Abstract
Aims: To investigate how specific factors, including knowledge, attitude, use of protective devices, safety climate, workload, and nurses’ behaviors can influence standard precautions in China through structural equation modeling techniques. Background: Although a number of empirical studies have been conducted, an investigation of how multiple variables influence behaviors of standard precautions among the nurses is still needed. Methods: The study was conducted by selecting registered nurses from 25 public hospitals that operate approximately 500 beds located in different areas of Guizhou Province in China. An anonymous, self-administered questionnaire was distributed to 1000 nurses, and 964 (96.4%) completed questionnaires were returned. exploratory factor analysis was employed to examine associations of attitudes, protective devices, safety climate, workload, and nurses’ behaviors with standard precautions. The identified factors were integrated in the proposed structural equation model. Findings: Protective devices had a positive and major influence on nurses’ use of standard precautions. Knowledge had a positive impact on the use of standard precautions through attitude mediation, and the safety climate had a positive impact on the use of standard precautions. In contrast, increasing workload had a negative effect on the use of standard precautions. The factors affecting the use of standard precautions among nurses in order of decreasing effect size were: protective devices, knowledge, attitude, safety climate, and workload. Conclusions: This study offer valuable information for healthcare management regarding the use of standard precautions to reduce occupational exposure among nurses.
Keywords: Nurses, standard precautions, behavior, occupational exposure, blood-borne pathogens
Introduction
Healthcare workers, especially nurses, are at risk of being exposed to blood and body fluids containing blood-borne pathogens (BBPs) [1,2]. The most common BBPs that can be transmitted through occupational exposures are hepatitis B virus (HBV), hepatitis C virus (HCV), and human immunodeficiency virus (HIV) [3]. A seroepidemiological survey on HBV infection in China conducted in 2006 showed that the HBV surface antigen (HBsAg) carrier rate was 7.18% among the overall population [4]. Accordingly, the estimated number of HBV carriers was 93 million, and these include 30 million patients with chronic hepatitis B infection [5]. Another study reported that approximately 780,000 people are living with HIV and AIDS in China [6]. In addition, the incidences of HCV and syphilis have been rapidly increasing in China in recent years [7,8]. Thus, the risk of occupational exposures to these BBPs among nursing staff in China is very high, especially in comparison to risks to nursing staff in other countries where the incidences of these infections are lower [9].
Compliance with standard precautions (SPs) has been regarded as an effective means of preventing occupational exposures to infections (e.g., BBPs). However, SP compliance among health care workers in China has been found to be greatly insufficient [10]. A number of studies have investigated how knowledge of SPs as well as attitude and behavior can influence the practice of SPs [9]. For example, Osborne [10] studied how health beliefs among nurses in operating rooms in Australia influenced their use of double gloves and goggles following the theoretical framework of the health belief model. Researcher [11] investigated associations between organizational factors and standard preventive behaviors. However, these previous studies considered the effects of only some compliance factors on the use of standard precautions (SPs). Moreover, the statistical analysis methods used were univariate analysis or general linear regression, which cannot distinguish correlations between direct and indirect variables nor provide an evaluation of the contribution of each variable and estimates of uncertainty and error.
The SP behaviors are usually associated with many factors (i.e., variables in statistical learning) such as healthcare workers’ knowledge, attitudes, use of protective devices, workload, etc. These variables are also inter-related, making their analysis a causal inference problem, requiring the identification of causal relationships from the sampling data for each variable. In order to address this, a causal model must be established. The most frequently used causal models can be classified as (1) causal Bayesian networks or (2) structural equation models (SEMs) [12].
Apart from causal inference, machine learning techniques also can be employed to establish a predictive model. Machine learning, i.e., learning from data, usually includes supervised learning and unsupervised learning [13]. Supervised learning mainly refers to data used for training the model have got labels; that is, the training data comprise a pair of input vectors along with the corresponding target vectors. In unsupervised learning, the training data consist of a set of input vectors without any corresponding target values. Unsupervised learning is also referred to as density estimation in statistics (e.g., usually presented in a histogram). The goal of such unsupervised learning problems may be to discover groups of similar examples within the data, which is called clustering. The common algorithms used in supervised learning include linear regression, logistic regression, neural networks, and support vector machines. Algorithms that are used for unsupervised learning include clustering, dimension reduction, and others. In addition, other algorithms are available for addressing particular problem such as gradient descent algorithms for regression analysis, back propagation algorithms for neutral networks, and sequential minimal optimization for support vector machines.
