Abstract
Objective: To explore a new identification and protection method of the parathyroid gland in reoperation for thyroid diseases. Method: 54 patients receiving reoperation for thyroid diseases were selected. The experiment group intraoperatively adopted carbon nanoparticles suspension for negative development of the parathyroid gland, whereas the control group did not use carbon nanoparticles suspension. Results: At 48 h after surgery, the parathyroid hormone level was lower than the normal state in 9 patients (33.30%) of the control group and 1 patient (3.70%) of the experiment group; meanwhile, 6 months after surgery, 8 patients of the control group (29.63%) and 1 patient of the experiment group (3.70%) showed a lower level than the normal state with statistical differences. The serum calcium level in 10 patients of the control group (37.04%) and 2 patients of the experiment group (7.41%) was lower than the normal state at 48 h after surgery, while a lower level than the normal state was also shown in 8 patients of the control group (29.63%) and 1 patient of the experiment group (3.70%) 6 months after surgery with statistically significant between the two groups. A total of 10 (37.04%) and 1 parathyroid gland (3.70%) were detected with a statistical difference in both groups. Conclusion: By adopting carbon nanoparticles in reoperation for the thyroid diseases and negative development of the parathyroid gland for identification and protection of the parathyroid gland, the incidence of hypoparathyroidism is reduced effectively, thus improving the postoperative quality of life of the patients.
Keywords: Reoperation for the thyroid diseases, protection of the parathyroid gland, carbon nanoparticles
Introduction
The standard surgeries for thyroid diseases include thyroid lobectomy, near-total thyroidectomy and total thyroidectomy. However, a lack of standardized understanding of resection range for different thyroid gland diseases and wide application of resection of thyroid carcinoma, partial thyroidectomy and other non-standard surgeries in clinical work and especially in the grass-roots hospitals often result in increasing recurrence rate of thyroid diseases and reoperation rate year by year [1]. Whereas, in reoperation, the surgery difficulty and postoperative complications are increased due to organization structure damage, adhesions and scar formation. Among them, the incidence of the parathyroid damage is obviously higher than that in the first surgery, so that the incidence of postoperative permanent hypoparathyroidism markedly rises, thereby affecting seriously the postoperative quality of life of the patients. According to the foreign reports, the incidence of permanent hypoparathyroidism was 3% to 10% after the first surgery for thyroid diseases while 9% to 35% after reoperation [2]. So, how to effectively decrease the probability of the parathyroid damage in reoperation for the thyroid diseases has become a pressing problem for the surgeons in thyroid surgery. In the present experiment, a comparative analysis was made in 54 recurrent thyroid carcinoma patients who were admitted and treated in our department from Jan 2012 to Dec 2014, and the results indicated that intra-operative application of carbon nanoparticles suspension for development of thyroid gland and negative development of the parathyroid gland can significantly reduce the incidence of the parathyroid damage. Now the details are reported below.
Subjects and clinical data
General data
54 patients (4 males and 50 females) with recurrent thyroid carcinoma who were treated in our department from Jan 2012 to Dec 2014 were included in the experiment, with the size of the maximum tumor being 8 cm*5 cm*4 cm and the size of the minimum of 1 cm*1 cm. Among them, 36, 11, 2, 3 and 2 patients were found to have bilateral, left, right, right + isthmus and left + isthmus enlargement, respectively, and the time interval from reoperation to the last surgery was 4 days to 40 years. All patients were randomized into the experiment group and the control group. 27 patients (2 males and 25 females; mean age: 49.4±2.5 (15-71) years) in the experiment group used intraoperatively carbon nanoparticles suspension for negative development of the parathyroid gland. Whereas, 27 patients (2 males and 25 females; mean age: 52.5±1.8 (18-73) years) in the control group did not use intraoperatively carbon nanoparticles suspension. Results of x 2 tests showed no statistical difference in the age, sex and tumor size between two groups (Table 1). The postoperative pathological examination showed nodular goiter in 18 patients, Hashimoto disease in 4 patients, papillocarcinoma in 27 patients, follicular carcinoma in 3 patients and medullary carcinoma in 2 patients. Carbon nanoparticles suspension was provided by Chongqing Lummy Pharmaceutical Co., ltd. As for the data involved and methods used in the paper had been agreed by the patients and approved by the Ethics Committee of the hospital.
