Abstract
Purpose
To determine predictors of reoperation and abnormal binocularity outcomes (including amblyopia and diplopia) following pediatric strabismus surgery.
Design
Retrospective cross-sectional study.
Methods
Setting: Review of a national insurance database. Study population: Children under age 18 years having strabismus procedures between 2007 and 2013. Interventions: Adjustable or fixed suture strabismus surgery, or botulinum toxin injection. Outcome measures: Reoperation or diagnosis of abnormal binocularity in the first postoperative year.
Results
Of 11,115 children having strabismus procedures, 851 (7.7%) underwent reoperation. The reoperation rate was 7.4% for fixed suture surgeries, 9.6% for adjustable suture surgeries (p=0.18), and 44.9% for botulinum injections (p<0.001). Age under 2 years was associated with higher reoperation and abnormal binocularity rates (p<0.001). For horizontal strabismus, the postoperative abnormal binocularity rate was 12.8% for fixed suture surgery and 26.5% for botulinum injection (p=0.005). Reoperation rates tended to be higher with adjustable sutures (odds ratio [OR] 1.69, 95% confidence interval [CI] 0.94 to 3.03, p=0.08), or botulinum toxin injection (OR 10.36, 95% CI 5.75 to 18.66, p<0.001) and lower with 3- or 4-muscle surgery (p=0.001). Esotropia, hyperopia, and botulinum injection were independently associated with higher rates of postoperative abnormal binocularity (p<=0.005). For vertical surgeries, predictors of reoperation were adjustable suture use (OR 2.51, p=0.10) and superior oblique surgery (OR 2.36, p<0.001).
Conclusions
Adjustable sutures were not associated with a lower reoperation rate in children. Younger age, esotropia, hyperopia, and botulinum injection were associated with postoperative abnormal binocularity. Superior oblique surgery and botulinum injection were associated with higher rates of reoperation.
Introduction
Surgical correction of childhood strabismus can produce proper eye alignment and facilitate the development of binocular vision.1 Surgical strategies include conventional fixed suture strabismus surgery, adjustable suture surgery, and extraocular muscle botulinum toxin injection.
The approach to strabismus can involve some flexibility in selecting muscles for surgery. For instance, one- vs. two-muscle surgery for smaller angle strabismus has been debated.2 Similarly, whether to operate on two, or more than two, muscles in large angle esotropia is not well-defined.3 In addition, for exotropia, unilateral two-muscle surgery has been found to have a lower reoperation rate than bilateral single-muscle surgery in a retrospective review of adult surgery4 and in randomized trials which included primarily children.5,6
In addition to selecting muscles on which to operate, the surgeon must decide whether to place fixed or adjustable sutures. Adjustable suture strabismus surgery offers the opportunity to refine the muscle position in the immediate postoperative period. Adjustable surgery has been advocated in children by several authors,7–13 but use in this age group presents particular challenges. Children often have difficulty cooperating with visual target fixation when experiencing discomfort from surgery and residual effects from anesthesia. Increased anesthesia time to place the suture in the operating room, and to tie off or adjust the suture afterwards, can be required in younger children.
In addition to,14 or in place of15 incisional surgery, the surgeon may inject botulinum toxin into the extraocular muscles. Botulinum injection by itself has been found to produce similar motor and sensory outcomes in children with persistent strabismus following incisional surgery.16,17 Extraocular muscle scarring is avoided, and the short procedure duration minimizes anesthesia time. The latter is particularly advantageous in patients under age four years, in whom general anesthesia might have deleterious effects on cognitive development.18,19 Unfortunately, botulinum toxin effects may not persist.20 To our knowledge, randomized comparisons of botulinum toxin with incisional surgery have not been published for primary pediatric strabismus procedures, although this is an area of active interest.21
We studied the outcome of pediatric strabismus procedures by determining reoperation rates (a motor outcome) and abnormal binocularity (a sensory outcome) in a large national insurance database.
Methods
This retrospective population-based cross-sectional study was approved by the Office of Research Subjects Protection of the Virginia Commonwealth University. The study utilized the MarketScan Commercial Claims and Encounters, and the Medicare Supplemental and Coordination of Benefit databases (Truven Health Analytics, Ann Arbor, MI, USA) from the years 2007 through 2013 (the most recent year the databases were available). The MarketScan family of databases comprises the largest convenience-based proprietary database in the US, annually encompassing approximately 50 million patients with employer-sponsored or supplemental insurance.22 These databases consist of de-identified, individual-level health records (inpatient and outpatient), obtained from large employers, hospitals, and Medicare programs. Additional details regarding the MarketScan databases, sampling methodologies, and limitations are described elsewhere.22 These databases have been used to report various ophthalmic treatment outcomes,23,24 including strabismus surgery reoperation in adults.4
We searched the databases for children under age 18 having strabismus procedures. The procedure (coded using the Current Procedural Terminology, CPT) and diagnosis (coded using the International Classification of Disease, ICD-9) were noted. Strabismus procedures included horizontal (CPT 67311, 67312) or vertical (CPT 67314, 67316, 67318) muscle surgery or botulinum toxin injection (CPT 67345) on one or both eyes. We only included patients who had insurance for a full year postoperatively. We excluded patients having an index surgery diagnosis code for nystagmus (ICD 379.50–379.56).
We identified patients having a reoperation (a motor outcome), a diagnosis of abnormal binocularity (a sensory outcome), or either of these outcomes in the first year after surgery. We counted either horizontal or vertical procedures as reoperations, as done previously.4 In the present study, any additional incisional strabismus surgery or botulinum injection within the first year counted as a reoperation. All of these procedures usually involve general anesthesia in children. For combined horizontal plus vertical surgeries, it was not clear from the claim whether the adjustable suture was used for a horizontal or a vertical muscle. Moreover, due to half-tendon width and other transpositions, and for other reasons, horizontal muscle surgery might influence vertical alignment, and vice-versa. Abnormal binocularity was defined to include office visit claims of amblyopia, diplopia, or anomalous retinal correspondence (Table 1).
