Abstract
Objective
To describe family-reported health service needs of children with medical complexity, and to assess which needs are more often addressed in a tertiary care center-based structured clinical program for children with medical complexity.
Study design
Mailed survey to families of children with medical complexity enrolled in a structured-care program providing care coordination and oversight at one of three children’s hospitals. Outcomes included receipt of 14 specific health service needs. Paired t-tests compared unmet health care needs prior to and following program enrollment.
Results
441 of 968 (46%) surveys were returned and analyzed. Respondents reported their children had a mean age of 7 (standard deviation 5) years. A majority of respondents reported the child had developmental delay (79%) and feeding difficulties (64%). Of respondents, 56% regarded the primary care provider as the primary point of contact for medical issues. Respondents reported an increase in meeting all fourteen health services needs after enrollment in a tertiary care center-based structured clinical program, including primary care checkups (82% v 96%), therapies (78% v 91%), mental health care (34% v 58%), respite care (56% v 75%), and referrals (51% v 83%) (all p<.001).
Conclusions
Tertiary care center-based structured clinical care programs for children with medical complexity may address and fulfill a broad range of health service needs that are not met in the primary care setting.
Keywords: medical home, children with special health care needs, children with medical complexity
Children with special health care needs (CSHCN) “have or are at increased risk for a chronic physical, developmental, behavioral, or emotional condition and require health and related services of a type or amount beyond that required by children generally.”(1) Of specific interest among CSHCN are children with medical complexity (CMC): the most medically fragile and the highest resource utilizers of all CSHCN due to multiple subspecialty care needs, functional limitations, and medical technology needs.(2) The prevalence of CMC is rising in large part due to increasing premature and low weight births, advances in surgical and intensive care, and increased use of medical technology to maintain health and functioning.(3)
CMC require a high level of health care and supportive services that families report are frequently not met, such as preventive care, oral health care, access to specialty care, mental health care, transition of care services, and care coordination.(4–7) Almost half (48.8%) of families of CMC report ≥1 unmet health care need, and 5.4% report ≥5 unmet needs.(8) The high level of unmet needs occurs across all races/ethnicities, incomes, or insurance types of the child.(9) Families of CMC report inadequate access to the pediatric subspecialty and mental health care providers that could mitigate the high level of unmet health care needs.(10–14)
Community-based primary care physicians (PCPs) report limited capacity to care for CMC.(15, 16) Dedicated tertiary care center-based structured clinical programs for CMC at children’s hospitals have emerged to meet the need for care management and coordination. These programs typically provide dedicated care coordinators, co-location of specialists, or a multidisciplinary team that address growth and nutrition, medical technology management, and access to appropriate care.(2, 17–22) Their location in tertiary care centers where CMC frequently access services(2, 18, 20) may enable the necessary intensive and effective care coordination and case management.(17, 19–21) Cost savings of the programs due to reduction of preventable inpatient and emergency department (ED) visits have been described.(20, 22–24) Specific health service needs of families of CMC who attend such programs, however, have not previously been described, particularly after enrollment in these programs.
The objectives of this study were to describe the family-reported health service needs of children with medical complexity enrolled in a tertiary-based structured clinical care program, and t o determine the extent to which needs are addressed by programs for CMC.
Methods
This study is a multisite survey of families of children currently enrolled in structured, comprehensive care programs for CMC at three tertiary care children’s hospitals: Medical Home Clinic, Arkansas Children’s Hospital; Special Needs Program, Children’s Hospital of Wisconsin; and Complex Care Service, Boston Children’s Hospital. The programs were identified as relatively mature structured complex care programs, with each program in existence for at least eight years prior to the survey. Each program is consultative, with all patients continuing to have a local PCP. Common enrollment criteria included the presence of multiple chronic conditions requiring care from multiple specialists. The study sample was limited to children who were currently enrolled in one of the programs.
Study enrollment criteria included all families of CMC who were currently enrolled in each clinical program and had been enrolled in the prior five years. Prior analyses from on the National Survey of Children with Special Health Care Needs (NS-CSHCN) suggest that almost 50% of CMC have at least one unmet medical service need, and 20% of non-CMC have ≥1 unmet medical service need.(9) Based on a power of .8 and a two-tailed alpha of .05, assuming equal sample sizes, a difference of ≥1 unmet needs of 50% versus 35% would require a total sample size of 366. We assumed a 50% return rate.