Table 1.
Basic information of patients
| Parameters | Experiment group (n=27) | Control group (n=27) | x 2 | P value |
|---|---|---|---|---|
| Age (years old) | 49.4±2.5 | 52.5±1.8 | 5.021 | 1 |
| Minimal age | 15 | 18 | ||
| Maximal age | 71 | 73 | ||
| Gender | 2.773 | 0.5 | ||
| Male | 2 | 2 | ||
| Female | 25 | 25 | ||
| Tumor size (cm) | 5.021 | 1 | ||
| ≤ 2 | 7 | 6 | ||
| 2-4 | 16 | 19 | ||
| ≥ 4 | 4 | 2 | ||
| Location | 13.941 | 1 | ||
| Bilateral | 16 | 20 | ||
| Right | 1 | 1 | ||
| Left | 6 | 5 | ||
| Right + isthmus | 2 | 1 | ||
| Left + isthmus | 2 | 0 |
Surgical procedures
All patients received general anesthesia and surgical methods as shown in Table 2. There was no significant difference of operation methods between two groups. The surgery steps were as follows: after the patient adopted a horizontal and head hyperextension position, an arc incision was made along with the original incision of the neck, and the residual thyroid gland was fully exposed after entering along with the outside of the linea alba cervicalis or sternohyoid muscle. In the experiment group, after exposing the thyroid gland, carbon nanoparticles suspension was injected into the gland from the upper, middle and lower point with a 1 ml syringe, about 0.1 ml for each point, and over-dose must be avoided. Withdrawal was performed while injecting to avoid mistakenly injecting into the vessels (Figure 1). After completing the injection, the injected sites were pressed gently with the gauze for 1-3 min and the thyroid gland was developed (Figure 2). 5 to 10 min later, the lymphatic vessels and lymph nodes were developed whereas the parathyroid glands were not developed (Figure 3). Both groups completed the surgery according to the surgical methods listed in Table 2, and adopted fine anatomy during the surgery while the parathyroid glands and serum supply were protected properly (Figure 4).
Table 2.
Surgical methods
| Surgical methods | N (%) | Experiment group (%) | Control group (%) | x 2 | P value |
|---|---|---|---|---|---|
| Bilateral subtotal resection of thyroid gland | 3 (5.56) | 1 (1.85) | 2 (3.7) | 65.609 | 1 |
| Bilateral total resection of thyroid gland | 9 (16.67) | 4 (7.4) | 5 (9.26) | ||
| Bilateral total resection of thyroid gland, bilateral functional cervical lymphadenectomy | 6 (11.12) | 3 (5.56) | 3 (5.56) | ||
| Bilateral total resection of thyroid gland, right functional cervical lymphadenectomy | 7 (12.96) | 2 (3.7) | 5 (9.26) | ||
| Bilateral total resection of thyroid gland, left functional cervical lymphadenectomy | 9 (16.67) | 6 (11.12) | 3 (5.56) | ||
| Right + isthmus total resection of thyroid gland | 1 (1.85) | 1 (1.85) | 0 (0) | ||
| Right + isthmus total resection of thyroid gland, left functional cervical lymphadenectomy | 1 (1.85) | 0 (0) | 1 (1.85) | ||
| Right + isthmus total resection of thyroid gland, left subtotal resection of thyroid gland, left functional cervical lymphadenectomy | 1 (1.85) | 1 (1.85) | 0 (0) | ||
| Right total resection of thyroid gland | 1 (1.85) | 1 (1.85) | 0 (0) | ||
| Right total resection of thyroid gland, bilateral functional cervical lymphadenectomy | 1 (1.85) | 0 (0) | 1 (1.85) | ||
| Left + isthmus total resection of thyroid gland | 2 (3.7) | 1 (1.85) | 1 (1.85) | ||
| Left + isthmus total resection of thyroid gland, right subtotal resection of thyroid gland | 1 (1.85) | 0 (0) | 1 (1.85) | ||
| Left + isthmus total resection of thyroid gland, right subtotal resection of thyroid gland, left functional cervical lymphadenectomy | 1 (1.85) | 1 (1.85) | 0 (0) | ||
| Left subtotal resection of thyroid gland | 3 (5.56) | 1 (1.85) | 2 (3.7) | ||
| Left subtotal resection of thyroid gland, left functional cervical lymphadenectomy | 1 (1.85) | 1 (1.85) | 0 (0) | ||
| Left total resection of thyroid gland | 7 (12.96) | 4 (7.4) | 3 (5.56) | ||
| Total | 54 (100) | 27 (50) | 27 (50) |
Figure 1.
