Abstract
To develop the next generation of translational investigators, New York University School of Medicine (NYUSOM) and the NYU‐NYC Health and Hospitals Corporation Clinical and Translational Science Institute (NYU‐HHC CTSI) developed the Master's of Science in Clinical Investigation dual‐degree (MD/MSCI) program. This 5‐year program dedicates 1 year to coursework and biomedical research, followed by a medical school/research overlap year, to prepare students for academic research careers. This paper details the MD/MSCI program's curriculum and approach to mentorship, describes the research/professional interests of students, and reports student productivity. In the first 4 years of the program (2010–2014) 20 students were matriculated; 7 (35%) were women, and 12 (60%) research projects were in surgical specialties. To date, 14 students have applied to residency, and half pursued surgical residency programs. Our students have produced 68 accepted abstracts, 15 abstracts in submission, 38 accepted papers, and 24 papers in submission. Despite the time‐limited nature of this program, additional training in research design and implementation has promoted a high level of productivity. We conclude that dual‐degree training in medicine and translational research is feasible for medical students and allows for meaningful participation in valuable projects. Follow‐up is warranted to evaluate the academic trajectory of these students.
Keywords: medical student education, dual degree, translational research, MD/MSCI
Background: Educating Physician Scientists
The National Institutes of Health (NIH) funds a consortium of academic medical centers across the United States to promote translational research and to educate the next generation of translational researchers. The National Center for Advancing Translational Science (NCATS) launched the Clinical and Translational Science Award (CTSA) program in 2006 to develop and support a national workforce that efficiently accelerates discoveries improving patient care and public health.1 In concert with this effort, US medical schools and their affiliated Clinical and Translational Science Institutes (CTSIs) have begun to offer formal programs teaching translational research methodologies to medical students interested in research careers. The New York University–New York City Health and Hospitals Clinical and Translational Science Institute (NYU–HHC CTSI) at the NYU School of Medicine (NYUSOM) is one such program that aims to effectuate training at the earliest career stage.
In 2010, we implemented a dual‐degree program allowing medical students to earn both MD and Master's of Science in Clinical Investigation degrees (MD/MSCI) after 5 years of study. Inspired by the NCATS initiative and the K30 award program, the MD/MSCI program teaches medical students the skills to critically interpret research, to apply appropriate study design methodology, and to carry out collaborative research projects. By going beyond the classic medical school curriculum, the MD/MSCI program aims to prepare medical students for research‐related careers by combining formal didactic coursework, focused professional mentoring, and the opportunity to perform patient‐centered translational research. The goals of our MD/MSCI program are to encourage medical students to explore and define their interest in clinical/translational research, while building their skills and enhancing their confidence in becoming physician‐scientists.
All 62 CTSIs offer formal postdoctoral training programs, 33 of which offer clinical research master's degree programs to medical students.1 Although program descriptions and outcomes data have been published for other common dual‐degree programs (MD/PhD, MD/MPH, MD/MBA), published data regarding MSCI programs are sparse, particularly in the contexts of medical student MD/MSCI training.2, 3, 4, 5, 6, 7, 8 Experience sharing is important for designing new programs, improving established programs, and identifying solutions to structural challenges. Here we describe our MD/MSCI program to promote similar program development and to encourage an ongoing dialogue about educating the next generation of translational researchers.
Historical perspective on medical student research education
According to the Association of American Medical Colleges (AAMC), more than half of students (57.1%) in the Class of 2013 nationwide were involved in research prior to medical school.9 Upon graduation, more than two‐thirds (68.2%) of respondents participated in research as medical students.10 However, less than half expressed confidence in their skills to critically evaluate the medical literature, and a smaller percentage planned to be significantly involved in research during their careers.10 Medical students may participate in research and other “résumé‐building” activities during medical school in hopes of securing highly coveted residency training positions. According to the 2014 National Resident Match Program (NRMP) outcomes data, students who successfully matched in the most competitive residencies (plastic surgery, neurosurgery, orthopedic surgery, dermatology) had the greatest number of research experiences, abstracts, and publications.11
The fact that many medical students do not continue to participate in research beyond their schooling may reflect a perception that they are not suited to be researchers. Only a third of Canadian senior medical students studied in a survey reported a good understanding of research methods,12 raising the possibility that the lack of knowledge about how to design, perform, and carry out research may be an important contributor to the observed drop‐off in interest. Focused coursework emphasizing patient‐centered translational research could therefore help sustain and reinvigorate medical student interest in research.