TABLE 1.
Diagnostic Categories in Strabismus Patients.
| Patient category. | Definition. |
|---|---|
| Esotropia. | ICD 378.00–378.08, 378.21, 378.22, 378.35, 378.41, 378.54, 378.84. |
| Exotropia. | ICD 378.10–378.18, 378.23, 378.24, 378.42, 378.81, 378.83, 378.86. |
| Refractive asymmetry. | Aniseikonia (ICD 367.32), anisometropia (367.31). |
| Myopia subtypes. | Myopia (ICD 367.1), progressive high myopia (360.21) |
| Abnormal binocularity. | Amblyopia: unspecified (ICD 368.00), strabismic (368.01), deprivation (368.02), refractive (368.03), diplopia (368.2), 368.30 (binocular vision disorder unspecified), 368.31 (suppression of binocular vision), 368.32 (simultaneous visual perception without fusion), 368.33 (fusion with defective stereopsis), 368.34 (abnormal retinal correspondence) |
ICD = International Classification of Diseases.
In the analysis comparing horizontal strabismus surgery and botulinum toxin injection, patients had to have a diagnosis code consistent with esotropia, exotropia, or Duane syndrome (ICD 378.71, Table 1). Without these diagnosis codes, it is unclear if an injection was for a horizontal or vertical deviation.
Variables associated with outcomes in the first year were determined. Patient groupings for univariate analysis included age (0–1, 2–4, 5–8, and 9–17 years), use of adjustable suture (CPT 67335), number of muscles operated, and several procedure and diagnosis categories (Table 1). The following strabismus types were defined as previously: complex, incomitant, paralytic, alternating, A or V pattern, mechanical, intermittent.4 As previously, monocular deviation was defined as ICD 378.01–378.04, 378.11–378.14, or 378.34.4 Diagnosis codes for refractive error (e.g. hyperopia, ICD 367.0, and regular astigmatism 367.21) and abnormal binocularity were identified in the claims record, which included office visits, in the two years prior to surgery (Table 1).
The patient was included in the adjustable suture group if an adjustable suture was used on any muscle, even if other muscles in the same or the contralateral eye were sutured in the conventional fashion. Because adjustable sutures are not typically used for oblique muscle surgery, we performed secondary analyses which excluded patients having superior oblique surgery (CPT 67318) or fourth nerve palsy (ICD 378.53).
Proportions were compared by the Fisher exact test. A multivariable logistic regression model was prepared in a stepwise backwards fashion. Stated odds ratios (OR) and 95% confidence intervals (CI) apply to multivariable analysis. Analysis was performed in SPSS (version 22, SPSS Inc., Chicago, IL, USA).
Results
Overall analysis of all patients
Of 11,115 total children who underwent strabismus procedures, 7.7% had a reoperation, 12.1% had abnormal binocularity, and 18.2% had either (or both) of these outcomes in the first postoperative year (Table 2).
TABLE 2.
Overall Rates of Reoperation and Abnormal Binocularity Following Strabismus Surgery.
| Type of Surgery. |
Total. | Reoperation | Abnormal binocularity. |
Reoperation or abnormal binocularity. |
|||
|---|---|---|---|---|---|---|---|
| n | n | % | n | % | n | % | |
| Fixed suture surgery. | 10,806 | 804 | 7.4% | 1313 | 12.2% | 1955 | 18.1% |
| Adjustable surgery. | 260 | 25 | 9.6% | 24 | 9.2% | 45 | 17.3% |
| Botulinum injection only. | 49 | 22 | 44.9% | 13 | 26.5% | 25 | 51.0% |
| Total. | 11,115 | 851 | 7.7% | 1350 | 12.1% | 2025 | 18.2% |
n = number of patients.
Younger age was consistently associated with reoperation and abnormal binocularity. For instance, children under age 2 had an odds ratio for reoperation of 3.24, compared with children age 5 to 17, and an odds ratio for abnormal binocularity of 2.34 compared with children age 9 to 17 (Supplemental Tables 1 and 2 at AJO.com, both p<0.001).
Only 2.3% of incisional surgeries in this sample were performed in an adjustable fashion (Table 2). Reoperations were performed after 9.6% of adjustable suture surgeries and after 7.4% of fixed suture surgeries (p=0.19, Table 2). After controlling for age and other factors, adjustable sutures were associated with a higher rate of reoperation (multivariable odds ratio 1.65, 95% CI 1.08 to 2.54, p=0.02, Supplemental Table 1 at AJO.com). Postoperatively, reoperation and/or abnormal binocularity occurred in 17.3% of adjustable surgery patients and in 18.1% of fixed suture patients (p=0.81, Table 2). The combined outcome of reoperation and/or abnormal binocularity with adjustable sutures did not differ significantly from that with fixed sutures (OR 1.16, 95% CI 0.82 to 1.63, p=0.41, Supplemental Table 3 at AJO.com).
Because adjustable sutures are infrequently used for oblique muscle surgery, we repeated the analysis after exclusion of surgeries of the superior oblique or for fourth nerve palsy. Reoperations were performed after 8.2% of adjustable suture surgeries (20 of 244) and after 7.1% of fixed suture surgeries (705 of 9950, p=0.53). The association of adjustable sutures with reoperations was not statistically significant (multivariable odds ratio 1.47, 95% CI 0.91 to 2.36, p=0.11). Postoperatively, reoperation and/or abnormal binocularity occurred in 16.4% of adjustable surgery patients and in 18.0% of fixed suture patients (p=0.56, Supplemental Tables 1 and 4 at AJO.com). The combined outcome of reoperation and/or abnormal binocularity with adjustable sutures did not differ significantly from that with fixed sutures (OR 1.08, 95% CI 0.75 to 1.56, p=0.67, Supplemental Table 3 at AJO.com).