In our study, it is known that the use of SPs is related to many variables, some of which are interrelated. Thus, a causal inference approach is appropriate for studying the relationships among these variables and SP use [14]. Whereas causal Bayesian networks specify a density for a variable as a function of the values of its causes, SEMs specify the value of a variable as a function of the values of its causes (typically including some unmeasured noise terms). In this study, a SEM was used to investigate the use of SPs against occupational exposures to blood and bodily fluids among nurses in China. Quantitative analysis of influential factors and a clear understanding of the potential relationship between variables can provide a reference for managing the protection of nurses from occupational exposures. In addition, two levels of analysis, using the measurement model and the structure model, were performed. The measurement model verifies how hypothetical constructs are measured in terms of the observed variables, and the structural model examines the relationships among the constructs [15].
This paper is structured as follows: section 2 describes the methods applied in this research study; section 3 identifies influential factors and proposes a set of hypotheses; section 4 presents the results of the analysis and modeling process; section 5 presents a validation of the hypothesis; and section 6 gives the conclusions.
We described the identification of factors affecting the behaviors of nursing staff with respect to SPs related to occupational exposures and propose a set of hypotheses.
Behavior change is a long and complex process that can be affected by many internal factors such as knowledge, attitudes, intention, self-efficacy, and stress as well as external factors such as social support and environment [16,17]. The behaviors of nursing staff with respect to SPs related to occupational exposures also can be influenced by both internal and external factors, such as the SP knowledge, attitudes, policies, use of safety equipment, organization environment, and human resources [18]. The SEM of factors affecting behaviors regarding SPs related to occupational exposures among nurses was built based on two theoretical framework models: (i) the knowledge, attitude, belief, practice (KABP) model [13], which is a cognitive theory applied to health education that asserts that behavior change involves three processes: acquiring knowledge, coming into belief, and changing behavior. The chain of knowledge, attitude, and behavior primarily explains the effects of personal intrinsic factors on behaviors; and (ii) the precede-proceed model, which is a broad and inclusive framework [19,20] that asserts that three domains can affect behavior: predisposing, enabling, and reinforcing factors. The purpose of the complete model is to change people’s healthy behaviors through both internal factors and external factors. These models are perhaps the most widely used in health promotion, and they have been applied internationally in areas such as community nursing, disease prevention, and self-care [21,22].
Influential factors are related to personal characteristics that affect the likelihood that one will behave in a particular way. These include a person’s attitudes, values, beliefs, knowledge, and existing skills and are best thought of as personal preferences that may facilitate or hinder behavior change. Knowledge has been described as a necessary but insufficient prerequisite for behavior [23]. Whether healthcare workers have sufficient SP knowledge is increasingly attracting more attention [24]. A survey study conducted in China previously reported that Chinese healthcare workers and medical students have considerably limited knowledge of SPs mainly due to deficient learning resources [25,26]. Thus, the following hypotheses were made regarding knowledge.
Hypothesis 1: Knowledge has a positive impact on nurses’ behavioral practice of SPs.
Hypothesis 2: Knowledge has a positive impact on nurses’ attitudes regarding SPs.
Positive attitudes can promote active behaviors, whereas negative attitudes have a negative effect on behaviors. Nurses’ behaviors related to SPs are affected by their attitudes towards occupational exposures to blood and bodily fluids. For example, in many developing countries, knowledge of needle stick injury hazards among healthcare works is insufficient, and therefore, the average worker has a careless attitude toward such injuries in clinical practice [27,28]. Suboptimal adherence to SPs among healthcare workers has been well-documented, with the main given or interpreted reasons being a lack of knowledge, a passive attitude, a lack of time, forgetfulness, and interference with patient care [26]. Hence, the following hypothesis is made.
Hypothesis 3: Attitudes have a positive impact on nursing staff behaviors related to SPs.
Enabling factors can affect the behaviors of both individuals and organizations [18]. Contributing factors to occupational exposure protection are health authorities, hospital protection management systems, safety protection facilities, human resources, and simple processes of escalation and monitoring of occupational exposures. The Blood borne Pathogens Standard released by the Occupational Safety and Health Administration (OSHA) in 1991 and the amendments in the Federal Needle stick Safety and Prevention Act of 2000 require healthcare facilities to implement engineering controls, and the use of personal protective equipment such as gloves, gowns, masks, goggles, and face shields is imperative to prevent sharps injuries and other exposures to blood and bodily fluid [29]. There is evidence of moderate quality that double gloving can reduce the incidences of skin perforations and blood contact during surgery compared to the use of a single pair of gloves, resulting in a decrease in the overall incidence of percutaneous exposures [30]. Thus, two hypotheses were made to examine the impact of the use of safety devices on SP-related behaviors.