Incorporating research experiences and additional research methods coursework into medical education may improve interests and attitudes toward academic medicine.13, 14, 15, 16 In a cross‐sectional study, students who recently completed a research methods course scored highest in terms of knowledge and attitudes towards research.6 Although a causal relationship between course offerings and student attitudes cannot be proven directly, dedicated training in clinical research likely plays an important role in sustaining student interest.
Performing research in medical school
Dismantling barriers to performing clinical research may encourage medical students to incorporate research into their careers. Four such barriers are time constraints, finding a supportive research mentor, lack of formal training in research methods, and concerns regarding acknowledgement/recognition for their contributions (Figure 1 A).12, 17 In designing the NYUSOM MD/MSCI program with goals congruent with those of NCATS, we developed a dynamic and pragmatic educational program to further encourage medical students to participate in research, and ultimately pursue careers in clinical and translational research. We examined our dual‐degree students' ability to conduct successful research at this early career stage. We also assessed whether dual‐degree students were more likely to apply to competitive residency programs, such as the surgical specialties, which typically expect applicants to publish or present research as medical students.
Figure 1.
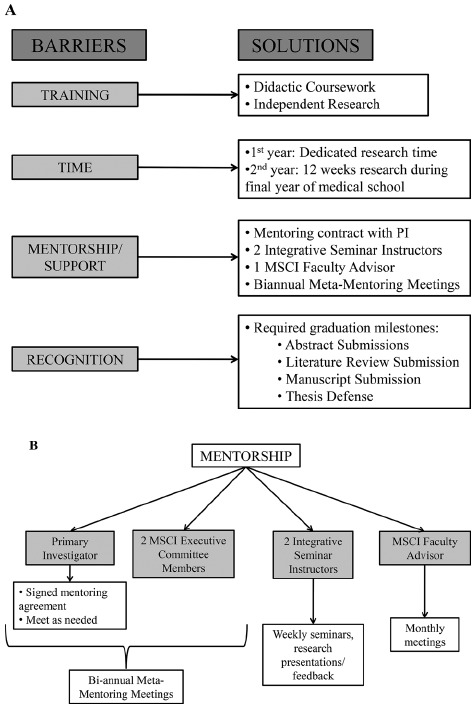
(A) Barriers for physician‐scientists in training and NYUSOM MD/MSCI program solutions.11, 17 (B) NYUSOM MD/MSCI mentorship resources.
Overview of NYUSOM MD/MSCI Program
Overcoming barriers
The NYUSOM MD/MSCI program is accredited by the New York State Department of Education, and addresses each of the aforementioned barriers by providing students with formal didactic coursework; protected, for‐credit research time; multifaceted mentoring from their primary investigator and NYU CTSI faculty; and longitudinal guidance on career development. To offset the additional financial barrier involved with clinical research training, the master's degree is heavily subsidized and students do not pay medical school tuition during the first year of the MSCI arm.
Eligibility
Students are selected for the MD/MSCI program by a competitive application process. Applicants must be matriculated in good academic standing at NYUSOM. The application includes a personal statement, research proposal, curriculum vita, as well as letters of recommendation. Prospective dual‐degree students are required to identify a research mentor and “take ownership” of a defined research project. The MSCI Executive Committee critically reviews the applications and admission decisions are made by consensus. Once accepted, the student and mentor sign a mentorship agreement that delineates expectations prior to the start of the program. The first cohort of NYU MD/MSCI dual‐degree students graduated in May, 2012.