Abnormal binocularity before surgery was associated with a slight tendency to fewer reoperations (OR 0.78, p=0.01), but was strongly associated with a higher probability of abnormal binocularity postoperatively (OR 7.38, 95% CI 6.52 to 8.36, p<0.001). Vertical surgery was associated with a higher likelihood of reoperation (OR 1.39, p<0.001, Supplemental Tables 1 and 2 at AJO.com).
Because botulinum injection was used only for horizontal surgery, and because a previous analysis demonstrated effect modification for the association of adjustable surgery with reoperation rate depending on whether a horizontal or vertical surgery was performed,4 we present below separate analyses of isolated horizontal and vertical muscle surgery.
Isolated horizontal muscle procedures
Of 7740 children having procedures exclusively on horizontal muscles, 6.7% had a reoperation, 12.7% had abnormal binocularity, and 18.1% had either (or both) of these outcomes in the first postoperative year (Tables 3 and 4, and Supplemental Table 5 at AJO.com). The CPT code often applied with scarring due to prior surgery (67332) was used in 1015 cases (13%, Supplemental Table 6 at AJO.com). Only 1 patient had the - 58 modifier to indicate a planned reoperation.
TABLE 3.
Predictors of Reoperation Following Horizontal Strabismus Surgery.
| Clinical Factor | Reoperation | Multivariable Analysis. | |
|---|---|---|---|
| Odds Ratio (95% CI) | p value. | ||
| Age 5 to 17 years. | 5.0% (228/4551) | 1.00 (reference) | -- |
| ……2 to 4 years. | 6.9% (162/2352) | 1.35 (1.09 to 1.67) | 0.005 |
| ……0 to 1 year. | 15.4% (129/836) | 3.33 (2.63 to 4.21) | <0.001 |
| Fixed suture. | 6.4% (484/7521) | 1.00 (reference) | -- |
| Adjustable suture. | 7.6% (13/170) | 1.69 (0.94 to 3.03) | 0.08 |
| Botulinum toxin only. | 44.9% (22/49) | 10.36 (5.75 to 18.66) | <0.001 |
| 3 or 4 muscles operated. | 3.7% (44/1178) | 0.58 (0.42 to 0.80) | 0.001 |
| Monocular deviation. | 4.7% (56/1192) | 0.75 (0.56 to 1.00) | 0.049 |
| Astigmatism. | 15.9% (10/63) | 2.85 (1.40 to 5.74) | 0.004 |
| Abnormal binocularity, preoperative. | 5.2% (81/1571) | 0.74 (0.58 to 0.95) | 0.02 |
| Total. | 6.7% (519/7740) | -- | -- |
CI = confidence interval.
TABLE 4.
Predictors of Abnormal Binocularity Following Horizontal Strabismus Surgery.
| Clinical Factor | Abnormal binocularity (%) |
Multivariable Analysis. | |
|---|---|---|---|
| Odds Ratio (95% CI) | p value. | ||
| Age 9 to 17 years. | 7.7% (174/2260) | 1.00 (reference) | -- |
| ……0 to 8 years. | 14.8% (812/5480) | 1.82 (1.50 to 2.19) | <0.001 |
| Fixed suture. | 12.8% (959/7521) | 1.00 (reference) | -- |
| Botulinum toxin only. | 26.5% (13/49) | 2.75 (1.36 to 5.56) | 0.005 |
| Adjustable suture. | 8.2% (14/170) | 0.66 (0.36 to 1.20) | 0.17 |
| 3 or 4 muscles operated. | 16.9% (199/1178) | 1.40 (1.16 to 1.70) | <0.001 |
| Esotropia. | 16.4% (667/4072) | 1.51 (1.29 to 1.76) | <0.001 |
| Astigmatism. | 28.6% (18/63) | 2.80 (1.57 to 5.15) | <0.001 |
| Abnormal binocularity, preoperative. | 36.3% (570/1571) | 7.15 (6.17 to 8.28) | <0.001 |
| Hyperopia | 25.4% (93/366) | 1.74 (1.32 to 2.30) | <0.001 |
| Refractive asymmetry | 33.9% (20/59) | 2.00 (1.08 to 3.70) | 0.03 |
| Total. | 12.7% (986/7740) | -- | -- |
CI = confidence interval.
Younger age was associated with a higher rate of reoperation and abnormal binocularity. The reoperation rate decreased progressively from 15.4% for those under age 2 to 5.0% for those over age 4 (p<0.001, Table 3). Similarly, the likelihood of abnormal binocularity in the first postoperative year decreased from 14.8% for those under age 9 to 7.7% for those ages 9 to 17 (p<0.001, Table 4).
The reoperation rate was 7.4% with one muscle operated (106 of 1434), and 6.8% with 2 muscles operated (347 of 5079, p=0.48, Supplemental Table 7 at AJO.com). The rate of abnormal binocularity after surgery was 9.3% with one muscle operated (134 of 1434) and 12.6% with two muscles operated (640 of 5079, p=0.001, Supplemental Table 6 at AJO.com). As compared with 1-or 2-muscle surgery, operating on 3 or 4 muscles had a lower reoperation rate of 3.7% (p=0.001, Table 3), but a higher rate of abnormal postoperative binocularity of 16.9% (p<0.001, Table 4).