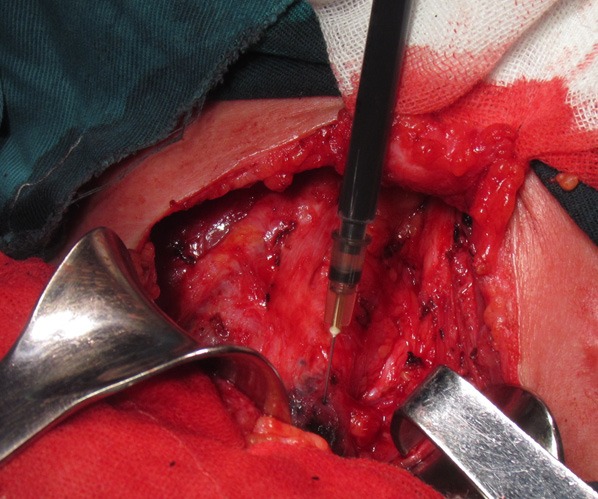
Intra-operative injection of carbon nanoparticles in the experiment group.
Figure 2.
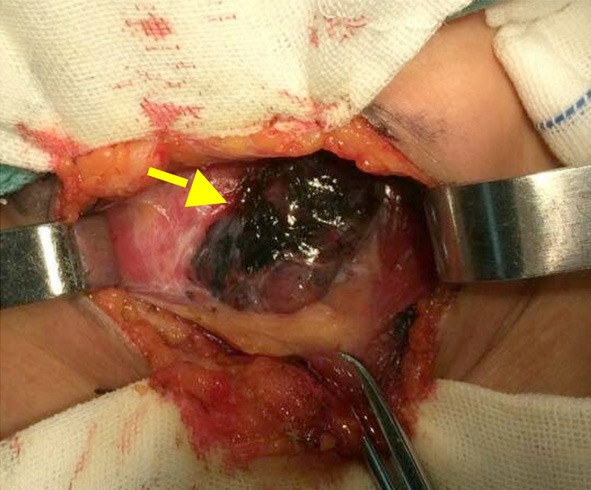
The arrow showing intraoperative development of thyroid gland in the experiment group.
Figure 3.
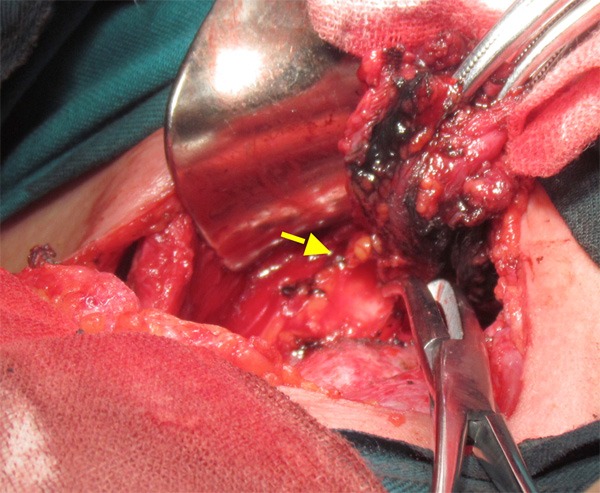
Black-stained thyroid gland during the surgery in the experiment group and the arrow showing negative development of the parathyroid gland in the experiment group.
Figure 4.
