Abstract
Background: To evaluate the safety and effectiveness of pedicle screw fixation for treatment of thoracolumbar fracture via Wiltse paraspinal approach. Methods: From June 2009 to June 2012, we enrolled into our study 53 cases of thoracolumbar fractures (single segment compressive or burst fractures) without neurologic injury, among whom 28 were treated by mini-open operation via Wiltse approach (group A) and 25 by conventional posterior open surgery (group B). We recorded and compared the intraoperative and postoperative performance between the two groups. Results: There was no serious complications occurring during our study, such as infection, blood vessel injury, spinal cord or nerve root injury. We did not find any statistically difference between the two groups in corrected rate of Cobb’s angle or vertebral body height (P>0.05). However, the mini-open method had apparent advantages over the conventional open method in operative time, intraoperative blood loss, postoperative drainage, and postoperative improvement on visual analog scale (VAS) scores at 3 days, 1 month, and 6 months after operation (P<0.05). After 9-24-month follow-up, the number of patients with low back pain in group A was less than that in group B. Conclusion: In the premise of strict controlling surgery indications, pedicle screw fixation via Wiltse paraspinal approach has the advantages of simple operation and less trauma in treatment of single-segment thoracolumbar fracture without neurologic injury.
Keywords: Thoracolumbar fracture, wiltse approach, pedicle screw, minimally invasive
Introduction
Posterior thoracolumbar surgery is one of the most common surgical approaches in treatment of thoracolumbar fracture. A wide range of paravertebral muscle splitting and pull in conventional posterior approach cause ischemic necrosis, and denervation in the muscle, leading to flatback deformity and intractable back pain [1]. With the development of minimally invasive theory in orthopedics and medical instrumentation, less invasive stabilization system have been increasingly used to treat thoracolumbar fracture, with preferable clinical outcomes [2-4].
Pedicle screw fixation using mini-open operation via Wiltse approach in treatment of unstable thoracolumbar fractures can effectively restore physiological curvature of the spine, reconstruct vertebral body height, reset the fracture blocks, and achieve the goal of three-dimensional fixation. It has been widely used in clinical work due to the advantages in simple operation and good curative benefit [5].
In the current study, we enrolled 53 patients who had single-segment thoracolumbar fracture, but without neurologic injury, We introduced a novel mini-open pedicle screw fixation via Wiltse approach and compared its reliability and safety with the conventional posterior open method.
Materials and methods
Patients
Fifty-three patients who presented to our department with single-segment thoracolumbar fractures without neurologic injury between June 2009 and June 2012 were enrolled in this study (Table 1). According to ASIA score, they were all at level D or E. The preoperative ratio of the anterior height of the body was 45%-73% (mean 58.6%), the Cobb angle was 15°-34° (mean 23.7°), and average preoperative load-sharing classification of spine fractures was 5.3. We randomized the participants into two groups: mini-open operation via Wiltse approach (Group A, 28 cases) and conventional posterior open approach (Group B, 25 cases). Group A included 19 men and 9 women, aged 27 to 63 years old with median age of 41.4 years (42.3±8.5), among whom 10 cases had pure vertebral compressive fractures and 18 had burst fractures. One patient was in T10, 3 in T11, 10 in T12, 11 in L1 and 3 in L2. Group B included 18 men and 7 women, aged 30 to 61 years old with median age of 44.1 (39.8±7.9), Among whom 8 patients had pure vertebral compressive fractures and 17 had burst fractures. Three patients were in T11, 9 in T12, 8 in L1, 3 in L2 and 2 in L3. There was no statistically significant difference between the two groups in age, gender, fracture type and site (P>0.05).
Table 1.
