Abstract
Background
Low vision affects over 300 million people worldwide and can compromise both activities of daily living and quality of life. Rehabilitative training and vision assistive equipment (VAE) may help, but some visually impaired people have limited resources to attend in-person visits at rehabilitation clinics. These people may be able to overcome barriers to care through remote, Internet-based consultation (i.e., telerehabilitation).
Objectives
To compare the effects of telerehabilitation with face-to-face (e.g., in-office or inpatient) vision rehabilitation services for improving vision-related quality of life and reading speed in people with visual function loss due to any ocular condition. Secondary objectives are to evaluate compliance with scheduled rehabilitation sessions, abandonment rates for visual assistive equipment devices, and patient satisfaction ratings.
Search methods
We searched CENTRAL (which contains the Cochrane Eyes and Vision Group Trials Register) (2015 Issue 5), Ovid MEDLINE, Ovid MEDLINE In-Process and Other Non-Indexed Citations, Ovid MEDLINE Daily, Ovid OLDMEDLINE (January 1980 to June 2015), EMBASE (January 1980 to June 2015), PubMed (1980 to June 2015), ClinicalTrials.gov (www.clinicaltrials.gov) and the World Health Organization (WHO) International Clinical Trials Registry Platform (ICTRP) (www.who.int/ictrp/search/en). We did not use any language restriction or study design filter in the electronic searches; however, we restricted the searches from 1980 onwards because the Internet was not introduced to the public until 1982. We last searched the electronic databases on 15 June 2015.
Selection criteria
We planned to include randomized controlled trials (RCTs) or controlled clinical trials (CCTs) in which participants were diagnosed with low vision and were undergoing low vision rehabilitation using an Internet, web-based technology compared with an approach based on in-person consultations.
Data collection and analysis
Two authors independently screened titles and abstracts, and then full-text articles against the eligibility criteria. We planned to have two authors independently abstract data from included studies. We resolved discrepancies by discussion.
Main results
We did not find any study that met the inclusion criteria for this review and, hence, we did not conduct a quantitative analysis. As a part of the background, we discussed review articles on telemedicine for facilitating communication with elderly individuals or for providing remote ophthalmological care.
Authors’ conclusions
We did not find any evidence on whether the use of telerehabilitation is feasible or a potentially viable means to remotely deliver rehabilitation services to individuals with low vision. Given the disease burden and the growing interest in telemedicine, there is a need for future pilot studies and subsequent clinical trials to explore the potential for telerehabilitation as a platform for providing services to people with low vision.
BACKGROUND
Description of the condition
Low vision is defined as “a visual impairment, not corrected by standard eyeglasses, contact lenses, medication, or surgery, that interferes with the ability to perform everyday activities” (NEI glossary). Visual impairment can result from a variety of ocular and systemic disorders and may present as reduced central vision, reduced peripheral vision, blind spots, loss of contrast sensitivity, or a combination of these symptoms. Currently, it is estimated that 314 million people have low vision worldwide (Foster 2008). In the United States, 3.5 million people older than 40 years of age suffer from low vision, making it the tenth most prevalent cause of disability (Congdon 2004; Massof 2002). With the increase in life span and diseases like diabetic retinopathy, the number of people with low vision is expected to increase significantly by 2030 (https://www.nei.nih.gov/news/pressreleases/020113).
Without effective interventions, reading, mobility, and functional independence decrease with low vision, and the risk of falls and fractures increases (Lamoureux 2008); these changes are associated with withdrawal from society and depression, resulting in a devastating impact on the quality of life (Goldstein 2012). The National Eye Institute's strategic plan, the Low Vision and Blindness Rehabilitation - National Plan for Eye and Vision Research, recommends developing rehabilitation programs and determining the most effective interventions for people with visual impairments (https://www.nei.nih.gov/strategicplanning/np_low).
Description of the intervention
Low vision rehabilitation is the primary intervention for people with chronic, disabling visual impairment (Markowitz 2006). The goal is to improve activities of daily living by helping people with reduced visual function optimize the use of their remaining sight through the provision of appropriate refractive correction as well as training in the use of vision assistive equipment (VAE) and compensatory strategies (Binns 2012). Patients are taught to cope with their disability by initiating lifestyle and habitat modifications. Successful use of VAE depends highly on skill reinforcement with a rehabilitation specialist. The Low Vision Intervention Trial (LOVIT) demonstrated a positive effect of inpatient low vision rehabilitation on self-reported visual function (Stelmack 2008); however, the current outpatient-based approach for delivering low vision rehabilitation presents significant challenges due to transportation barriers and insufficient compliance with VAE device training.
Patients may be provided with limited instructions or training in the use of newly prescribed VAE. VAE often functions best at very close working distances, which are unnatural for the patient and require training, education, practice, and skill reinforcement. Patients may become frustrated and not return for follow-up visits when they continue to experience difficulty using VAE at home or if their vision or general health decline.
Furthermore, the majority of the population seeking outpatient low vision rehabilitation services are elderly, with 73% of patients aged 65 and older (Goldstein 2012). In addition to their vision impairment, there are age-associated physical, psychological, and cognitive issues, including memory deficits.
This group relies heavily on others for support and transportation. One study found that about two-thirds of the low vision population do not drive (Goldstein 2012). Transportation issues and comorbidities limit peoples’ ability to return for the necessary follow-up sessions, which commonly focus on training with VAE. Given all these challenges, VAE has variable effectiveness and high rates of abandonment (Watson 1997). The potential efficacy of low vision rehabilitation may not be fully achieved. The strategy of inpatient rehabilitation employed in the LOVIT study incorporated multiple rehabilitation sessions and found effect sizes that far outweighed typical outpatient low vision rehabilitation (Stelmack 2008), which often may involve only one visit to a low vision clinic.
Telerehabilitation refers to the delivery of rehabilitation services via information and communication technologies (Brennan 2011). Clinically, this term encompasses a range of rehabilitation services that include assessment, monitoring, prevention, intervention, supervision, education, consultation, and counseling. Telerehabilitation has commonly been used for patients with stroke, brain injury, joint replacement, or spinal cord injury (Rogante 2010), and it usually involves audio and video technology.
How the intervention might work
Telerehabilitation may offer several important advantages over traditional in-office care and has the potential to lead to improvement in vision- and health-related outcomes (Rogante 2010). First of all, it can potentially overcome transportation difficulties. Furthermore, health professionals can evaluate patients in their home environment rather than in a clinical setting, thereby providing more personalized care. In addition, telerehabilitation has the potential to expand rehabilitation modalities through the use of secure, Internet-based communication technology (e.g., computers, smartphones), and it may also increase efficiency by optimizing the use of time and other resources.
Why it is important to do this review
In ophthalmology, most studies of telemedicine have involved transfer of patients’ ocular images among providers for interpretation, diagnosis, and management of ocular disease, while fewer appear to have used telemedicine to communicate directly with patients or to provide low vision rehabilitation (Tang 2005). The goal of low vision rehabilitation services, whether in person or remotely via telemedicine, is to help people with vision loss maintain visual functioning and activities of daily living, as well as social and psychological well-being. While telemedicine may overcome some barriers, such as transportation, it may present other technological challenges in interactions with visually impaired patients. We are interested in determining whether studies on telerehabilitation have achieved success with the low vision population.
OBJECTIVES
To compare the effects of telerehabilitation with face-to-face (e.g., in-office or inpatient) vision rehabilitation services for improving vision-related quality of life and reading speed in people with visual function loss due to any ocular condition. Secondary objectives are to evaluate compliance with scheduled rehabilitation sessions, abandonment rates for visual assistive equipment devices, and patient satisfaction ratings.
