Abstract
Objective
The purpose of this study was to prospectively examine adolescent and maternal posttraumatic stress symptoms (PTSS) and maternal communication from time near cancer diagnosis to 12-month follow-up to identify potential risk factors for adolescent PTSS.
Methods
Forty-one adolescents with cancer (10–17 years, 54% female) and their mothers self-reported PTSS at T1 (two months after cancer diagnosis) and T3 (one year follow-up). At T2 (three months after T1), mother-adolescent dyads were videotaped discussing cancer and maternal communication was coded with macro (harsh and withdrawn) and micro (solicits and validations) systems.
Results
Adolescent PTSS at T1 was associated with adolescent PTSS at T3. Greater maternal PTSS at T1 predicted greater harsh maternal communication at T2. There was an indirect effect of maternal PTSS at T1 on adolescent PTSS at T3 through maternal validations at T2.
Conclusions
Findings underscore the importance of maternal PTSS, maternal communication, and subsequent adolescent PTSS over the course of treatment of childhood cancer.
Keywords: Cancer, Oncology, Adolescents, Posttraumatic stress, Communication
Introduction
Adolescents with cancer and their parents are faced with significant stress at diagnosis and throughout treatment. Research has examined posttraumatic stress symptoms (PTSS) in youth diagnosed with cancer, as well as survivors in early adulthood. PTSS in this population are particularly concerning because they are associated with lower health-related quality of life and increased distress and could interfere with future, long-term follow-up care [1,2,3]. Indeed, several researchers, including Kazak et al. [2] and Bruce et al. [4]), have argued PTSS is an important area of research, as continuous symptom counts may be most applicable to the experiences of families with child cancer diagnoses and even sub-threshold levels of symptoms are associated with impairment and distress that is clinically significant ([2,5]). Therefore an important focus for research is to identify predictors of PTSS during treatment and recovery to alert clinicians to families needing intervention and inform treatment targets.
Kazak et al. [2] present a model of pediatric medical traumatic stress that emphasizes distinct stages from diagnosis (Phase I), through treatment (Phase II), and into survivorship (Phase III). However, there has been relatively little longitudinal research that characterizes distress at early stages and follows families through these phases. Demographic factors associated with adolescent distress, including female sex, older age, and lower SES, have been inconsistently linked to PTSS in pediatric cancer patients [3,4]. However, meta-analyses examining PTSS risk factors from various forms of trauma indicate that PTSS close to the time of trauma predict subsequent PTSS [6,7]. Longitudinal prospective studies are rare in pediatric cancer, but Barakat et al. [8] found that PTSS reported months after treatment were associated with subsequent behavioral problems. Therefore, there is evidence to suggest that adolescent PTSS near time of diagnosis will be related to PTSS at one-year follow-up.
Adolescents’ wellbeing during cancer diagnosis and treatment is also closely tied to parents’ wellbeing, and at least a subgroup of these parents are at risk for PTSS themselves (e.g., [9,10]). Meta-analyses indicate that parent PTSS is a risk factor for child and adolescent PTSS in response to trauma [6,11]. In a review of posttraumatic stress in childhood cancer survivors, maternal PTSS was identified as a predictor of youth symptoms, although studies have largely been cross-sectional [4].
Parents serve a vital role during cancer diagnosis and treatment, providing both emotional support and information to their child [12]. However, the components of parent-adolescent communication that impact youth PTSS have not been clearly identified and research has been limited by two methodological factors. First, longitudinal studies are needed to examine mechanisms through which parent symptoms may impact adolescent symptoms over time. Second, specific communication patterns have rarely been examined in the context of parent and adolescent PTSS. Studies that have examined parenting in association with PTSS have been restricted to self-reports of family functioning and perception of family conflict [13,14]. Researchers have called for observational studies of parent-child interactions (e.g., [2,4]) to reduce the possibility of shared method variance among measures of key constructs and to characterize specific communication patterns that underlie the relation between maternal and adolescent PTSS.
Research on the role of parenting and PTSS can be guided by a model proposed by Scheeringa and Zeanah [15]. They suggest that parental symptoms may disrupt parent-child interactions, which may then exacerbate child symptoms. They propose that harmful communication patterns may occur, including withdrawn/unresponsive, overprotective/constricting, and frightening patterns. Although this model was originally proposed for parents of younger children, support for these communication patterns has been found in samples of parents of older children and adolescents as well. There is evidence for the negative effects of the withdrawn pattern, as parental avoidance behaviors are correlated with child PTSS in studies outside of pediatric oncology [16,17]. Support has also been found for the negative effects of maternal harsh communication in mothers who experienced war-related trauma [18], and parents with PTSD are more likely to report using harsh parenting tactics [19]. Withdrawn and harsh maternal communication styles may have particularly negative consequences for adolescents with cancer, who need support in processing their diagnosis and treatment.
Maternal PTSS may also impact adolescent symptoms through micro-level patterns of communication that allow adolescents to process their experiences. Parenting at the micro-level reflects moment-to-moment exchanges between parents and adolescents, similar to discourse pragmatics [20]. Therefore in the current study, micro-level analyses were used to capture maternal responses that allow adolescents to express their thoughts and emotions surrounding their cancer diagnosis and responses that validate those thoughts and emotions. Specifically, maternal solicits (asking questions of the adolescent to elicit information) and validations (confirming, emphasizing, or praising adolescent utterances) were examined during conversations about cancer in the present study. There is preliminary evidence that parents’ requests for information and confirmations (analogous to solicits and validations) are positively related to child wellbeing in families of healthy children [21], but this has not yet been examined in pediatric oncology. In this way, macro- and micro-level coding systems draw on separate but complementary information during the course of interaction. Integrating these analyses can better characterize communication patterns, specify mechanisms of effect, and provide targets for intervention [12,22].
