the holding water from becoming anoxic and foul, we initially replenished half of the holding water with fresh water on a daily basis. However, when parasitized snails began to die, we reduced the volume of water removal-replenishment to a third of the holding volume and the survival of parasitized snails improved. In addition, we recommend to use at least 100 snails for infection during each generation, to ensure continuance of the life cycle.
One large gap in our knowledge of Neorickettsia biology that laboratory life cycles can help address is understanding the quantitative aspects of Neorickettsia perpetuation during the complex digenean life cycle (Vaughan et al., 2012). Similar to other types of heritable microorganisms (e.g., Rickettsia, Wolbachia), Neorickettsia must coordinate its replication with the reproduction of its invertebrate host. For digeneans, this includes both sexual and asexual reproduction. Greiman et al. (2013) were able to determine the vertical transmission efficiency of N. risticii within asexual stages (sporocysts and cercariae) of P. elegans in naturally infected snails, but not within sexual stages (adults and eggs), something that is now possible using the laboratory model described herein.
Another important gap in our knowledge of Neorickerttsia transmission biology is the lack of understanding of their horizontal transmission. Although horizontal transmission of neorickettsiae from digenean to vertebrate host occurs and can cause disease, it is not known whether horizontal transmission of neorickettsiae can go in the opposite direction from vertebrates to digeneans. It is also unknown whether neorickettsiae can be transmitted from Neorickettsia-infected digeneans to uninfected digeneans within a parasitized snail or vertebrate (i.e., through co-feeding transmission). Such alternate transmission pathways could play a vital part in both circulation and evolution of Neorickettsia. Availability of a laboratory model will help to elucidate the probability of such events.
The maintenance of Neorickettsia throughout complete life cycles of digeneans in laboratory makes it possible to conduct controlled studies and thereby gain a more thorough understanding of the biology and transmission of these enigmatic bacterial endosymbionts capable of causing disease in humans, domestic animals and wildlife.
Highlights.
Maintenance of Neorickettsia, for the first time, through a laboratory digenean life cycle.
Laboratory life cycle allows for greater study of Neorickettsia transmission biology.
Neorickettsia cause disease in humans, domestic animals, and wildlife.
Acknowledgments
We are grateful to Kayla Steffes, Christopher Bothun, and Spencer Carmichael for their help with snail colony maintenance. This work was supported in part by the grant R15AI092622 from the National Institute of Health, USA.
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
References
- Barlough JE, Rikihisa Y, Madigan JE. Nested polymerase chain reaction for detection of Ehrlichia risticii genomic DNA in infected horses. Vet Parasitol. 1997;68:367–373. doi: 10.1016/s0304-4017(96)01083-7. [DOI] [PubMed] [Google Scholar]
- Cheng TC, Snyder RW. Studies on the host-parasite relationships between larval trematodes and their hosts. I. Review. II. The utilization of the host’s glycogen by the intramolluscan larvae of Glypythelmins pennsylvaniensis Cheng, and associated phenomena. Transactions of the American Microscopical Society. 1962;81:209–228. [Google Scholar]
- Cribb TH, Bray RA, Littlewood DTJ, Pichelin SP, Herniou EA. Interrelationships of the Platyhelminthes. Taylor and Francis London: 2001. Relationships of the Digenea - evidence from molecules and morphology; pp. 168–185. [Google Scholar]
- Gibson KE, Rikihisa Y, Zhang C, Martin C. Neorickettsia risticii is vertically transmitted in the trematode Acanthatrium oregonense and horizontally transmitted to bats. Environmental Microbiology. 2005;7:203–212. doi: 10.1111/j.1462-2920.2004.00683.x. [DOI] [PubMed] [Google Scholar]