METHODS
Criteria for considering studies for this review
Types of studies
We planned to include randomized controlled trials (RCTs) and controlled clinical trials (CCTs). We also planned to summarize non-randomized studies, such as cohort studies and case series.
Types of participants
We planned to include studies in which participants were diagnosed with low vision, that is, visual function loss due to any ocular condition, as defined in the individual studies. According to the World Health Organization (WHO), low vision is diagnosed when the best-corrected visual acuity in the better eye is between 20/400 and 20/60 (WHO low vision definition); however, because this definition is not universally accepted, we decided to accept the definitions specified in the included studies.
Types of interventions
The main intervention of interest is the use of web-based technology to provide rehabilitation services to the low vision population. The comparison intervention is any face-to-face communication, such as traditional office-based approaches for providing low vision rehabilitation. Low vision rehabilitation includes assessing visual status, prescribing VAE (e.g., magnifiers, telescopes, optical or electronic devices), training, education, and counseling. For each telerehabilitation intervention, we planned to document whether it was combined with any initial or subsequent in-office visits, also noting the frequency of each type of encounter (i.e., number and proportion of in-person visits).
Types of outcome measures
Primary outcomes
The primary outcome of the review was vision-related quality of life, measured by any validated instrument used in the trial at 6 to 12 months after starting the intervention. We planned to analyze both absolute values at a follow-up time point and change from baseline when data were available to us. We also planned that when data from multiple time points were available (e.g., when a trial reported both 6- and 12-month data), we would use the data from the longest follow-up time point.
Secondary outcomes
The secondary outcomes included:
short-term (less than six months) vision-related quality of life measured by any validated instrument;
clinical measures, such as reading speed at all documented post-intervention time points;
patient satisfaction with the intervention, as assessed in an included trial, at the end of the intervention phase; and
compliance at the end of the intervention phase, as judged in the included trial.
We planned to use standardized and validated measurement methods when they were available (e.g., reading speed in words per minute or critical print size in M decimal notation using validated texts such as the MNread acuity charts) or validated questionnaire data (e.g., the National Eye Institute Visual Function Questionnaire (NEI-VFQ) or Veteran Affairs Low-Vision Visual Functioning Questionnaire (VALVVFQ)).
We planned to report any adverse events related to the interventions.
Search methods for identification of studies
Electronic searches
We searched CENTRAL (which contains the Cochrane Eyes and Vision Group Trials Register) (2015 Issue 5), Ovid MEDLINE, Ovid MEDLINE In-Process and Other Non-Indexed Citations, Ovid MEDLINE Daily, Ovid OLDMEDLINE (January 1980 to June 2015), EMBASE (January 1980 to June 2015), PubMed (1980 to June 2015), ClinicalTrials.gov (www.clinicaltrials.gov) and the World Health Organization (WHO) International Clinical Trials Registry Platform (ICTRP) (www.who.int/ictrp/search/en). We did not use any language restriction or study design filter in the electronic searches; however, we restricted the searches from 1980 onwards because the Internet was not introduced to the public until 1982. We last searched the electronic databases on 15 June 2015.
See: Appendices for details of search strategies for CENTRAL (Appendix 1), MEDLINE (Appendix 2), EMBASE (Appendix 3), PubMed (Appendix 4), ClinicalTrials.gov (Appendix 5) and the ICTRP (Appendix 6).
Searching other resources
We planned to search reference lists of included studies to identify additional studies for inclusion.
Data collection and analysis
Selection of studies
We imported all search results into an EndNote database and removed duplicates. Two authors independently screened the titles and abstracts against the eligibility criteria and labeled each record as ’definitely relevant’, ’possibly relevant’, or ’definitely not relevant’. We retrieved full-text reports for each record labeled as ’definitely relevant’ or ’possibly relevant’ by both authors. Two authors independently assessed the full-text reports for final eligibility, documenting reasons for exclusion and resolving discrepancies through discussion.
We did not include any studies in this review. If eligible studies are identified in the future, we will use the following methods for data abstraction and analysis.
Data extraction and management
Two authors working independently will extract data from included studies into a web-based, electronic data collection form developed using the Systematic Review Data Repository (SRDR) (http://srdr.ahrq.gov/). We will adapt a ’common data items form’ developed and piloted by the Cochrane Eyes and Vision Group US Project (CEVG@US) in SRDR (Li 2015). Data items to extract include information on study design (e.g., study setting, countries in which the participants were recruited, sample size, study duration, types of design and analysis, funding source for the study and any potential conflict of interests), participant characteristics (e.g., inclusion and exclusion criteria of the individual study, underlying disease, diagnosis, vision and medical history), interventions and comparators (e.g., treatment modality, duration, timing), and outcomes (e.g., outcome domain, specific measurement tool, metric, method of aggregation, and time frame). One author will enter data into Cochrane's statistical software Review Manager (RevMan 2014), and a second author will verify the data entered. We will present summary data in the ’Characteristics of included studies’ table and resolve discrepancies between data extractors through discussion. We will contact study investigators for any missing or unclear information; if we receive no response within two weeks, we will proceed with available information.
Assessment of risk of bias in included studies
Two authors will independently assess the risk of bias in included RCTs and CCTs following the guidance outlined in Chapter 8 (Higgins 2011a) and Chapter 13 (Reeves 2011) of the Cochrane Handbook for Systematic Reviews of Interventions. Specifically, we will assess random sequence generation, allocation concealment, masking (blinding) of outcome assessors, and completeness of outcome data. Because of the nature of the intervention, masking of providers and participants is unlikely to be feasible. We will assign each domain as being at ’low’, ’unclear’, or ’high’ risk of bias following the criteria outlined in the Handbook and document reasons and rationales for our assessment.
Measures of treatment effect
We will treat ordinal outcomes and measurement scales, such as level of satisfaction and vision-related quality of life, as continuous data or dichotomous data as appropriate, depending on the length of the scale used and the manner in which the outcomes are reported.
Continuous outcomes
For continuous outcomes (e.g., reading speed rates or critical print size), we will use difference in means to measure the treatment effect, and we will determine 95% confidence intervals (CIs).
Dichotomous outcomes
For dichotomous outcomes, such as compliance with follow-up (defined as the attendance rate of scheduled follow-up visits within a specified window of time, and based on a pre-defined threshold for compliance), we will use risk ratios (RRs) to estimate treatment effects.
Unit of analysis issues
Because of the nature of the intervention, we expect that individual participants will be randomized in included studies.
Dealing with missing data
We will contact trial authors for missing or unclear information, for example, information required to assess risk of bias or for unclear or underreported outcomes. We will allow two weeks for the authors to respond and will move forward with best available information otherwise. We will estimate missing outcome data based on multiple imputation or other imputation approaches that account for the uncertainty in imputing the missing outcome data. When no such estimates are possible, we will use estimates reported by the authors and discuss the potential bias that could be introduced by missing data.
Assessment of heterogeneity
We will assess clinical and methodological heterogeneity by carefully evaluating the design and participant characteristics of the included studies for factors that may affect the reliability of estimates of the magnitude and direction of treatment effects. Clinical and methodological heterogeneity may manifest as statistical heterogeneity. We will quantify statistical heterogeneity using the I2 statistic, the Q statistic and the Chi2 test for heterogeneity, and the Tau2 value when a sufficient number of studies are available (Turner 2012). We will use an I2 value of 75% or greater as a cutoff for indicating considerable heterogeneity (Higgins 2011a).