The features of patients in two groups
| Variable | Group A | Group B | P |
|---|---|---|---|
| Patients (N) | 28 | 25 | |
| Mean age (years) | 42.3±8.5 | 39.8±7.9 | 0.064 |
| Sex ratios (M/F) | 19/9 | 18/7 | 0.058 |
| Mean sagittal Cobb’s angle (°) | 11.5±6.4 (10.2) | 12.3±7.2 (11.6) | 0.061 |
| Mean anterior vertebral body height | 61.4±9.4 (63.1) | 64.7±8.2 (66.8) | 0.052 |
| Mean preoperative load-sharing classification | 4.2±1.9 (5.1) | 4.9±2.1 (5.8) | 0.054 |
Surgical approach
Surgery was performed under general anesthesia and fracture site was determined with locator and C-arm. In group A, patients were in the prone position with vacated abdomen. After a standard prep and drape, four 1.5-2.0 centimeters incisions were made, and dissection was then performed till the outer edge of the facet joints was reached through the intermuscular plane between the multifidus and the longissimus muscules. The pedicle entry point was exposed clearly with the help of mini-retractor. The determination of the entry point was also based on the anatomical landmarks according to the AO method. The guide wire was inserted perpendicular to the corresponding supraspinal ligament, and C-arm was then performed to check whether the guide wire was in the pedicle before pedicle screw placement. If the guide wire was in a satisfactory position, the pedicle screw was inserted; otherwise, position of the guide wire was adjusted. Likewise, after the procedure of rod installation and distraction for restoration, positions of pedicle screws and height of the fractured vertebrae were confirmed using C-arm again (Figure 1). In group B, we first performed a posterior midline incision at the target segment and striped the paraspinal muscle along the spinous process and the vertebral lamina. Then, the facet joints and roots of the transverse process were exposed by an automatic retractor. The entry point was determined based on anatomical landmarks using the same method as group A (Figure 2).
Figure 1.
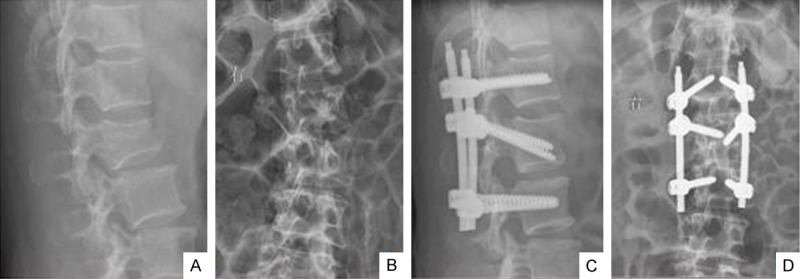
A 56-year old female patient with L2 burst fracture. A and B. Preoperative ratio of the anterior height of the body was 64.3%, the Cobb’s angle was 18°; C and D. Postoperative ratio was 100%, the Cobb’s angle was 4°.
Figure 2.
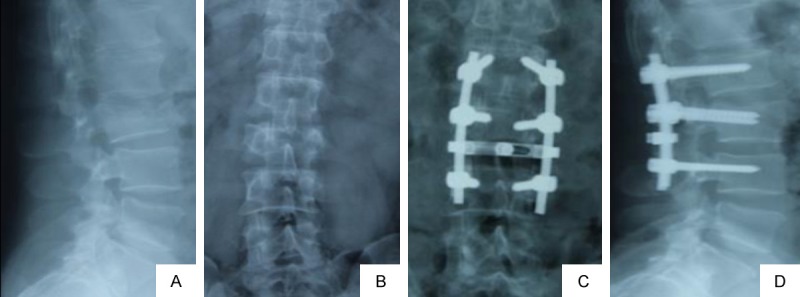
A 63-year old male patient with L2 burst fracture. A and B. Preoperative ratio of the anterior height of the body was 55.3%, the Cobb’s angle was 21°; C and D. Postoperative ratio was 100%, the Cobb’s angle was 2°.
All patients from the mini-open group were mobile with the protection of the waist brace 24 hours after surgery and discharged after an average of 3.4 days after surgery. For those patients who underwent open surgery, the drainage tubes were removed on the second postoperative day, the mean postoperative hospital stay was 9.1 days, and activity was permitted at least two weeks after surgery.
Inspection indicators
We prospectively recorded the intraoperative and postoperative observations in detail and extensively compared several clinical measures between the two groups, including operative time, intraoperative blood loss, postoperative drainage, visual analog scale (VAS) scores at 3 days, 1 month, 6 month after operation, corrected rate of Cobb’s angle and vertebral body height. All patients in the two groups completed the survey independently, without any given suggestions during the investigation.
Statistics
Statistical analysis was done using SPSS 17.0. Measurement data were expressed as mean ± standard deviation, Two-sample-t test was used to compare the measurements between groups. P<0.05 was considered statistically significant.
Results
All patients were operated successfully and did not required intraoperative adjustment. There was no serious complication such as infection, blood vessel injury, spinal cord or nerve root injury. The accuracy of pedicle screw placement was 95.7% and 96.4% in group A and B, respectively. Operative time, intraoperative blood loss, postoperative drainage, VAS scores were significantly different between group A and B (Table 2) (P<0.05). The results showed that the mini-open method was advantageous in these aspects over the conventional open method. Differences were not found in corrected rate of Cobb’s angle and vertebral body height between two groups (Table 3) (P>0.05). All patients were followed up for 9 to 24 months. During this period, 6 patients in group A and 11 in group B complained about low back pain.