Unilateral surgery on two horizontal muscles comprised only 9.1% of horizontal cases, while bilateral one muscle surgery comprised 56.5% of horizontal cases. There was no significant difference in reoperation rate with unilateral surgery on two horizontal muscles (6.0%) compared with bilateral surgery on one horizontal muscle (7.0%, p=0.16, Supplemental Table 7 at AJO.com). With separate evaluations of esotropia and of exotropia, these two types of two-muscle surgery continued to have similar reoperation rates (Supplemental Table 8 at AJO.com). For exotropia, the reoperation rate was 6.0% with bilateral one-muscle surgery (117 of 1953) and was 5.3% with unilateral two-muscle surgery (20 of 375, p=0.72, Supplemental Table 8 at AJO.com). The rate of postoperative abnormal binocularity was also similar with bilateral one muscle surgery (12.3%, 539 of 4374) and unilateral two-muscle surgery (14.3%, 101 of 705, p=0.14, Supplemental Table 6 at AJO.com).
The reoperation rate in the first postoperative year was 7.6% with adjustable sutures (13 of 170) and 6.4% with fixed sutures (484 of 7521, p=0.53, Supplemental Table 5 at AJO.com, Figure 1). After controlling for relevant factors, the reoperation rate with adjustable sutures was not significantly different (multivariable OR 1.69, 95% CI 0.94 to 3.03, p=0.08, Table 3). The 8.2% rate of abnormal binocularity with adjustable sutures tended to be lower than the 12.8% seen with fixed sutures (multivariable OR 0.66, p=0.17, Table 4). The combined outcome of reoperation and/or abnormal binocularity was not significantly different with adjustable sutures (15.3%, multivariable OR 1.04, 95% CI 0.66 to 1.62, p=0.88) compared with fixed sutures (17.9%, Supplemental Tables 5 and 9 at AJO.com).
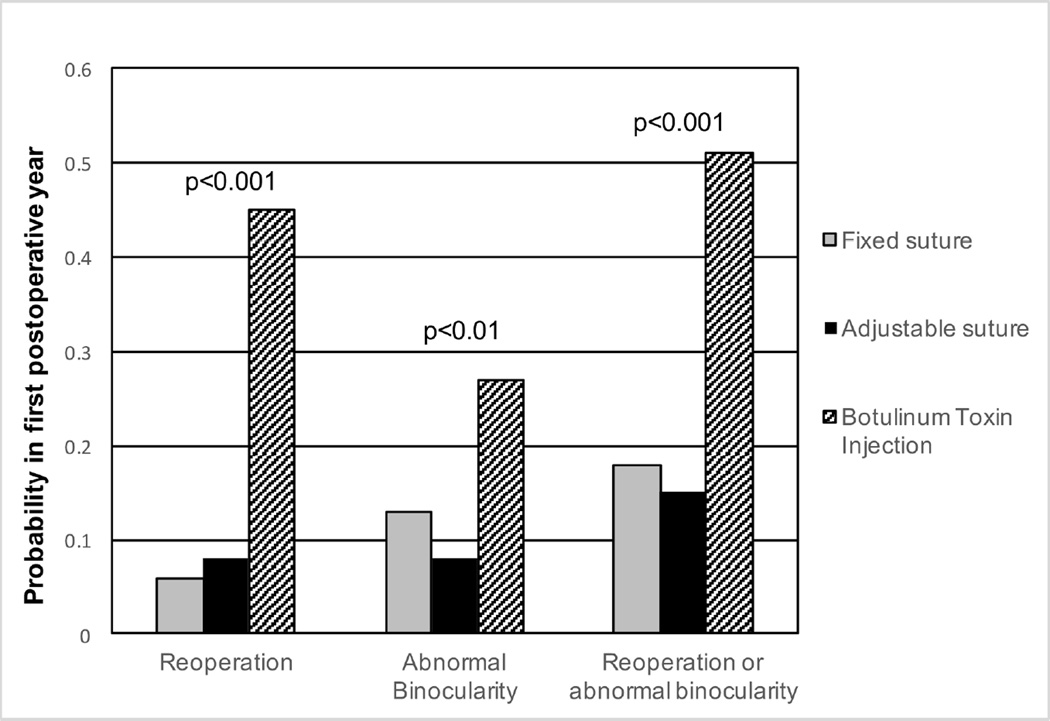
FIGURE 1.
Probability of Reoperation, Abnormal Binocularity, or Either Outcome in the First Year after Horizontal Strabismus Surgery.
There was no benefit of adjustable sutures in an analysis restricted to older patients. For instance, in patients age 5 to 17 with one- or two-muscle surgery, and none of the risk factors associated with reoperation, the reoperation rate was 11.6% with adjustable sutures (8 of 69 patients) and actually tended to be lower with fixed suture technique (5.7%, 69 of 1204, p=0.06, Supplemental Table 10 at AJO.com).
Patients with monocular deviation had a reoperation rate of 4.7%, slightly less than comparison cases (OR 0.75, p=0.049, Table 3). Patients with claims for astigmatism had higher rates of both reoperation (OR 2.85) and abnormal binocularity after surgery (OR 7.15, p<=0.004, Tables 3 and 4). Horizontal surgery patients with abnormal binocularity before surgery or having 3 or 4 muscles operated had slightly lower rates of reoperation (OR 0.74 and 0.58, respectively), but had higher rates of postoperative abnormal binocularity (OR 7.15 and 1.40, respectively, Tables 3 and 4). Paralytic deviations had a rate of reoperation of 11.1%, which was significantly elevated in the univariate analysis only (p=0.01, Supplemental Table 7 at AJO.com).
Compared with the overall rate of postoperative abnormal binocularity of 12.7%, significantly elevated rates were seen in patients with esotropia (16.4%), and claims for hyperopia (25.4%) and interocular refractive asymmetry (33.9%, all p<=0.03, Table 4). Intermittent deviations had a rate of postoperative abnormal binocularity of 9.9%, which was lower than expected in the univariate analysis only (p=0.007, Supplemental Table 6 at AJO.com).
