Abstract
Background
Anxiety and depression display frequent comorbidity. Individuals with comorbid disorders also often have more extreme symptomatology than those with single disorders. This correlation between comorbidity and severity poses an interesting question: are comorbid forms of anxiety and depression essentially just more severe versions of the pure disorders?
Methods
In a large major depression case-control sample of individuals from the CONVERGE project, we examined the patterns of lifetime anxiety comorbidity (including generalized anxiety disorder – GAD, panic disorder and five phobia subtypes) among major depression (MD) cases (N=5,864) in this population. Binary and multinomial logistic regression was used to estimate associations between risk factors and outcomes including MD as well as latent class membership, which were compared using continuation ratios.
Results
We found a five-class solution to fit best, and each resulting class had a distinct pattern of association with the tested risk factors. The use of continuation ratios suggests that a class characterized by high endorsement of GAD is comparable to a more severely affected ‘pure MD’ group. The other three classes (characterized by agoraphobia, various specific phobias, and by high endorsement of all comorbid anxiety disorders, respectively) appear to differ meaningfully from MD alone.
Conclusions
Risk for MD resulting from environmental and psychosocial factors may also predispose individuals to GAD, and less consistently, other anxiety disorders. Presentations of MD with certain phobias display distinguishably different patterns of risk, however, and are therefore likely qualitatively distinct.
Keywords: Anxiety/Anxiety Disorders, Depressive Disorder, GAD/Generalized Anxiety Disorder, Panic Attacks/Agoraphobia, Phobia/Phobic Disorders
Introduction
One of the most consistent findings in psychiatric research is the frequent comorbidity between anxiety disorders and depressive disorders1–3. While patients with comorbid illnesses meet criteria for a particular anxiety and depressive disorder, the severity of symptoms in comorbid disorders is often worse than in disorders that occur alone. Compared to those with pure major depression (MD) patients with co-morbid generalized anxiety disorder (GAD) have poorer social functioning4; those with comorbid social phobia have increased severity of their depressive symptoms5; and those comorbid panic disorder have a reduced likelihood of their depression remitting6.
There may be a causal relationship between the onset of one disorder and the risk of developing a second (such as when GAD precedes MD7), which has important implications for treatment: successful treatment of the first disorder may reduce risk for the second. Since the onset of MD may occur before or after anxiety disorders8, delineating risk profiles for individuals likely to develop comorbid disorders may aid the provision of optimal treatment.
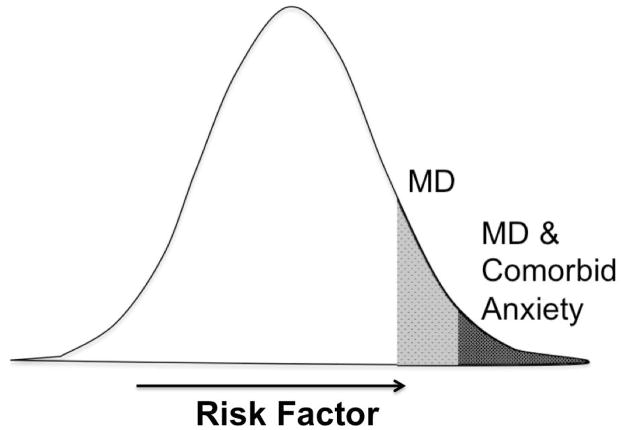
Co-morbidity has many origins. The genetic factors contributing to anxious and depressive symptomatology are shared9, 10. Environmental experiences, such as stressful life events11, 12 also contribute to both. The factors leading to the comorbid state of anxiety and depressive disorders together versus a single disorder are still unclear, but seem multifactorial and variable across individuals. If the majority of contributory factors are shared between anxiety disorders and MD, it’s plausible that those who meet criteria for both MD and an anxiety disorder carry a larger burden of risk (that is, the pool of shared etiological factors contributing to the likelihood of MD and anxiety disorder diagnoses) than those who suffer from only one disorder type. If this is true, the degree to which risk factors contribute to the risk of comorbid MD and anxiety disorder in comparison to MD without anxiety disorder comorbidity can be tested through the use of the continuation ratio13. The continuation ratio assesses the degree to which a risk factor’s association strength differs in predicting multiple levels of severity. For a better framework of understanding, it is useful to consider these levels of severity as lying along a continuous underlying scale; see Figure 1. This might be conceived as a scale of ‘psychological distress’, containing the intervals of MD alone, and MD comorbid with anxiety disorder (as well as perhaps a putative third level below both of these on the scale reflecting non-pathological distress, which is not measured in the current study or displayed in Figure 1). In the continuation ratio, the “risk factor is seen as acting on the entire latent scale and thereby affecting all the categories simultaneously”13. While this proposed underlying scale may not reflect the ultimate reality, it serves as a helpful context for testing the consistency of a risk factor’s effect between outcomes.
Figure 1.
Continuous scale underlying MD and anxiety comorbidity latent class with respect to a risk factor.