Table 2.
Operative time, intraoperative blood loss and postoperative drainage in two groups
| Group | n | Operative time (min) | Intraoperative blood loss (ml) | Postoperative drainage (ml) |
|---|---|---|---|---|
| A | 28 | 78.64±7.51a | 96.97±36.87b | 94.69±34.89b |
| B | 25 | 86.89±6.90 | 261.00±65.55 | 184.85±61.18 |
P<0.05 group A vs group B;
P<0.05 group A vs group B.
Table 3.
VAS scores, corrected rate of Cobb’s angle and vertebral body height in two groups
| Group | N | VAS scores (postoperation) | Corrected rate of Cobb’s angle (%) | Vertebral body height (%) | ||
|---|---|---|---|---|---|---|
|
| ||||||
| 3 days | 1 month | 6 months | ||||
| A | 28 | 3.27±0.89a | 1.72±0.93a | 1.58±0.91a | 91.82±2.09b | 92.17±1.38b |
| B | 25 | 3.98±0.69 | 2.30±0.88 | 2.17±0.97 | 91.64±2.59 | 91.94±1.48 |
P>0.05 group A vs group B;
P<0.05 group A vs group B.
Discussion
Ninety percent of all spine fractures are related to the thoracolumbar region [6]. Especially, the majority of thoracolumbar injuries occur at the T11 to L2 level, which is the biomechanically weak for stress [7]. The primary goals of treatment of thoracolumbar fracture are to keep patients alive, to protect them from further neural damage, to confer stability by reconstructing anatomical alignment of spinal columns, and to allow patients return to workplace through early mobilization and rehabilitation. However, it is still debatable about the treatment methods. Neurologic injury should be identified by thorough physical examination for motor and sensory nerve systems in order to determine the appropriate treatment. The mechanical stability of fracture should also be evaluated by plain radiographs and computed tomography. In some cases, magnetic resonance imaging is required to evaluate soft tissue injury involving neurologic structure or posterior ligament complex. Based on these physical examinations and imaging studies, fracture stability is evaluated and it is determined whether to use the conservative or operative treatment. Recent advancement in instruments has created an increased interest in the operative treatment through minimal invasive approach. The rear of thoracolumbar muscle and ligament plays an important role in maintaining the stability of thoracolumbar segment. Therefore, these muscle and ligament should be protected or restored during operation of thoracolumbar fractures. In the conventional open posterior pedicle screw fixation with posterior midline incision, detachment of the paraspinal muscles may be required to reduce soft tissue ischemia, alleviate dysfunction of the paraspinal muscles and relieve chronic pain [8,9]. In addition, this open approach may be limited by prolonged operative time, increased intraoperative bleeding and delayed functional rehabilitation [10].
In 1968, Wiltse [11] first described the paraspinal sacrospinalis-splitting approach between the multifidus and the longissimus which was associated with less bleeding and tissue dissection compared with the single midline incision approach. Wiltse approach has several advantages: ① avoiding extensive stripping of paraspinal muscle, and electrical-burn damage from electric scalpel; ② shortening mechanical compression by automatic retractor; ③ good operative field and making pedicle screw fixation easier; ④ rapid recovery with slight pain and shorter hospitalization time. In recent years, Wiltse approach has been widely used for lumbar spinal disorders. We used this approach for treatment of thoracolumbar fracture, lumbar spinal revision, lumbar disc herniation lumbar spondylolisthesis and spinal stenosis, and observed satisfactory clinical outcomes. In this series, patients with vertebral burst fracture could get anatomic reduction through this approach, which has the advantages of shorter incision, less blood loss and more simple procedure as compared with conventional approach. At the level of T12, the muscle space is located at about 1.5 cm from the midline, while at the level of L4, it is about 3.5 cm to the midline, from which the transverse process and facet joint of T10-S1 could be easily exposed and the pedicle screws could be inserted precisely [12,13]. During procedure, some small blood vessels give us a reference position that can be easily recognized, ligated or cut to reduce bleeding.
In this study, the results showed that the operative time, intraoperative blood loss, postoperative drainage, and VAS scores were statistically significantly different between the two groups. Wiltse approach showed advantages in these aspects compared with the conventional approach. However, no difference was found in corrected rate of Cobb’s angle and vertebral body height between the two groups, suggesting that mini-open approach was similar to the conventional method in clinical outcomes. Currently the major limitation of the mini-open approach is that it is not suitable for posterior laminectomy and posterolateral fusion. Therefore, our inclusion criteria was strictly limited to cases of single segment thoracolumbar vertebral fractures.