Assessment of reporting biases
When study protocols are available, we will compare the study protocol with study publications to identify any discrepancies in reporting of outcomes. When a sufficient number of studies (10 or more) are included, we will use a funnel plot to visualize small study effects and the potential for publication bias.
Data synthesis
We will combine results quantitatively using random-effects meta-analysis when three or more studies reporting the same outcome are included and when the studies are homogeneous clinically, methodologically, and statistically. We will not combine studies in a meta-analysis when there is considerable statistical heterogeneity (i.e., I2 value of 75% or greater). We will not include observational studies, cohort studies, or case series in meta-analysis.
Subgroup analysis and investigation of heterogeneity
We will consider the following subgroups: underlying disease (e.g., age-related macular degeneration versus glaucoma), severity of visual impairment (e.g., early versus advanced stage of vision loss; legal blindness or not), and type of impairment (e.g., central versus peripheral visual impairment). Based on our clinical knowledge, we expect that the treatment effect may vary according to these factors.
Sensitivity analysis
We will conduct a sensitivity analysis by excluding studies graded at ’high’ risk of bias for allocation concealment before randomization to assess the robustness of our findings.
Summary of findings
We will summarize the main findings, including the strengths and limitations of evidence for each main outcome. We will provide a summary of our perception of how the intervention may work, for whom, and under what circumstances. We will provide a general interpretation of the evidence we find in the context of other evidence and discuss implications for practice and future research. We will use a ‘summary of Findings’ table when appropriate, and two authors will independently grade the overall certainty of the evidence for each outcome using the GRADE classification (www.gradeworkinggroup.org/).
RESULTS
Description of studies
Results of the search
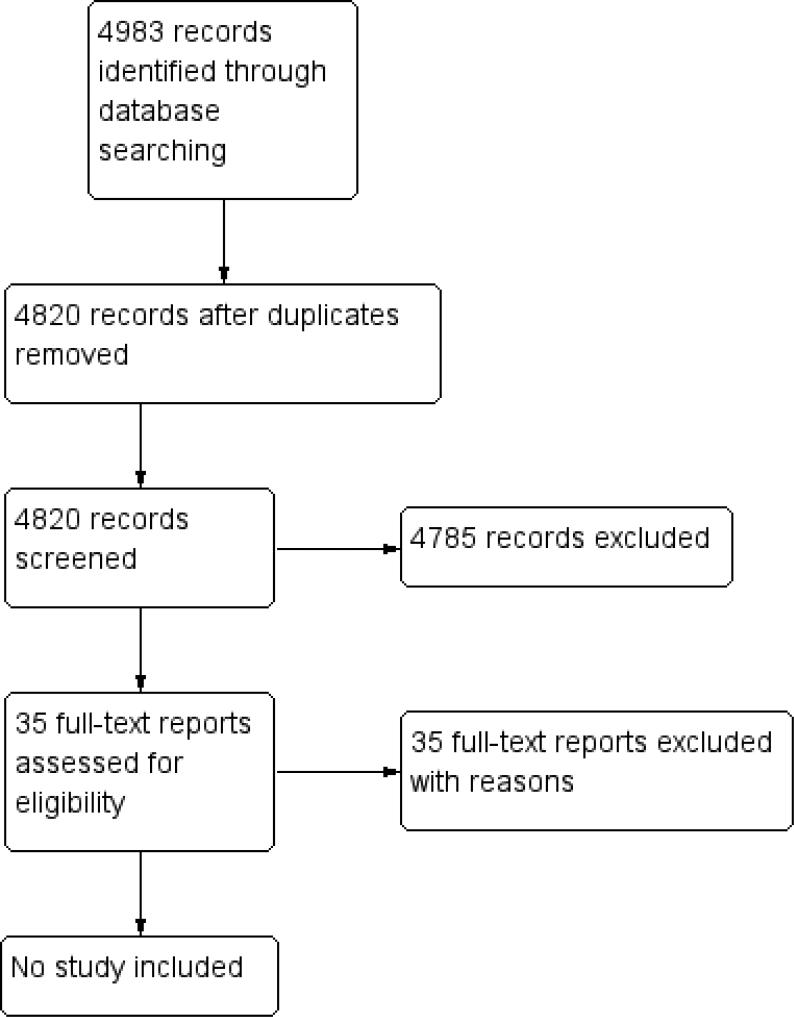
The electronic searches up to 15 June 2015 identified 4820 unique records. We assessed 4785 as not relevant and reviewed full-texts for 35 studies (Figure 1). No study was eligible for this review.
Figure 1.
Study flow diagram.
Included studies
There were no included studies.
Excluded studies
We excluded 35 studies after assessment of the full-text reports. Fifteen studies were not RCTs or CCTs, and the remaining 20 did not compare traditional face-to-face communication with treatment using Internet, web-based communication technology that facilitated provision of remote, low vision rehabilitation services (’Characteristics of excluded studies’ table).
Risk of bias in included studies
There were no included studies for which we could assess the risk of bias.
Effects of interventions
There were no included studies to be used for evidence synthesis.
DISCUSSION
Summary of main results
We did not find any RCT or CCT that met our inclusion criteria. We found a few review articles that cited studies that are relevant to our topic; those are summarized in Agreements and disagreements with other studies or reviews.
Overall completeness and applicability of evidence
Delivering low vision rehabilitation services remotely via telemedicine has the potential to help people with vision loss maintain function and activities of daily living as well as social and psychological well-being. Although we did not find any study that specifically addressed telerehabilitation for people with low vision, we found review articles that cited projects that had assessed the needs and feasibility of telemedicine for ophthalmologic or other medical conditions. These findings are supportive and highlight the need for more specific research on telerehabilitation for people with low vision.
Quality of the evidence
We found no evidence of the benefit or harm of telerehabilitation for people with low vision. Thus, the quality of the evidence is moot.
Potential biases in the review process
We followed the Cochrane Handbook for Systematic Reviews of Interventions (Higgins 2011b) and Methodological Expectations of Cochrane Intervention Reviews (MECIR) Standards for the reporting of new Cochrane Intervention Reviews (http://editorial-unit.cochrane.org/mecir) in conducting this review. A trained informationist designed and conducted the electronic search. Two authors performed independent screenings of search results. None of the authors have any financial conflicts of interest.
Agreements and disagreements with other studies or reviews
Need for telemedicine
A literature review of eye health in rural Australia highlighted the need for services capable of reaching individuals living in rural areas, who had poor access to eye care providers, reduced utilization of services, and increased prevalence of blinding eye diseases (e.g., glaucoma). However, this review was conducted 15 years ago and did not contemplate the use of telehealth for low vision rehabilitation (Madden 2002).
Feasibility of telerehabilitation
An overview of telemedicine for eye care suggested that low vision consultation through tele-ophthalmology could improve access to specialized care that was otherwise unavailable in underserved areas. The authors of this report described a low vision population who received consultation using a tele-ophthalmology approach without traveling to the low vision center at the University of Texas at Houston. The tele-ophthalmology services were discontinued after the grant funding ended; no further details are available (Tang 2005).
Two review articles of tele-ophthalmology in India described real-time interactions using a videoconferencing system between the remotely located ophthalmologists and patients undergoing screening for ocular diseases (Murthy 2012; Prathiba 2011). Also in India, the Aravind Tele-ophthalmology Network and Madras Diabetes Research Foundation have provided a videoconferencing system for the retinal specialist at a base hospital to communicate directly with patients in a mobile screening van (Murthy 2012). However, there was no indication that low vision rehabilitation services were delivered to these patients via tele-ophthalmology in these projects. One review specifically stated that low vision consultation could be one potential tele-ophthalmology service (Prathiba 2011).