Curriculum
After completing the third year of medical school, dual‐degree students dedicate an academic year to their MSCI didactic coursework and perform mentored research. During each semester of the MSCI arm, there is a mandatory Integrative Research Seminar, which meets under the direction of a senior faculty member, and serves as a forum for presenting works in progress, brainstorming, troubleshooting, and exchanging ideas in a supportive, small group setting. The full list of courses offered, class type, evaluations, and credit hours is presented in Table 1.
Table 1.
NYUSOM MD/MSCI curriculum
| Term | Course | Credit hours | Class type | Evaluation |
|---|---|---|---|---|
| Summer year 1 | Clinical Research Methods | 3 | S | A, P, Pr, Pa |
| Fall year 1 | Introduction to Biostatistics | 3 | S, CL | A, P, Q, E |
| Medical Informatics | 3 | S | A, P, Pr, Pa | |
| Advanced Epidemiology (Selective) | 3 | S, CL | A, P, Pr, Pa | |
| Drug Development in a New Era (Selective) | 3 | S | A, P, Pa | |
| Integrative Seminar | 1 | S, JC, RD | A, P, RPr | |
| Mentored Independent Research | 1 | |||
| Spring year 1 | Scientific Integrity and the Responsible Conduct of Research | 0 | S | E |
| Clinical Trials Design | 4 | S, CL | A, P, Q, E | |
| Biotechnology Industry, Structure & Strategy (Optional) | 3 | S | A, P, Pr, Pa | |
| Molecular Signaling and Drug Development (Optional) | 4 | S | A, P, Pr, Pa | |
| Biomolecular Medicine | 3 | S | A, P, Pa | |
| Integrative Seminar | 1 | S, JC, RD | A, P, RPr | |
| Mentored Independent Research | 3 | |||
| Fall year 2 | Integrative Seminar | 1 | S, JC, RD | A, P, RPr |
| Mentored Independent Research | 3 | |||
| Spring year 2 | Integrative Seminar | 1 | S, JC, RD | A, P, RPr |
| Mentored Independent Research | 5 |
S = seminar class; CL = computer lab; JC = journal club; RPr = research presentation; A = attendance; P = participation; Pa = paper; Pr = presentation; Q = quiz; E = examination.
After completing their dedicated research year, MD/MSCI candidates return to clinical rotations in their final (fifth) year of study, during which they commit a minimum of 12 weeks to the completion of their MSCI thesis, in addition to regular attendance at their weekly integrative seminars. Additional time may be spent at the students' initiative as needed to complete their research and milestone requirements.
Deliverables and milestones
Prespecified deliverables and milestones are required for graduation. During their first year in the MSCI arm (year 4 of MD/MSCI dual‐degree program), students are required to submit their human subject research protocol to the NYU‐Langone Medical Center Institutional Review Board (IRB) and obtain IRB approval, as well as complete the Collaborative Institutional Training Initiative (CITI) tutorial in human subject research. To reinforce knowledge in their field of study, students are expected to write a curated literature review paper related to their research focus. Students are also expected to effectively contribute to their research group's projects to warrant inclusion in an abstract submission to a regional/national meeting. During the second year of the MSCI arm (fifth and final year of MD/MSCI dual‐degree program), students are required to submit a lead‐author abstract to a regional/national meeting, prepare an original manuscript for publication, write a research report (master's thesis) documenting and reflecting on all research activities performed during the program, and submit an academic portfolio. All students are required to defend their thesis in a formal oral presentation to the NYU CTSI/MSCI community, including to faculty and other trainees (Table 2).
Table 2.
NYUSOM MD/MSCI deliverables/milestones and academic productivity, matriculated students 2010–2013
| Milestones | Deliverables | Outcomes |
|---|---|---|
|
Abstracts accepted | 68 |
| Abstracts in submission | 15 | |
| Papers accepted | 38 | |
| Papers in submission | 24 | |
| Awards | 9 |
Each semester, students and their research mentors participate in academic mentoring meetings. The formal mentoring meetings bring together the student, the primary mentor, and two MSCI Mentoring Committee members to review learning goals, curricular options (electives), and research progress and to troubleshoot programmatic and/or productivity challenges. These formal biannual mentoring meetings are supplemented with monthly group meetings led by a dedicated faculty advisor to discuss any day‐to‐day challenges the students are facing with their research or coursework during the program (Figure 1 B).