The purpose of this study is to examine associations among adolescent and maternal PTSS due to cancer diagnosis and maternal communication over time, in order to identify potential risk factors that predict adolescent PTSS at one-year follow-up. Maternal and adolescent PTSS were assessed near the time of the adolescent’s diagnosis (Kazak’s Phase I), and again 12 months later (Kazak’s Phase II [2]). Mothers and adolescents were video-recorded while communicating about cancer between the baseline and follow-up assessments and coded on both macro (harsh and withdrawn) and micro (solicits and validations) levels. We hypothesized that (1) adolescents’ and mothers’ PTSS near the time of cancer diagnosis will predict adolescent PTSS at one year follow-up; (2) maternal communication will be associated with maternal and adolescent PTSS, such that greater maternal PTSS near diagnosis will be related to greater harsh and withdrawn communication and fewer validations and solicits three months later, and these will be related to greater adolescent PTSS at one-year follow-up; and (3) maternal communication at three months follow-up will mediate the relation between mothers’ PTSS near diagnosis and adolescents’ PTSS at one-year follow-up.
Method
Participants
Participants were involved in a longitudinal study investigating family adjustment to childhood cancer. Families were recruited from two pediatric oncology centers in the Midwestern and Southern United States. Eligible families had children who (a) were ages 5–17 years old, (b) had a new cancer diagnosis or recent recurrence, (c) were actively receiving treatment through the oncology division, and (d) had no developmental disability. Participants included 41 adolescents and their mothers. The current sample differed from the larger sample in that only families of adolescents (age 10–17; adolescence defined as the second decade of life [23]) were included, because youth younger than 10 were not expected to be valid self-reporters of PTSS [24]. Adolescents were on average 13.27 years old (SD=2.33) and 54% were female. Thirty-seven (90.2%) were Caucasian, 3 (7.3%) African-American, and the remainder reported “Other” for their race; 1 (2.4%) was Hispanic/Latino. Cancer diagnoses included leukemia (36.6%), lymphoma (22.0%), and other solid tumor (41.5%; e.g., sarcomas), but not brain tumors. At T3 follow-up, 20 (49%) were still receiving treatment while 21 (51%) were off treatment. Mothers were on average 41.80 years old (SD=7.82); educational backgrounds ranged from high school to graduate school (M=3 years of college or trade school). Families reported a range of family income levels (12%: $25,000 or less; 32%: $25,001–50,000; 19%: $50,001–75,000; 15%: $75,000–100,000; 22%: $100,000 or above).
Procedure
At Time 1, approximately two months after the adolescent’s cancer diagnosis, mothers and adolescents completed self-report measures of PTSS and mothers reported family demographics. Approximately three months later (Time 2), families were approached to participate in an optional video-recorded observation of a discussion between the mother and adolescent about the adolescent’s cancer diagnosis and treatment. At Time 3, on average one year after T1, families completed the same questionnaires they completed at T1.
For inclusion in the current analyses, families completed assessments at T1 and T3, as well as the observation at T2. Of the 98 families who completed assessments at both T1 and T3, 41 families had English-speaking mother-adolescent dyads participate in the observation. Reasons for declining the observation included lack of time, not wanting to be videotaped, and lack of interest. Families who completed the observation did not significantly differ from those who declined on adolescent age, mother age, adolescent race, adolescent ethnicity, family income, relapse status, or adolescent or maternal PTSS at either time point.
During the observation, dyads were brought to a private room at the hospital and graduate-level research assistants instructed mothers and adolescents to have a conversation about the adolescent’s cancer in whatever way felt natural to them. Mothers received a card with written prompts (e.g., What have we each learned about cancer and how it is treated?) to help guide the conversation as needed. After 15 minutes the research assistant returned and debriefed the participants to address any potential questions or distress. Mothers and children responded to a questionnaire assessing the representativeness of their communication during the task. In response to the statement “The discussion represented how I usually communicate with my mother/child about cancer,” 100% of adolescents and 93% of mothers endorsed “somewhat” or “very” true.
The Institutional Review Boards of the participating academic medical centers approved all study procedures. Informed consent and assent were obtained from participants. Families were compensated with checks or gift cards.
Measures
Family demographics
Mothers reported adolescents’ age and race/ethnicity, and self-reported age, family income, and educational attainment.
Medical information
Adolescent cancer diagnoses and treatment information were obtained from medical records.