There is heterogeneity in the mood and anxiety disorders, both within individual disorders and in how they occur in comorbid presentations. Latent class analysis is a useful method of capturing heterogeneity, assigning individuals to groups based on a few key metrics, such as symptoms. Depression subtypes estimated from latent class analysis show both quantitative and qualitative differences14. Specific combinations of anxiety and mood disorders also display statistically distinguishable patterns: a latent class analysis in the National Comorbidity Survey15 found contrasts between somatic and psychological symptoms and between symptoms of anxiety and depression. The present study aims to characterize trends within the broader context of MD with any anxiety comorbidity – using latent class analysis to distinguish classes based on lifetime comorbidity between a variety of anxiety disorders and recurrent MD.
We set out to apply these approaches to a case-control study of women with recurrent MD, all Han Chinese. We ask how many classes can be distinguished using comorbid diagnoses. Using these classes, we examine whether psychosocial risk factors differ in predicting MD case status and comorbid anxiety disorders. We also ask whether the predictive strength of these risk factors differs meaningfully between the less severe level of MD only and the more severe level of comorbid anxiety disorder latent class membership.
Materials and Methods
The subjects included in this analysis are part of the China, Oxford and VCU Experimental Research on Genetic Epidemiology (CONVERGE) study. Of the 5,935 MD clinically-ascertained cases, and 5,907 controls without MD that come from more than 30 cities, 11,647 individuals with valid data for the chosen predictors and outcomes were used in the present analysis, comprising 5,783 controls, 3,107 MD cases with some type of anxiety disorder comorbidity, and 2,757 MD cases without comorbid anxiety. Anxiety disorders were only assessed in MD cases in this sample; there are no individuals falling into the category of anxiety disorders without major depression and hence the present analyses of anxiety disorders are limited to those comorbid with major depression only.
This article was motivated by earlier work in a large sample of clinically ascertained Han Chinese women designed to study the genetics of MD16. MD has a genetic correlation between men and women of less than unity10 and signal-to-noise ratio in association signals is improved by increased genetic homogeneity (achieved by ensuring all participants had four Han Chinese biological grandparents ). Cases were excluded for bipolar disorder, psychosis and intellectual disability, and controls were screened by personal interview for depressive episode. In addition, cases had a minimum age of 30 to reduce the chance of later manifestation of bipolar disorder, and controls had a minimum age of 40, to minimize the chance of late-onset MD.
Each subject was interviewed with a computerized assessment, and all interviewers were medically trained in addition to 7+ days of training with the CONVERGE group. Interviews included evaluations of personality, demographic characteristics, family history of depression, stressful life events, parental bonding, MD clinical features, diagnostic information on dysthymia, GAD, phobias, psychosis and panic disorder, and more.
The diagnoses of depressive (dysthymia and MD) and anxiety disorders (GAD, panic disorder with or without agoraphobia) were made with a version of the Composite International Diagnostic Interview17, Chinese version) which classifies diagnoses according to the Diagnostic and Statistical Manual of Mental Disorders fourth edition (DSM-IV) criteria, with a modified symptom duration requirement of at least one month for GAD diagnosis, instead of six months. Phobias, divided into five subtypes (animal, situational, social and blood-injury, and agoraphobia), were diagnosed using an adaptation of DSM-IV criterion D18 requiring one or more unreasonable fears that interfered with the respondents’ life or resulted in severe anxiety when exposed to the phobic stimulus. The assessment of phobias was translated by the CONVERGE team from the interview used in the Virginia Adult Twin Study of Psychiatric and Substance Use Disorders (VATSPUD)19. The history of lifetime MD in the parents and siblings was assessed using the Family History Research Diagnostic criteria20. Neuroticism was measured with the 23-item Eysenck Personality Questionnaire21.
The diagnoses of MD were also informed by information collected in the medical records and DSM-IV symptoms during the worst episode. Symptom information collected for the diagnoses of co-morbid disorders of MD was for lifetime comorbidity. Diagnostic information collected from the CIDI17 and phobia assessment detailed above is used to define the diagnoses central to this analysis, including MD and comorbid anxiety diagnoses. 7 lifetime anxiety diagnoses (GAD, Panic Disorder, and five phobias: animal, blood-injury, situational, agoraphobia and social phobia) comorbid with recurrent MD are used as indicator variables to distinguish subtypes in the latent class analysis. 4 characteristics of MD presentation (age of onset, number of major depressive episodes, number of MD symptoms endorsed in most severe episode, and family history of MD ratio) are used as predictors to determine differential relationships between depression severity and latent comorbid anxiety class. Family history ratio is calculated as a simple division of all first-degree relatives who met criteria for MD (by participant report) by total number of first-degree relatives indexed. Additional items included as predictors include neuroticism score, endorsement of childhood sexual abuse (CSA) involving physical contact, number of stressful life events experienced (excluding CSA), and scores on the parental (both maternal and paternal) warmth sub-dimension of the 16-item Parental Bonding Instrument (PBI) modified by Kendler22 based on the original 25-item instrument described by Parker et al.23. Parental warmth is derived from seven items with four response categories in which the respondent is asked to report how accurately a statement describes their parent. All non-binary variables are standardized for ease of comparability.