The study protocol was approved separately by Institutional Review Boards (IRB) at the University of Arkansas for Medical Sciences, Children’s Hospital of Wisconsin, and Boston Children’s Hospital. Following the individual requirements of the IRBs, the surveys for children at Arkansas and Wisconsin were mailed from and returned to research staff at Arkansas. Surveys for Boston Children’s Hospital were mailed from and returned directly to Boston, with de-identified data shared to study investigators based in Arkansas. Prior to mailing, the survey was piloted with five families at Arkansas Children’s Hospital, with revisions made from feedback on clarity and readability. We verified that the survey took less than ten minutes to complete. Surveys were mailed out with reminders to encourage survey completion using a modified Dillman approach.(25) The initial survey was mailed with a $1 bill as an incentive to complete the survey.
The survey content was developed by adapting questions used in the 2009–10 NS-CSHCN. This survey provides prevalence estimates of CSHCN and a description of services utilized by CSHCN and their families, as well as detailed aspects of health care utilization, health status, and family burden.(26) The NS-CSHCN is conducted annually by the National Center for Health Statistics and uses a computer-assisted telephone interview on a national random population sample.(26) The survey was administered in English only. The survey had two mai outcomes: primary care and met/unmet needs. Families were asked whether they received specific services by the primary care provider in the prior twelve months. Specific services included receipt of well child care; chronic illness management, such as care planning and referrals; and nutritional support. Families were asked about fourteen specific health service needs (Figure; available at www.jpeds.com) that were adapted from the NS-CSHCN for a written, paper survey format. For each health service need, respondents were asked if the child had an unmet need upon enrollment in the comprehensive care program and during the 12 months after enrollment. A child was considered to have a met need if the respondent indicated that there was a need and that need was met. An aggregate variable of unmet needs was calculated by adding the number of unmet needs indicated per child.
Figure 1.
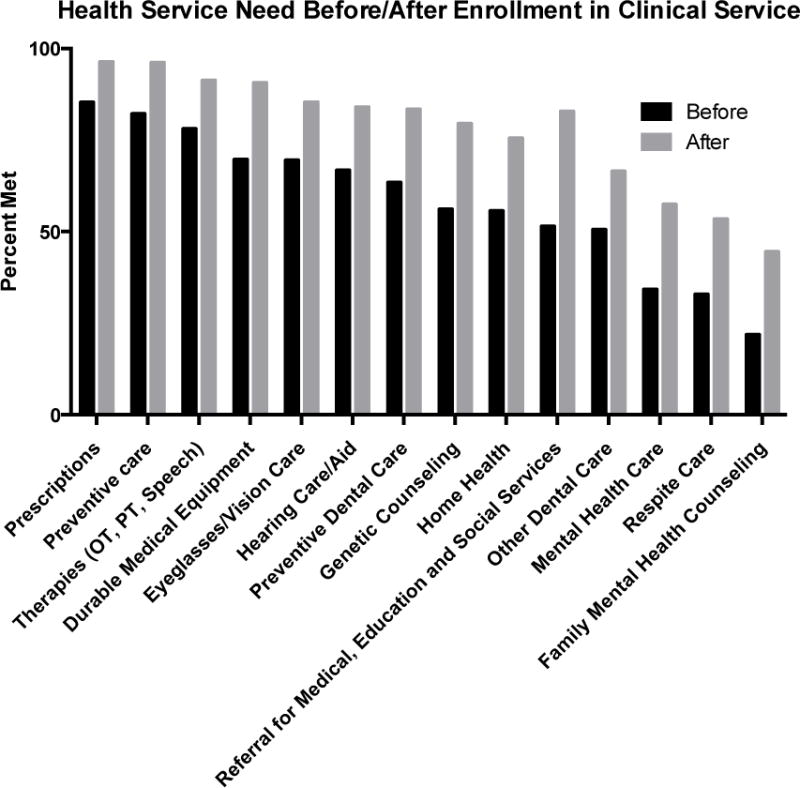
Health Service Need Before/After Enrollment in Structured Clinical Service.
All p<.001
Descriptive variables included the age and race/ethnicity of the child, and the age of the responding parent caregiver. Clinical conditions were assessed by survey response to describe parental perception of health care diagnoses and needs. The health and functional status of the child was subjectively described by the respondent’s assessment of the functional level of the child, need for specific technology, the number and type of specialists seen, and hospital and emergency department use in the prior year. Families were asked about the number of hours families spent per week on care coordination and direct home care, as well as the out of pocket financial costs in the last year, using questions adapted from the NS-CSHCN. Categorical variables were selected to ease survey administration.