Demographics
We compiled and reviewed student demographics including age, gender, research field, and desired postgraduate (residency) specialization. We defined urology, neurosurgery, otolaryngology, ophthalmology, plastic surgery and general surgery as “surgical specialties.” Internal medicine, pediatrics, and primary care were defined as “medical specialties.” All other research or residency programs, such as radiology, anesthesia, dermatology or radiation oncology, were categorized as “other.”
To date, 20 students have enrolled in the MD/MSCI dual‐degree program (2010–2014), out of a total of 648 medical students at the NYUSOM in the same time period (162 students per medical school class); there is currently a 0% attrition rate. At the time of entry into the MD/MSCI dual‐degree program, the students' ages ranged from 24 to 27 years, consistent with an average age range of 21–24 years for students at entry to our medical school, which is slightly younger than the average age of 24 at entry into American medical schools overall.18 Seven, or approximately one‐third (35.0%) of the MD/MSCI dual‐degree students were women, in comparison to 44.7% of the current first year NYUSOM class (Figure 2 A).19 The majority of student research topics (12, or 60.0%) were in surgical specialties including urology, neurosurgery, otolaryngology, and plastic surgery (Figure 2 B). Of the 14 dual‐degree students who have already applied for residency training, half applied into surgical fields, with only two students applying to either medicine or pediatrics (Figure 2 C). In contrast, of the 48 trainees who have participated in our 2‐year postdoctoral MSCI program, 34 (70.8%) work in medical and/or medical subspecialty fields, and 32 (66.7%) are women.
Figure 2.
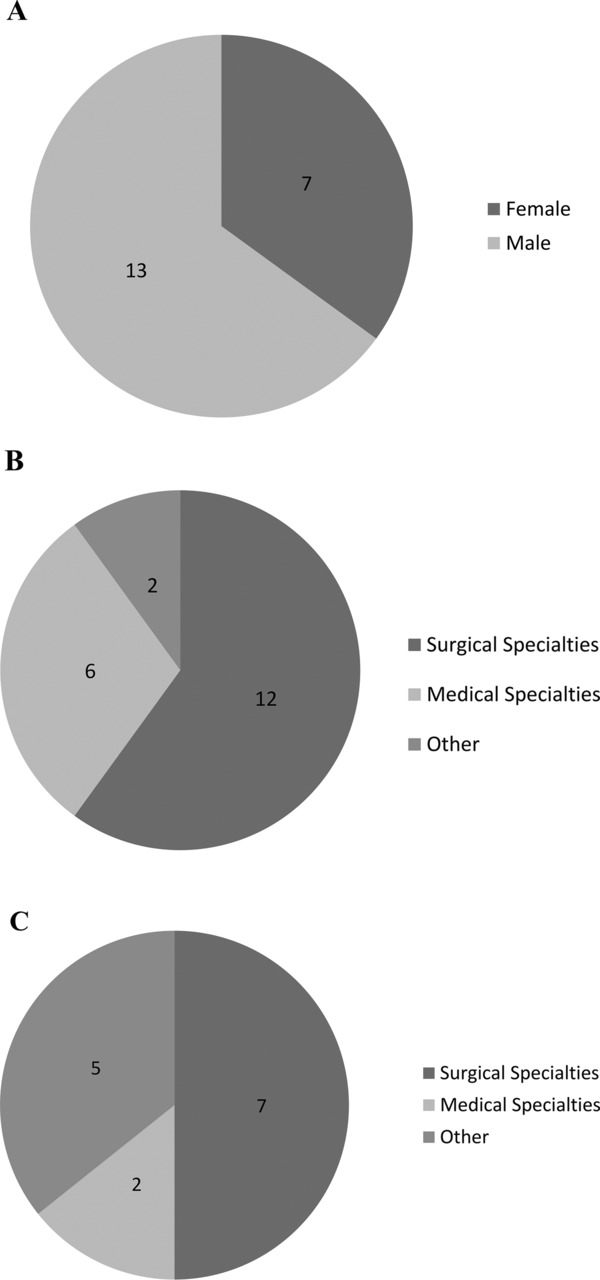
(A) Student demographics: gender 2010–2014. (B) Student demographics: research area of interest 2010–2014. Surgical specialties: neurosurgery, urology, otolaryngology, ophthalmology, plastic surgery, general surgery. Medical specialties: medicine, pediatrics. Other: radiology, dermatology. (C) Student demographics: residency of interest 2010–2013. Surgical specialties: neurosurgery, urology, otolaryngology. Medical Specialties: medicine, pediatrics. Other: radiology, anesthesiology, radiation oncology.