Latent class analysis was performed in R 2.15.124, using the package “poLCA”25. The 7 comorbid anxiety disorder diagnoses (and age as a demographic covariate) were used to separate the MD cases into implicit subgroups that tended to suffer from similar patterns of anxiety comorbidity, or lack thereof. Groups were formed computationally based on tendencies for the anxiety comorbidities to covary, and the largest group in each model comprised MD cases without anxiety comorbidity – a ‘pure MDD’ or low anxiety class. Models including 2 to 6 latent classes were tested, and individuals given probabilities of assignment into each latent class based upon their comorbidity pattern. Lower Akaike Information Criterion (AIC) values, which use the number of parameters to adjust the -2 log likelihood values for each model and summarize how well balanced different models are between explanatory power and parsimony were used to inform final model selection. Bayesian Information Criterion (BIC) values and assessments of the interpretability of the resulting classes were also considered. Multiple imputation was used to include all cases in all latent classes for analysis, with each observation (each person and latent class pair) weighted by the probability of that individual being assigned to that class. Binary logistic regression was used to generate odds ratios for effects of risk factors on MD status (comparing controls without MD to all individuals with MD, whether or not they had an anxiety comorbidity diagnosis as well) and multinomial logistic regression used for their effects on the latent classes of anxiety comorbidity as well as the effects of clinical MD features on the latent anxiety comorbidity classes (comparing these classes only within MD cases). All regressions and continuation ratios13 were calculated in R 2.15.124, to determine the extent to which the risk factors were consistent in predicting MD and each latent class.
Results
As shown in Table 1, anxiety comorbidity is very common in the recurrent MD cases in the CONVERGE sample (53% of MD cases met criteria for at least one comorbid anxiety disorder). Total rates of specific anxiety disorders in the MD cases in the sample were 25.6% for GAD, 6.8% for panic disorder, 22.3% for animal phobia, 15.9% for blood-injury phobia, 14.8% for situational phobia, 12% for agoraphobia, and 10.8% for social phobia. The mean number of comorbid anxiety disorders was 1.08 (S.D. = 1.42). 53.2% of those with comorbid anxiety disorders had more than one.
Table 1.
Frequencies and prevalence of comorbid anxiety disorders in the MD cases of the CONVERGE sample.
| Comorbid disorder* | Number of individuals (out of 5,864 recurrent major depression cases) | Proportion of valid cases in category |
|---|---|---|
|
| ||
| No Anxiety Disorder | 2,757 | 47.0% |
| GAD | 1471 | 25.5% |
| Animal Phobia | 1269 | 22.1% |
| Blood-injury Phobia | 900 | 15.7% |
| Situational Phobia | 846 | 14.7% |
| Agoraphobia | 677 | 11.8% |
| Social Phobia | 611 | 10.6% |
| Panic Disorder | 387 | 6.7% |
All categories overlap partially except the first ‘No Anxiety Disorder’ category. Many individuals meet criteria for multiple comorbid anxiety disorders; as many as all 7 comorbid anxiety disorders.
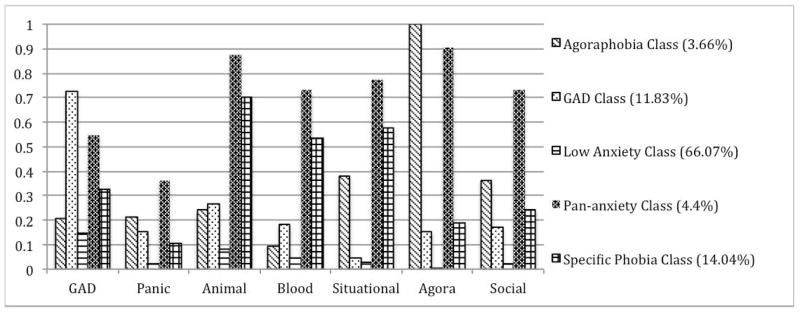
Table 2 lists the AIC and BIC fit statistics for the latent class models. The 5-class model had the lowest AIC, high interpretability, and so the 5-class solution was chosen for the remainder of the analyses. The resulting classes were given descriptive names based on the involvement of individual anxiety comorbidities in each (See Figure 2). The agoraphobia class was characterized by unanimous endorsement of agoraphobia and low to moderate rates of the other comorbidities; the GAD class endorsed GAD at high levels, and low levels of the other comorbidities; the low anxiety group had minimal endorsement of all anxiety comorbidities save some endorsement of GAD; the pan-anxiety group had among the highest levels of most anxiety comorbidities, and the specific phobia class had high levels of animal, blood-injury, and situational phobias, and moderate-low endorsement of the other anxiety comorbidities.
Table 2.
Latent Class AIC Fit Statistics
| Number of Latent Classes | AIC Statistic | BIC Statistic |
|---|---|---|
| 2 | 29074.05 | 29179.82 |
| 3 | 28960.42 | 29125.69 |
| 4 | 28896.16 | 29120.92 |
| 5 | 28867.02 | 29151.27 |
| 6 | 28873.99 | 29217.73 |
Figure 2. Endorsement of comorbid anxiety disorders in the 5 latent class solutions .