Data Analyses
Descriptive demographic statistics were compiled from the raw data. Bivariate analyses were performed with t-tests for continuous variables and chi-square for categorical variables. A comparison of health care services received before and after enrollment in the comprehensive care program was accomplished using paired t-tests. Some variables had missing data, but generally the missing data were 2% or less; because of this low percentage, subjects with missing data were excluded. Study findings of health care services were similar between all three services, and hence are presented in the aggregate. All analyses were conducted using STATA 12.0.
Results
Of 968 mailed surveys, 441 (46%) were completed and returned. The survey response rates were 43% (n = 140) for Boston families, 46% (n = 201) for Arkansas families, and 50% (n = 100) for Wisconsin families. _The characteristics of the respondents and their children are presented in Table I. Most (83.9%) respondents were the mother of the child. The average age of the child at the time of the survey was 6.9 (standard deviation [SD] 5.4) years. Children from Arkansas were younger [4.9 years (SD 3.9)] compared with the other services [Boston = 8.3 (SD 6.0), Wisconsin = 8.8 (SD 5.7)]. The majority (73.0%) of respondents’ children enrolled in a structured clinical care program were White/Caucasian; 15.7% were Black/African American; and 11.1% were Hispanic. Most respondents (72.1%) indicated that they had either public insurance or a combination of private and public insurance, and only 0.2% of respondents had no insurance.
Table 1.
Characteristics of Children Enrolled in Outpatient, Tertiary-Care Structured Clinical Programs for Children with Medical Complexity.
| Overall (N=441) | Medical Home Clinic, Arkansas (N=201) | Special Needs Program, Wisconsin (N=100) | Complex Care Service, Boston (N=140) | |
|---|---|---|---|---|
| Respondent* | ||||
| Mother | 83.9% | 85.6% | 82.8% | 82.1% |
| Father | 8.9% | 4.5% | 12.1% | 12.9% |
| Grandmother | 4.1% | 6.5% | 2.0% | 2.1% |
| Other | 3.2% | 3.5% | 3.0% | 2.9% |
| Child Mean age, years+ | 6.9 (sd 5.4) | 4.9 (sd 3.9) | 8.8 (sd 5.7) | 8.3 (sd 6.0) |
| Race/ethnicity of child (not mutually exclusive) | ||||
| White/Caucasian | 73.0% | 67.5% | 78.0% | 77.1% |
| Black/African American+ | 15.7% | 25.0% | 9.0% | 7.1% |
| Hispanic# | 11.1% | 6.0% | 12.0% | 17.9% |
| Asian/Pacific Islander* | 2.7% | 0.6% | 2.0% | 5.7% |
| Native American | 2.5% | 4.5% | 1.0% | 0.7% |
| Insurance coverage | ||||
| Private insurance | 27.7% | 13.6% | 31.3% | 45.3% |
| Public insurance only | 54.0% | 69.4% | 50.5% | 34.5% |
| Private + Public | 18.1% | 16.6% | 18.2% | 20.1% |
| None | 0.2% | 0.5% | 0% | 0% |
p < .05 between programs
p < .01
p < .001
Developmental delay (79.3%) and feeding difficulties (63.6%) were the most common chronic health problems endured by the children (Table II). Other common health problems included gastroesophageal reflux (52.6%), constipation (38.0%), and growth problem/underweight (36.8%). Forty-three percent of children were born prematurely.
Table 2.
Clinical Characteristics of Children Enrolled in an Outpatient, Tertiary-Care Structured Clinical Program for Children with Medical Complexity.