A systematic review of telemedicine for elderly patients with any health condition found that some telemedicine studies had excluded people with visual impairment. These studies did not provide data with regard to the impact of vision loss on people's ability to participate in the videoconferencing sessions (Van den Berg 2012). Most studies of telemedicine in elderly patients found benefits for behavioral outcomes, such as adherence, self-efficacy, quality of life, and economic outcomes. These findings are encouraging since most low vision populations are elderly; however, the potential for vision loss to limit access to or use of a videoconferencing portal for telemedicine has not been formally evaluated in an older population.
We identified a recent study on usage of relevant technologies by patients with low vision, which potentially could be used to deliver telerehabilitation services. In 2014, use of a tablet device was reported by nearly half (48%) of 132 people with low vision or no vision (Crossland 2014). Most respondents (81%) indicated that they used a smartphone and about half (51%) used their camera and screen as a magnifier. While this study did not specify the proportion who used video chat on their device, it did suggest that devices with video functionality were being used by the survey respondents.
In addition, an ongoing pilot study being conducted by two authors of this systematic review found that approximately 75% of the 100 participants have access to a computer or handheld device (e.g., tablet or smartphone); of this group, 90% have Internet access in their current residence. Preliminary analysis suggests that having an Internet-ready device (e.g., computer, tablet, smartphone), having home Internet access, and being employed are associated with willingness to try telerehabilitation (data not yet published; Johns Hopkins Bloomberg School of Public Health IRB# 00005090).
AUTHORS’ CONCLUSIONS
Implications for practice
At the moment, there is no evidence from controlled trials available to support the use of telerehabilitation for people with low vision. Several observational studies and projects have indicated the potential benefit and feasibility of delivering ophthalmologic care via the Internet. However, previous studies and projects have not demonstrated the efficacy of telerehabilitation for low vision and utility for practice.
Implications for research
Given the disease burden and the growing interest in telemedicine, there is a need for future studies to explore the potential for telerehabilitation as a platform for providing remote services to people with low vision. As a logical first step, it would be helpful for research to explore patients’ preferences for receiving telerehabilitation versus in-office rehabilitation, considering both ex ante and post hoc elicitation of preferences, as well as people's ability to access the Internet for telerehabilitation services. If there is sufficient support for telerehabilitation, a pilot feasibility study could initially evaluate whether people with low vision can successfully use and satisfactorily communicate with a provider using a secure, videoconferencing portal after an initial in-person consultation. Such a study would be followed by a randomized clinical trial to compare the outcomes following low vision rehabilitation delivered in-office versus remotely via the Internet. Quality monitoring is necessary for such a study to ensure that the low vision participants are using the system correctly. Despite the growing interest in telerehabilitation, the absence of any studies with data for people with low vision may reflect limited funding mechanisms for such research, or concerns about long-term feasibility and sustainability given limited payment reimbursement mechanisms for this type of service. However, supportive evidence from a randomized controlled trial of telerehabilitation for low vision could be used to help drive policy changes and implement programs that help provide payment to cover remote services.
CHARACTERISTICS OF STUDIES
Characteristics of excluded studies [ordered by study ID]
| Study | Reason for exclusion |
|---|---|
| Aimola 2014 | Not the intervention of interest |
| Arnold 2002 | Not a RCT or CCT: a case series; not the intervention of interest |
| Bai 2007 | Not a RCT or CCT: a report of two observational studies; not the intervention of interest |
| Beumer 2000 | Not the intervention of interest |
| CITT 2008 | Not the participants of interest |
| CITT 2009 | Not the participants of interest |
| Gall 2012 | Not a RCT or CCT: a prospective non-controlled open-label trial |
| Gell 2013 | Not a RCT or CCT: a retrospective cross-sectional study; not the intervention of interest |
| George 2011 | Not the intervention of interest. |
| Jacobson 2005 | Not a RCT or CCT: a report for an non-controlled interventional study; not the intervention of interest; not the population of interest |
| Jeon 2012 | Not the intervention of interest |
| Jiang 2005 | Not a RCT or CCT: a case series |
| Kasten 1995 | Not the intervention of interest |
| Kasten 2000 | Not the intervention of interest |
| Kasten 2001 | Not the intervention of interest |
| Kerkhoff 1998 | Not the intervention of interest |
| Komm 2009 | Not the intervention of interest. |
| Kampf 2001 | Not the intervention of interest. |
| Kampf 2008 | Not the intervention of interest |
| Larizza 2014 | Not a RCT or CCT: an observational study |
| Mines 2011 | Not a RCT or CCT: a retrospective, non-comparative, consecutive case series; not the intervention of interest |
| Powers 2009 | Not a RCT or CCT: a retrospective cross-sectional study; not the intervention of interest |
| Puig de la Bellacasa 1980 | Not a RCT or CCT: an observational study |
| Ross 1992 | Not the intervention of interest |
| Schenk 2013 | Not the intervention of interest |
| Schiefer 2006 | Not a RCT or CCT: an experimental study for a computer-based procedure development; not the intervention of interest |
| Schinzel 2011 | Not the intervention of interest |
| Srinivasan 2012 | Not the intervention of interest |
| Tan 2013 | Not a RCT or CCT: a prospective interventional non-comparative study; not the intervention of interest |
| Tatarinov 1993 | Not a RCT or CCT: a prospective, non-randomized, non-controlled trial |
| Tennant 2001 | Not the intervention of interest |
| Tsitsiashvili 2007 | Not the intervention of interest |
| Ulrich 2009 | Not a RCT or CCT: a cross-sectional non-comparative study; not the intervention of interest |
| Widdig 2006 | Not a RCT or CCT: a non-comparative study |
| Zhang 2013 | Not the intervention of interest |
CCT: controlled clinical trial; RCT: randomized controlled trial
PLAIN LANGUAGE SUMMARY.
Telerehabilitation for people with low vision
Review question
This systematic review aimed to evaluate the benefits of providing remote vision rehabilitation services for people with low vision via telerehabilitation, which uses an Internet-based approach rather than the usual office-based consultations. The main outcome of interest is vision-related quality of life, but we also are interested in visual function measures such as reading speed, as well as compliance with scheduled sessions and patient satisfaction.
Background
Low vision is a reduction in visual function that cannot be fixed by eyeglasses, contact lenses, or other medical and surgical treatments. People with low vision may find it difficult to perform daily activities such as reading and driving. Currently, about 314 million people have low vision worldwide.
One way to help people with low vision is rehabilitation, during which they are taught to use magnification devices and techniques to make the most of their remaining vision; they are also evaluated periodically to reinforce skills. Office-based rehabilitation for low vision has been shown to be effective; however, transportation barriers may decrease compliance with training and undermine the overall effectiveness of the program.
It is possible to deliver low vision rehabilitation through the Internet (i.e., telerehabilitation). Telerehabilitation avoids the challenges related to transportation to in-office visits and also offers the convenience and practicality of rehabilitation sessions in the home.
Key results and quality of the evidence
The authors of this review did not find any eligible study that directly addressed the research question. The search is current to 15 June 2015.
ACKNOWLEDGEMENTS
We acknowledge Lori Rosman, Trials Search Co-ordinator for the Cochrane Eyes and Vision Group (CEVG), who designed the electronic search strategies. We thank Karla Zadnik, Barbara Hawkins, and the CEVG editorial group for comments to drafts of this protocol. We also thank Angus Turner, Barbara Hawkins, and other peer reviewers for comments to our manuscript.