Hypothesis 4: Availability and use of the safety devices (device equipment) have a positive impact on nurses’ use of SPs.
Hypothesis 5: Availability and use of the safety devices have a positive effect on nurses’ attitudes regarding SPs.
A previous study reported that workload is one of the most dangerous factors resulting in occupational exposures among nurses [31]. Van Bogaert et al. [32] found that the incidence of needle stick injures was three times higher than normal among nurses with an increased workload. Moreover, when the working staff isinsufficientand resource distribution is imbalanced, the incidence of needle stick injuries was up to twice as high as the incidence under normal conditions. Thus, a reasonable schedule for nurses’ shifts and reduced workload can reduce the incidence of occupational exposures to blood and bodily fluids. In China, there is an insufficient number of nurses, and thus, the workload of nurses is generally heavy, which is likely to impact SP-related behaviors and explain why the occurrence of occupational injuries was found to be increasing in the studies described above. Based on these considerations, the following hypothesis was made.
Hypothesis 6: Increased workload has a negative impact on nurses’ use of SPs.
Reinforcing factors are related to the consequences of behaviors and may affect the likelihood that a behavior will be repeated over time [22]. The precede-proceed model proposes that organizational climate affects behavior change. A favorable atmosphere can promote and maintain behavior change, and safety climate that includes awareness of occupational exposures provides obvious warning signs to healthcare workers. Such a safety climate encourages colleagues to remind each other of risks at work and create a harmonious team spirit. study showed that a good safety climate including an awareness of occupational exposures can improve compliance with SPs among medical staff and reduce the incidence of occupational injuries [33]. To examine the relationship between safety climate and SPs, the following hypothesis was made.
Hypothesis 7: A safety climate has a positive impact on nurses’ use of SPs.
Methods
Aims
To investigate how specific factors, including knowledge, attitude, use of protective devices, safety climate, workload, and nurses’ behaviors can influence standard precautions in China through structural equation modeling techniques.
Participants
We selected 1000 registered practical nurses from 25 public hospitals located in different regions of the Guizhou Province of China (i.e., northern, western, southern, and eastern regions) and operating approximately 500 beds. Among 1000 nurses, 964 nurses responded to the survey, and thus, the response rate was 96.4%.
Data collection
All participants were informed that they had the right to withdraw from the study at any time. The questionnaires were completed anonymously, and no individual’s answers were discussed in this study. The survey was performed from January, 2014 to April, 2014.
Measures
The questionnaire employed in this study was developed after consultations with clinical nursing experts, one education nursing expert, two nursing management experts, one infection control expert, and one medical management expert. The questionnaire was composed of two parts: (i) demographic questions, which requested information regarding gender, age, marital status, work experience, size of hospital department, educational level, and time schedule of shift (day vs. night); and (ii) questions regarding factors affecting the use of SPs, which requested information regarding SP knowledge, attitudes, use of protective devices, safety climate, workload, and behaviors. Each item was scored on a five-point scale ranging from 1 (strongly disagree) to 5 (strongly agree).
Ethical considerations
Approval for this study was obtained from the Institutional Review Board of each hospital.
Data analysis and model testing
The statistical analysis was carried out using the SPSS 18.0 and AMOS 20.0 software packages. First, the demographic profile of the respondents was described. Descriptive survey results were reviewed and interpreted. Following the standard process for structuring a SEM, we first identified a set of factors associated with the behaviors of nursing staff regarding SPs related to occupational exposure and proposed a series of hypotheses. Next, we designed questionnaires based on the proposed hypotheses. Then we analyzed the survey data, including the demographic profiles of the respondents, and examined the reliability and validity of the results. Lastly, we developed the SEM and analyzed the outcomes.