Botulinum toxin injection was used only for horizontal cases. Eight chiildren (0.1%) had incisional horizontal surgery, while 49 children (0.6%) had botulinum injection alone (Supplemental Table 5 at AJO.com). Of these 49 injected children, 22 (44.9%) had reoperation, 13 (26.5%) had abnormal binocularity, and 25 (51.0%) had either (or both) of these outcomes (Fig. 1, Table 3 and 4, Supplemental Table 5 at AJO.com). In contrast, following incisional surgery, 6.5% of children had reoperation, and 12.7% had abnormal binocularity (Supplemental Table 5 at AJO.com). As compared with fixed suture surgery, botulinum injection had an odds ratio for reoperation of 10.36 (95% CI 5.75 to 18.66) and an odds ratio for postoperative abnormal binocularity of 2.75 (95% CI 1.36 to 5.56, both p≤0.005, Tables 3 and 4).
The strabismus etiology was identified as paralytic in 20.4% of the cases involving botulinum toxin injection (10 of 49 cases). When presence or absence of a paralytic etiology was forced into the multivariable regression model, botulinum injection still had an odds ratio for reoperation of 9.77 (95% CI 5.40 to 17.67, p<0.001) and an odds ratio for postoperative abnormal binocularity of 2.78 (95% CI 1.37 to 5.65, p=0.005).
Isolated vertical muscle surgery
Of 1534 children having procedures exclusively on vertical muscles, 11.0% had a reoperation, 10.0% had abnormal binocularity, and 18.6% had either (or both) of these outcomes in the first postoperative year (Tables 5 and 6).
TABLE 5.
Predictors of Reoperation Following Vertical Strabismus Surgery.
| Clinical Factor | Reoperation (%) | Multivariable Analysis. | |
|---|---|---|---|
| Odds Ratio (95% CI) | p value. | ||
| Age 5 to 17 years. | 7.1% (68/958) | 1.00 (reference) | -- |
| ……2 to 4 years. | 14.6% (58/398) | 1.86 (1.22 to 2.82) | 0.004 |
| ……0 to 1 year. | 23.6% (42/178) | 4.41 (2.68 to 7.28) | <0.001 |
| Fixed suture. | 10.8% (163/1512) | 1.00 (reference) | -- |
| Adjustable suture. | 22.7% (5/22) | 2.51 (0.85 to 7.38) | 0.10 |
| Superior oblique surgery. | 20.6% (46/223) | 2.36 (1.61 to 3.46) | <0.001 |
| Total. | 11.0% (168/1534) | -- | -- |
CI = confidence interval.
TABLE 6.
Predictors of Abnormal Binocularity Following Vertical Strabismus Surgery.
| Clinical Factor | Abnormal Binocularity (%) |
Multivariable Analysis. | |
|---|---|---|---|
| Odds Ratio (95% CI) | p value. | ||
| Age 9 to 17 years. | 6.7% (35/524) | 1.00 (reference) | -- |
| ……2 to 8 years. | 11.1% (92/832) | 2.61 (1.68 to 4.07) | <0.001 |
| ……0 to 1 year. | 15.2% (27/178) | 4.25 (2.36 to 7.65) | <0.001 |
| Fixed suture. | 9.8% (148/1512) | 1.00 (reference) | -- |
| Adjustable suture. | 27.3% (6/22) | 3.46 (1.19 to 10.08) | 0.02 |
| Myopia, any type. | 27.6% (8/29) | 3.76 (1.42 to 9.99) | 0.008 |
| Abnormal binocularity, preoperative. | 29.5% (82/278) | 7.99 (5.53 to 11.56) | <0.001 |
| Total. | 10.0% (154/1534) | -- | -- |
CI = confidence interval.
Children under age 2 years had a reoperation in 23.6% of the cases (OR 4.41, p<0.001). Surgery involving the superior oblique muscle involved reoperation in 20.6% of cases, and was an independent risk factor for reoperation (OR 2.36, 95% CI 1.61 to 3.46, p<0.001). In a univariate analysis, surgery for Brown’s syndrome was associated with a reoperation rate of 23.0% (17 of 74 cases, p=0.002, Supplemental Tables 11 and 12 at AJO.com).
Adjustable suture surgery resulted in reoperation rate of 22.7% (5 of 22 cases, OR 2.51, 95% CI 0.85 to 7.38, p=0.10, Table 5). Adjustable suture surgery was associated more frequently with reoperation and/or abnormal binocularity (OR 2.61, 95% CI 1.02 to 6.69, p=0.045, Supplemental Table 13 at AJO.com). With exclusion of superior oblique surgery and fourth nerve palsy, adjustable sutures were not significantly associated with reoperation (OR 1.26, 95% CI 0.27 to 5.97, p=0.77, Supplemental Tables 14 and 15 at AJO.com) or the combined outcome of reoperation and/or abnormal binocularity (OR 2.11, p=0.20, Supplemental Tables 13 to 18 at AJO.com).
Myopia and preoperative abnormal binocularity were associated with a higher rate of abnormal binocularity following vertical muscle surgery (p<=0.008, Table 6). The number of claims involving a code for myopia was small, making this finding uncertain.
DISCUSSION
This study analyzed a large insurance database to determine reoperation rates and abnormal binocularity outcomes in the first year after pediatric strabismus surgery. Reoperation was defined as any subsequent strabismus procedure. Reoperation rates have been suggested as an important strabismus surgery outcome.4,25 Diagnoses of abnormal binocularity were identified from office visit claims, and included amblyopia, diplopia, and anomalous retinal correspondence.