| Overall | Arkansas | Wisconsin | Boston | |
|---|---|---|---|---|
| Developmental delay | 79.3% | 77.6% | 85.0% | 77.7% |
| Feeding difficulties# | 63.6% | 62.7% | 77.0% | 55.4% |
| Gastroesophageal reflux | 52.6% | 54.0% | 57.0% | 47.5% |
| Communication impairment+ | 44.1% | 32.3% | 53.0% | 54.7% |
| Premature* | 43.0% | 51.3% | 32.3% | 38.7% |
| Constipation# | 38.0% | 30.9% | 52.0% | 38.1% |
| Growth problem/underweight | 36.8% | 38.3% | 38.0% | 33.8% |
| Visual impairment+ | 35.5% | 24.4% | 49.0% | 42.0% |
| Dysphagia/difficulty swallowing+ | 33.7% | 51.0% | 23.0% | 16.6% |
| Intellectual disability# | 30.4% | 21.7% | 38.0% | 37.4% |
| Genetic syndrome+ | 29.3% | 19.4% | 37.0% | 38.1% |
| Aspiration | 29.1% | 33.8% | 31.0% | 20.9% |
| Cerebral palsy | 27.3% | 24.9% | 28.0% | 30.2% |
| Bone/joint problem# | 26.1% | 18.9% | 35.0% | 30.2% |
| Oromotor dysfunction/speech production# | 25.3% | 17.9% | 30.3% | 32.4% |
| Asthma | 21.0% | 19.5% | 25.0% | 20.1% |
| Chronic lung disease# | 20.4% | 24.2% | 27.0% | 10.1% |
| Sleep disturbance# | 18.9% | 12.4% | 23.0% | 25.2% |
| Hearing loss | 18.0% | 13.4% | 22.0% | 21.6% |
| Food allergies | 16.6% | 17.4% | 16.0% | 15.8% |
| Obstructive sleep apnea | 15.7% | 13.9% | 17.0% | 17.3% |
| Behavioral/emotional difficulties# | 15.7% | 9.5% | 17.0% | 23.7% |
| Kidney problem | 15.2% | 12.4% | 17.0% | 18.0% |
| Chronic pain# | 8.2% | 4.0% | 16.0% | 8.6% |
| Urinary tract infection, recurrent | 8.0% | 7.5% | 10.0% | 7.3% |
| Autism | 5.9% | 3.5% | 9.0% | 7.2% |
| Migraine/headache+ | 5.7% | 2.0% | 15.0% | 4.3% |
| Urinary retention | 5.2% | 3.0% | 9.0% | 5.8% |
| ADHD* | 3.9% | 1.5% | 4.0% | 7.2% |
| Inconsolability | 2.3% | 2.0% | 1.0% | 3.6% |
p < .05 between programs
p < .01
p < .001
Regarding medical equipment used by the children, 63.2% had a gastrostomy tube, 28.2% used supplemental oxygen, 11.2% had a ventriculoperitoneal shunt, and 9.1% had a tracheostomy (Table III). Forty percent of parents rated their child’s health condition as “very severe.” Sixty-eight percent of children were under the care of five or more specialists. The most frequently used specialties were neurology (66.2%), gastroenterology (56.9%), otorhinolaryngology (56.0%), and pulmonology (47.3%). Almost half (45.6%) of caregivers indicated that they spent at least 20 hours a week providing direct home care for the child. Almost a third (29.0%) reported at least three emergency department visits in the past twelve months, and 10.3% reported at least 31 days in the hospital. Over one-third (35.5%) indicated out of pocket expenses over the prior twelve months from the survey was greater than $1000. Thirty-nine percent of respondents lived > 60 miles from the site of the tertiary care program.
Table 3.
Medical Equipment and Health Service Needs of Children Enrolled in an Outpatient, Tertiary-Care Structured Clinical Program for Children with Medical Complexity.
| Overall | Arkansas | Wisconsin | Boston | |
|---|---|---|---|---|
| Medical Equipment | ||||
| Gastrostomy tube | 63.2% | 63.0% | 84.0% | 48.6% |
| Special formula+ | 44.0% | 46.7% | 57.0% | 30.7% |
| Supplemental oxygen+ | 28.2% | 21.5% | 44.0% | 26.4% |
| Ventriculoperitoneal shunt | 11.2% | 12.5% | 14.1% | 7.1% |
| Tracheostomy | 9.1% | 6.5% | 13.1% | 10.0% |
| Central venous line+ | 5.5% | 2.0% | 20.2% | 0% |
| Baclofen pump | 3.2% | 2.0% | 6.1% | 2.9% |
| Home ventilator | 3.0% | 2.0% | 3.0% | 4.3% |
| Health Services | ||||
| Sees ≥5 specialists+ | 68.1% | 53.5% | 86.9% | 75.9% |
| ≥20 hrs/week care for child+ | 45.6% | 38.2% | 59.6% | 45.3% |
| Child health problem very severe# | 40.2% | 35.1% | 50.0% | 40.4% |
| Located ≥60 miles from CMC clinic# | 38.5% | 47.5% | 39.4% | 25.2% |
| Out of pocket expenses ≥$1000+ | 35.5% | 25.8% | 41.4% | 46.1% |
| ≥3 ED visits in last 12 months+ | 29.0% | 28.0% | 36.4% | 24.3% |
| ≥31 days in hospital in last 12 mo+ | 10.3% | 12.1% | 11.1% | 7.1% |
p < .05 between programs
p < .01
p < .001
Almost all children (95.4%) had at least one regular well child checkup in the past year, and most children (88.5%) had at least one sick visit with the PCP (Table IV). However, the PCP was the primary point of contact for illness management for 55.4% of children. Just over half of caregivers (55.2%) received help with specialty referrals from the PCP, with 49.5% receiving care coordination and 42.7% reporting that their care plan for emergent health problems was maintained by the PCP. Thirty-nine percent received chronic illness management from their PCP, and 24.0% received help with referrals to family support services.