Validity and reliability
The reliability and validity of the results were examined using Cronbach’s alpha as a reliability test and factor analysis for construct validity. Each factor with a reliability coefficient greater than 0.70 was considered to be valid. The Kaiser-Meyer Olkin (KMO) value of 0.925 and Bartlett’s value of 3069.40 (P<0.01) for the scale showed that the sample size was adequate for factor analysis
Results
The demographic characteristics of the respondents are presented in Table 1. Among the 964 nurses included in the study, 94.30% were female, 63.6% were married, and the average age was 29.37±6.93 years old (age range: 18-54 years old). Most nurses worked in a general internal medicine department, surgical department, or intensive care unit (ICU). With respect to education, 88.10% of respondents had a formal educational degree at the bachelors and below bachelors level, and 96.9% had a primary or medium-grade professional title. The night shift rate was 57.3%. Statistical discrepancies within the demographic profile can be attributed to missing data on the survey questionnaire.
Table 1.
Demographic characteristics of respondents (N=964)
| Nurse characteristics | N | % |
|---|---|---|
| Gender | ||
| Male | 55 | 5.7 |
| Female | 909 | 94.3 |
| Age (years) | ||
| 18-35 | 814 | 84.4 |
| 35 | 150 | 15.6 |
| Years in nursing | ||
| 1-10 | 765 | 79.4 |
| >10 | 199 | 20.6 |
| Marital Status | ||
| Married | 613 | 63.6 |
| Single | 351 | 36.4 |
| Department | ||
| Internal Medicine dept. | 227 | 23.5 |
| Surgical dept. | 232 | 24.1 |
| Operating room | 86 | 8.9 |
| Emergency dept. | 88 | 9.1 |
| Pediatric dept. | 77 | 8.0 |
| Gynecology and obstetrics dept. | 72 | 7.5 |
| Intensive care unit (ICU) | 104 | 10.8 |
| Other dept. | 78 | 8.0 |
| Education level | ||
| Doctorate | 1 | 0.1 |
| Masters | 7 | 0.8 |
| Bachelors | 455 | 47.2 |
| Below bachelors | 501 | 52.0 |
| Work shift | ||
| Day shift | 412 | 42.7 |
| Night shift | 551 | 57.3 |
Factor analysis was performed to identify the various aspects of factors affecting the SP-related behavior of nurses. The following reliability coefficients (Cronbach’s alphas) were computed for each factor to estimate the reliability of each subscale: knowledge (0.812), attitude (0.872), protective devices (0.884), safety climate (0.832), workload (0.827), and use of SPs (0.832). We employed the principal component analysis method and Varimax with Kaiser normalization rotation to delineate the underlying dimensions of the scale. All items with factor loadings less than 0.50 were discarded. Finally, 24 observed variables were extracted. The accumulation percentage of the total variance explained was 67.15%, which is greater than 60%. Thus, the construct validity was considered to be good (Table 2).
Table 2.
Observed and latent variables of the improved causal model (N=964)
| Latent variables | Observed variables | Loading | Eigenvalue | Reliability coefficient |
|---|---|---|---|---|
| Protective devices | 2.388 | 0.872 | ||
| Satisfaction with availability of personal protective device in the workplace | 0.90 | |||
| Quality of protective devices | 0.82 | |||
| Personal suitability of protective devices | 0.79 | |||
| Safety climate | 2.667 | 0.832 | ||
| Establishment of occupational exposure management group and assumption of responsibility | 0.72 | |||
| Relevant system and operation regulations for SPs in the clinical department | 0.88 | |||
| Noticeable “warning signs” of SPs in the workplace | 0.80 | |||
| Active participation in SP management | 0.57 | |||
| Workload | 3.242 | 0.827 | ||
| Standing time >4 h/day | 0.52 | |||
| Work fatigue | 0.72 | |||
| Application for annual leave and statutory holiday | 0.63 | |||
| Confrontation with critical patients | 0.69 | |||
| Contact with patients’ blood, bodily fluids, and other secretions | 0.79 | |||
| Contact with blood-borne and infectious agents (e.g., hepatitis B/AIDS/gonorrhea/syphilis) | 0.66 | |||
| Protective knowledge | 2.863 | 0.812 | ||
| Understanding the aim of SPs | 0.61 | |||
| Route of transmission of hepatitis B/AIDS/gonorrhoea/syphilis | 0.74 | |||
| Relevant knowledge of hand hygiene | 0.76 | |||
| Application of SP when touching blood, other bodily fluids, secretions, or excrement using protective devices as instructed | 0.66 | |||
| Classification processing method for medical waste | 0.64 | |||
| Attitudes | 2.476 | 0.884 | ||
| The importance of SPs | 0.78 | |||