Post-traumatic stress symptoms (PTSS)
Adolescents and mothers completed self-reports of PTSS specific to the child’s cancer diagnosis and treatment on the Impact of Events Scale- Revised [25]. Participants were asked to answer items “using your/your child’s cancer and treatment as the stressful event” to avoid priming participants to view the cancer diagnosis as traumatic. The IES-R was developed to parallel DSM-IV criteria for PTSD and includes 22 items that assess symptoms in the domains of Hyperarousal, Intrusion/Re-experiencing, and Avoidance in the past 7 days. Responses are on a 5-point scale (0=“Not at all” to 4=“Extremely”). The IESR demonstrates good reliability and validity [25] and it has been used previously with pediatric cancer populations (e.g., [26,27,28]). Severity of PTSS on the IES-R was calibrated with a total score, reflecting number and frequency/severity of symptoms endorsed; previous research indicates that continuous symptom counts that capture frequency and severity of symptoms are well suited for pediatric oncology (see [2,5]). Internal consistency in the current sample was excellent for mothers and adolescents across T1 and T3 (Cronbach’s α=.90 to .94).
Observed maternal communication: Macro-level
The Iowa Family Interaction Scale (IFIRS; [29]) is a macro-level system used to code parents’ verbal and non-verbal communication, behaviors, and emotions from 1 (absent) to 9 (mainly characteristic). Frequency, intensity, and contextual or affective nature of the behavior as well as age of the child are taken into consideration during scoring. Trained graduate and undergraduate research assistants first passed a written test of code definitions with 90% accuracy and reached 80% reliability on previously coded videos. All videos were coded independently by two coders, who then met to reach consensus. Per the IFIRS manual, higher scores were used when ratings differed by a single point; ratings that differed by more than two points were resolved through discussion.
Two composite codes, harsh and withdrawn communication, were created for the current study and were theoretically derived to capture parenting styles that may result from PTSS [15]. A harsh communication composite code was created by averaging three codes (hostile, inconsistent discipline, intrusiveness) and a withdrawn communication composite code was created by averaging four codes (neglect/distancing, listener responsiveness, child monitoring, quality time), the last three of which were reverse scored. Codes and definitions are found in Table 1. Similar IFIRS composites have been used in previous research with other pediatric populations (e.g., [30]). Intraclass correlations (ICCs) for the individual codes within harsh communication ranged from .52 to .76 (M=.68). For withdrawn communication, individual code ICC’s ranged from .40 to .81 (M=.60).
Table 1.
Maternal communication macro- and micro-level codes and definitions
| Code | Definition | Examples | Mean (SD) | Range |
|---|---|---|---|---|
| IFIRS | ||||
| Harsh Communication | Hostile, inconsistent, and intrusive verbal and nonverbal behavior toward the adolescent | Attacks/criticisms or demonstrating irritability/frustration with the adolescent. “You’re being a pest.” | 2.42 (.98) | 1.00–4.67 |
| Withdrawn Communication | Neglectful, unresponsive, and uninvolved verbal or non-verbal behavior toward the adolescent | Looking away or not responding to the adolescent’s statements. “I don’t care what you do.” | 4.55 (.79) | 2.5–7.00 |
| Contingency | ||||
| Solicit | Mother asks a question in order to elicit a response from the adolescent | Adolescent: “I was scared.” Mother: “What was scary?” |
16.46 (11.99) | 1–45 |
| Validation | Mother confirms, empathizes, or praises the adolescent’s utterance without adding new content | Adolescent: “I was scared.” Mother: “I know.” |
2.49 (2.03) | 0–7 |
Observed maternal communication: Micro-level
Unlike macro-level coding which requires watching videos of interactions, micro-level coding is based on examining transcripts and coding individual parent utterances. The Contingency Coding System (CCS; [12]) was used to examine micro-level communication. The first two maternal utterances immediately after an adolescent’s utterance were coded, and each utterance received a single unique code. Solicits and validations were examined in the current study as they were hypothesized to be relevant to PTSS. Solicits are defined as questions asked by the mother to elicit a response while validations are utterances that confirm, emphasize, or praise the adolescent’s utterance without adding new content (c.f., [21,31]). See Table 1 for code definitions and examples. All observations were first transcribed and then coded by trained undergraduate and graduate coders who achieved 90% correct on a written test of code definitions and reached 80% reliability during training. All observations were coded using printed transcripts independently by two coders who met to reach consensus. Percent agreement was 95% for solicits and 80% for validations.
Data analyses
Analyses were conducted using SPSS (22nd edition). Adolescent and maternal PTSS and communication variables were within acceptable levels of Skewness and Kurtosis. Examination of multivariate outliers was conducted with Mahalanobis Distances. Power analyses indicated that with n=41, power=.80, and alpha=.05 one-tailed, significant correlations of medium effect sizes (r>.24) could be detected. Means and standard deviations were calculated for all study variables and Pearson’s r and Spearman rho correlations were calculated for associations among variables. One-tailed correlations were conducted for analyses that had a priori hypotheses (similar to previous studies with pediatric oncology, (e.g., [28]) and two-tailed correlations were conducted for all other analyses. To evaluate maternal communication as a possible mediator, the PROCESS macro for SPSS was used [32]. This is based on Ordinary Least Squares regression and incorporates a parametric bootstrapping procedure that provides confidence intervals on total, direct, and indirect effects as well as a kappa-based coefficient. The current analysis was conducted with a 95% confidence interval for the indirect effect with 10,000 bootstrap samples. Mediation occurs if an indirect effect contributes significantly to the model estimation, such that the confidence interval of the indirect path does not contain zero [33]. Similar analyses have been used with pediatric oncology [34]. Regression analyses conducted with SPSS (version 22) were also used to evaluate maternal communication as a significant predictor of adolescent PTSS at follow-up.