In conclusion, the mini-open surgery via Wiltse approach compared with the traditional surgery several advantages, including less bleeding, shorter operative time, less postoperative pain and tissue trauma, and shorter rehabilitative and hospitalization time. Wiltse approach provides a new alternative for effective management of thoracolumbar fractures.
Acknowledgements
This research was supported by the Science and Technology research funded projects of Ministry of Education of the People’s Republic of China (20110131120062).
Disclosure of conflict of interest
None.
References
- 1.Kim KT, Lee SH, Suk KS, Bae SD. The quantitative analysis of tissue injury markers after mini-open lumber fusion. Spine (Phila Pa 1976) 2006;31:712–6. doi: 10.1097/01.brs.0000202533.05906.ea. [DOI] [PubMed] [Google Scholar]
- 2.Ni WF, Huang YX, Chi YL, Xu HZ, Lin Y, Wang XY, Huang QS, Mao FM. Percutaneous pedicle screw fixation for neurologic intact thoracolumbar burst fractures. J Spinal Disord Tech. 2010;23:530–7. doi: 10.1097/BSD.0b013e3181c72d4c. [DOI] [PubMed] [Google Scholar]
- 3.Wang HW, Li CQ, Zhou Y, Zhang ZF, Wang J, Chu TW. Percutaneous pedicle screw fixation through the pedicle of fractured vertebra in the treatment of type A thoracolumbar fractures using Sextant system: an analysis of 38 cases. Chin J Traumatol. 2010;13:137–45. [PubMed] [Google Scholar]
- 4.Palmisani M, Gasbarrini A, Barbanti GB, De lure F, Cappuccio M, Boriani L, Amendola L, Boriani S. Minimally invasive percutaneous fixation in the treatment of thoracic and lumbar spine fractures. Eur Spine J. 2009;18(Suppl 1):71–4. doi: 10.1007/s00586-009-0989-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Gandhoke GS, Tempel Z, Bonfield CM, Madhok R, Okonkwo DO, Kanter AS. Technical nuances of the minimally invasive extreme lateral approach to treat thoracolumbar burst fractures. Eur Spine J. 2015;24(Suppl 3):353–60. doi: 10.1007/s00586-015-3880-7. [DOI] [PubMed] [Google Scholar]
- 6.Kim BG, Dan JM, Shin DE. Treatment of thoracolumbar fracture. Asian Spine J. 2015;9:133–46. doi: 10.4184/asj.2015.9.1.133. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Gertzbein SD. Scoliosis Research Society. Multicenter spine fracture study. Spine (Phila Pa 1976) 1992;17:528–40. doi: 10.1097/00007632-199205000-00010. [DOI] [PubMed] [Google Scholar]
- 8.Jiang XZ, Tian W, Liu B, Li Q, Zhang GL, Hu L, He D. Comparison of a paraspinal approach with a percutaneous approach in the treatment of thoracolumbar burst fractures with posterior ligamentous complex injury: a prospective randomized controlled trial. J Int Med Res. 2012;40:1343–56. doi: 10.1177/147323001204000413. [DOI] [PubMed] [Google Scholar]
- 9.Olivier E, Beldame J, Ould Slimane M, Ddfives T, Duparc F. Comparison between one midline cutaneous incision and two lateral incisions in the lumbar paraspinal approach by Wiltse: a cadaver study. Surg Radiol Anat. 2006;28:494–7. doi: 10.1007/s00276-006-0123-y. [DOI] [PubMed] [Google Scholar]
- 10.Li HJ, Yang L, Xie H, Yu LP, Wei HF, Cao XJ. Surgical outcomes of mini-open Wiltse approach and conventional open approach in patients with single-segment thoracolumbar fractures without neurologic injury. J Biomed Res. 2015;29:76–82. doi: 10.7555/JBR.29.20140083. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Wiltse LL, Bateman JG, Hutchinson RH, Nelson WE. The paraspinal sacrospinalis-splitting approach to the lumbar spine. J Bone Joint Surg Am. 1968;50:919–26. [PubMed] [Google Scholar]
- 12.Vialle R, Court C, Khouri N, Olivier E, Miladi L, Tassin JL, Defives T, Dubousset J. Anatomical study of the paraspinal approach to the lumbar spine. Eur Spine J. 2005;14:366–71. doi: 10.1007/s00586-004-0802-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Wu H, Wang CX, Gu CY, Zhang ZY, Tong S, Yan HD, Wang JC. Comparison of three different surgical approaches for treatment of thoracolumbar burst fracture. Chin J Traumatol. 2013;16:31–5. [PubMed] [Google Scholar]


