Abstract
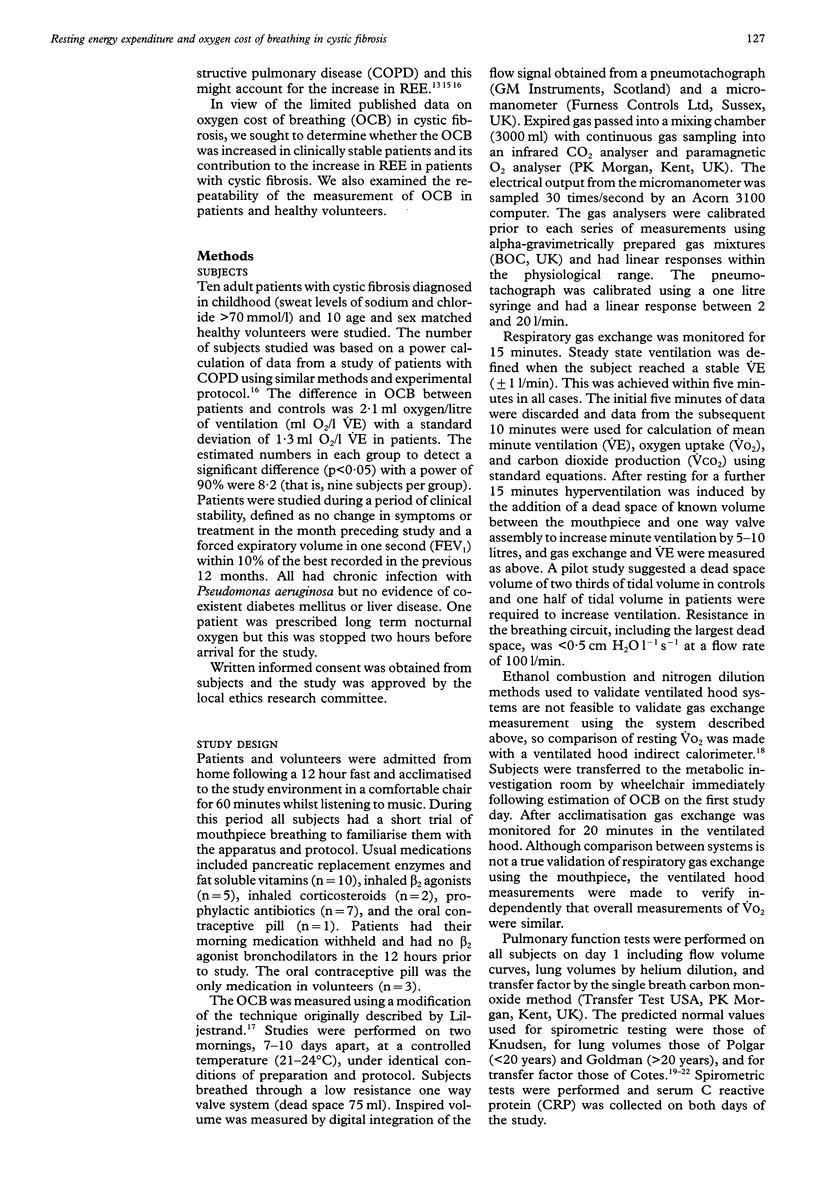
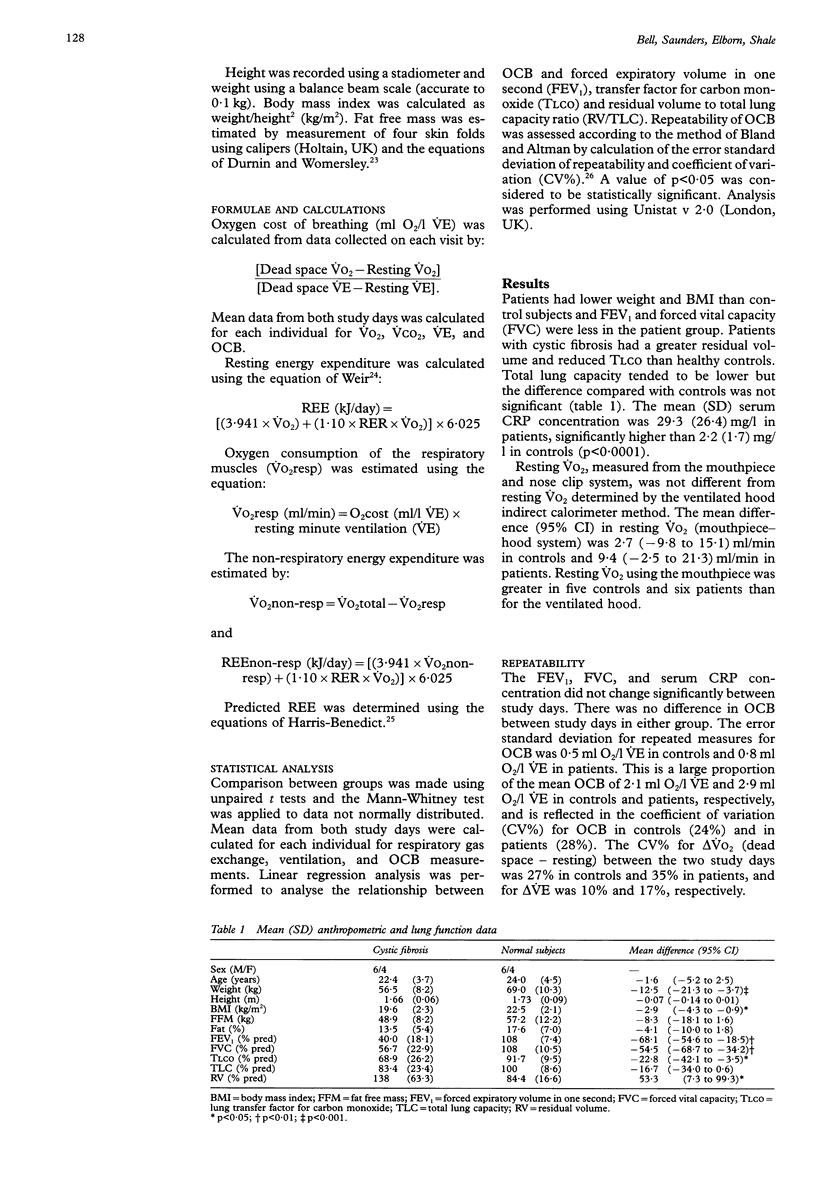
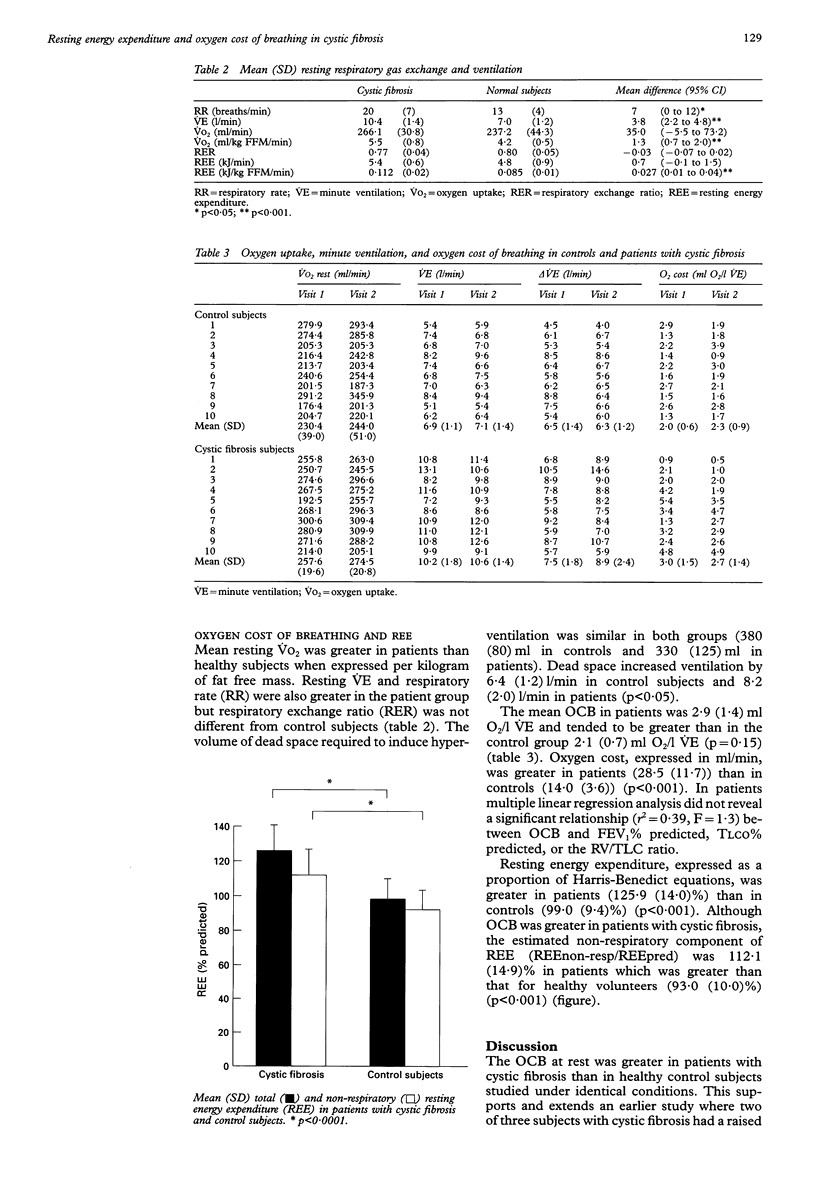
BACKGROUND: Resting energy expenditure (REE) is often increased and may contribute towards energy imbalance in patients with cystic fibrosis. Several mechanisms may lead to increased REE including the gene defect, the effect of chronic infection, and abnormal pulmonary mechanics. Increased oxygen cost of breathing (OCB) has been demonstrated in patients with chronic obstructive pulmonary disease (COPD), but has not been the subject of extensive study in cystic fibrosis. METHODS: Ten clinically stable patients with cystic fibrosis and 10 healthy control subjects were studied. OCB was estimated using the dead space hyperventilation method. Mixed expired gas fractions were measured by online gas analysers and ventilation by a pneumotachograph. After measurement of