Results
Preliminary Analyses
Means and standard deviations for communication variables are reported in Table 1. Bivariate correlations indicated that maternal harsh communication was positively related to maternal solicits (r=.44, p<.01). In addition, adolescent age was significantly negatively related to harsh communication (r=−.43, p<.01).
Means and standard deviations for adolescent and mother PTSS are reported in Table 2. Adolescents’ PTSS did not significantly change from T1 to T3, whereas mothers’ were significantly lower at T3 than at T1, t(40)=2.38, p=.02. Adolescent age, sex, and family income were not significantly related to adolescent PTSS or maternal PTSS at either time point. PTSS at T3 did not significantly differ according to treatment status (on or off treatment at T3). Therefore these variables were not included in further analyses.
Table 2.
Means, Standard Deviations, and Correlations among adolescents’ and mothers’ PTSS at T1 and T3
| M (SD) | 1 | 2 | 3 | 4 | ||
|---|---|---|---|---|---|---|
| Time 1 | 1 Mother PTSS | 27.53 (16.05) | - | |||
| 2 Adolescent PTSS | 22.72 (14.93) | .37* | - | |||
| Time 3 | 3 Mother PTSS | 20.70 (18.13) | .38** | .08 | - | |
| 4 Adolescent PTSS | 21.87 (18.21) | .28* | .43** | .16 | - |
p<.01,
p<.05
Note. N = 41. T1: Initial assessment near time of diagnosis. T3: 12-month follow-up. PTSS: Posttraumatic stress symptoms.
Hypothesis 1: Associations between maternal and adolescent PTSS
Correlations were calculated among mothers’ and adolescents’ symptoms at T1 and T3 (see Table 2). Adolescents’ PTSS at T1 were significantly positively related to adolescents’ PTSS at T3 (r=.43, p<.01). Mothers’ PTSS at T1 were significantly positively related to adolescents’ PTSS at T3 (r=.28, p<.05).
Hypothesis 2: Associations among PTSS and communication
Solicits were not significantly related to PTSS at either time point (see Table 3). Maternal PTSS at T1 were significantly positively correlated with maternal harsh communication at T2 (r=.35, p<.05) and maternal withdrawn communication at T2 (r=.27, p<.05), such that greater maternal PTSS at T1 were prospectively related to more harsh and withdrawn communication. However, neither maternal harsh or withdrawn communication at T2 was significantly related to adolescent PTSS at T3. Maternal PTSS at T1 was significantly negatively related to validations at T2 (r= −.29, p<.05), such that greater maternal symptoms were related to fewer validations three months later; maternal validations during the observation at T2 were significantly negatively related to adolescent PTSS at T3 (r=-.40, p<.01), such that fewer maternal validations were related to greater adolescent symptoms subsequently.
Table 3.
Correlations between maternal communication variables and mothers’ and adolescents’ PTSS
| Communication at T2 | Mothers’ PTSS at T1 | Adolescents’ PTSS at T3 |
|---|---|---|
| Macro-level | ||
| Harsh Communication | .35* | .13 |
| Withdrawn Communication | .27* | −.12 |
| Micro-level | ||
| Solicits | .11 | .22 |
| Validations | −.29* | −.39** |
p<.01,
p<.05
Note. N = 41. T1: Initial assessment near time of diagnosis. T2: Three months after T1. T3: 12-month follow-up. PTSS: Posttraumatic stress symptoms.
Hypothesis 3: Communication as mediator of PTSS
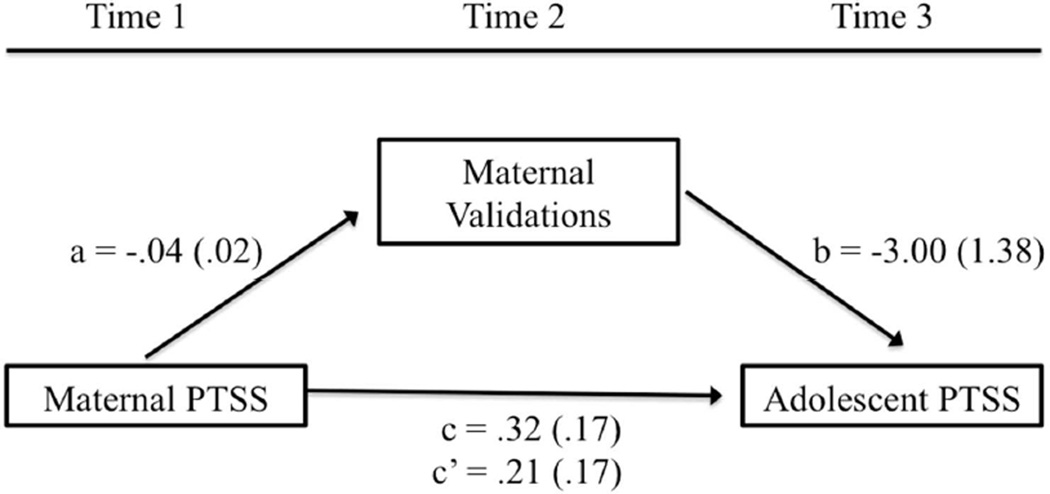
Given the pattern of findings above, only the indirect effect of maternal PTSS at T1 on adolescent PTSS at T3 through maternal validations was examined. In the model examining validations, the path coefficient of the total effect of maternal PTSS at T1 on adolescent PTSS at T3 was .32 (p=.08), the path coefficient of the direct effect was .21 (p=.24), and the indirect effect of maternal PTSS at T1 on adolescent PTSS at T3 through validations at T2 was .11 (Boot SE=.08, 95% CI=.01–.36). See Figure 1. The kappa2 coefficient was .10 (Boot SE=.06, CI=.01– .27), which is considered a medium effect size[35]. This indicates that maternal PTSS at T1 has a significant indirect relationship with adolescent PTSS 12 months later through maternal validations.