SOURCES OF SUPPORT
Internal sources
• No sources of support supplied
External sources
• The Cochrane Eyes and Vision Group U.S. Project is supported by grant 1 U01 EY020522, National Eye Institute, National Institutes of Health, USA.
• National Institute for Health Research (NIHR), UK.
• Richard Wormald, Co-ordinating Editor for the Cochrane Eyes and Vision Group (CEVG) acknowledges financial support for his CEVG research sessions from the Department of Health through the award made by the National Institute for Health Research to Moorfields Eye Hospital NHS Foundation Trust and UCL Institute of Ophthalmology for a Specialist Biomedical Research Centre for Ophthalmology.
• The NIHR also funds the CEVG Editorial Base in London.
The views expressed in this publication are those of the authors and not necessarily those of the NIHR, NHS, or the Department of Health.
APPENDICES
Appendix 1. CENTRAL search strategy
#1 MeSH descriptor: [Vision, Low] explode all trees
#2 MeSH descriptor: [Vision Disorders] explode all trees
#3 MeSH descriptor: [Visually Impaired Persons] explode all trees
#4 ((low* or handicap* or subnormal* or impair* or partial* or disab* or reduce* or diminish* or decrease*) near/3 (vision or visual* or sight*))
#5 ((Vision or visual) near/2 loss)
#6 #1 or #2 or #3 or #4 or #5
#7 MeSH descriptor: [Telecommunications] this term only
#8 MeSH descriptor: [Telemedicine] explode all trees
#9 MeSH descriptor: [Telemetry] explode all trees
#10 MeSH descriptor: [Videoconferencing] explode all trees
#11 MeSH descriptor: [Wireless Technology] explode all trees
#12 MeSH descriptor: [Computer Communication Networks] explode all trees
#13 MeSH descriptor: [Decision Making, Computer-Assisted] explode all trees
#14 MeSH descriptor: [Computer-Assisted Instruction] explode all trees
#15 MeSH descriptor: [Computers] explode all trees
#16 MeSH descriptor: [User-Computer Interface] explode all trees
#17 (Telecommunication* or telemed* or tele-med* or telemetry or telerehab* or tele-rehab* or Telehealth* or tele-health* or Teleconsult* or tele-consult* or Teleconference* or tele-conference* or tele-home* or telehome* or tele-coach or telecoach* or tele-care* or telecare* or tele-ophthalm* or teleophthalm* or tele-screen* or telescreen* or tele-therap* or teletherap* or tele-diagnosis or telediagnosis or tele-mentor* or telementor*)
#18 (eHealth or e-health or eMedicine or e-medicine or eRehab* or e-rehab*)
#19 (Mobile health or mHealth)
#20 (information technolog* or information communication technolog* or ICT)
#21 ((web* or internet* or virtual* or remote* or wireless* or mobile or video* or computer* or online or on-line) near/5 (rehab* or therap* or treatment or communication* or consult* or care or specialist* or monitor* or educat* or counsel* or train* or asses*))
#22 #7 or #8 or #9 or #10 or #11 or #12 or #13 or #14 or #15 or #16 or #17 or #18 or #19 or #20 or #21
#23 #6 and #22 from 1980
Appendix 2. MEDLINE (Ovid) search strategy
exp low vision/
exp vision disorders/
exp visually impaired persons/
((low* or handicap* or subnormal* or impair* or partial* or disab* or reduce* or diminish* or decrease*) adj3 (vision or visual* or sight*)).tw.
((Vision or visual) adj2 loss).tw.
or/1-5
Telecommunications/
exp telemedicine/
exp telemetry/
exp Videoconferencing/
exp Wireless Technology/
exp Computer Communication Networks/
exp Decision Making, Computer-Assisted/
exp Computer-Assisted Instruction/
exp computers/
exp User-Computer Interface/
(Telecommunication* or telemed* or tele-med* or telemetry or telerehab* or tele-rehab* or Telehealth* or tele-health* or Teleconsult* or tele-consult* or Teleconference* or tele-conference* or tele-home* or telehome* or tele-coach or telecoach* or tele-care* or telecare* or tele-ophthalm* or teleophthalm* or tele-screen* or telescreen* or tele-therap* or teletherap* or tele-diagnosis or telediagnosis or tele-mentor* or telementor*).tw.
(eHealth or e-health or eMedicine or e-medicine or eRehab* or e-rehab*).tw.
(Mobile health or mHealth).tw.
(information technolog* or information communication technolog* or ICT).tw.
((web* or internet* or virtual* or remote* or wireless* or mobile or video* or computer* or online or on-line) adj5 (rehab* or therap* or treatment or communication* or consult* or care or specialist* or monitor* or educat* or counsel* or train* or asses*)).tw.
or/7-21
6 and 22
limit 23 to yr=“1980 -Current”
Appendix 3. EMBASE.com search strategy
#1 ’visual impairment’/exp
#2 ’low vision’/exp
#3 ’visual disorder’/exp
#4 ((low* OR handicap* OR subnormal* OR impair* OR partial* OR disab* OR reduce* OR diminish* OR decrease*) NEAR/3 (vision OR visual* OR sight*)):ab,ti
#5 ((vision OR visual) NEAR/2 loss):ab,ti
#6 #1 OR #2 OR #3 OR #4 OR #5
#7 ’telehealth’/exp
#8 ’telemetry’/exp
#9 ’telecommunication’/de
#10 ’teleconference’/exp
#11 ’mass communication’/de
#12 ’internet’/exp
#13 ’videoconferencing’/exp
#14 ’webcast’/exp
#15 ’wireless communication’/exp
#16 ’computer network’/exp
#17 ’decision support system’/exp
#18 ’computer’/exp
#19 ’computer interface’/exp
#20 ’human computer interaction’/exp
#21 telecommunication*:ab,ti OR telemed*:ab,ti OR telemetry:ab,ti OR telerehab*:ab,ti OR telehealth*:ab,ti OR teleconsult*:ab,ti OR teleconference*:ab,ti OR telehome*:ab,ti OR telecoach*:ab,ti OR telecare*:ab,ti OR teleophthalm*:ab,ti OR telescreen*:ab,ti OR teletherap*:ab,ti OR telediagnosis:ab,ti OR telementor*:ab,ti
#22 (tele NEXT/1 (med* OR rehab* OR health* OR consult* OR conference* OR home* OR coach* OR care* OR ophthalm* OR screen* OR therap* OR diagnosis OR mentor*)):ab,ti
#23 ehealth:ab,ti OR ’e health’:ab,ti OR emedicine:ab,ti OR ’e medicine’:ab,ti
#24 (e NEXT/1 rehab*):ab,ti
#25 ’mobile health’:ab,ti OR mhealth:ab,ti
#26 ’information technology’:ab,ti OR ’information technologies’:ab,ti OR ’information communication technology’:ab,ti OR ’information communication technologies’:ab,ti OR ict:ab,ti
#27 ((web* OR internet* OR virtual* OR remote* OR wireless* OR mobile OR video* OR computer* OR online OR ’on line’) NEAR/5 (rehab* OR therap* OR treatment OR communication* OR consult* OR care OR specialist* OR monitor* OR educat* OR counsel* OR train* OR asses*)):ab,ti
#28 #7 OR #8 OR #9 OR #10 OR #11 OR #12 OR #13 OR #14 OR #15 OR #16 OR #17 OR #18 OR #19 OR #20 OR #21 OR #22 OR #23 OR #24 OR #25 OR #26 OR #27
#29 #6 AND #28
#30 #6 AND #28 AND [1980-2015]/py