resting ventilation and gas exchange, minute ventilation (VE) was stimulated by 6-10 1/min by the addition of a dead space and OCB calculated from the slope of the differences in oxygen uptake (VO2) and VE. REE and the non-respiratory component of REE were calculated from gas exchange data. To assess the repeatability of OCB all subjects had a further study performed one week later. RESULTS: The patients had lower weight, fat free mass (FFM), forced expiratory volume in one second (FEV1), forced vital capacity (FVC), and transfer factor for carbon monoxide (TLCO) than controls. Resting respiratory rate, VE, and oxygen uptake per kilogram of FFM (VO2/kg FFM) were higher in patients (20 (7), 10.4 (1.4) 1/min and 5.5 (0.8) ml/kg FFM/min) than in controls (13 (4), 7.0 (1.2), and 4.2 (0.5), respectively.) The error standard deviation for replicated measures of OCB was 0.5 ml O2/l VE in controls and 0.8 ml O2/l VE in patients with coefficients of variation of 24% in controls and 28% in patients. The mean OCB in patients was 2.9 (1.4) ml O2/l VE and 2.1 (0.7) ml O2/l VE in controls. OCB, expressed as ml/min (VO2resp) was 28.5 (11.7) in patients and 14.0 (3.6) in controls. REE was higher in patients (125.9 (14.0)% predicted) than in controls (99.0 (9.4)%). The estimated non-respiratory component of REE was 112.1 (14.9)% for patients and 93.0 (10.0)% for controls. CONCLUSIONS: In clinically stable patients with cystic fibrosis the OCB at rest is increased but is not the sole explanation for increased metabolic rate. This contrasts with the finding in COPD where the increase in REE is largely explained by increased OCB. This study also showed poor repeatability and OCB measurements similar to earlier studies, which indicates that the technique is not suitable for longitudinal studies.