| Recognition that all patients’ blood and bodily fluid can be infections | 0.92 | |||
| Necessity of using SPs | 0.87 | |||
| Behaviors | 2.257 | 0.832 | ||
| Wearing masks/gloves and protective goggles when contacting blood or bodily fluids | 0.86 | |||
| Washing hands or using hand sanitizers when contacting different patients | 0.90 | |||
| Placing sharp tools a sharps container immediately after use | 0.64 |
The hypothesized model indicated that as the use of protective devices, SP knowledge, attitudes, and safety climate improved and workload decreased, the practice of SP behaviors among nurses improved. The modified SEM (Figure 1) revealed that the protective devices had a positive impact on the nurses’ use of SPs through direct and indirect impacts. Knowledge had a positive impact on the nurses’ use of SPs through attitude mediation, and safety climate also had a positive impact on the nurses’ standard precautions. In contrast, the effect of increasing workload was negative. Fit indices of CMIN=degrees of freedom (df)¼ 2.146, comparative fit index (CFI)¼ 0.866, normalized fit index (NFI)¼ 0.740, and root mean square error of approximation (RMSEA)¼ 0.062 reveal that fit indices of goodness of fit index (GFI), NFI non-normalized fit index (NNFI), comparative fit index (CFI), incremental fit index (IFI), adjusted goodness of fit index (AGFI), and relative fit index (RFI) were greater than 0.9 individually, and those of root mean square residual (RMR), standardized root mean square residual (SRMR), and RESEA (root mean square error of approximation). RMSEA were less than 0.08 individually (X2/df=0.804). Also, the model fit the data well, indicating a good construct of variables.
Figure 1.
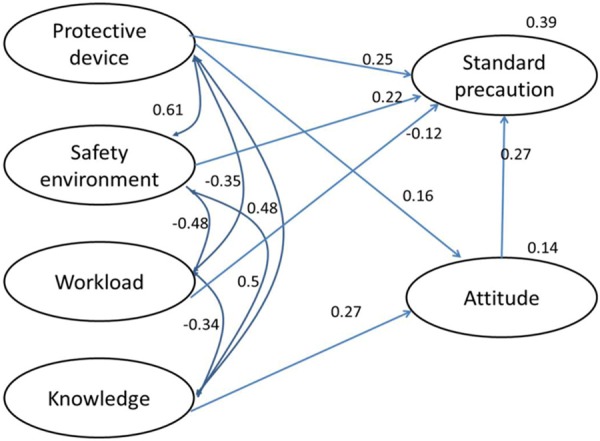
Structural equation modeling.
The pathway analysis of influential variables in the modified SEM provided the following results. Overall, the factors affecting the practice of SPs related to occupational exposures among the nurses could be ordered according to descending magnitude of effect as: protective devices, knowledge, attitudes, safety climate, and workload (Table 3).
Table 3.
Pathway analysis of variable factors affecting behavior
| External latent variables | Internal latent variables | Direct impact | Indirect impact | Overall impact |
|---|---|---|---|---|
| Knowledge | SP behaviors | - | 0.074 | 0.074 |
| Attitudes | SP behaviors | 0.272 | - | 0.272 |
| Protective devices | SP behaviors | 0.249 | 0.044 | 0.293 |
| Safety climate | SP behaviors | 0.220 | - | 0.220 |
| Workload | SP behaviors | -0.118 | - | -0.118 |
Discussion
The results of this study provided support for the hypothesized model of inter-related internal and external factors including knowledge, attitudes, protective devices, safety climate, workload, and SP behaviors related to occupational exposures to blood and bodily fluids among nurses in China.
The modified SEM showed that the variable protective devices was associated with the attitude variable and had a direct impact on SP-related behavior, with coefficients for direct and indirect effects of 0.249 and 0.044, respectively. The total coefficient of 0.293 made it the most influential factor among six variable factors analyzed. The precede-proceed theory considers the use of protective equipment as a behavioral change and alleges that external and internal factors can affect both behavior and each other. However, compared with the internal factors, external factors have a stronger impact on behavior change. The precede-proceed theory also suggests that good preventive measures can promote the use of SPs directly and, at the same time, deepen nurses’ awareness of occupational exposures and further promote behavioral change, which is consistent with the results of the present study. However, in developing countries, measures such as safe usage of needle are not often available, because of nurses’ poor compliance with SPs related to occupational exposure. This is a key factor in the high incidence of occupational exposures. The results of this study further indicate that improving nurses’ knowledge of SPs as well as attitudes regarding SPs is not sufficient to ensure sufficient compliance is achieved, because many protective devices are of poor quality and inadequate. In fact, most protective devices are not suitable or accessible. Hospital management departments should offer the preventive devices needed to meet the demand of clinical practice and improve compliance with SPs.