Figure 1.
Unstandardized path coefficients for the mediation model of the total, direct, and indirect effects of maternal PTSS at T1 on adolescent PTSS at T3 through maternal validations at T2. Standard errors are in parentheses.
To further examine the role of validations, a hierarchical linear regression predicting adolescent PTSS at T3 was conducted, controlling for adolescent PTSS at T1. Maternal PTSS at T1, adolescent PTSS at T1, and maternal validations at T2 were entered as predictors. The regression was significant, F(40) = 5.22, p<.01 (R2=.30). In the final step, both adolescent PTSS at T1 (β=.37, p<.05) and maternal validations at T2 (β= −.32, p<.05) were significant predictors.
Discussion
This longitudinal, multimethod study is unique in that it includes assessments during both Phase I and Phase II of Kazak et al.’s [2] model of pediatric medical traumatic stress, and examines associations among PTSS and communication during mother-adolescent discussions of cancer. The results identify risk factors for adolescent PTSS over time and suggest a pathway through which maternal PTSS is related to adolescent PTSS over time. This study therefore holds important clinical implications for families of adolescents with cancer.
Mean PTSS in mothers in the current sample are comparable to that of previous pediatric oncology studies using the IES-R (e.g., [26,34]). Results indicate that mothers’ PTSS decreased significantly over the 12 months between T1 and T3, similar to results of previous longitudinal studies [26,36]. Adolescents’ PTSS was lower than mothers’ at T1, which is also consistent with previous research (e.g., [27]). However, adolescents’ PTSS did not change over time, indicating that adolescent PTSS remains relatively stable over the period of one year after diagnosis. Given that this period is characterized by numerous treatments and hospitalizations [2], it is perhaps not surprising that distress does not decline. It also speaks to the potential utility of clinical services for adolescents during the first few months after diagnosis.
The first hypothesis was supported, as both adolescents’ PTSS at and mothers’ PTSS at T1 predicted adolescents’ PTSS one year later. Although parent PTSS has been found to be a risk factor for child PTSS over time [6], this has rarely been examined longitudinally in pediatric cancer. Similar to previous studies [13], adolescent and maternal PTSS were significantly correlated concurrently at T1. Interestingly, adolescent and maternal PTSS were not related at T3, suggesting that different processes may be unfolding for mothers and patients during the year after diagnosis as mothers’ distress declines and adolescents’ distress remain relatively stable.
The second hypothesis, that maternal communication is associated with PTSS, was partially supported. Of the two macro-level communication variables, both harsh and withdrawn communication were related to maternal PTSS at T1. This is similar to the results of a previous study, in which parents who met criteria for PTSD were more likely to report harsh parenting [19], but has not been examined with observational methods or in pediatric samples. This finding suggests that mothers with greater symptoms of distress are more likely to demonstrate intrusion and hostility, as well as decreased responsiveness, when communicating with their adolescents about cancer. Harsh communication was also positively correlated with solicits, suggesting that maternal harsh communication may include hostile or intrusive questioning. In addition, harsh communication was negatively related to age, suggesting that mothers of older adolescents demonstrated less irritability and frustration with their child. This may be because younger adolescents engage in more behaviors that can evoke harsh responses (e.g., “you’re being a pest,” see Table 1.)
However, neither macro-level communication variables were significantly related to adolescent’s PTSS at T3. Although the mean levels of harsh and withdrawn communication were similar to negative communication composites used in previous research with pediatric asthma samples [30], the standard deviation in the current study was narrower. Thus, the lack of findings may have been partially due to the restricted range of both of these codes in the current sample. In addition, it is important to consider that nine months passed between the communication task at T2 and T3 when other processes may have been unfolding. Of the two micro-level communication variables, solicits were not related to PTSS at either time point. Perhaps soliciting information is too broad a category to be consistently related to distress, and more context is needed about how the mother is asking questions and what information she is soliciting.
Importantly, results indicate that maternal PTSS at T1 had a significant indirect relationship with adolescent PTSS at T3 through maternal validations at T2, such that maternal validations mediated the relation between mothers’ and adolescents’ PTSS. It is noteworthy that even in the absence of significant total and direct effects, a significant indirect effect reflects mediation [33]. Regression analyses indicated that validations remained a significant predictor of PTSS at follow-up, even when controlling for adolescent PTSS at T1. Validations serve to confirm, empathize, or praise the adolescent’s utterance without adding new content, which may be particularly difficult for mothers experiencing heightened levels of PTSS regarding their adolescents’ diagnosis. It appears to be important for mothers to indicate that they are hearing what their child is saying, and to validate their child’s thoughts, ideas, and opinions. Although the number of validations was relatively low in the current sample, the mean and range of validations here are similar to that found in previous studies of parent-child communication in families of healthy children [21,31]; this may speak to the importance of even a small number of validations. Indeed, validating may go beyond allowing an adolescent to share thoughts and emotions about diagnosis and treatment, to communicating that those thoughts and emotions are acceptable (see [31]). In addition, validating may serve to keep the focus of the conversation on the adolescent’s contributions, instead of shifting to the mother’s own experience. This is similar to a previous study that found that confirmations were related to adolescent internalizing symptoms concurrently [21], but this is the first study to examine validations in relation to PTSS in a cancer sample.