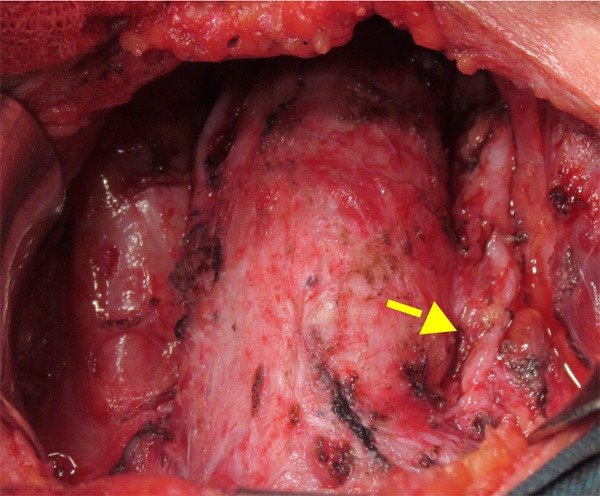
The arrow showing negative development of the parathyroid glands retained in situ after thyroidectomy.
Pre- and post-operative monitoring indicators
Serum calcium and PTH level before surgery and at 48 h and 6 months after surgery as well as number of detected parathyroid glands by postoperative pathological examination in the two groups were recorded. Meanwhile, we also observed whether there were the clinical manifestations such as numbness in the fingers and toes and around the lip after surgery. The normal range of serum parathyroid hormone (PTH) is from 15 to 88 pg/ml, meaning that < 15 pg/ml indicates hypoparathyroidism, and the normal range of serum calcium is between 2.08 and 2.80 mmol/L, indicating that < 2.08 mmol/L can serve as an indicator for hypocalcemia. If serum PTH and calcium level is still lower than the above-mentioned standard value 6 months after surgery, such patients are diagnosed with permanent hypoparathyroidism.
Statistical analysis
SPSS 17.0 was employed for statistical analysis of PTH and serum calcium at 48 h and 6 months after surgery as well as number of the parathyroid glands detected by postoperative pathological examination in the two groups. x2 test was used for inter-group comparison. P < 0.05 was considered statistically significant.
Results
No death was noted in both groups, and no toxic-side effect due to carbon nanoparticles was observed in the experiment group.
Postoperative PTH level
The preoperative PTH levels in both groups were normal. At 48 h after surgery, however, the level was lower than the normal state in 9 patients (33.30%) of the control group and 1 patient (3.70%) of the experiment group; meanwhile, 6 months after surgery, 8 patients of the control group (29.63%) and 1 patient of the experiment group (3.70%) showed a lower level than the normal state. There were statistical differences in the two time points between the two groups. See Table 3.
Table 3.
Comparison of postoperative PTH, serum Ca2+ and number of the parathyroid glands detected between the two groups
| Groups | n | Number of the patients showing lower PTH at 48 h after surgery | Number of the patients showing lower PTH 6 months after surgery | Number of the patients showing lower Ca2+ at 48 h after surgery | Number of the patients showing lower Ca2+ 6 months after surgery | Number of the parathyroid glands detected |
|---|---|---|---|---|---|---|
| Control group | 27 | 9 (33.30%) | 8 (29.63%) | 10 (37.04%) | 8 (29.63%) | 10 (37.04%) |
| Experiment group | 27 | 1 (3.70%) | 1 (3.70%) | 2 (7.41%) | 1 (3.70%) | 1 (3.70%) |
| x 2 | 7.71 | 4.80 | 6.73 | 4.80 | 9.08 | |
| P | 0.005 | 0.028 | 0.009 | 0.028 | 0.003 |
Postoperative serum calcium level
The preoperative serum calcium levels in both groups were normal. At 48 h after surgery, however, the level was lower than the normal state in 10 patients (37.04%) of the control group and 2 patients (7.41%) of the experiment group, and there was a statistical difference between the two groups. Moreover, 6 months after surgery, 8 patients of the control group (29.63%) and 1 patient of the experiment group (3.70%) showed a lower level than the normal state, and a statistical difference was found between the two groups. See Table 3. All the patients showing lower serum calcium than the normal range exhibited different degrees of numbness in the fingers and toes as well as around lips.
Number of the parathyroid glands detected by postoperative pathological examination
A total 10 cases (37.04%) and 1 case (3.70%) of the parathyroid gland(s) were detected in the control group and experiment group, respectively. The difference between the two groups was statistical significant. See Table 3.