Knowledge and attitudes regarding SPs are internal factors that affect protective behaviors. The SEM showed they are the second and third most influential factors, and after protective devices, SP knowledge has the greatest positive influence on protective behaviors through attitudes as an intermediary factor. According to the KABP model, a change in human behavior occurs via three consecutive processes composed of acquisition of knowledge, belief, and behavior. Thus, the theory indicates that a cause and effect relationship exists among knowledge, attitude, and behavior. Knowledge is the foundation of the attitude, and attitude provides the power for a behavior change. Aquiring more knowledge does not directly improve behavior. However, with knowledge and a right attitude and strong desire, people can overcome difficulties by translating knowledge into actions.
A safety climate has a positive effect on the use of SPs, with a total coefficient of 0.22. From the results of the research, the safety climate only affects protection behaviors after other variables are in place, namely, SP knowledge and a proper attitude regarding SPs. Based on the precede-proceed theory, a safety culture and safety environment within an organization are considered reinforcing factors for behavior change. A good safety culture can promote behavioral translation of knowledge. Previous studies have shown that the environment of an organization can affect the incidence of occupational exposures [34]. Hospital managers should establish a good system for encouraging occupational precautions and build a good saftely culture. The importance of SPs related to health protection should be prominent, and the issues of occupational safety and harmonious relationships between colleagues should be watched closely. Managers should remind colleagues of unsafe operations, and every staff member must take responsibility in ensuring the safest working environment. Meanwhile, managers should increase the awareness of senior personnel of the need to participate in occupational safety management and allow them to play the roles of administrators.
Workload had a negative effect on the use of SPs related to occupational exposures, and the total coefficient was -0.118. This result means that as the workload of the nursing staff increases, compliance with SPs worsens. Previous studies have shown that with the shortage of nurses in China and the corresponding increase in nursing labor intensity and work pressure, nurses cannot concentrate on their work as well and may easily suffer sharps-related injuries [35]. Also, they do not have time to report injuries or are unwilling to do so. They may perceived that reporting such an injury will only result in their being blamed for noncompliance with SPs, and for this reason, they may refuse to report these injuries. The present study shows that workload is associated with compliance with SPs. This result suggests that hospital managers need to increase human resources appropriately, reduce the amount of time nurses spend standing while at work, reduce work intensity in other ways, and improve compliance with SPs in order to reduce unsafe occupational factors.
Study limitations
There are some limitations in this study. First, the results are based on a theoretical model, and the clinical effects have not yet been determined but will be investigated further. Secondly, it is assumed that the subjects of the SEM are from the same province rather than from all over the China. Thus, there are certain geographical limitations to data completeness. Thirdly, this study applied a cross-sectional survey and investigated the work conditions of nurses over only 1 year. Therefore, the reliability of the data is not too strong.
Conclusion
This study employed a SEM to explore the factors affecting the practice of SPs related to occupational exposures to blood and bodily fluids among hospital nurses. We tested medical factors through a modified SEM. Each evaluation of the model showed that it was steady and met the requirements for validity. Factors influencing behavior were quantified, and the model indicated the key factors and secondary factors as well as the interactions between these factors. The results revealed that the practice of occupational SPs is mainly influenced by the use of protective devices, knowledge of SPs, attitudes towards SPs, and by both internal factors and external factors. Safety climate and workload also affected compliance with SPs to a certain degree. Nursing staff management should provide macro-level control and guidance to establish a protection policy related to occupational exposures and a comprehensive intervention policy for improve nursing staff compliance with SPs related to occupational exposures. A safe working environment is a necessity for any clinical nursing staff.
Acknowledgements
The study was supported by Science and Technology Office of Guizhou Province (The fund number is [2013] 7005).
Disclosure of conflict of interest
None.