Study strengths include the longitudinal, multi-method design that allowed for prospective examination of risk factors near the time of diagnosis and during mother-adolescent communication about cancer. Most previous studies of PTSS in adolescent and young adult cancer survivors were retrospective and unable to draw on important clinical information near the time of diagnosis. This study also included both maternal and adolescent reports as well as direct observation. Observational studies of parent-child communication are rare but gaining attention in pediatric populations (e.g., [9,22,30]), and provide important insights into family functioning and adolescent wellbeing. Although previous studies have examined communication in pediatric oncology specific to other dyads, such as patient-physician (e.g., [37]), this study gives attention to mother-child conversations about cancer.
One study limitation was a relatively small sample size, resulting in the potential for Type II error and relatively low statistical power. The sample also reflected a restricted range of racial and ethnic diversity, and therefore may not be applicable to families of children with cancer that are not Caucasian. For example, some studies have shown that African American parents may demonstrate increased behavioral control and decreased warmth when interacting with their children compared to European American parents [38]. In addition, the study focused on one domain of distress, PTSS, to the exclusion of other outcomes that adolescents may face after cancer diagnosis. Different patterns of communication may be relevant for parental and adolescent symptoms of depression and anxiety. This study also focused on maternal communication; it is possible that different relations would emerge when examining father-child communication. Another limitation is the exclusion of other processes that may be related to adolescent PTSS after cancer diagnosis, including coping and social support.
Given the current findings, an important topic for future research will be to examine PTSS using the DSM-5 model as well as symptom clusters within the new four-factor model [39]. Future work should also more closely examine trajectories of PTSS, to examine which families increase in distress over time and which decrease, and how this might be related to communication (e.g., [40]). In addition, future studies should continue to examine potentially modifiable risk factors and potentially efficacious treatments for adolescents and mothers who experience pediatric cancer as traumatic and continue to evidence symptoms of posttraumatic stress over time. The results of the current study can inform future interventions, including family-based interventions that target both maternal and adolescent symptoms near the time of diagnosis as well as maternal-adolescent communication. Encouraging maternal communication that validates adolescents’ experiences, thoughts, and emotions about their diagnosis and treatment would be an important intervention component.
Contributor Information
Murphy Lexa, Vanderbilt University, Department of Psychology & Human Development.
Rodriguez Erin, Vanderbilt University, Department of Psychology & Human Development.
Gerhardt Cynthia, The Research Institute at Nationwide Children's Hospital, Center for Biobehavioral Health; The Ohio State University, Department of Pediatrics.
Vannatta Kathryn, The Research Institute at Nationwide Children's Hospital, Center for Biobehavioral Health; The Ohio State University, Department of Pediatrics.
Schwartz Laura, The Research Institute at Nationwide Children's Hospital, Center for Biobehavioral Health.
Saylor Megan, Vanderbilt University, Department of Psychology & Human Development.
Bemis Heather, Vanderbilt University, Department of Psychology & Human Development.
Desjardins Leandra, Vanderbilt University, Department of Psychology & Human Development.
Compas Bruce, Vanderbilt University, Department of Psychology & Human Development.
References
- 1.Hobbie WL, Stuber M, Meeske K, Wissler K, Rourke MT, Ruccione K, Kazak AE. Symptoms of posttraumatic stress in young adult survivors of childhood cancer. Journal of Clinical Oncology. 2000;18(24):4060–4066. doi: 10.1200/JCO.2000.18.24.4060. [DOI] [PubMed] [Google Scholar]
- 2.Kazak AE, Kassam-Adams N, Schneider S, Zelikovsky N, Alderfer MA, Rourke M. An integrative model of pediatric medical traumatic stress. Journal of Pediatric Psychology. 2006;31(4):343–355. doi: 10.1093/jpepsy/jsj054. [DOI] [PubMed] [Google Scholar]
- 3.Schwartz L, Drotar D. Posttraumatic stress and related impairment in survivors of childhood cancer in early adulthood compared to healthy peers. Journal of Pediatric Psychology. 2006;31(4):356–366. doi: 10.1093/jpepsy/jsj018. [DOI] [PubMed] [Google Scholar]