The overall reoperation rate in the first year following incisional surgery in children (7.7%) is similar to our previous finding in adults (8.5%).4 The finding of higher rates of reoperation and abnormal binocularity in the youngest patients is not surprising. The association of abnormal binocularity with esotropia and hyperopia is also consistent with common clinical teachings.
The present study provided some insights on muscle selection for strabismus surgery. Operations on one or on two horizontal muscles had similar reoperation rates. Operating on more horizontal muscles (3 or 4) was associated with a lower reoperation rate than operating on 1 or 2 muscles. Therefore, a more aggressive surgical approach for large angle strabismus, in terms of number of muscles, might avoid future surgeries, but of course results in additional scarring and a more prolonged anesthesia time.
We previously observed in adults with exotropia a lower reoperation rate with unilateral surgery on two horizontal muscles compared with bilateral surgery on one horizontal muscle.4 Moreover, smaller randomized trials, primarily of children, with exotropia demonstrated a higher success rate with a unilateral recession-resection as compared with bilateral lateral rectus recessions.5,6 However, the present study in children with exotropia found no significant difference for the reoperation rate in unilateral two-muscle surgery (5.3%) as compared with bilateral one-muscle surgery (6.0%). Inter-study differences might be related to the surgical tables used by the single-surgeon studies, or the more specific selection criteria for these studies. Neither the present study, nor our previous analysis of adult strabismus,4 excluded cases of consecutive exotropia. The lack of a significant difference in the present study might be interpreted as support for the more common practice of bilateral one-muscle surgery. Surgeons should consider all available evidence when deciding on unilateral two-muscle versus bilateral one-muscle surgery for exotropia in children. This question is the subject of an ongoing randomized controlled clinical trial.26
In adults, we previously reported that adjustable sutures were associated with a lower reoperation rate for horizontal muscle surgery, but not for vertical muscle surgery.4 Several case series of adjustable suture strabismus surgery have included children and advocated the use of adjustable sutures in this age group.7–13 Most case series have been limited either exclusively7,8,11,12 or primarily10 to horizontal strabismus. The reported reoperation rate with adjustable sutures for strabismus in children has been 11% (5 of 45),10 13% (5 of 38),13 and 15% (13 of 89).8 In our study, the horizontal surgery reoperation rates were 7.6% with adjustable sutures and 6.4% with fixed sutures in the first postoperative year (p=0.53). In previous studies the followup period varied for each patient8,11,13 and was sometimes as short as six weeks,8,11 two months,13 or three months12 or was unstated.10 Only one study of pediatric adjustable suture strabismus surgery also presented a control group.12 This study stated that there was no significant difference between groups in reoperation rates, though the values were not presented. Stereopsis was absent in 35% in the adjustable suture group and 37% in the fixed suture group.12 Due to varying definitions and methods, it is difficult to compare these rates with our observation of claims for abnormal binocularity in 8.2% of patients following adjustable suture and in 12.8% after fixed suture horizontal surgery.
For vertical surgery, we also failed to demonstrate improvement in reoperation rates or abnormal binocularity outcomes with adjustable sutures. It is difficult to compare previous case series, which either excluded7,8,11,12 or included few,10,13 vertical strabismus patients.
To summarize the evidence on adjustable sutures in children, neither the present study, nor previous reports, demonstrate any significant improvement with adjustable sutures in rate of reoperation or in the combined outcome of reoperation and/or diagnosis of abnormal binocularity for either horizontal or vertical muscle surgery. Adjustable sutures require additional time for placement in the operating room. Traditional adjustable techniques often require additional general anesthesia in young children even if adjustment is not needed in order to tie the primary suture knot, remove a traction suture, and close the conjunctiva.10,12 Newer techniques require less extensive postoperative manipulation on patients not requiring adjustment.7,11,13 For some groups, adjustment may be performed in the operating room with intravenous propofol or laryngeal mask airway.11 Given the lack of evidence to justify the increased anesthesia time, we suggest that physicians should be selective in the use of adjustable sutures, particularly with surgical techniques which require general anesthesia in younger children even when adjustment is not needed.
Several small randomized trials of children with persistent deviations following incisional surgery for esotropia found similar motor and sensory outcomes between botulinum toxin injection and repeat incisional surgery.16,17 Our study differed in that we included children having a first surgery. We found that botulinum toxin injection was associated with a significantly higher reoperation rate (44.9%) than was fixed suture surgery (6.4%) for horizontal strabismus. On the other hand, anesthesia time with botulinum toxin injection is minimal. The procedure has been conducted for decades,15 and can be performed with anesthesia administered by mask, without the need for laryngeal mask airway or endotracheal intubation. Given the emerging information on cognitive deficits following general anesthesia in children under age four years,18,19 some families might choose a procedure which can avoid prolonged anesthesia in the first year in over half the patients. On the other hand, our finding of a higher rate of abnormal binocularity in the botulinum toxin group (26.5%) as compared with the fixed suture group (12.2%) suggests that persistent strabismus in the former group might be impairing visual development. If confirmed, these results would suggest that physicians be very selective in the use of botulinum injection during the visual development period. Botulinum injection might be best suited in patients felt to be at higher risk from prolonged anesthesia or intubation, or in those in whom the results of incisional surgery are felt to be less certain.
For vertical surgeries, Brown syndrome was associated with higher rates of reoperation in univariate analysis. In the multivariable analysis, this finding appeared to be due to the association of superior oblique surgery with reoperations. Superior oblique surgery, sometimes with a silicone spacer, might be difficult to titrate, and the use of a spacer can result in extrusion and other complications.27
The major strength of the study is the consistent application of the same metric in a large national database involving multiple providers. Reoperations could be identified even if a patient had the second surgery with a different provider.