References
- 1.Gorar ZA, Butt ZA, Aziz I. Risk factors for bloodborne viral hepatitis in healthcare workers of Pakistan: a population based case-control study. BMJ Open. 2014;4:e004767. doi: 10.1136/bmjopen-2013-004767. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Mohammadi N, Allami A, Malek Mohamadi R. Percutaneous exposure incidents in nurses: Knowledge, practice and exposure to hepatitis B infection: Percutaneous exposure incidents in nurses. Hepat Mon. 2011;11:186–190. [PMC free article] [PubMed] [Google Scholar]
- 3.MacCannell T, Laramie AK, Gomaa A, Perz JF. Occupational exposure of health care personnel to hepatitis B and hepatitis C: prevention and surveillance strategies. Clin Liver Dis. 2010;14:23–36. vii. doi: 10.1016/j.cld.2009.11.001. [DOI] [PubMed] [Google Scholar]
- 4.Lu F, Zhuang H. Management of hepatitis B in China. Chin Med J (Engl) 2009;122:3–4. [PubMed] [Google Scholar]
- 5.Ott JJ, Stevens GA, Wiersma ST. The risk of perinatal hepatitis B virus transmission: hepatitis B e antigen (HBeAg) prevalence estimates for all world regions. BMC Infect Dis. 2012;12:131. doi: 10.1186/1471-2334-12-131. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Rao D, Chen W, Pearson C, Simoni J, Fredriksen-Goldsen K, Nelson K, Zhao H, Zhang F. Social support mediates the relationship between HIV stigma and depression/quality of life among people living with HIV in Beijing, China. Int J STD AIDS. 2012;23:481–484. doi: 10.1258/ijsa.2009.009428. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Hao C, Yan H, Yang H, Huan X, Guan W, Xu X, Zhang M, Tang W, Wang N, Gu J, Lau JT. The incidence of syphilis, HIV and HCV and associated factors in a cohort of men who have sex with men in Nanjing, China. Sex Transm Infect. 2011;87:199–201. doi: 10.1136/sti.2010.042903. [DOI] [PubMed] [Google Scholar]
- 8.Liu J, Huang Y, Wang J, Guo N, Li J, Dong X, Ma H, Tiemuer M, Huang M, Wright DJ. The increasing prevalence of serologic markers for syphilis among Chinese blood donors in 2008 through 2010 during a syphilis epidemic. Transfusion. 2012;52:1741–1749. doi: 10.1111/j.1537-2995.2011.03527.x. [DOI] [PubMed] [Google Scholar]
- 9.Liu XN, Sun XY, van Genugten L, Shi YH, Wang YL, Niu WY, Richardus JH. Occupational exposure to blood and compliance with standard precautions among health care workers in Beijing, China. Am J Infect Control. 2014;42:e37–38. doi: 10.1016/j.ajic.2013.12.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Osborne S. Influences on compliance with standard precautions among operating room nurses. Am J Infect Control. 2003;31:415–423. doi: 10.1067/mic.2003.68. [DOI] [PubMed] [Google Scholar]
- 11.Brevidelli MM, Cianciarullo TI. Psychosocial and organizational factors relating to adherence to standard precautions. Rev Saude Publica. 2009;43:907–916. doi: 10.1590/s0034-89102009010700001. [DOI] [PubMed] [Google Scholar]
- 12.Tabri N, Elliott CM. Principles and practice of structural equation modeling. Canad Grad J Soc Crimin. 2012;1:59–60. [Google Scholar]
- 13.Bishop CM. Pattern recognition and machine learning. New York: Springer; 2006. [Google Scholar]
- 14.Spirtes P. Introduction to causal inference. J Mach Learn Res. 2010;11:1643–1662. [Google Scholar]
- 15.Hoe SL. Issues and procedures in adopting structural equation modeling technique. J Appl Quant Method. 2008;3:76–83. [Google Scholar]
- 16.Janßen C, Pfaff H. Psychosocial environments. Oxford, UK: Elsevier; 2005. [Google Scholar]
- 17.Luszczynska A, Sutton S. ABC of behavior change. Oxford, UK: Elsevier; 2005. Attitudes and expectations; pp. 71–84. [Google Scholar]
- 18.Mandana BN, Losimba LJ. Healthcare professionals’ knowledge, attitudes and practices in relation to standard hospital precautions. Sante publique (Vandoeuvre-les-Nancy, France) 2012;25:663–673. [PubMed] [Google Scholar]
- 19.Sharma M, Romas JA. Theoretical foundations of health education and health promotion. Jones & Bartlett Publishers; 2011. [Google Scholar]