Appendix 4. PubMed search strategy
#1 ((low*[tiab] OR handicap*[tiab] OR subnormal*[tiab] OR impair*[tiab] OR partial*[tiab] OR disab*[tiab] OR reduce*[tiab] OR diminish*[tiab] OR decrease*[tiab]) AND (vision[tiab] OR visual*[tiab] OR sight*[tiab])) NOT Medline[sb]
#2 ((Vision[tiab] OR visual[tiab]) AND loss[tiab]) NOT Medline[sb]
#3 #1 OR #2
#4 (Telecommunication*[tiab] OR telemed*[tiab] OR tele-med*[tiab] OR telemetry[tiab] OR telerehab*[tiab] OR tele-rehab*[tiab] OR Telehealth*[tiab] OR tele-health*[tiab] OR Teleconsult*[tiab] OR tele-consult*[tiab] OR Teleconference*[tiab] OR tele-conference*[tiab] OR tele-home*[tiab] OR telehome*[tiab] OR tele-coach[tiab] OR telecoach*[tiab] OR tele-care*[tiab] OR tele-care*[tiab] OR tele-ophthalm*[tiab] OR teleophthalm*[tiab] OR tele-screen*[tiab] OR telescreen*[tiab] OR tele-therap*[tiab] OR teletherap*[tiab] OR tele-diagnosis[tiab] OR telediagnosis[tiab] OR tele-mentor*[tiab] OR telementor*[tiab]) NOT Medline[sb]
#5 (eHealth[tiab] OR e-health[tiab] OR eMedicine[tiab] OR e-medicine[tiab] OR eRehab*[tiab] OR e-rehab*[tiab]) NOT Medline[sb]
#6 (Mobile health[tiab] OR mHealth[tiab]) NOT Medline[sb]
#7 (information technolog*[tiab] OR information communication technolog*[tiab] OR ICT[tiab]) NOT Medline[sb]
#8 ((web*[tiab] OR internet*[tiab] OR virtual*[tiab] OR remote*[tiab] OR wireless*[tiab] OR mobile[tiab] OR video*[tiab] OR computer*[tiab] OR online[tiab] OR on-line[tiab]) AND (rehab*[tiab] OR therap*[tiab] OR treatment[tiab] OR communication*[tiab] OR consult*[tiab] OR care[tiab] OR specialist*[tiab] OR monitor*[tiab] OR educat*[tiab] OR counsel*[tiab] OR train*[tiab] OR asses*[tiab])) NOT Medline[sb]
#9 #4 OR #5 OR #6 OR #7 OR #8
#10 #3 AND #9
#11 #1 AND #10
Appendix 5. ClinicalTrials.gov search strategy
low vision AND (telemedicine OR internet OR website OR remote)
Appendix 6. ICTRP search strategy
low vision AND telemedicine OR low vision AND internet OR low vision AND website OR low vision AND remote
Footnotes
Citation: Bittner AK, Wykstra SL, Yoshinaga PD, Li T. Telerehabilitation for people with low vision. Cochrane Database of Systematic Reviews 2015, Issue 8. Art. No.: CD011019. DOI: 10.1002/14651858.CD011019.pub2.
CONTRIBUTIONS OF AUTHORS
Conceived the review: AKB, PDY, TL
Designed the review: AKB, TL
Coordinated the review: AKB, TL
Screened search results: AKB, SLW, PDY, TL
Organized retrieval of papers: AKB, SLW, PDY, TL
Screened retrieved papers against inclusion criteria: AKB, SLW, PDY, TL
Wrote the review: AKB, SLW, PDY, TL
Performed previous work that was the foundation of current study: AKB, TL
Guarantor of the review: AKB
DECLARATIONS OF INTEREST
One reason for conducting this systematic review is to establish the knowledge base for designing an RCT to evaluate the efficacy of telerehabilitation for a primarily elderly, visually impaired population. Along with this systematic review, Dr Tianjing Li has received funding to collect pilot data to demonstrate the feasibility of using telerehabilitation as a platform for delivering low vision rehabilitation services. The systematic review and the pilot data collected will lay the foundation for preparing an RCT application.
DIFFERENCES BETWEEN PROTOCOL AND REVIEW
We did not follow all methods as set forth in the protocol for the review as there were no included studies, and thus, no meta-analysis. We revised methods for future updates of this review to include, when possible, GRADE assessment and a Summary of Findings table.
DATA AND ANALYSES
This review has no analyses.
REFERENCES
References to studies excluded from this review
- Aimola L, Lane AR, Smith DT, Kerkhoff G, Ford GA, Schenk T. Efficacy and feasibility of home-based training for individuals with homonymous visual field defects. Neurorehabilitation and Neural Repair. 2014;28(3):207–18. doi: 10.1177/1545968313503219. [DOI] [PubMed] [Google Scholar]
- Arnold RW. Use of a consumer video system to enhance low vision in children and adults. Journal of Pediatric Ophthalmology and Strabismus. 2002;39(4):245–7. doi: 10.3928/0191-3913-20020701-16. [DOI] [PubMed] [Google Scholar]
- Bai VT, Murali V, Kim R, Srivatsa SK. Teleophthalmology-based rural eye care in India. Telemedicine Journal and E-Health. 2007;13(3):313–21. doi: 10.1089/tmj.2006.0048. [DOI] [PubMed] [Google Scholar]
- Beumer JJ, De Haan A, Van der Ven J. Implications of computer-mediated communication for people who are visually impaired in dealing with complex visualization tasks. Journal of Visual Impairment and Blindness. 2000;94(7):453–6. [Google Scholar]
- Convergence Insufficiency Treatment Trial Study Group Randomized clinical trial of treatments for symptomatic convergence insufficiency in children. Archives of Ophthalmology. 2008;126(10):1336–49. doi: 10.1001/archopht.126.10.1336. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Convergence Insufficiency Treatment Trial Study Group Long-term effectiveness of treatments for symptomatic convergence insufficiency in children. Optometry and Vision Science. 2009;86(9):1096–103. doi: 10.1097/OPX.0b013e3181b6210f. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gall C, Sabel BA. Reading performance after vision rehabilitation of subjects with homonymous visual field defects. PM&R: the Journal of Injury, Function, and Rehabilitation. 2012;4(12):928–35. doi: 10.1016/j.pmrj.2012.08.020. [DOI] [PubMed] [Google Scholar]
- Gell NM, Rosenberg DE, Demiris G, Lacroix AZ, Patel KV. Patterns of technology use among older adults with and without disabilities. Gerontologist. 2015;55(3):412–21. doi: 10.1093/geront/gnt166. [DOI] [PMC free article] [PubMed] [Google Scholar]
- George S, Hayes A, Chen C, Crotty M. The effect of static scanning and mobility training on mobility in people with hemianopia after stroke: a randomized controlled trial comparing standardized versus non-standardized treatment protocols. BMC Neurology. 2011;11(87):1–6. doi: 10.1186/1471-2377-11-87. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Jacbson WH. Transforming a traditional personnel preparation program in orientation and mobility into an online program at the University of Arkansas at Little Rock. Journal of Visual Impairment and Blindness. 2005;99(11):707–11. [Google Scholar]
- Jeon ST, Maurer D, Lewis TL. The effect of video game training on the vision of adults with bilateral deprivation amblyopia. Seeing and Perceiving. 2012;25(5):493–520. doi: 10.1163/18784763-00002391. [DOI] [PubMed] [Google Scholar]