Table 4.
Reported Care Coordination and Management from PCP in the Prior 12 Months.
| Yes | |
|---|---|
| ≥1 regular well child checkup | 95.4% |
| Sick visits for any reason | 88.5% |
| Serve as primary point of contact | 55.8% |
| Help referring to specialists | 55.2% |
| Care coordination with therapies and specialists | 49.5% |
| Make a care and emergency plan | 42.7% |
| Chronic illness management | 38.9% |
| Help referring to community services | 32.8% |
| In-hospital care for child | 27.7% |
| Help referring to family support services/networks | 24.0% |
At baseline, prior to enrollment, most respondents (78.1%–85.3%) described having preventive care services, prescription needs, and therapies met, with about two-thirds reporting having their needs met for vision, hearing, dental care, and durable medical equipment needs. The fewest needs met were for family mental health counseling (21.9%), respite care (32.9%), and mental health care (34.2%).
The mean number of unmet health care needs decreased from 2.8 (SD 3.2) to 2.2 (SD 3.4) (out of a total of 14 healthcare needs) following enrollment in a structured clinical care program (p<.001). Respondents indicated a rise in meeting the needs of all fourteen health care services after enrollment (Figure). Of respondents, 82.2% of indicated that they had all of their preventive care service needs met before enrollment, rising to 96.2% after enrollment. Just over half of families had their referral needs met (51.4%) before enrollment, with 82.9% after enrollment indicating they had all of their referral needs met after enrollment. Other notable rises include preventive dental care (63.4% to 83.5%), therapies (78.1% to 91.4%), mental health care (34.2% to 57.5%) and respite care (32.9% to 53.4%). Changes of needs met were consistent among the three clinical care programs.
Discussion
The main findings from this study suggest that despite high use of primary and specialty care, CMC enter structured clinical care programs at tertiary care centers with a number of unmet health care service needs. Mental health needs for the child and family and respite care for the family were met the least upon enrollment. Enrollment in a targeted, structured clinical care program at a tertiary care center was associated with significant increases in met health service needs. The striking part of the study findings is the across-the-board improvement of meeting a range of health service needs, as parents reported improvement across all fourteen health care service needs.
Families of CMC have previously reported a high number of unmet health care needs regardless of insurance type, race/ethnicity, or income level.(8, 9) The combination of unmet needs reported by families and the lack of receipt of sufficient services from the primary care setting are consistent with the gaps in services, or even a feeling of abandonment, that families have reported.(11, 27) Literature examining parent outcomes at single centers report improvement in continuity of care, care coordination, and comprehensiveness of care, with limited impact on family health and access to overall services.(28, 29) Even after enrollment in this study, substantial percentages of children still had unmet needs related to mental health and respite care. Further investigation is needed to determine how to best meet all of the health care needs of children with medical complexity in the most efficient and effective way.
All three clinics participating in this study share common model parameters, including identification of the target patient population, a multi-disciplinary approach, an assigned care coordinator or provider as a point of contact, patient education, the development and maintenance of care plans, and support to the primary care physician. A dedicated care coordinator serving a panel of patients in each clinic may have been directly responsible for the substantial improvement in addressing the need for referrals. However, we found that a range of needs was met regardless of whether specific services were being provided in the clinic. For example, respite care needs were met more frequently after enrollment, even though no clinic provided specific respite care services. This improvement may have addressed under-referrals to available resources; increased family knowledge for advocacy; or enabled additional time for parents to pursue specific needs not directly addressed in the clinic setting. Also striking was that many of these needs could be met despite the fact that almost 40% of children lived a significant distance from the comprehensive care program.