Percentages refer to the proportion of MD cases assigned to each latent class.
We tested the effects of known and putative risk factors for MD on both MD diagnosis and latent comorbid anxiety disorders classes using multiple imputation (see methods section). When each predictor was tested individually (see Table 3), many were associated with more than one anxiety comorbidity class. The largest latent class, the low anxiety class, was used as a reference category for multinomial regressions, meaning the odds ratios listed reflect the risk of being in a specific other latent class as opposed to the low anxiety class. Neuroticism, and stressful life events strongly predicted every kind of anxiety comorbidity and MD diagnosis. Parental warmth was protective against MD diagnosis, and paternal warmth was also protective against membership in the GAD class. Clinical features indicating higher severity of MD were predictive of all anxiety comorbidity classes to varying degrees though number of MD criteria was the most robust predictor. The pan-anxiety class, interestingly, was associated with all MD clinical features except age of onset and all risk factors except parental warmth.
Table 3.
Associations of major depressive disorder features and personal risk factors with the likelihood of major depression, and anxiety disorder comorbidity latent class membership analyzed in univariate regression.
| Risk Factor | MD1 | Low Anxiety Class2 | Agoraphobia Class2 | Pan-anxiety Class2 | Specific Phobia Class2 | GAD Class2 |
|---|---|---|---|---|---|---|
| Age of MD Onset* | - | 1 (Ref.) | 0.98 (0.77–1.26) | 0.82 (0.65–1.03) | 0.96 (0.84–1.10) | 0.77 (0.66–0.89) |
| # of MD Episodes* | - | 1 (Ref.) | 1.15 (0.95–1.40) | 1.23 (1.06–1.43) | 1.16 (0.99–1.26) | 1.06 (0.91–1.23) |
| # of MD Criteria* | - | 1 (Ref.) | 1.42 (1.05–1.92) | 1.70 (1.24–2.33) | 1.24 (1.08–1.44) | 1.28 (1.09–1.51) |
| FH of MD Ratio* | - | 1 (Ref.) | 1.19 (0.95–1.50) | 1.45 (1.23–1.71) | 1.22 (1.07–1.39) | 1.18 (1.03–1.37) |
| Neuroticism* | 8.69 (7.78–9.74) | 1 (Ref.) | 1.72 (1.28–2.32) | 3.49 (2.29–4.89) | 1.75 (1.48–2.06) | 1.85 (1.55–2.21) |
| Severe CSA | 5.48 (3.95–7.78) | 1 (Ref.) | 1.48 (0.65–3.36) | 2.19 (1.13–4.23) | 1.41 (0.88–2.25) | 1.54 (0.95–2.50) |
| Stressful Life Events* | 1.56 (1.47–1.67) | 1 (Ref.) | 1.50 (1.23–1.84) | 1.73 (1.45–2.06) | 1.43 (1.27–1.61) | 1.32 (1.16–1.51) |
| Maternal Warmth* | 0.63 (0.59–0.67) | 1 (Ref.) | 0.95 (0.75–1.19) | 0.95 (0.77–1.18) | 0.99 (0.87–1.12) | 0.94 (0.82–1.07) |
| Paternal Warmth* | 0.60 (0.56–0.64) | 1 (Ref.) | 0.99 (0.78–1.24) | 0.91 (0.74–1.13) | 0.98 (0.87–1.11) | 0.87 (0.76–0.99) |
Binary (for MD) and multinomial (for class membership) logistic regression risk ratios are presented with 99.64% confidence intervals (adjusted conservatively for 14 independent tests). Bold results are significant at this threshold.
Sample size for binary logistic regression predicting MD status with psychosocial risk factors, including all individuals with valid data, is 11,647.
Sample size for multinomial logistic regression predicting anxiety comorbidity latent class membership with MD clinical features and psychosocial risk factors, including only MD cases with valid data, is 5,864.
indicates a standardized variable.
When the predictors are entered into multivariate analysis (see Table 4), the results for individual risk factors are less strong, as expected. Only Neuroticism robustly predicted MD and all anxiety comorbidity classes. Clinical features of MD showed some associations with specific comorbidities. Early age of MD onset increased risk of membership in the GAD class. The family history of MD ratio predicted membership in the pan-anxiety class. Stressful life events significantly predicted all latent anxiety comorbidity classes, but didn’t independently predict MD after adjusting for the other risk factors.
Table 4.