Productivity
We measured student productivity by the number of manuscripts submitted as an author or coauthor as well as the number accepted for peer‐reviewed publication. We also tabulated the number of abstracts submitted to regional meetings and national conferences. The 14 students who were matriculated in our program between 2010 and 2013 have, as of this writing, a total of 68 accepted abstracts, with 15 additional abstracts currently in submission. Furthermore, the students were listed as authors on 38 accepted papers, with 24 additional papers in submission. Six students have received a total of nine awards for their research activities (Table 2). Student feedback for the MSCI program (in including both postdoctoral and dual‐degree students) has been highly favorable. The postprogram survey is anonymous and thus we are not able to parse out MD/MSCI dual‐degree student responses from the rest of the MSCI class. We plan to substratify responses by type of student on future surveys.
Discussion and Dialogue
The NYUSOM NYU–HHC CTSI MD/MSCI dual‐degree program is a comprehensive translational research‐training program for medical students that encompasses didactic coursework, strong mentorship, and mentored research, and provides the necessary structure and environment for medical students to acquire a translational research skill set. Students have been highly productive, with numerous peer‐reviewed publications, abstracts, and awards to their credit.
The majority of students participating in the NYUSOM MD/MSCI dual‐degree program conducted research in a surgical specialty and then applied to residency programs in those highly competitive fields. Surgical residency programs often incorporate 1–2 years of mandatory research activities, and students who complete the MD/MSCI program may be more desirable and prepared applicants. These students may be more interested in the MD/MSCI dual‐degree program than their “medical” classmates because of the “hidden curriculum” of surgical training described by Hill et al. The “hidden curriculum” represents students' perceived expectations for matching into competitive surgical training programs, including research.20 Further supporting this observation, only two dual‐degree medical students to date have applied to residency in internal medicine or pediatrics, which do not generally mandate dedicated research time during residency. Such individuals may seek research training later in their careers, demonstrated by the fact that the majority of our postdoctoral level master's trainees are from medical subspecialties. Thus, institutions seeking to develop dual‐degree programs should be aware that their students' needs, vis‐à‐vis training, may vary with both their long‐term interests and with the inherent arcs of different possible careers. From this perspective, the MD/MSCI dual‐degree program has the potential to fulfill a “hidden” gap in the classic medical curriculum for students interested in surgical specialties.
Many medical students and physicians may benefit more from less intensive programs that allow trainees to maintain an ongoing interest and momentum in research and investigation. At our institution, we are currently experimenting with short‐form research training programs for our non–dual‐degree medical students.21 The impact of these experiences in encouraging trainees to consider investigational careers in the future remains to be determined.
Another finding is that more men than women participated in our MD/MSCI dual‐degree program. This may reflect the fact that women are less likely to pursue postdoctoral training in disproportionally male‐dominated fields, such as surgical specialties.22, 23 Moreover, this could reflect the gender gap in the academic sciences, a phenomena which impacts women at all career stages.24 This further emphasizes the need to attract, promote and support women to academic medicine. Once again, the life stages of our trainees demand consideration: among our postdoctoral level trainees in the same period, the majority of trainees have been women.