The children whose parents were surveyed in this study continued to have a relatively high utilization of primary care provider services, as indicated by almost all children having at least one regular well child checkup in past twelve months. Many families, however, reported not receiving adequate chronic care management or assistance with referral to specialists, family support services, or community services from the primary care setting, despite receiving preventive care checkups. The survey did not ask whether these services could be or were previously provided by the PCP. The level of unmet needs prior to service enrollment, however, suggests that social/family needs were not being met from the primary care setting alone.
There are a number of limitations to our findings. The results are subject to significant recall bias as some caregivers were asked to remember needs dating back up to five years. The study criteria excludes families whose child left the program or died and the sample may be biased towards those who favor the program. With a response rate of 46%, the results are limited to the study sample, and may not adequately represent all of the clinical services provided to or needed by all children who have medical complexity. The survey questions on health service needs were adapted from a telephone survey and thus have not been validated for a mailed paper survey, although the level of unmet needs for this clinically identified population is higher than previously described in the NS-CSHCN.(8) Unmet needs could have been addressed by temporal trends (e.g. parenting experience, advocacy supports). The survey was only administered in English, a decision made as a result of not having reliable information about the preferred language, but in all likelihood the survey reflects English-fluent households only. Certain variables were available only as categorical data, a choice made to ease administration of the survey, but some information is lost with this approach.
In summary, this study suggests that health service needs of families of CMC were better met after enrollment in a comprehensive structured care program at a tertiary care center. Health care reform suggests that comprehensive care may be supported by payments for Patient-Centered Medical Homes in the primary care setting,(30) but PCPs are concerned about their ability to care for CMC due to time and payment constraints.(15, 16, 31) Our findings suggest that many CMC receive preventive medical care in the PCP setting but not the full array of care coordination and social/family services that many CMC need. Advantages of a structured care program in the tertiary care setting include proximity to specialists and dedicated medical expertise in complex care.(32, 33) Cost savings and reduction of potentially preventable highcost encounters such as hospitalizations may be achieved with increased use of such outpatient specialty services.(20, 23, 24) The financial impact of addressing mental health needs remains unknown, and payment for comprehensive care and care coordination remain a challenge from all settings.(20) This study cannot conclude whether the best access to care coordinators, social workers, and specialists is the tertiary care center or the PCP setting with additional support. Future studies must evaluate different models of care for different populations of CMC according to conditions, functionality, and distance to the tertiary care center.
Acknowledgments
We thank Linda Wright for data collection and entry support.
D.K. was supported by was supported by the Translational Research Institute (UL1TR000039 and KL2TR000063) through the National Institutes of Health (NIH) National Center for Research Resources and the National Center for Advancing Translational Sciences. The content is solely the responsibility of the authors and does not necessarily represent the official views of the NIH.
Abbreviations
- CMC
children with medical complexity
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
The authors declare no conflicts of interest.
Portions of the study were presented at the meeting of the Pediatric Academic Societies, Vancouver, B, Canada, May 3–6, 2014, as well as at the meeting of the American Academy for Cerebral Palsy and Developmental Medicine, San Diego, CA, September <days>, 2014.