Associations of major depressive disorder features and personal risk factors with the likelihood of major depression, and anxiety disorder comorbidity latent class membership analyzed in multivariate regression.
| Risk Factor | MD1 | Low Anxiety Class2 | Agoraphobia Class2 | Pan-anxiety Class2 | Specific Phobia Class2 | GAD Class2 |
|---|---|---|---|---|---|---|
| Age of MD Onset* | 1 (Ref.) | 1.05 (0.78–1.40) | 0.89 (0.67–1.20) | 1.00 (0.85–1.17) | 0.82 (0.68–0.98) | |
| # of MD Episodes* | - | 1 (Ref.) | 1.13 (0.91–1.39) | 1.06 (0.86–1.31) | 1.07 (0.93–1.23) | 1.01 (0.85–1.19) |
| # of MD Criteria* | - | 1 (Ref.) | 1.20 (0.85–1.69) | 1.32 (0.90–1.95) | 1.10 (0.92–1.31) | 1.17 (0.96–1.43) |
| FH of MD Ratio* | - | 1 (Ref.) | 1.13 (0.87–1.45) | 1.31 (1.08–1.60) | 1.15 (0.99–1.33) | 1.10 (0.93–1.30) |
| Neuroticism* | 8.21 (7.20–9.41) | 1 (Ref.) | 1.45 (1.02–2.07) | 2.83 (1.88–4.28) | 1.57 (1.29–1.92) | 1.64 (1.32–2.04) |
| Severe CSA | 1.73 (1.03–2.94) | 1 (Ref.) | 0.93 (0.31–2.78) | 1.04 (0.42–2.58) | 0.97 (0.52–1.80) | 1.00 (0.53–1.90) |
| Stressful Life Events* | 0.91 (0.82–1.01) | 1 (Ref.) | 1.38 (1.08–1.78) | 1.44 (1.16–1.80) | 1.32 (1.14–1.53) | 1.21 (1.02–1.42) |
| Maternal Warmth* | 0.93 (0.82–1.05) | 1 (Ref.) | 0.97 (0.71–1.33) | 1.14 (0.85–1.54) | 1.07 (0.90–1.28) | 1.09 (0.90–1.32) |
| Paternal Warmth* | 0.87 (0.77–0.98) | 1 (Ref.) | 1.12 (0.81–1.55) | 1.03 (0.76–1.38) | 1.08 (0.90–1.29) | 0.96 (0.79–1.16) |
Risk ratios are presented with 99.64% confidence intervals (adjusted conservatively for 14 independent tests). Bold results are significant at this threshold.
Sample size for binary logistic regression predicting MD status with psychosocial risk factors, including all individuals with valid data, is 11,647.
Sample size for multinomial logistic regression predicting anxiety comorbidity latent class membership with MD clinical features and psychosocial risk factors, including only MD cases with valid data, is 5,864.
indicates a standardized variable.
Finally, for those predictors that could be analyzed in association with both MD and the comorbid anxiety disorder classes, we calculated continuation ratios (Tables 5 A–D). We determined whether they were consistently associated with both MD and class membership in each class sequentially, with the exception of the low-anxiety group, which served as the reference group in the multinomial logistic regression. Using odds ratios from individual predictor regressions (as in Table 3), we determined that stressful life events predicted risk of membership in the agoraphobia, pan-anxiety and specific phobia classes more strongly than expected from its effect on MD. Neuroticism was also more strongly predictive of pan-anxiety class membership than expected from neuroticism’s effect on MD. The specific phobia class had a less protective association with paternal warmth than did MD as well. Finally, the GAD class didn’t display notable differences in risk factor associations from a more severe level of MD alone.
Table 5.
A–D.The relationship between selected demographic, personality, and life experience risk factors and MD diagnosis and any comorbid anxiety diagnoses given MD diagnosis.
| A. Continuation ratio between major depression and agoraphobia latent class. | |||
|---|---|---|---|
| Risk Factor | MD (OR) | Agoraphobia Class | Continuation ratio (p-value) |
| Neuroticism* | 8.69 | 1.72 | −0.114 (p=0.449) |
| Severe CSA | 5.48 | 1.48 | −0.110 (p=0.794) |
| Stressful Life Events* | 1.56 | 1.50 | 0.301 (p=0.003) |
| Maternal Warmth* | 0.63 | 0.95 | 0.108 (p=0.369) |
| Paternal Warmth* | 0.60 | 0.99 | 0.172 (p=0.157) |
| B. Continuation ratio between major depression and pan-anxiety latent class. | |||
|---|---|---|---|
| Risk Factor | MD (OR) | Pan-Anxiety Class | Continuation ratio (p-value) |
| Neuroticism* | 8.69 | 3.49 | 0.559 (p=0.009) |
| Severe CSA | 5.48 | 2.19 | 0.248 (p=0.463) |
| Stressful Life Events* | 1.56 | 1.73 | 0.433 (p=1.6e-6) |
| Maternal Warmth* | 0.63 | 0.95 | 0.109 (p=0.309) |
| Paternal Warmth* | 0.60 | 0.91 | 0.092 (p=0.385) |
| C. Continuation ratio between major depression and specific phobias latent class. | |||
|---|---|---|---|
| Risk Factor | MD (OR) | Specific Phobia Class | Continuation ratio (p-value) |
| Neuroticism* | 8.69 | 1.75 | −0.116 (p=0.173) |
| Severe CSA | 5.48 | 1.41 | −0.178 (p=0.460) |
| Stressful Life Events* | 1.56 | 1.43 | 0.223 (p=2.2e-4) |
| Maternal Warmth* | 0.63 | 0.99 | 0.155 (p=0.019) |
| Paternal Warmth* | 0.60 | 0.98 | 0.170 (p=0.005) |
| D. Continuation ratio between major depression and GAD latent class. | |||
|---|---|---|---|
| Risk Factor | MD (OR) | GAD Class | Continuation ratio (p-value) |
| Neuroticism* | 8.69 | 1.85 | −0.061 (p=0.496) |
| Severe CSA | 5.48 | 1.54 | −0.097 (p=0.693) |
| Stressful Life Events* | 1.56 | 1.32 | 0.158 (p=0.016) |
| Maternal Warmth* | 0.63 | 0.94 | 0.108 (p=0.122) |
| Paternal Warmth* | 0.60 | 0.87 | 0.063 (p=0.365) |
Odds ratios taken from individual predictor regressions (Table 3)
Bold results significant after multiple testing correction (for 14 tests for MD and Any Anxiety Comorbidity, and for 5 tests for the continuation ratio)
indicates a standardized variable.