Limitations of this study include the lack the following comparison groups: MD‐degree medical students who took a research‐year at the NYUSOM, and MD/MSCI dual‐degree students at other CTSA programs. Furthermore, this study is descriptive and not predictive of research productivity and future career trajectories. Continued research is necessary to further assess the long‐term impacts of the MD/MSCI program.
Lessons learned from the MD/MSCI program
Clinical and translational research training programs for medical students, such as the NYUSOM MD/MSCI dual‐degree program, provide students with positive and productive experiences in translational research and represent the first step in creating a national translational workforce as envisioned by NCATS. Along with other CTSI programs across the country, our program aims to develop successful physician‐scientists in the earliest stages of their education and careers. Our principal goal for these physician‐scientists is for them to become adept at critical analysis, design, and implementation of translational research in hopes of positively affecting patient care and public health systems. Our MD/MSCI dual‐degree program described here can serve as a model for other like‐minded medical educational programs. In promoting these future endeavors, our program evaluation also underscores the need to improve the diversity of the MD/MSCI student body to include more women and students interested in medical specialties and primary care. Evaluation of the research impact and academic trajectory of these dual‐degree students is warranted.
Funding/Support
Michael Pillinger, MD, Claudia S. Plottel, MD, MSc, Bruce N. Cronstein, MD, Judith S. Hochman, MD, MA, and Gabrielle Gold‐von Simson, MD, MSc are supported in part by the NYU CTSA grant UL1TR000038 from the National Center for the Advancement of Translational Science (NCATS), NIH. Gabrielle Gold‐von Simson, MD, MSc is the principal investigator of the Drug Development Educational Program grant R25DK092170‐02 from the National Institute for Diabetes and Digestive and Kidney Diseases (NIDDK), NIH.
Disclosures
No conflict of interest, financial or otherwise, exists among the authors of this manuscript. Those persons listed as authors contributed for authorship and all qualified authors are listed.
Ethical Approval
This is a descriptive study of an existing educational program/curriculum which is exempt from continuous IRB review per 45 CFR 46.101(b).
Previous Presentations
Poster presentation entitled “Educating Translational Physician‐Scientists: The NYU School of Medicine MD/MSc dual‐degree in Translational Investigation” at the Translational Science Meeting, Washington DC, 2013.
Acknowledgment
We would like to thank Dr. Lynn Buckvar‐Keltz, Associate Dean for Student Affairs at the NYU School of Medicine.
References
- 1. Clinical & Translational Science Awards Portal . Available at: https://www.ctsacentral.org/. Accessed July 10, 2014.
- 2. Jeffe DB, Andriole DA, Wathington HD, Tai RH. Educational outcomes for students enrolled in MD‐PhD programs at medical school matriculation, 1995–2000: a national cohort study. Acad Med. 2014; 89(1): 84–93. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. Sherrill WW. Dual‐degree MD‐MBA students: a look at the future of medical leadership. Acad Med. 2000; 75(10 Suppl): S37–S39. [DOI] [PubMed] [Google Scholar]
- 4. Cooper SP, McCormick JB, Chappell CL, Clare N, Vela L, Walker T, Smith MA, Heilbrun LP, Stark DL, Schoenly R, et al. Texas needs physicians trained in public health: a new 4‐year integrated MD/MPH degree program. Tex Med. 2010; 106(4): e1. [PubMed] [Google Scholar]
- 5. Crites GE, Ebert JR, Schuster RJ, Shuster RJ. Beyond the dual degree: development of a five‐year program in leadership for medical undergraduates. Acad Med. 2008; 83(1): 52–58. [DOI] [PubMed] [Google Scholar]
- 6. Martina CA, Mutrie A, Ward D, Lewis V. A sustainable course in research mentoring. Clin Transl Sci. 2014; 7(5): 413–419. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Knapke JM, Haynes EN, Kuhnell P, Tsevat J. NIH grant awards as a metric of clinical and translational research training effectiveness. Clin Transl Sci. 2014; 8(1): 52–56. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. Knapke JM, Tsevat J, Succop PA, Djawe K, Kuhnell P, Haynes EN. Publication track records as a metric of clinical research training effectiveness. Clin Transl Sci. 2013; 6(6): 458–462. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Matriculating Student Questionnaire 2011, Association of American Medical Colleges; 2011.