However, the study had multiple limitations. Some reoperations might have been planned or staged, although very few contained a modifier to indicate such deliberate staging. Although a reoperation may indicate that neither the physician nor the family believed that the first surgery had attained the final treatment goals, reoperation rates may not reflect all dissatisfied families, and might therefore underestimate the rate of persistent strabismus. Some families might consider the surgery unsuccessful, but might forgo or delay reoperation. Both physicians and families might vary in their indications for repeat surgery. Ideally, a goal-directed analysis which considers alignment, diplopia, binocularity, and other factors, can be used to evaluate surgical success.28
We used multivariable analysis in an attempt to control for patient characteristics, such as age and known clinical factors. However, unidentified confounders could account for intergroup differences. In other words, it is possible that some baseline differences between the treatment groups were not reflected in the insurance claim data.
The analysis of insurance claim databases has additional limitations. The patient’s preoperative and postoperative angle of alignment is unknown. Information regarding diagnosis, comorbidities, and visual and neurologic status is unavailable or incomplete. Insurance claims can be inaccurate and incomplete, due to delayed and revised billing, and other factors. Reoperations for which payment is denied are not reflected in the database. Surgeons might have differed in the method of suture placement, and in the timing of postoperative adjustment.
In conclusion, one- and two-muscle horizontal strabismus surgery had similar reoperation rates, but both types of surgery had higher reoperation rates than observed for three- and four-muscle horizontal surgery. Unilateral two-muscle surgery had a reoperation rate similar to that of bilateral one-muscle surgery. Adjustable sutures were not associated with a lower rate of reoperation following strabismus surgery in children in this sample. Younger age, esotropia, and hyperopia were associated with abnormal binocularity after surgery. Botulinum toxin injection was associated with higher rates of reoperation and abnormal binocularity. Superior oblique surgery was associated with higher rates of reoperation. Although the study cannot provide definitive answers regarding pediatric strabismus procedures, we have illustrated an approach that could be extended to other insurance databases. Moreover, the data could help in performing the power calculations required in designing large randomized controlled trials.
Supplementary Material
Acknowledgements
Funding/Support: Partially supported by National Institutes of Health (Bethesda, MD) Center Core Grant P30EY014801 and Research to Prevent Blindness (New York, NY) Unrestricted Grant to the University of Miami.
Dr. Schwartz has received reimbursement for personal fees from Vindico, Alimera Sciences (Alpharetta, GA), and Bausch + Lomb (Madison, NJ).
Other Acknowledgments: None.
Biography

Christopher T. Leffler earned his MD at Harvard Medical School and his MPH at the Harvard School of Public Health. He served as a Diving Medical Officer in the U.S. Navy. He performed his ophthalmology residency and fellowship in pediatric ophthalmology at Virginia Commonwealth University, and is currently on faculty. He is the treasurer of the Cogan Ophthalmic History Society. His research interests are pediatric ophthalmology, strabismus, comprehensive ophthalmology, and ophthalmology history.
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
Supplemental Material available at AJO.com.
Financial Disclosures: Dr. Leffler, Dr. Vaziri, Dr. Cavuoto, Dr. McKeown, Dr. Kishor and Dr. Janot: No financial disclosures.
References
- 1.Webber AL, Wood J. Amblyopia: prevalence, natural history, functional effects and treatment. Clin Exp Optom. 2005;88(6):365–375. doi: 10.1111/j.1444-0938.2005.tb05102.x. [DOI] [PubMed] [Google Scholar]
- 2.Wang L, Nelson LB. One muscle strabismus surgery. Curr Opin Ophthalmol. 2010;21(5):335–340. doi: 10.1097/ICU.0b013e32833bd953. [DOI] [PubMed] [Google Scholar]
- 3.Vroman DT, Hutchinson AK, Saunders RA, Wilson ME. Two-muscle surgery for congenital esotropia: rate of reoperation in patients with small versus large angles of deviation. J AAPOS. 2000;4(5):267–270. doi: 10.1067/mpa.2000.106960. [DOI] [PubMed] [Google Scholar]
- 4.Leffler CT, Vaziri K, Cavuoto KM, McKeown CA, Schwartz SG, Kishor KS, Pariyadath A. Strabismus Surgery Reoperation Rates With Adjustable and Conventional Sutures. Am J Ophthalmol. 2015;160(2):385–390. doi: 10.1016/j.ajo.2015.05.014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Kushner BJ. An evaluation of the semiadjustable suture strabismus surgical procedure. J AAPOS. 2004;8(5):481–487. doi: 10.1016/j.jaapos.2004.07.005. [DOI] [PubMed] [Google Scholar]
- 6.Jeoung JW, Lee MJ, Hwang JM. Bilateral lateral rectus recession versus unilateral recess-resect procedure for exotropia with a dominant eye. Am J Ophthalmol. 2006;141(4):683–688. doi: 10.1016/j.ajo.2005.11.021. [DOI] [PubMed] [Google Scholar]