- 4.Bruce M. A systematic and conceptual review of posttraumatic stress in childhood cancer survivors and their parents. Clinical Psychology Review. 2006;26(3):233–256. doi: 10.1016/j.cpr.2005.10.002. [DOI] [PubMed] [Google Scholar]
- 5.Stuber ML, Meeske KA, Leisenring W, Stratton K, Zeltzer LK, Dawson K, Krull KR. Defining medical posttraumatic stress among young adult survivors in the Childhood Cancer Survivor Study. General Hospital Psychiatry. 2011;33(4):347–353. doi: 10.1016/j.genhosppsych.2011.03.015. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Alisic E, Jongmans MJ, van Wesel F, Kleber RJ. Building child trauma theory from longitudinal studies: A meta-analysis. Clinical Psychology Review. 2011;31(5):736–747. doi: 10.1016/j.cpr.2011.03.001. [DOI] [PubMed] [Google Scholar]
- 7.Trickey D, Siddaway AP, Meiser-Stedman R, Serpell L, Field AP. A meta-analysis of risk factors for post-traumatic stress disorder in children and adolescents. Clinical Psychology Review. 2012;32(2):122–138. doi: 10.1016/j.cpr.2011.12.001. [DOI] [PubMed] [Google Scholar]
- 8.Barakat L, Kazak AE, Gallagher MA, Meeske K, Stuber ML. Posttraumatic stress symptoms and stressful life events predict the long-term adjustment of survivors of childhood cancer and their mothers. Journal of Clinical Psychology in Medical Settings. 2000;7:189–196. [Google Scholar]
- 9.Dunn MJ, Rodriguez EM, Miller KS, Gerhardt CA, Vannatta K, Saylor MM, Schuele CM, Compas BE. Direct observation of mother-child communication in pediatric cancer: Assessment of verbal and non-verbal behavior and emotion. Journal of Pediatric Psychology. 2011;36:565–575. doi: 10.1093/jpepsy/jsq062. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Vrijmoet-Wiersma CJ, van Klink JM, Kolk AM, Koopman HM, Ball LM, Egeler RM. Assessment of parental psychological stress in pediatric cancer: A review. Journal of Pediatric Psychology. 2008;33(7):694–706. doi: 10.1093/jpepsy/jsn007. [DOI] [PubMed] [Google Scholar]
- 11.Morris A, Gabert-Quillen C, Delahanty D. The association between parent PTSD/depression symptoms and child PTSD symptoms: a meta-analysis. Journal of Pediatric Psychology. 2012;37(10):1076–1088. doi: 10.1093/jpepsy/jss091. [DOI] [PubMed] [Google Scholar]
- 12.Rodriguez EM, Dunn MJ, Zuckerman T, Hughart L, Vannatta K, Gerhardt CA, Compas BE. Mother–Child Communication and Maternal Depressive Symptoms in Families of Children With Cancer: Integrating Macro and Micro Levels of Analysis. Journal of Pediatric Psychology. 2013;38:732–743. doi: 10.1093/jpepsy/jst018. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Kazak AE, Barakat LP, Meeske K, Christakis D, Meadows AT, Casey R, Stuber ML. Posttraumatic stress, family functioning, and social support in survivors of childhood leukemia and their mothers and fathers. Journal of Consulting and Clinical Psychology. 1997;65(1):120. doi: 10.1037//0022-006x.65.1.120. [DOI] [PubMed] [Google Scholar]
- 14.Brown RT, Madan-Swain A, Lambert R. Posttraumatic stress symptoms in adolescent survivors of childhood cancer and their mothers. Journal of Traumatic Stress. 2003;16(4):309–318. doi: 10.1023/A:1024465415620. [DOI] [PubMed] [Google Scholar]
- 15.Scheeringa MS, Zeanah CH. A relational perspective on PTSD in early childhood. Journal of Traumatic Stress. 2001;14(4):799–815. doi: 10.1023/A:1013002507972. [DOI] [PubMed] [Google Scholar]
- 16.Laor N, Wolmer L, Mayes LC, Gershon A, Weizman R, Cohen DJ. Israeli preschool children under Scuds: a 30-month follow-up. Journal of the American Academy of Child & Adolescent Psychiatry. 1997;36(3):349–356. doi: 10.1097/00004583-199703000-00013. [DOI] [PubMed] [Google Scholar]
- 17.Nugent NR, Ostrowski S, Christopher NC, Delahanty DL. Parental posttraumatic stress symptoms as a moderator of child’s acute biological response and subsequent posttraumatic stress symptoms in pediatric injury patients. Journal of Pediatric Psychology. 2007;32(3):309–318. doi: 10.1093/jpepsy/jsl005. [DOI] [PubMed] [Google Scholar]
- 18.van Ee E, Kleber RJ, Mooren T. War trauma lingers on: Associations between maternal posttraumatic stress disorder, parent–child interaction, and child development. Infant Mental Health Journal. 2012;33(5):459–468. doi: 10.1002/imhj.21324. [DOI] [PubMed] [Google Scholar]
- 19.Leen-Feldner EW, Feldner MT, Bunaciu L, Blumenthal H. Associations between parental posttraumatic stress disorder and both offspring internalizing problems and parental aggression within the National Comorbidity Survey-Replication. Journal of Anxiety Disorders. 2011;25(2):169–175. doi: 10.1016/j.janxdis.2010.08.017. [DOI] [PubMed] [Google Scholar]
- 20.Lasky EZ, Klopp K. Parent-child interactions in normal and language-disordered children. Journal of Speech and Hearing Disorders. 1982;47:7–18. doi: 10.1044/jshd.4701.07. [DOI] [PubMed] [Google Scholar]