Discussion
We began by investigating how many distinguishable patterns of anxiety comorbidity in MD could be resolved by latent class analysis. The five latent classes resulting from our analysis suggest that individuals suffering from a course of recurrent MD complicated with comorbid anxiety disorders may tentatively be grouped into descriptive classes, which have signature presentations as well as differential associations with common risk factors (the second part of our investigation). A few trends emerge from the characteristics of the classes that resulted.
GAD occurred in all classes to varying degrees: even in the low anxiety group endorsement rates did not approach zero. The phobias tend to co-occur, with most phobic individuals, such as those in the pan-anxiety or specific phobia groups, having a high likelihood of endorsing multiple phobias. The class characterized by unanimous agoraphobia endorsement was somewhat peculiar; many robust risk factors failing to predict membership in this class. The possibility that this class may be less well distinguished from the others in the data also exists, as latent class analysis, as an atheoretical technique, can find patterns that are not reflected in nature.
Logistic regression suggests that the best predictors of belonging to a class characterized by comorbid anxiety disorders with MD (of those tested) are neuroticism, number of stressful live events experienced, number of MD criteria endorsed and, to a lesser degree, proportion of MD in 1st-degree relatives of probands. The analyses of all risk factors collectively in multivariate regression suggests heterogeneity in the effectiveness of family history in predicting comorbid anxiety disorder class membership, however, and that the number of MD criteria is likely not a robust predictor of these patterns of anxiety comorbidity, losing explanatory power in the multivariate model.
Our final question of risk factor consistency for MD and the anxiety comorbidity classes was addressed by our continuation ratio results, presented in Tables 5 A–D. If a risk factor acts on MD and an anxiety comorbidity class as different levels along an underlying scale (as in Figure 1), the continuation ratio should be approximately zero. If significantly positive, the predictor’s risk contribution to membership in the anxiety comorbidity class is greater than its effects on the risk of MD status. If significantly negative, the predictor increases risk of MD status more than it does risk of membership in an anxiety comorbidity class. There are notable departures of the continuation ratio from zero to be seen in Tables 5 A–C.
Our study has some limitations. Latent class analysis is an exploratory technique, and its findings rely on interpretation. The possibility of more meaningful classification models cannot be excluded. The CONVERGE sample may be imperfectly representative of MD and the anxiety disorders. Results from CONVERGE have been largely consistent with MD results from other populations, however26, 27, so the present analysis is expected to be generalizable to MD and comorbid anxiety disorders in other populations. The logistic regressions were unadjusted for demographic characteristics, but since the sample is largely homogenous (same ethnicity, same sex, and relatively limited age range), it’s probable that this biased the estimates minimally. In addition, the effect of age of MD onset (which is correlated with age) was assessed and the latent class analysis included age as a covariate, so the latent classes are age-adjusted. It’s possible other factors may be significantly associated with MD and/or comorbid anxiety disorders but were unmeasured. In order to manage multiple testing correction, not all risk factors were included in the analysis, and indeed, some putative ones weren’t assessed in CONVERGE, such as certain chronic medical conditions28, and self-esteem29. The absence of anxiety disorder groups without MD could cause the failure of the local independence assumption, if there are factors that cause correlation between the indicator variables (anxiety disorder diagnoses) not accounted for by latent class membership. This should be tested in future studies that include anxiety disorder groups without major depression. Finally, this investigation is cross-sectional, and therefore temporality cannot be established in most associations between variables. Since all risk factors, clinical features, and diagnoses used are lifetime indices it is equally plausible in some cases that the ‘predictor’ (for example, a stressful life event) occurred after the ‘outcome’ (such as the onset of MD). However since the focus of this investigation is on lifetime risk factors, most included predictors will be relatively constant in an individual person’s life (such as neuroticism or parental warmth), and most stressful life events occurred before MD onset in this sample (96.5% of recorded events), we expect that in most cases the associations are indeed ‘predictive’, if not necessarily causal.
Conclusion
Based on these results, it seems the best indicators of an MD course complicated by comorbid anxiety pathology are stressful life events, and high neuroticism, as suggested by past literature3, 15. These risk factors are also associated with MD itself. Less well-studied risk factor results include early age of depression onset predicting comorbid GAD, and family history ratio predicting pan-anxiety class membership, affected with multiple comorbid anxiety disorders. The fact that a high density of MD in one’s family predicts anxiety comorbidity class membership is suggestive of the shared genetic underpinnings of the two types of disorders9, 10. Genetic factors that contribute to neuroticism overlap with those that influence MD, as well as anxiety disorders30; these risk factors representing genetic influences are predictably associated with both MD and anxiety comorbidity.