Discussion
Hypoparathyroidism is a common complication after surgery for the thyroid diseases, especially after reoperation [3]. The incidence of the parathyroid damage in reoperation is obviously higher than that in the first operation, thus directly leading to a markedly rising incidence of postoperative permanent hypoparathyroidism [4]. The patients with temporary hypoparathyroidism may manifest as numbness in the fingers and toes and around lips, and severe cases may have hypocalcemic tetany, all of which can return to the normal condition after intravenous or oral administration of calcium. Nevertheless, permanent hypoparathyroidism patients might cause a frequent attack of the symptoms such as numbness in the fingers and toes, pain and hypocalcemic tetany, and even induce anxiety, depression, confusion of consciousness and other mental symptoms. So, such patients need long-term oral or intravenous supplement of calcium. If the serum calcium level is lower than the normal value for a long time, apart from long-term symptoms above, bone- and joint-related diseases may also be caused. Additionally, excessive calcium supplement also results in bone- and joint-related diseases as well as stones. Hence, the permanent hypoparathyroidism patients need long-term medical testing and maintaining the serum calcium level, which brings a heavy physical, mental and economic burden to the patients and also promotes occurrence of medical disputes. From this reason, identification and functional protection of the parathyroid glands is particularly significant in the process of reoperation for the thyroid diseases [5].
Concerning protection of the parathyroid gland in the reoperation for the thyroid diseases, some scholars have advocated that, by using “fine dissection operation”, total thyroidectomy is performed during the surgery while the parathyroid glands could be protected. However, in case of the parathyroid ectopia or sanguine in the operative field leading to difficulty for identification, the parathyroid glands are often difficult to note. Meanwhile, as the patients receiving reoperation generally suffer from adhesion and scar formation in the operative area as well as significantly changed anatomical structure, the conventional anatomical landmarks is hard to play a role in seeking parathyroid glands during surgery and is more difficult to identify the parathyroid glands [6]. Moreover, some scholars adopted preoperative ultrasound and intraoperative biological dye. Whereas, because of only 1 mm thickness in normal parathyroid gland and similarity to thyroid echo, the parathyroid glands are different to develop by ultrasound during the surgery. Although nuclide has the advantages of accurate development and high identification rate, it is expensive, has a certain equipment requirements and causes radioactive contamination; furthermore, it may play a role in localizing the parathyroidoma, but is limited in localizing normal parathyroid glands [7]. As for intraoperative use of biological dye (e.g., methylene blue), quick diffusion of methylene blue after injected into the thyroid gland causes blue staining of the parathyroid glands and sentinel lymph nodes of thyroid gland, so that parathyroid gland can not be identified [8-10]. Similarly, applying these methods is ineffective in seeking parathyroid glands intraoperatively. Because the difficulty of identification of the parathyroid gland in reoperation for the thyroid diseases significantly increases, the probability of the parathyroid damage occurring after thyroid lobectomy, near-total thyroidectomy, total thyroidectomy or the standard surgical methods is obviously higher than that after the first surgery, directly causing a obvious increase of the incidence of post-operative permanent hypoparathyroidism. The postoperative hypoparathyroidism and refractory hypocalcemia will seriously affect the quality of life of the patients [11].