References
- 1.McPherson M, Arango P, Fox H, Lauver C, McManus M, Newacheck PW, et al. A new definition of children with special health care needs. Pediatrics. 1998;102:137–40. doi: 10.1542/peds.102.1.137. [DOI] [PubMed] [Google Scholar]
- 2.Srivastava R, Stone BL, Murphy NA. Hospitalist care of the medically complex child. Pediatr Clin North Am. 2005;52:1165–87. doi: 10.1016/j.pcl.2005.03.007. [DOI] [PubMed] [Google Scholar]
- 3.Wise PH. The transformation of child health in the United States. Health Aff (Millwood) 2004;23:9–25. doi: 10.1377/hlthaff.23.5.9. [DOI] [PubMed] [Google Scholar]
- 4.Bitsko RH, Visser SN, Schieve LA, Ross DS, Thurman DJ, Perou R. Unmet health care needs among CSHCN with neurologic conditions. Pediatrics. 2009;124(Suppl 4):S343–51. doi: 10.1542/peds.2009-1255D. [DOI] [PubMed] [Google Scholar]
- 5.Singh GK, Strickland BB, Ghandour RM, van Dyck PC. Geographic disparities in access to the medical home among US CSHCN. Pediatrics. 2009;124(Suppl 4):S352–60. doi: 10.1542/peds.2009-1255E. [DOI] [PubMed] [Google Scholar]
- 6.Kane DJ, Kasehagen L, Punyko J, Carle AC, Penziner A, Thorson S. What factors are associated with state performance on provision of transition services to CSHCN? Pediatrics. 2009;124(Suppl 4):S375–83. doi: 10.1542/peds.2009-1255H. [DOI] [PubMed] [Google Scholar]
- 7.Kenney MK. Oral health care in CSHCN: state Medicaid policy considerations. Pediatrics. 2009;124(Suppl 4):S384–91. doi: 10.1542/peds.2009-1255I. [DOI] [PubMed] [Google Scholar]
- 8.Kuo DZ, Cohen E, Agrawal R, Berry JG, Casey PH. A National Profile of Caregiver Challenges Among More Medically Complex Children with Special Health Care Needs. Arch Pediatr Adolesc Med. 2011;165:1020–6. doi: 10.1001/archpediatrics.2011.172. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Kuo DZ, Goudie A, Cohen E, Houtrow A, Agrawal R, Carle AC, et al. Inequities in health care needs for children with medical complexity. Health Aff (Millwood) 2014;33:2190–8. doi: 10.1377/hlthaff.2014.0273. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Dusing SC, Skinner AC, Mayer ML. Unmet need for therapy services, assistive devices, and related services: data from the national survey of children with special health care needs. Ambul Pediatr. 2004;4:448–54. doi: 10.1367/A03-202R1.1. [DOI] [PubMed] [Google Scholar]
- 11.MacKean GL, Thurston WE, Scott CM. Bridging the divide between families and health professionals’ perspectives on family-centred care. Health Expect. 2005;8:74–85. doi: 10.1111/j.1369-7625.2005.00319.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Warfield ME, Gulley S. Unmet need and problems accessing specialty medical and related services among children with special health care needs. Matern Child Health J. 2006;10:201–16. doi: 10.1007/s10995-005-0041-3. [DOI] [PubMed] [Google Scholar]
- 13.Mayer ML, Skinner AC, Slifkin RT. Unmet need for routine and specialty care: data from the National Survey of Children With Special Health Care Needs. Pediatrics. 2004;113:e109–15. doi: 10.1542/peds.113.2.e109. [DOI] [PubMed] [Google Scholar]
- 14.McPherson M, Weissman G, Strickland BB, van Dyck PC, Blumberg SJ, Newacheck PW. Implementing community-based systems of services for children and youths with special health care needs: how well are we doing? Pediatrics. 2004;113:1538–44. [PubMed] [Google Scholar]
- 15.Kuo DZ, Robbins JM, Burns KH, Casey PH. Individual and Practice Characteristics Associated with Physician Provision of Recommended Care for Children with Special Health Care Needs. Clin Pediatr (Phila) 2011;50:704–11. doi: 10.1177/0009922811398961. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Agrawal R, Shah P, Zebracki K, Sanabria K, Kohrman C, Kohrman AF. The capacity of primary care pediatricians to care for children with special health care needs. Clin Pediatr (Phila) 2013;52:310–4. doi: 10.1177/0009922813476572. [DOI] [PubMed] [Google Scholar]
- 17.Berman S, Rannie M, Moore L, Elias E, Dryer LJ, Jones MD., Jr Utilization and costs for children who have special health care needs and are enrolled in a hospital-based comprehensive primary care clinic. Pediatrics. 2005;115:e637–42. doi: 10.1542/peds.2004-2084. [DOI] [PubMed] [Google Scholar]