- Jiang P, Luo T, Mo CJ, Gan XQ, Wang HJ. Intelligentized strabismus and amblyopia therapeutic apparatus for 216 cases of children's amblyopia. International Journal of Ophthalmology. 2005;5(2):395–7. [Google Scholar]
- Kämpf U, Muchamedjarow F, Seiler T. Amblyopia treatment by means of computer games with background stimulation: a placebo controlled pilot study of 10 days [Unterstützende Amblyopiebehandlung durch Computerspiele mit Hintergrundstimulation: Eine 10–tägige plazebokontrollierte Pilot–Studie]. Klinische Monatsblätter für Augenheilkunde. 2001;218(4):243–50. doi: 10.1055/s-2001-14921. [DOI] [PubMed] [Google Scholar]
- Kämpf U, Shamshinova A, Kaschtschenko T, Mascolus W, Pillunat L, Haase W. Long-term application of computer-based pleoptics in home therapy: selected results of a prospective multicenter study. Strabismus. 2008;16(4):149–58. doi: 10.1080/09273970802451125. [DOI] [PubMed] [Google Scholar]
- Kasten E, Sabel BA. Visual field enlargement after computer training in brain-damaged patients with homonymous deficits: an open pilot trial. Restorative Neurology and Neuroscience. 1995;8(3):113–27. doi: 10.3233/RNN-1995-8302. [DOI] [PubMed] [Google Scholar]
- Kasten E, Poggel DA, Sabel BA. Computer-based training of stimulus detection improves color and simple pattern recognition in the defective field of hemianopic subjects. Journal of Cognitive Neuroscience. 2000;12(6):1001–12. doi: 10.1162/08989290051137530. [DOI] [PubMed] [Google Scholar]
- Kasten E, Müller-Oehring E, Sabel BA. Stability of visual field enlargements following computer-based restitution training - results of a follow-up. Journal of Clinical and Experimental Neuropsychology. 2001;23(3):297–305. doi: 10.1076/jcen.23.3.297.1180. [DOI] [PubMed] [Google Scholar]
- Kerkhoff G. Rehabilitation of visuospatial cognition and visual exploration in neglect: a cross-over study. Restorative Neurology and Neuroscience. 1998;12(1):27–40. [PubMed] [Google Scholar]
- Komm DU, Kasten E, Sabel BA, Gall C. Rehabilitation outcome in chronic neglect patients with associated visual field loss: results of a blinded, randomized crossover study. European Journal of Neurology. 2009;16(S3):456. [Google Scholar]
- Larizza MF, Zukerman I, Bohnert F, Busija L, Bentley SA, Russell RA, et al. In-home monitoring of older adults with vision impairment: exploring patients', caregivers' and professionals' views. Journal of the American Medical Informatics Association. 2014;21(1):56–63. doi: 10.1136/amiajnl-2012-001586. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mines MJ, Bower KS, Lappan CM, Mazzoli RA, Poropatich RK. The United States Army ocular teleconsultation program 2004 through 2009. American Journal of Ophthalmology. 2011;152(1):126–32. doi: 10.1016/j.ajo.2011.01.028. [DOI] [PubMed] [Google Scholar]
- Powers MK, Grisham JD, Wurm JK, Wurm WC. Improving visual skills: II-remote assessment via Internet. Optometry. 2009;82(2):61–9. doi: 10.1016/j.optm.2008.01.025. [DOI] [PubMed] [Google Scholar]
- Puig de la Bellacasa R. Telecommunications, computers and other complementary communication means on behalf of the disabled. International Journal of Rehabilitation Research. 1980;3(2):191–204. doi: 10.1097/00004356-198006000-00005. [DOI] [PubMed] [Google Scholar]
- Ross FL. The use of computers in occupational therapy for visual-scanning training. American Journal of Occupational Therapy. 1992;46(4):314–22. doi: 10.5014/ajot.46.4.314. [DOI] [PubMed] [Google Scholar]
- Schenk T, Aimola L, Lane AR, Smith DT, Kerkhoff G, Ford G. Efficacy and feasibility of a home-based computer training for individuals with homonymous visual field defects. Behavioural Neurology. 2013;27(3):316. doi: 10.1177/1545968313503219. [DOI] [PubMed] [Google Scholar]
- Schiefer U, Nowomiejska K, Krapp E, Pätzold J, Johnson CA. K-Train - a computer-based, interactive training program with an incorporated certification system for practicing kinetic perimetry: evaluation of acceptance and success rate. Graefe's Archive for Clinical and Experimental Ophthalmology. 2006;244(10):1300–9. doi: 10.1007/s00417-006-0291-9. [DOI] [PubMed] [Google Scholar]
- Schinzel J, Dietze H, Muhlberg T, Paul F, Dorr J. Efficacy of vision restoration therapy after optic neuritis. Multiple Sclerosis. 2011;17(10 Suppl):S476. [Google Scholar]
- Srinivasan K, Ramesh SV, Babu N, Sanker N, Ray A, Karuna SM. Efficacy of a remote based computerised visual acuity measurement. British Journal of Ophthalmology. 2012;96(7):987–90. doi: 10.1136/bjophthalmol-2012-301751. [DOI] [PubMed] [Google Scholar]
- Tan JC, Poh EW, Srinivasan S, Lim TH. A pilot trial of tele-ophthalmology for diagnosis of chronic blurred vision. Journal of Telemedicine and Telecare. 2013;19(2):65–9. doi: 10.1177/1357633x13476233. [DOI] [PubMed] [Google Scholar]
- Tatarinov SA, Amel'ianova SG, Kashchenko TP, Lakomkin VI, Avuchenkova TN, Galich VI. The importance of using the computer in treating children with strabismus and amblyopia [Znachenie ispol'zovaniia komp'iutera pri lechenii deteǐ s kosoglaziem i ambliopieǐ ]. Vestnik Oftalmologii. 1993;109(5):28–9. [PubMed] [Google Scholar]
- Tennant MT, Greve MD, Rudnisky CJ, Hillson TR, Hinz BJ. Identification of diabetic retinopathy by stereoscopic digital imaging via teleophthalmology: a comparison to slide film. Canadian Journal of Ophthalmology. 2001;36(4):187–96. doi: 10.1016/s0008-4182(01)80039-9. [DOI] [PubMed] [Google Scholar]
- Tsitsiashvili E. Application of special computer programs for diagnostics and treatment of amblyopia. Georgian Medical News. 2007;(150):7–10. [PubMed] [Google Scholar]
- Ulrich JN, Poudyal G, Marks SJ, Vrabec TR, Marks B, Thapa AB, et al. Ocular telemedicine between Nepal and the USA: prevalence of vitreoretinal disease in rural Nepal. British Journal of Ophthalmology. 2009;93(5):698–9. doi: 10.1136/bjo.2008.151357. [DOI] [PubMed] [Google Scholar]
- Widdig W, Wagner D, Pleger B, Schmitz J, Malin JP, Tegenthoff M. Therapy options for cortical visual disorders: with particular consideration of tele-rehabilitation in cortical blindness [Therapiemöglichkeiten kortikaler sehstörungen: Unter besonderer berücksichtigung der tele–rehabilitation bei kortikaler blindheit]. Ergotherapie und Rehabilitation. 2006;45(10):10–4. [Google Scholar]