The departure of the continuation ratio from zero for neuroticism in the prediction of the pan-anxiety class suggests this class may represent a distinct genetic profile rather than a higher dose of the MD genetic risk. Other factors, such as stressful life events and parental warmth may index genetic risk less directly, but the degree to which they function similarly between MD and anxiety comorbidity classes is indicative perhaps of latent environmental correlation between these outcomes. The agoraphobia, pan-anxiety and specific phobia classes seem to respond differently to these important measures of life experiences, and therefore their etiology may involve some processes distinct from MD’s. Since all tested continuation ratios were not appreciably different from zero for the GAD class, it’s possible that the GAD class is consistent with being a more severe form of MD; the individuals in this class may be able to attribute their comorbid generalized anxiety disorder to most of the same etiological origins as their MD. The causes of their anxiety comorbidity may be similar to the causes of their MD itself, with little more than a difference in degree separating them from those in the low-anxiety class. The extent of the factors that determine the onset of MD and whether it will be joined with a comorbid anxiety disorder are still incompletely understood. Future studies incorporating genetic, environmental, and person-level information will be necessary to further illuminate the etiological landscape underlying MD and anxiety disorders. Only when a comprehensive understanding of both the shared factors that contribute to depressive and anxiety disorders as well as those influences that distinguish them is gained will we be able to make substantial progress in their assessment and treatment.
Acknowledgments
The authors would like to thank all of the individuals involved in the CONVERGE project for their excellent work involved in collecting and managing the data set.
A. Moscati is supported by institutional training grant award no. T32 MH20030 from the National Institutes of Health and National Institute of Mental Health for Research Training in Psychiatric and Statistical Genetics
Footnotes
The authors of this manuscript have no conflict of interest to disclose.
References
- 1.Breslau N. Depressive symptoms, major depression, and generalized anxiety: a comparison of self-reports on CES-D and results from diagnostic interviews. Psychiatry research. 1985;15(3):219–29. doi: 10.1016/0165-1781(85)90079-4. Epub 1985/07/01. [DOI] [PubMed] [Google Scholar]
- 2.Breslau N, Davis GC. DSM-III generalized anxiety disorder: an empirical investigation of more stringent criteria. Psychiatry research. 1985;15(3):231–8. doi: 10.1016/0165-1781(85)90080-0. Epub 1985/07/01. [DOI] [PubMed] [Google Scholar]
- 3.Kessler RC, Gruber M, Hettema JM, Hwang I, et al. Co-morbid major depression and generalized anxiety disorders in the National Comorbidity Survey follow-up. Psychological medicine. 2008;38(3):365–74. doi: 10.1017/S0033291707002012. Epub 2007/12/01. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Zimmerman M, Chelminski I. Generalized anxiety disorder in patients with major depression: is DSM-IV’s hierarchy correct? The American journal of psychiatry. 2003;160(3):504–12. doi: 10.1176/appi.ajp.160.3.504. Epub 2003/03/04. [DOI] [PubMed] [Google Scholar]
- 5.Smits JA, Minhajuddin A, Jarrett RB. Cognitive therapy for depressed adults with comorbid social phobia. Journal of affective disorders. 2009;114(1–3):271–8. doi: 10.1016/j.jad.2008.08.008. Epub 2008/09/23. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.DeVeaugh-Geiss AM, West SL, Miller WC, Sleath B, et al. Depression and comorbid panic in primary care patients. Journal of affective disorders. 2010;123(1–3):283–90. doi: 10.1016/j.jad.2009.09.013. Epub 2009/10/16. [DOI] [PubMed] [Google Scholar]
- 7.Mathew AR, Pettit JW, Lewinsohn PM, Seeley JR, et al. Co-morbidity between major depressive disorder and anxiety disorders: shared etiology or direct causation? Psychological medicine. 2011;41(10):2023–34. doi: 10.1017/S0033291711000407. Epub 2011/03/29. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Moffitt TE, Harrington H, Caspi A, Kim-Cohen J, et al. Depression and generalized anxiety disorder: cumulative and sequential comorbidity in a birth cohort followed prospectively to age 32 years. Archives of general psychiatry. 2007;64(6):651–60. doi: 10.1001/archpsyc.64.6.651. Epub 2007/06/06. [DOI] [PubMed] [Google Scholar]
- 9.Kendler KS, Neale MC, Kessler RC, Heath AC, et al. Major depression and generalized anxiety disorder. Same genes, (partly) different environments? Archives of general psychiatry. 1992;49(9):716–22. doi: 10.1001/archpsyc.1992.01820090044008. Epub 1992/09/01. [DOI] [PubMed] [Google Scholar]