- 7.Parikh RK, Leffler CT. Loop suture technique for optional adjustment in strabismus surgery. Middle East Afr J Ophthalmol. 2013;20(3):225–228. doi: 10.4103/0974-9233.114797. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Chan TK, Rosenbaum AL, Hall L. The results of adjustable suture technique in paediatric strabismus surgery. Eye (Lond) 1999;13(Pt 4):567–570. doi: 10.1038/eye.1999.140. [DOI] [PubMed] [Google Scholar]
- 9.Coats DK. Ripcord adjustable suture technique for use in strabismus surgery. Arch Ophthalmol. 2001;119(9):1364–1367. doi: 10.1001/archopht.119.9.1364. [DOI] [PubMed] [Google Scholar]
- 10.Dawson E, Bentley C, Lee J. Adjustable squint surgery in children. Strabismus. 2001;9(4):221–224. doi: 10.1076/stra.9.4.221.694. [DOI] [PubMed] [Google Scholar]
- 11.Engel JM, Rousta ST. Adjustable sutures in children using a modified technique. J AAPOS. 2004;8(3):243–248. doi: 10.1016/j.jaapos.2004.01.007. [DOI] [PubMed] [Google Scholar]
- 12.Awadein A, Sharma M, Bazemore MG, Saeed HA, Guyton DL. Adjustable suture strabismus surgery in infants and children. J AAPOS. 2008;12(6):585–590. doi: 10.1016/j.jaapos.2008.06.005. [DOI] [PubMed] [Google Scholar]
- 13.Nihalani BR, Whitman MC, Salgado CM, Loudon SE, Hunter DG. Short tag noose technique for optional and late suture adjustment in strabismus surgery. Arch Ophthalmol. 2009;127(12):1584–1590. doi: 10.1001/archophthalmol.2009.305. [DOI] [PubMed] [Google Scholar]
- 14.Lueder GT, Galli M, Tychsen L, Yildirim C, Pegado V. Long-term results of botulinum toxin-augmented medial rectus recessions for large-angle infantile esotropia. Am J Ophthalmol. 2012;153(3):560–563. doi: 10.1016/j.ajo.2011.08.019. [DOI] [PubMed] [Google Scholar]
- 15.McNeer KW, Tucker MG, Spencer RF. Botulinum toxin management of essential infantile esotropia in children. Arch Ophthalmol. 1997;115(11):1411–1418. doi: 10.1001/archopht.1997.01100160581010. [DOI] [PubMed] [Google Scholar]
- 16.Tejedor J, Rodríguez JM. Retreatment of children after surgery for acquired esotropia: reoperation versus botulinum injection. Br J Ophthalmol. 1998;82(2):110–114. doi: 10.1136/bjo.82.2.110. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Tejedor J, Rodríguez JM. Early retreatment of infantile esotropia: comparison of reoperation and botulinum toxin. Br J Ophthalmol. 1999;83(7):783–787. doi: 10.1136/bjo.83.7.783. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Backeljauw B, Holland SK, Altaye M, Loepke AW. Cognition and brain structure following early childhood surgery with anesthesia. Pediatrics. 2015;136(1):e1–e12. doi: 10.1542/peds.2014-3526. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Cavuoto KM, Rodriguez LI, Tutiven J, Chang TC. General anesthesia in the pediatric population. Curr Opin Ophthalmol. 2014;25(5):411–416. doi: 10.1097/ICU.0000000000000088. [DOI] [PubMed] [Google Scholar]
- 20.Spencer RF, McNeer KW. Botulinum toxin paralysis of adult monkey extraocular muscle. Structural alterations in orbital, singly innervated muscle fibers. Arch Ophthalmol. 1987;105(12):1703–1711. doi: 10.1001/archopht.1987.01060120101035. [DOI] [PubMed] [Google Scholar]
- 21.Esotropia Treatment with Botulinum Toxin-A Injection Data Collection. [Accessed 8/11/2015];Pediatric Eye Disease Investigator Group. Available at http://pedig.jaeb.org/Studies.aspx?RecID=207. [Google Scholar]
- 22.Danielson E. White Paper: Health Research Data for the Real World: The MarketScan® Databases. [Accessed 11/11/2014];Truven Health Analytics. 2014 Jan; Available at http://truvenhealth.com/Portals/0/Users/031/31/31/PH_13434%200314_MarketScan_WP_web.pdf. [Google Scholar]
- 23.Vaziri K, Schwartz SG, Kishor KS, Fortun JA, Moshfeghi DM, Moshfeghi AA, Flynn HW., Jr Incidence of postoperative suprachoroidal hemorrhage after glaucoma filtration surgeries in the United States. Clin Ophthalmol. 2015;9:579–584. doi: 10.2147/OPTH.S78359. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Gregori NZ, Flynn HW, Jr, Schwartz SG, Rosenfeld PJ, Vaziri K, Moshfeghi AA, Fortun JA, Kovach JL, Dubovy SR, Albini TA, Davis JL, Berrocal AM, Smiddy WE. Current Infectious Endophthalmitis Rates After Intravitreal Injections of Anti-Vascular Endothelial Growth Factor Agents and Outcomes of Treatment. Ophthalmic Surg Lasers Imaging Retina. 2015;46(6):643–648. doi: 10.3928/23258160-20150610-08. [DOI] [PubMed] [Google Scholar]
- 25.Haridas A, Sundaram V. Adjustable versus non-adjustable sutures for strabismus. Cochrane Database Syst Rev. 2013 Jul 2;7 doi: 10.1002/14651858.CD004240.pub3. [DOI] [PubMed] [Google Scholar]
- 26.A Randomized Trial of Bilateral Lateral Rectus Recession versus Unilateral Lateral Rectus Recession with Medial Rectus Resection for Intermittent Exotropia - Extended Follow Up. [Accessed 10/13/2015];Pediatric Eye Disease Investigator Group. Available at: http://pedig.jaeb.org/Studies.aspx?RecID=336. [Google Scholar]
- 27.Wright KW. Superior oblique silicone expander for Brown syndrome and superior oblique overaction. J Pediatric Ophthalmol Strabismus. 1990;28(2):101–107. doi: 10.3928/0191-3913-19910301-11. [DOI] [PubMed] [Google Scholar]
- 28.Ehrenberg M, Nihalani BR, Melvin P, Cain CE, Hunter DG, Dagi LR. Goal-determined metrics to assess outcomes of esotropia surgery. J AAPOS. 2014;18(3):211–216. doi: 10.1016/j.jaapos.2013.12.016. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.