- 10. Graduation Questionnaire 2013, Association of American Medical Colleges; 2013.
- 11. National Resident Matching Program, Charting Outcomes in the Match, 2014 Washington, DC; 2014.
- 12. Siemens DR, Punnen S, Wong J, Kanji N. A survey on the attitudes towards research in medical school. BMC Med Educ. 2010; 10: 4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. Hren D, Luki´c IK, Marusi´c A, Vodopivec I, Vujaklija A, Hrabak M, Marusi´c M. Teaching research methodology in medical schools: students' attitudes towards and knowledge about science. Med Educ. 2004; 38(1): 81–86. [DOI] [PubMed] [Google Scholar]
- 14. Halpain MC, Jeste D V, Trinidad GI, Wetherell JL, Lebowitz BD. Intensive short‐term research training for undergraduate, graduate, and medical students: early experience with a new national‐level approach in geriatric mental health. Acad Psychiatry. 2005; 29(1): 58–65. [DOI] [PubMed] [Google Scholar]
- 15. Black ML, Curran MC, Golshan S, Daly R, Depp C, Kelly C, Jeste DV. Summer research training for medical students: impact on research self‐efficacy. Clin Transl Sci. 2013; 6(6): 487–489. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16. Vujaklija A, Hren D, Sambunjak D, Vodopivec I, Ivanis A, Marusi´c A, Marusi´c M. Can teaching research methodology influence students' attitude toward science? Cohort study and nonrandomized trial in a single medical school. J Investig Med. 2010; 58(2): 282–286. [DOI] [PubMed] [Google Scholar]
- 17. Salgueira A, Costa P, Gonçalves M, Magalhães E, Costa MJ. Individual characteristics and student's engagement in scientific research: a cross‐sectional study. BMC Med Educ. 2012; 12: 95. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18. Abramson SB, Jacob D, Rosenfeld M, Buckvar‐Keltz L, Harnik V, Francois F, Rivera R, Hopkins MA, Triola M, Grossman RI. A 3‐year M.D.–accelerating careers, diminishing debt. N Engl J Med. 2013; 369: 1085–1087. [DOI] [PubMed] [Google Scholar]
- 19. Magyar R. NYU School of Medicine Welcomes an Eclectic Class of 2018. 2014. Available at: http://communications.med.nyu.edu/media‐relations/news/nyu‐school‐medicine‐welcomes‐eclectic‐class‐2018. Accessed August 28, 2015.
- 20. Hill E, Bowman K, Stalmeijer R, Hart J. You've got to know the rules to play the game: how medical students negotiate the hidden curriculum of surgical careers. Med Educ. 2014; 48(9): 884–894. [DOI] [PubMed] [Google Scholar]
- 21. Plottel CS, Aphinyanaphongs Y, Shao Y, Micoli KJ, Fang Y, Goldberg JD, Galeano CR, Stangel JH, Chavis‐Keeling D, Hochman JS, et al. Designing and implementing INTREPID, an intensive program in translational research methodologies for new investigators. Clin Transl Sci. 2014; 7(6): 493–499. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22. Dyrbye LN, Shanafelt TD, Balch CM, Satele D, Sloan J, Freischlag J. Relationship between work‐home conflicts and burnout among American surgeons: a comparison by sex. Arch Surg. 2011; 146(2): 211–217. [DOI] [PubMed] [Google Scholar]
- 23. Weiss A, Lee KC, Tapia V, et al. Equity in surgical leadership for women: more work to do. Am J Surg. 2014; 208(3): 494–498. [DOI] [PubMed] [Google Scholar]
- 24. Moss‐Racusin CA, Dovidio JF, Brescoll VL, Graham MJ, Handelsman J. Science faculty's subtle gender biases favor male students. Proc Natl Acad Sci U S A. 2012; 109(41): 16474–16479. [DOI] [PMC free article] [PubMed] [Google Scholar]