Currently, carbon nanoparticles suspension as a lymph node tracer has been used clinically, with the mean diameter of 150 nm and a lymphatic tendency. Since the space between capillary endothelial cells is between 20 and 50 nm while the space between capillary lymphatic endothelial cells ranges from 120 to 150 nm, carbon nanoparticles can cause black-stained lymph nodes but can not enter the capillaries. As a lymph node tracer, carbon nanoparticles have been used for treatment of gastric cancer, breast cancer, colon cancer and other diseases [12-16], but its application in reoperation for the thyroid diseases is rarely reported in clinic. According to the present study, after very few carbon nanoparticles were injected to the residual thyroid glands for reoperation (via the upper, middle and lower point, 0.1 ml each), a better staining of the thyroid gland and the surrounding lymph nodes was reached while the parathyroid glands were not stained. This achieves development of the thyroid gland and the surrounding lymph nodes and negative development of the parathyroid glands. In the surgery, only black-stained tissues needed to be removed while the tissues that were not black-stained were retained, which can not only ensure complete removal of the thyroid gland, but also reserve the parathyroid glands, thereby effectively protecting the parathyroid glands and serum supply during the surgery. There were statistical differences in serum calcium and PTH level at 48 h and 6 months after the surgery and number of the parathyroid gland detected by pathological examination after surgery between the experiment group and the control group. 6 months after surgery, although the parathyroid glands experienced self-compensation, hypocalcemia still occurred in 8 patients of the control group and 1 patient of the experiment group. The aforementioned results indicated that use of carbon nanoparticles in reoperation for the thyroid diseases can effectively reduce the incidence of the parathyroid damage. Through the clinical practice, the author found that the precautions are as follows: (a) we should try to select 1 ml syringe for injection, and the injection volume should not over-dose, 0.1 to 0.2 ml each. If the development is not ideal, we can perform three-point or multi-point injection. (b) the injection point should be selected in the middle of the section of the normal thyroid gland tissues, which should not be too shallow or too deep. Meanwhile, carbon nanoparticles should not be injected into the tumor tissues, trying to select a trisection point or the middle of the gland and avoiding being close to the upper and lower poles. (c) we should know whether there is blood by withdrawal prior to injection. If the injected vessels can not be developed, the force should be small when infusing and the best infusion time is > 1 min. (d) a negative pressure should be adopted to withdraw the needles, and the injection sites should be immediately pressed with the gauze for 1 to 3 min. (e) development of only the thyroid gland and negative development of the parathyroid gland can be reached within 1 min after injection. If the lymph nodes need to be developed, lymph node development of the central area and lateral neck needs waiting 3-5 min and 10 min, respectively. Moreover, prior to injection, only the front of the thyroid gland needs to be exposed, and the lateral and posterior envelope of the thyroid gland should not be damaged. (f) in the operation process, the pseudocapsule of the thyroid gland should be kept intact to prevent leakage of carbon nanoparticles. (g) if there are unstained small nodules on the surface of thyroid gland, additional carbon nanoparticles could be injected to identify the thyroid gland from the parathyroid glands. (h) if the tumor is larger, and there have not been normal thyroid tissues, carbon nanoparticles are not recommended, as the tumor tissues can induce lymphatic obstruction so as to lead to incomplete development.
In short, use of carbon nanoparticles in reoperation for the thyroid diseases, by adopting negative development of the parathyroid gland to identify and protect the parathyroid gland, can effectively decrease the incidence of hypoparathyroidism, thus improving the postoperative quality of life of the patients. Therefore, this method is worthy of clinical application and promotion. However, due to few sample size in the present study, the prospect of this method needs to be further in-depth investigated.