Full text
PDF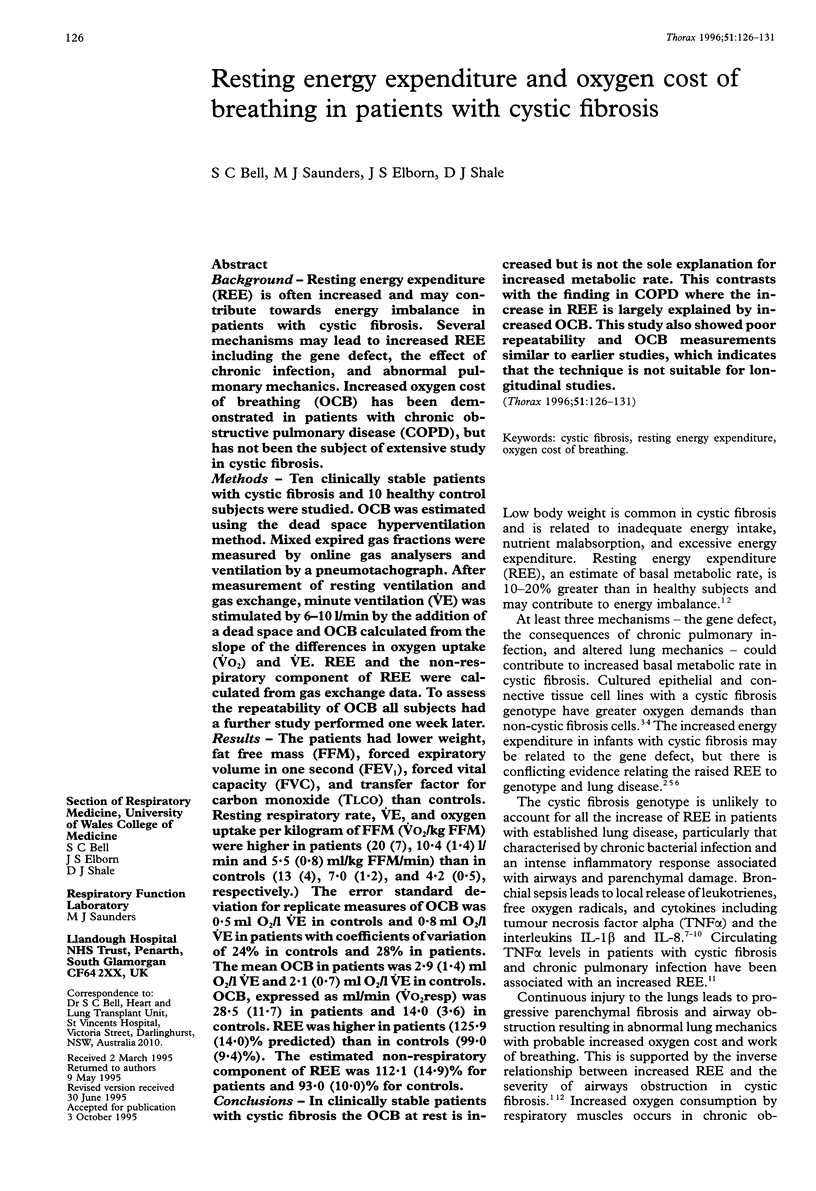
Selected References
These references are in PubMed. This may not be the complete list of references from this article.