- 20.Tramm R, McCarthy A, Yates P. Using the Precede-Proceed Model of Health Program Planning in breast cancer nursing research. J Adv Nurs. 2012;68:1870–1880. doi: 10.1111/j.1365-2648.2011.05888.x. [DOI] [PubMed] [Google Scholar]
- 21.Kattelmann KK, White AA, Greene GW, Byrd-Bredbenner C, Hoerr SL, Horacek TM, Kidd T, Colby S, Phillips BW, Koenings MM. Development of Young Adults Eating and Active for Health (YEAH) Internet-based intervention via a community-based participatory research model. J Nutr Edu Behav. 2014;46:S10–S25. doi: 10.1016/j.jneb.2013.11.006. [DOI] [PubMed] [Google Scholar]
- 22.Kawamura M, Komabayashi T, Sasahara H, Okada M, Taguchi N, Ogawa T. PRECEDEPROCEED model modification in communitybased oral health promotion by using the linear structural relations programme. Oral Heal Prevent Dent. 2009;8:315–321. [PubMed] [Google Scholar]
- 23.Tso DK, Athreya S. Reducing blood-borne exposure in interventional radiology: what the IR should know. Cardiovasc Interven Radiol. 2013;36:913–916. doi: 10.1007/s00270-013-0580-8. [DOI] [PubMed] [Google Scholar]
- 24.Mehrdad R, Meshki M, Pouryagub G. Effects of training course on occupational exposure to bloodborne pathogens: a controlled interventional study. Int J Prev Med. 2013;4:1236–1242. [PMC free article] [PubMed] [Google Scholar]
- 25.Yao WX, Wu YL, Yang B, Zhang LY, Yao C, Huang CH, Qian YR. Occupational safety training and education for needlestick injuries among nursing students in China: Intervention study. Nurse Educ Today. 2013;33:834–837. doi: 10.1016/j.nedt.2012.02.004. [DOI] [PubMed] [Google Scholar]
- 26.Zhou Y, Zhang D, Chen Y, Zhou S, Pan S, Huang Y, Ba-Thein W. Healthcare-associated infections and shanghai clinicians: a multicenter cross-sectional study. PLoS One. 2014;9:e105838. doi: 10.1371/journal.pone.0105838. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Habib F, Khan DK, Bhatti F, Zafar A. Knowledge and beliefs among health care workers regarding hepatitis B infection and needle stick injuries at a tertiary care hospital, karachi. J Coll Phys Surg Pakistan. 2011;21:317. [PubMed] [Google Scholar]
- 28.Memish ZA, Assiri AM, Eldalatony MM, Hathout HM, Alzoman H, Undaya M. Risk analysis of needle stick and sharp object injuries among health care workers in a tertiary care hospital (Saudi Arabia) J Epidemiol Glob Health. 2013;3:123–129. doi: 10.1016/j.jegh.2013.03.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Vadgama A. OSHA Bloodborne Pathogens Standard Revisited Impact of the Needlestick Safety and Prevention Act. Professional Safety. 2002;47:42–48. [Google Scholar]
- 30.Mischke C, Verbeek JH, Saarto A, Lavoie MC, Pahwa M, Ijaz S. Gloves, extra gloves or special types of gloves for preventing percutaneous exposure injuries in healthcare personnel. Cochrane Database Syst Rev. 2014 doi: 10.1002/14651858.CD009573.pub2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Aiken LH, Clarke SP, Sloane DM, Sochalski J, Silber JH. Hospital nurse staffing and patient mortality, nurse burnout, and job dissatisfaction. Jama. 2002;288:1987–1993. doi: 10.1001/jama.288.16.1987. [DOI] [PubMed] [Google Scholar]
- 32.Van Bogaert P, Clarke S, Willems R, Mondelaers M. Nurse practice environment, workload, burnout, job outcomes, and quality of care in psychiatric hospitals: a structural equation model approach. J Adv Nurs. 2013;69:1515–1524. doi: 10.1111/jan.12010. [DOI] [PubMed] [Google Scholar]
- 33.Gershon RR, Stone PW, Zeltser M, Faucett J, MacDavitt K, Chou SS. Organizational climate and nurse health outcomes in the United States: a systematic review. Ind Health. 2007;45:622–636. doi: 10.2486/indhealth.45.622. [DOI] [PubMed] [Google Scholar]
- 34.Dehdashti A. A Structural Equation Modelling method to describe work environment risk factors and musculoskeletal symptoms among hospital nurses. Occup Environ Med. 2014;71:A68. [Google Scholar]
- 35.Lin PH, Tsai YA, Chen WC, Huang SF. Prevalence, characteristics, and work-related risk factors of low back pain among hospital nurses in Taiwan: a cross-sectional survey. Int J Occup Med Environ Heal. 2012;25:41–50. doi: 10.2478/s13382-012-0008-8. [DOI] [PubMed] [Google Scholar]