Disclosure of conflict of interest
None.
References
- 1.Dralle H, Lorenz K, Machens A. State of the art: surgery for endemic goiter--a plea for individualizing the extent of resection instead of heading for routine total thyroidectomy. Langenbecks Arch Surg. 2011;396:1137–1143. doi: 10.1007/s00423-011-0809-4. [DOI] [PubMed] [Google Scholar]
- 2.Youssef T, Gaballah G, Abd-Elaal E, El-Dosoky E. Assessment of risk factors of incidental parathyroidectomy during thyroid surgery: a prospective study. Int J Surg. 2010;8:207–211. doi: 10.1016/j.ijsu.2009.12.008. [DOI] [PubMed] [Google Scholar]
- 3.Ban EJ, Yoo JY, Kim WW, Son HY, Park S, Lee SH, Lee CR, Kang SW, Jeong JJ, Nam KH, Chung WY, Park CS. Surgical complications after robotic thyroidectomy for thyroid carcinoma: a single center experience with 3,000 patients. Surg Endosc. 2014;28:2555–2563. doi: 10.1007/s00464-014-3502-1. [DOI] [PubMed] [Google Scholar]
- 4.Duren M, Duh QY, Siperstein AE, Clark OH. Recurrent or persistent thyroid cancer of follicular cell origin. Curr Treat Options Oncol. 2000;1:339–343. doi: 10.1007/s11864-000-0049-2. [DOI] [PubMed] [Google Scholar]
- 5.Thomusch O, Sekulla C, Walls G, Fasshauer M, Dralle H. Analysis of Surgery-Related Complications in Thyroid Carcinoma-A German Prospective Multicentre Study with 275 Patients. Acta Chir Austriaca. 2001;33:194–198. [Google Scholar]
- 6.Chao TC, Jeng LB, Lin JD, Chen MF. Reoperative thyroid surgery. World J Surg. 1997;21:644–647. doi: 10.1007/s002689900287. [DOI] [PubMed] [Google Scholar]
- 7.Akbaba G, Berker D, Isik S, Aydin Y, Ciliz D, Peksoy I, Ozuguz U, Tutuncu YA, Guler S. A comparative study of pre-operative imaging methods in patients with primary hyperparathyroidism: ultrasonography, 99mTc sestamibi, single photon emission computed tomography, and magnetic resonance imaging. J Endocrinol Invest. 2012;35:359–364. doi: 10.3275/7764. [DOI] [PubMed] [Google Scholar]
- 8.Blower PJ, Carter NJ. Rapid preparation of 123I-labelled methylene blue and toluidine blue: potential new agents for parathyroid scintigraphy. Nucl Med Commun. 1990;11:413–420. doi: 10.1097/00006231-199006000-00003. [DOI] [PubMed] [Google Scholar]
- 9.Czerniak A, Zwas ST, Shustik O, Avigad I, Ayalon A, Dolev E. The use of radioiodinated toluidine blue for preoperative localization of parathyroid pathology. Surgery. 1991;110:832–838. [PubMed] [Google Scholar]
- 10.Sippel RS, Elaraj DM, Poder L, Duh QY, Kebebew E, Clark OH. Localization of recurrent thyroid cancer using intraoperative ultrasoundguided dye injection. World J Surg. 2009;33:434–439. doi: 10.1007/s00268-008-9797-0. [DOI] [PubMed] [Google Scholar]
- 11.Miccoli P, Frustaci G, Fosso A, Miccoli M, Materazzi G. Surgery for recurrent goiter: complication rate and role of the thyroid-stimulating hormone-suppressive therapy after the first operation. Langenbecks Arch Surg. 2015;400:253–258. doi: 10.1007/s00423-014-1258-7. [DOI] [PubMed] [Google Scholar]
- 12.Kunisaki C, Yamaoka H, Wakasugi J, Takahashi M, Koizumi Y, Akiyama H, Minabe D, Kunihiro O, Hosaka N, Shimada H. Lymphatic Flow Using Activated Carbon Particle in Lymph Node Metastasis and Skip Metastasis in Gastric Cancer. Jpn J Gastroenterol Surg. 1997;30:2127–2133. [Google Scholar]
- 13.Maruyama K, Sasako M, Kinoshita T, Sano T, Katai H. Can sentinel node biopsy indicate rational extent of lymphadenectomy in gastric cancer surgery? Fundamental and new information on lymph-node dissection. Langenbecks Arch Surg. 1999;384:149–157. doi: 10.1007/s004230050185. [DOI] [PubMed] [Google Scholar]
- 14.Chen J, Wang L, Yao Q, Ling R, Li K, Wang H. Drug concentrations in axillary lymph nodes after lymphatic chemotherapy on patients with breast cancer. Breast Cancer Res. 2004;6:R474–477. doi: 10.1186/bcr819. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Kosuga T, Ichikawa D, Okamoto K, Komatsu S, Shiozaki A, Fujiwara H, Otsuji E. Survival benefits from splenic hilar lymph node dissection by splenectomy in gastric cancer patients: relative comparison of the benefits in subgroups of patients. Gastric Cancer. 2011;14:172–177. doi: 10.1007/s10120-011-0028-2. [DOI] [PubMed] [Google Scholar]
- 16.Yang Q, Wang XD, Chen J, Tian CX, Li HJ, Chen YJ, Lv Q. A clinical study on regional lymphatic chemotherapy using an activated carbon nanoparticle-epirubicin in patients with breast cancer. Tumour Biol. 2012;33:2341–2348. doi: 10.1007/s13277-012-0496-y. [DOI] [PubMed] [Google Scholar]