- Gibson KE, Rikihisa Y. Molecular link of different stages of the trematode host of Neorickettsia risticii to Acanthatrium oregonense. Environmental Microbiology. 2008;10:2064–2073. doi: 10.1111/j.1462-2920.2008.01625.x. [DOI] [PubMed] [Google Scholar]
- Gorman AM. The University of Leeds Department of Pure and Applied Zoology. 1980. Studies on the biology of Plagiorchis elegans (Rudolphi, 1802), (Trematodas: Digenea) in its mammalian and molluscan hosts. Dissertation. [Google Scholar]
- Greani S, Quilichini Y, Foata J, Greiman SE, Ndiaye PI, Tkach VV, Marchand B. Vitellogenesis of the digenean Plagiorchis elegans (Rudolphi, 1802) (Plagiorchiodea, Plagiorchiidae) Parasitology International. 2014;63:537–543. doi: 10.1016/j.parint.2013.12.010. [DOI] [PubMed] [Google Scholar]
- Greiman SE, Tkach VV, Vaughan JA. Transmission rates of the bacterial endosymbiont, Neorickettsia risticii during the asexual phase of its digenean host, Plagiorchis elegans within naturally infected lymnaeid snails. Parasites and Vectors. 2013;6:303. doi: 10.1186/1756-3305-6-303. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Greiman SE, Tkach VV, Pulis E, Fayton TJ, Curran SS. Large scale screening of Digeneans for Neorickettsia endosymbionts using real-time PCR reveals new Neorickettsia genotypes, host associations and geographic records. PLOS ONE. 2014;9:e98453. doi: 10.1371/journal.pone.0098453. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mwangi IN, Sanchez MC, Gerald MM, Agola LE, Runo SM, Cupit PM, Cunningham C. Praziquantel sensitivity of Kenyan Schistosoma mansoni isolates and the generation of a laboratory strain with reduced susceptibility to the drug. International Journal of Parasitology: Drugs and Drug Resistance. 2014;4:296–300. doi: 10.1016/j.ijpddr.2014.09.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ndiaye PI, Quilichini Y, Tkach VV, Greiman SE, Ba CT, Marchand B. Ultrastructure of the Spermatozoon of the Digenean Plagiorchis elegans (Rudolphi, 1802) (Plagiorchioidea, Plagiorchiidae) Journal of Morphology. 2012;247:965–972. doi: 10.1002/jmor.20152. [DOI] [PubMed] [Google Scholar]
- Philip CB, Hadlow WJ, Hughes LE. Neorickettsia helmintheca, a new rickettsia-like disease agent of dogs in western United States transmitted by a helminth. Communication abstracts VI International Congress of Microbiology. 1953;2:256–257. [Google Scholar]
- Philip CB. There is always something new under the “parasitological sun” (the unique story of helminth-borne salmon poisoning disease) Journal of Parasitology. 1955;41:125–148. [PubMed] [Google Scholar]
- Pinheiro J, Amato SB. Eurytrema coelomaticum (Digenea, Dicrocoeliidae): the effect of infection on carbohydrate contents of its intermediate snail host, Bradybaena similaris (Gastropoda, Xanthocychidae) Memorias do Instituto Oswaldo Cruz. 1994;89:407–410. [Google Scholar]
- Pusterla N, Johnson EM, Chae JS, Madigan JE. Digenetic trematodes, Acanthatrium sp. and Lecithodendrium sp., as vectors of Neorickettsia risticii, the agent of Potomac horse fever. Journal of Helminthology. 2003;77:335–339. doi: 10.1079/joh2003181. [DOI] [PubMed] [Google Scholar]
- Smyth JD, Halton DW. The physiology of trematodes. 2nd. Cambridge, UK: Cambridge University Press; 1984. [Google Scholar]
- Tkach VV, Pawlowski J. A new method of DNA extraction from the ethanol-fixed parasitic worms. Acta Parasitologica. 1999;44:147–148. [Google Scholar]
- Tkach VV, Schroeder JA, Greiman SE, Vaughan JA. New genetic lineages, host associations and circulation pathways of Neorickettsia endosymbionts of digeneans. Acta Parasitologica. 2012;57:285–292. doi: 10.2478/s11686-012-0043-4. [DOI] [PubMed] [Google Scholar]
- Vaughan JA, Tkach VV, Greiman SE. Neorickettsial endosymbionts of the Digenea: diversity, transmission and distribution. Advances in Parasitology. 2012;79:253–297. doi: 10.1016/B978-0-12-398457-9.00003-2. [DOI] [PubMed] [Google Scholar]
- Zakikhani M, Rau ME. Plagiorchis elegans (Digenea: Plagiorchiidae) infections in Stagnicola elodes (Pulmonata: Lymnaeidae): host susceptibility growth, reproduction, mortality and cercarial production. Journal of Parasitology. 1999;85:454–463. [PubMed] [Google Scholar]