- Zhang W, Yang X, Liao M, Zhang N, Liu L. Internet-based perceptual learning in treating amblyopia. European Journal of Ophthalmology. 2013;23(4):539–45. doi: 10.5301/ejo.5000269. [DOI] [PubMed] [Google Scholar]
Additional references
- Binns AM, Bunce C, Dickinson C, Harper R, Tudor-Edwards R, Woodhouse M, et al. How effective is low vision service provision? A systematic review. Survey of Ophthalmology. 2012;57(1):34–65. doi: 10.1016/j.survophthal.2011.06.006. [DOI] [PubMed] [Google Scholar]
- Brennan DM, Tindall L, Theodoros D, Brown J, Campbell M, Christiana D, et al. A blueprint for telerehabilitation guidelines-October 2010. Telemedicine Journal and E-Health. 2011;17(8):662–5. doi: 10.1089/tmj.2011.0036. [DOI] [PubMed] [Google Scholar]
- Congdon N, O'Colmain B, Klaver CC, Klein R, Muñoz B, Friedman DS, et al. Causes and prevalence of visual impairment among adults in the United States. Archives of Ophthalmology. 2004;122(4):477–85. doi: 10.1001/archopht.122.4.477. [DOI] [PubMed] [Google Scholar]
- Crossland MD, Silva RS, Macedo AF. Smartphone, tablet computer and e-reader use by people with vision impairment. Ophthalmic and Physiological Optics. 2014;34(5):552–7. doi: 10.1111/opo.12136. [DOI] [PubMed] [Google Scholar]
- Foster A, Gilbert C, Johnson G. Changing patterns in global blindness: 1988-2008. Community Eye Health Journal. 2008;21(67):37. [PMC free article] [PubMed] [Google Scholar]
- Goldstein JE, Massof RW, Deremeik JT, Braudway S, Jackson ML, Kehler KB, et al. Baseline traits of low vision patients served by private outpatient clinical centers in the United States. Archives of Ophthalmology. 2012;130(8):1028–37. doi: 10.1001/archophthalmol.2012.1197. [DOI] [PMC free article] [PubMed] [Google Scholar]
- The Cochrane Collaboration Higgins JPT, Altman DG, Sterne JAC, Higgins JPT, Green S, editors. Chapter 8: Assessing risk of bias in included studies. Cochrane Handbook for Systematic Reviews of Interventions Version 5.1.0 (updated March 2011) 2011 Available from www.cochrane-handbook.org.
- The Cochrane Collaboration Higgins JPT, Green S, editors. Cochrane Handbook for Systematic Reviews of Interventions Version 5.1.0 (updated March 2011) 2011 Available from www.cochrane-handbook.org.
- Lamoureux EL, Chong E, Wang JJ, Saw SM, Aung T, Mitchell P, et al. Visual impairment, causes of vision loss, and falls: the Singapore Malay Eye Study. Investigative Ophthalmology and Visual Science. 2008;49(2):528–33. doi: 10.1167/iovs.07-1036. [DOI] [PubMed] [Google Scholar]
- Li T, Vedula SS, Hadar N, Parkin C, Lau J, Dickersin K. Innovations in data collection, management, and archiving for systematic reviews. Annals of Internal Medicine. 2015;162(4):287–94. doi: 10.7326/M14-1603. [DOI] [PubMed] [Google Scholar]
- Madden AC, Simmons D, McCarty CA, Khan MA, Taylor HR. Eye health in rural Australia. Clinical and Experimental Ophthalmology. 2002;30(5):316–21. doi: 10.1046/j.1442-9071.2002.00549.x. [DOI] [PubMed] [Google Scholar]
- Markowitz SN. Principles of modern low vision rehabilitation. Canadian Journal of Ophthalmology. 2006;41(3):289–312. doi: 10.1139/I06-027. [DOI] [PubMed] [Google Scholar]
- Massof RW. A model of the prevalence and incidence of low vision and blindness among adults in the U.S. Optometry and Vision Science. 2002;79(1):31–8. doi: 10.1097/00006324-200201000-00010. [DOI] [PubMed] [Google Scholar]
- Murthy KR, Murthy PR, Kapur A, Owens DR. Mobile diabetes eye care: experience in developing countries. Diabetes Research and Clinical Practice. 2012;97(3):343–9. doi: 10.1016/j.diabres.2012.04.025. [DOI] [PubMed] [Google Scholar]
- National Eye Institute, National Institutes of Health [13 August 2013];Low vision glossary. www.nei.nih.gov/lowvision/content/glossary.asp.
- Prathiba V, Rema M. Teleophthalmology: a model for eye care delivery in rural and underserved areas of India. International Journal of Family Medicine. 2011;2011 doi: 10.1155/2011/683267. Article ID 683267. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Reeves BC, Deeks JJ, Higgins JPT, Wells GA, The Cochrane Collaboration Higgins JPT, Green S, editors. Chapter 13: Including non-randomized studies. Cochrane Handbook for Systematic Reviews of Interventions Version 5.1.0 (updated March 2011) 2011 Available from www.cochrane-handbook.org.
- The Nordic Cochrane Centre, The Cochrane Collaboration. The Cochrane Collaboration . Review Manager (RevMan). 5.3. The Nordic Cochrane Centre; Copenhagen: 2014. [Google Scholar]
- Rogante M, Grigioni M, Cordella D, Giacomozzi C. Ten years of telerehabilitation: a literature overview of technologies and clinical applications. NeuroRehabilitation. 2010;27(4):287–304. doi: 10.3233/NRE-2010-0612. [DOI] [PubMed] [Google Scholar]
- Stelmack JA, Tang XC, Reda DJ, Rinne S, Mancil RM, Massof RW, et al. Outcomes of the Veterans Affairs Low Vision Intervention Trial (LOVIT). Archives of Ophthalmology. 2008;126(5):608–17. doi: 10.1001/archopht.126.5.608. [DOI] [PubMed] [Google Scholar]
- Tang RA, Morales M, Ricur G, Schiffman JS. Telemedicine for eye care. Journal of Telemedicine and Telecare. 2005;11(8):391–6. doi: 10.1177/1357633X0501100803. [DOI] [PubMed] [Google Scholar]
- Turner RM, Davey J, Clarke MJ, Thompson SG, Higgins JP. Predicting the extent of heterogeneity in meta-analysis, using empirical data from the Cochrane Database of Systematic Reviews. International Journal of Epidemiology. 2012;41(3):818–27. doi: 10.1093/ije/dys041. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Van den Berg N, Schumann M, Kraft K, Hoffmann W. Telemedicine and telecare for older patients--a systematic review. Maturitas. 2012;73(2):94–114. doi: 10.1016/j.maturitas.2012.06.010. [DOI] [PubMed] [Google Scholar]
- Watson GR, De L'Aune W, Stelmack J, Maino J, Long S. National survey of the impact of low vision device use among veterans. Optometry and Vision Science. 1997;74(5):249–59. doi: 10.1097/00006324-199705000-00019. [DOI] [PubMed] [Google Scholar]
- World Health Organization [13 August 2013];Priorities and objectives - What do we want to achieve? Chapter 3.5.4 Low vision. www.who.int/ncd/vision2020 actionplan/contents/3.5.4.htm.
References to other published versions of this review
- Bittner AK, Wykstra SL, Yoshinaga PD, Li T. Telerehabilitation for people with low vision. Cochrane Database of Systematic Reviews. 2014;(3) doi: 10.1002/14651858.CD011019. DOI: 10.1002/14651858.CD011019. [DOI] [PMC free article] [PubMed] [Google Scholar]