- 18.Cohen E, Friedman J, Nicholas DB, Adams S, Rosenbaum P. A home for medically complex children: the role of hospital programs. J Healthc Qual. 2008;30:7–15. doi: 10.1111/j.1945-1474.2008.tb01137.x. [DOI] [PubMed] [Google Scholar]
- 19.Kelly A, Golnik A, Cady R. A medical home center: specializing in the care of children with special health care needs of high intensity. Matern Child Health J. 2008;12:633–40. doi: 10.1007/s10995-007-0271-7. [DOI] [PubMed] [Google Scholar]
- 20.Gordon JB, Colby HH, Bartelt T, Jablonski D, Krauthoefer ML, Havens P. A tertiary care-primary care partnership model for medically complex and fragile children and youth with special health care needs. Arch Pediatr Adolesc Med. 2007;161:937–44. doi: 10.1001/archpedi.161.10.937. [DOI] [PubMed] [Google Scholar]
- 21.Tanios AT, Lyle RE, Casey PH. ACH medical home program for special needs children. A new medical era. J Ark Med Soc. 2009;105:163–5. [PubMed] [Google Scholar]
- 22.Mosquera RA, Avritscher EB, Samuels CL, Harris TS, Pedroza C, Evans P, et al. Effect of an enhanced medical home on serious illness and cost of care among high-risk children with chronic illness: a randomized clinical trial. JAMA. 2014;312:2640–8. doi: 10.1001/jama.2014.16419. [DOI] [PubMed] [Google Scholar]
- 23.Casey PH, Lyle RE, Bird TM, Robbins JM, Kuo DZ, Brown C, et al. Effect of Hospital-Based Comprehensive Care Clinic on Health Costs for Medicaid-Insured Medically Complex Children. Arch Pediatr Adolesc Med. 2011;165:392–8. doi: 10.1001/archpediatrics.2011.5. [DOI] [PubMed] [Google Scholar]
- 24.Klitzner TS, Rabbitt LA, Chang RK. Benefits of Care Coordination for Children with Complex Disease: A Pilot Medical Home Project in a Resident Teaching Clinic. J Pediatr. 2010;156:1006–10. doi: 10.1016/j.jpeds.2009.12.012. [DOI] [PubMed] [Google Scholar]
- 25.Dillman D. Mail and Internet Surveys: The Tailored Design Method. New York: Wiley; 2000. [Google Scholar]
- 26.Blumberg SJ, Welch EM, Chowdhury SR, Upchurch HL, Parker EK, Skalland BJ. Design and operation of the National Survey of Children with Special Health Care Needs 2005–06. National Center for Health Statistics; 2008. [PubMed] [Google Scholar]
- 27.Wells N, Krauss MW, Anderson B, Gulley S, Leiter V, O’Neil M, et al. What do families say about health care for children with special health care needs? Your voice counts!! The Family Partners Project report to families. Boston, MA: Family Voices at the Federation for Children with Special Health Care Needs; 2000. [Google Scholar]
- 28.Cohen E, Friedman JN, Mahant S, Adams S, Jovcevska V, Rosenbaum P. The impact of a complex care clinic in a children’s hospital. Child Care Health Dev. 2010;36:574–82. doi: 10.1111/j.1365-2214.2009.01069.x. [DOI] [PubMed] [Google Scholar]
- 29.Kuo DZ, Robbins JM, Lyle RE, Barrett KW, Burns KH, Casey PH. Parent-reported outcomes of comprehensive care for children with medical complexity. Fam Syst Health. 2013;31:132–41. doi: 10.1037/a0032341. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Edwards ST, Abrams MK, Baron RJ, Berenson RA, Rich EC, Rosenthal GE, et al. Structuring Payment to Medical Homes After the Affordable Care Act. J Gen Intern Med. 2014 Oct;29:1410–3. doi: 10.1007/s11606-014-2848-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Agrawal R, Shah P, Zebracki K, Sanabria K, Kohrman C, Kohrman AF. Barriers to care for children and youth with special health care needs: perceptions of Illinois pediatricians. Clin Pediatr (Phila) 2012;51:39–45. doi: 10.1177/0009922811417288. [DOI] [PubMed] [Google Scholar]
- 32.Cohen E, Kuo DZ, Agrawal R, Berry JG, Bhagat SK, Simon TD, et al. Children With Medical Complexity: An Emerging Population for Clinical and Research Initiatives. Pediatrics. 2011;127:529–38. doi: 10.1542/peds.2010-0910. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Berry JG, Agrawal R, Kuo DZ, Cohen E, Risko W, Hall M, et al. Characteristics of Hospitalizations for Patients who Utilize a Structured Clinical-Care Program for Children with Medical Complexity. J Pediatr. 2011;159:284–90. doi: 10.1016/j.jpeds.2011.02.002. [DOI] [PMC free article] [PubMed] [Google Scholar]