- 21.Bohanek JG, Fivush R, Zaman W, Lepore CE, Merchant S, Duke MP. Narrative interaction in family dinnertime conversations. Merrill-Palmer Quarterly. 2009;55(4):488–515. doi: 10.1353/mpq.0.0031. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Murray CB, Amaro CM, Devine KA, Psihogios AM, Murphy LK, Holmbeck GN. Observed macro-and micro-level parenting behaviors during preadolescent family interactions as predictors of adjustment in emerging adults with and without spina bifida. Journal of Pediatric Psychology. 2015;40(1):18–32. doi: 10.1093/jpepsy/jsu030. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Lerner RM, Steinberg L. Handbook of Adolescent Psychology, Individual Bases of Adolescent Development. Vol. 1. John Wiley & Sons; 2009. [Google Scholar]
- 24.Hawkins SS, Radcliffe J. Current measures of PTSD for children and adolescents. Journal of Pediatric Psychology. 2006;31(4):420–430. doi: 10.1093/jpepsy/jsj039. [DOI] [PubMed] [Google Scholar]
- 25.Weiss DS, Marmar CR. The Impact of Event Scale–Revised. In: Wilson JP, Keane TM, editors. Assessing psychological trauma and PTSD. New York: Guilford Press; 1997. [Google Scholar]
- 26.Dolgin MJ, Phipps S, Fairclough DL, Sahler OJZ, Askins M, Noll RB, Katz ER. Trajectories of adjustment in mothers of children with newly diagnosed cancer: A natural history investigation. Journal of Pediatric Psychology. 2007;32(7):771–782. doi: 10.1093/jpepsy/jsm013. [DOI] [PubMed] [Google Scholar]
- 27.Kazak AE, Alderfer M, Rourke MT, Simms S, Streisand R, Grossman JR. Posttraumatic stress disorder (PTSD) and posttraumatic stress symptoms (PTSS) in families of adolescent childhood cancer survivors. Journal of Pediatric Psychology. 2004;29(3):211–219. doi: 10.1093/jpepsy/jsh022. [DOI] [PubMed] [Google Scholar]
- 28.Mullins LL, Fedele DA, Chaffin M, Hullmann SE, Kenner C, Eddington AR, McNall-Knapp RY. A clinic-based interdisciplinary intervention for mothers of children newly diagnosed with cancer: a pilot study. Journal of Pediatric Psychology. 2012;37(10):1104–1115. doi: 10.1093/jpepsy/jss093. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Melby JN, Conger RD. The Iowa Family Interaction Rating Scales: Instrument summary. In: Kerig PK, Lindahl KM, editors. Family observational coding systems. Mahwah, NJ: Erlbaum; 2001. pp. 1–22. [Google Scholar]
- 30.Lim J, Wood BL, Miller BD. Maternal depression and parenting in relation to child internalizing symptoms and asthma disease activity. Journal of Family Psychology. 2008;22(2):264. doi: 10.1037/0893-3200.22.2.264. [DOI] [PubMed] [Google Scholar]
- 31.McLean KC, Mansfield CD. The co-construction of adolescent narrative identity: Narrative processing as a function of adolescent age, gender, and maternal scaffolding. Developmental Psychology. 2012;48(2):436. doi: 10.1037/a0025563. [DOI] [PubMed] [Google Scholar]
- 32.Hayes AF. An Introduction to Mediation, Moderation, and Conditional Process Analysis: A Regression-Based Approach. New York, NY: Guilford Press; 2013. [Google Scholar]
- 33.Hayes AF. Beyond Baron and Kenny: Statistical mediation analysis in the new millennium. Communication Monographs. 2009;76(4):408–420. [Google Scholar]
- 34.Harper FW, Peterson AM, Uphold H, Albrecht TL, Taub JW, Orom H, Penner LA. Longitudinal study of parent caregiving self-efficacy and parent stress reactions with pediatric cancer treatment procedures. Psycho-Oncology. 2013;22(7):1658–1664. doi: 10.1002/pon.3199. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Preacher KJ, Kelley K. Effect size measures for mediation models: quantitative strategies for communicating indirect effects. Psychological methods. 2011;16(2):93. doi: 10.1037/a0022658. [DOI] [PubMed] [Google Scholar]
- 36.Pöder U, Ljungman G, von Essen L. Posttraumatic stress disorder among parents of children on cancer treatment: a longitudinal study. Psycho-Oncology. 2008;17(5):430–437. doi: 10.1002/pon.1263. [DOI] [PubMed] [Google Scholar]
- 37.Mellblom AV, Finset A, Korsvold L, Loge JH, Ruud E, Lie HC. Emotional concerns in follow-up consultations between paediatric oncologists and adolescent survivors: a video-based observational study. Psycho-Oncology. 2014 doi: 10.1002/pon.3568. [DOI] [PubMed] [Google Scholar]
- 38.Richman SB, Mandara J. Do socialization goals explain differences in parental control between black and white parents? Family Relations: An Interdisciplinary Journal of Applied Family Studies. 2013;62(4):625–636. [Google Scholar]
- 39.American Psychiatric Association. Diagnostic and statistical manual of mental disorders. (5th ed.) 2013 [Google Scholar]
- 40.Kwak M, Zebrack BJ, Meeske KA, Embry L, Aguilar C, Block R, Cole S. Prevalence and predictors of post-traumatic stress symptoms in adolescent and young adult cancer survivors: a 1-year follow-up study. Psycho-Oncology. 2013;22(8):1798–1806. doi: 10.1002/pon.3217. [DOI] [PubMed] [Google Scholar]