- BARTLETT R. G., Jr, BRUBACH H. F., SPECHT H. Oxygen cost of breathing. J Appl Physiol. 1958 May;12(3):413–424. doi: 10.1152/jappl.1958.12.3.413. [DOI] [PubMed] [Google Scholar]
- Bland J. M., Altman D. G. Statistical methods for assessing agreement between two methods of clinical measurement. Lancet. 1986 Feb 8;1(8476):307–310. [PubMed] [Google Scholar]
- Buchdahl R. M., Cox M., Fulleylove C., Marchant J. L., Tomkins A. M., Brueton M. J., Warner J. O. Increased resting energy expenditure in cystic fibrosis. J Appl Physiol (1985) 1988 May;64(5):1810–1816. doi: 10.1152/jappl.1988.64.5.1810. [DOI] [PubMed] [Google Scholar]
- CAMPBELL E. J., WESTLAKE E. K., CHERNIACK R. M. Simple methods of estimating oxygen consumption and efficiency of the muscles of breathing. J Appl Physiol. 1957 Sep;11(2):303–308. doi: 10.1152/jappl.1957.11.2.303. [DOI] [PubMed] [Google Scholar]
- CAMPBELL E. J., WESTLAKE E. K., CHERNIACK R. M. The oxygen consumption and efficiency of the respiratory muscles of young male subjects. Clin Sci. 1959 Feb;18(1):55–64. [PubMed] [Google Scholar]
- CHERNIACK R. M. The oxygen consumption and efficiency of the respiratory muscles in health and emphysema. J Clin Invest. 1959 Mar;38(3):494–499. doi: 10.1172/JCI103826. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cotton C. U., Stutts M. J., Knowles M. R., Gatzy J. T., Boucher R. C. Abnormal apical cell membrane in cystic fibrosis respiratory epithelium. An in vitro electrophysiologic analysis. J Clin Invest. 1987 Jan;79(1):80–85. doi: 10.1172/JCI112812. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Donahoe M., Rogers R. M., Wilson D. O., Pennock B. E. Oxygen consumption of the respiratory muscles in normal and in malnourished patients with chronic obstructive pulmonary disease. Am Rev Respir Dis. 1989 Aug;140(2):385–391. doi: 10.1164/ajrccm/140.2.385. [DOI] [PubMed] [Google Scholar]
- Durnin J. V., Womersley J. Body fat assessed from total body density and its estimation from skinfold thickness: measurements on 481 men and women aged from 16 to 72 years. Br J Nutr. 1974 Jul;32(1):77–97. doi: 10.1079/bjn19740060. [DOI] [PubMed] [Google Scholar]
- Elborn J. S., Cordon S. M., Western P. J., Macdonald I. A., Shale D. J. Tumour necrosis factor-alpha, resting energy expenditure and cachexia in cystic fibrosis. Clin Sci (Lond) 1993 Nov;85(5):563–568. doi: 10.1042/cs0850563. [DOI] [PubMed] [Google Scholar]
- Feigal R. J., Shapiro B. L. Mitochondrial calcium uptake and oxygen consumption in cystic fibrosis. Nature. 1979 Mar 15;278(5701):276–277. doi: 10.1038/278276a0. [DOI] [PubMed] [Google Scholar]
- GOLDMAN H. I., BECKLAKE M. R. Respiratory function tests; normal values at median altitudes and the prediction of normal results. Am Rev Tuberc. 1959 Apr;79(4):457–467. doi: 10.1164/artpd.1959.79.4.457. [DOI] [PubMed] [Google Scholar]
- Girardet J. P., Tounian P., Sardet A., Veinberg F., Grimfeld A., Tournier G., Fontaine J. L. Resting energy expenditure in infants with cystic fibrosis. J Pediatr Gastroenterol Nutr. 1994 Feb;18(2):214–219. doi: 10.1097/00005176-199402000-00015. [DOI] [PubMed] [Google Scholar]