- 10.Kendler KS, Gardner CO, Gatz M, Pedersen NL. The sources of co-morbidity between major depression and generalized anxiety disorder in a Swedish national twin sample. Psychological medicine. 2007;37(3):453–62. doi: 10.1017/S0033291706009135. Epub 2006/11/24. [DOI] [PubMed] [Google Scholar]
- 11.Kessler RC. The effects of stressful life events on depression. Annual review of psychology. 1997;48:191–214. doi: 10.1146/annurev.psych.48.1.191. Epub 1997/01/01. [DOI] [PubMed] [Google Scholar]
- 12.Kendler KS, Hettema JM, Butera F, Gardner CO, et al. Life event dimensions of loss, humiliation, entrapment, and danger in the prediction of onsets of major depression and generalized anxiety. Archives of general psychiatry. 2003;60(8):789–96. doi: 10.1001/archpsyc.60.8.789. Epub 2003/08/13. [DOI] [PubMed] [Google Scholar]
- 13.MacLean CJ. Assessing changes in risk factor effect over multiple levels of severity. American journal of epidemiology. 1988;127(3):663–73. doi: 10.1093/oxfordjournals.aje.a114841. Epub 1988/03/01. [DOI] [PubMed] [Google Scholar]
- 14.Lamers F, de Jonge P, Nolen WA, Smit JH, et al. Identifying depressive subtypes in a large cohort study: results from the Netherlands Study of Depression and Anxiety (NESDA) The Journal of clinical psychiatry. 2010;71(12):1582–9. doi: 10.4088/JCP.09m05398blu. Epub 2010/08/03. [DOI] [PubMed] [Google Scholar]
- 15.Unick GJ, Snowden L, Hastings J. Heterogeneity in comorbidity between major depressive disorder and generalized anxiety disorder and its clinical consequences. The Journal of nervous and mental disease. 2009;197(4):215–24. doi: 10.1097/NMD.0b013e31819d954f. Epub 2009/04/14. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Li Y, Shi S, Yang F, Gao J, et al. Patterns of co-morbidity with anxiety disorders in Chinese women with recurrent major depression. Psychological medicine. 2012;42(6):1239–48. doi: 10.1017/S003329171100273X. Epub 2011/12/01. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Organization WH. Composite International Diagnostic Interview (CIDI) Version 2.1. Geneva: World Health Organization; 1997. [Google Scholar]
- 18.APA. Diagnostic and Statistical Manual of Mental Disorders. Washington, DC: American Psychiatric Association; 1994. [Google Scholar]
- 19.Kendler KSPCA. Genes, Environment, and Psychopathology: Understanding the Causes of Psychiatric and Substance Use Disorders. 1. New York: Guildford Press; 2006. [Google Scholar]
- 20.Endicott JAN, Spitzer RL. Family History Research Diagnostic Criteria. New York: Biometrics Research, New York State Psychiatric Institute; 1975. [Google Scholar]
- 21.Eysenck HJE, SBG . Manual of the Eysenck Personality Questionnaire. London: Hodder and Stoughton; 1975. [Google Scholar]
- 22.Kendler KS. Parenting: a genetic-epidemiologic perspective. The American journal of psychiatry. 1996;153(1):11–20. doi: 10.1176/ajp.153.1.11. Epub 1996/01/01. [DOI] [PubMed] [Google Scholar]
- 23.Parker GTH, Brown L. A Parental Bonding Instrument. British Journal of Medical Psychology. 1979;52:1–10. [Google Scholar]
- 24.Team RC. R: A language and environment for statistical computing. Vienna, Austria: R Foundation for Statistical Computing; 2012. [Google Scholar]
- 25.Linzer DALJ. poLCA: An R Package for Polytomous Variable Latent Class Analysis. Journal of Statistical Software. 2011;42(10):1–29. [Google Scholar]
- 26.Flint J, Chen Y, Shi S, Kendler KS, et al. Epilogue: Lessons from the CONVERGE study of major depressive disorder in China. Journal of affective disorders. 2012;140(1):1–5. doi: 10.1016/j.jad.2011.09.006. Epub 2011/10/01. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Kendler KS, Aggen SH, Li Y, Lewis CM, et al. The similarity of the structure of DSM-IV criteria for major depression in depressed women from China, the United States and Europe. Psychological medicine. 2015;45(9):1945–54. doi: 10.1017/S0033291714003067. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Jann MW, Slade JH. Antidepressant agents for the treatment of chronic pain and depression. Pharmacotherapy. 2007;27(11):1571–87. doi: 10.1592/phco.27.11.1571. Epub 2007/10/30. [DOI] [PubMed] [Google Scholar]
- 29.Sowislo JF, Orth U. Does low self-esteem predict depression and anxiety? A meta-analysis of longitudinal studies. Psychological bulletin. 2013;139(1):213–40. doi: 10.1037/a0028931. Epub 2012/06/27. [DOI] [PubMed] [Google Scholar]
- 30.Hettema JM, Neale MC, Myers JM, Prescott CA, et al. A population-based twin study of the relationship between neuroticism and internalizing disorders. The American journal of psychiatry. 2006;163(5):857–64. doi: 10.1176/appi.ajp.163.5.857. Epub 2006/05/02. [DOI] [PubMed] [Google Scholar]