- Greally P., Hussein M. J., Cook A. J., Sampson A. P., Piper P. J., Price J. F. Sputum tumour necrosis factor-alpha and leukotriene concentrations in cystic fibrosis. Arch Dis Child. 1993 Mar;68(3):389–392. doi: 10.1136/adc.68.3.389. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Katsardis C. V., Desmond K. J., Coates A. L. Measuring the oxygen cost of breathing in normal adults and patients with cystic fibrosis. Respir Physiol. 1986 Sep;65(3):257–266. doi: 10.1016/0034-5687(86)90011-3. [DOI] [PubMed] [Google Scholar]
- Knudson R. J., Slatin R. C., Lebowitz M. D., Burrows B. The maximal expiratory flow-volume curve. Normal standards, variability, and effects of age. Am Rev Respir Dis. 1976 May;113(5):587–600. doi: 10.1164/arrd.1976.113.5.587. [DOI] [PubMed] [Google Scholar]
- Kronborg G., Hansen M. B., Svenson M., Fomsgaard A., Høiby N., Bendtzen K. Cytokines in sputum and serum from patients with cystic fibrosis and chronic Pseudomonas aeruginosa infection as markers of destructive inflammation in the lungs. Pediatr Pulmonol. 1993 May;15(5):292–297. doi: 10.1002/ppul.1950150506. [DOI] [PubMed] [Google Scholar]
- MCGREGOR M., BECKLAKE M. R. The relationship of oxygen cost of breathing to respiratory mechanical work and respiratory force. J Clin Invest. 1961 Jun;40:971–980. doi: 10.1172/JCI104336. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Norman D., Elborn J. S., Cordon S. M., Rayner R. J., Wiseman M. S., Hiller E. J., Shale D. J. Plasma tumour necrosis factor alpha in cystic fibrosis. Thorax. 1991 Feb;46(2):91–95. doi: 10.1136/thx.46.2.91. [DOI] [PMC free article] [PubMed] [Google Scholar]
- O'Rawe A., McIntosh I., Dodge J. A., Brock D. J., Redmond A. O., Ward R., Macpherson A. J. Increased energy expenditure in cystic fibrosis is associated with specific mutations. Clin Sci (Lond) 1992 Jan;82(1):71–76. doi: 10.1042/cs0820071. [DOI] [PubMed] [Google Scholar]
- Sridhar M. K., Carter R., Lean M. E., Banham S. W. Resting energy expenditure and nutritional state of patients with increased oxygen cost of breathing due to emphysema, scoliosis and thoracoplasty. Thorax. 1994 Aug;49(8):781–785. doi: 10.1136/thx.49.8.781. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Suter S., Schaad U. B., Roux-Lombard P., Girardin E., Grau G., Dayer J. M. Relation between tumor necrosis factor-alpha and granulocyte elastase-alpha 1-proteinase inhibitor complexes in the plasma of patients with cystic fibrosis. Am Rev Respir Dis. 1989 Dec;140(6):1640–1644. doi: 10.1164/ajrccm/140.6.1640. [DOI] [PubMed] [Google Scholar]
- Vaisman N., Pencharz P. B., Corey M., Canny G. J., Hahn E. Energy expenditure of patients with cystic fibrosis. J Pediatr. 1987 Oct;111(4):496–500. doi: 10.1016/s0022-3476(87)80107-5. [DOI] [PubMed] [Google Scholar]
- Weissman C., Damask M. C., Askanazi J., Rosenbaum S. H., Kinney J. M. Evaluation of a non-invasive method for the measurement of metabolic rate in humans. Clin Sci (Lond) 1985 Aug;69(2):135–141. doi: 10.1042/cs0690135. [DOI] [PubMed] [Google Scholar]
- van der Poll T., Sauerwein H. P. Tumour necrosis factor-alpha: its role in the metabolic response to sepsis. Clin Sci (Lond) 1993 Mar;84(3):247–256. doi: 10.1042/cs0840247. [DOI] [PubMed] [Google Scholar]



